Abstract
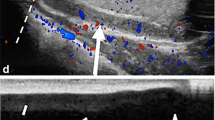
Scrotal ultrasonography (US) is usually the initial imaging modality for evaluating patients who present with acute pathologic conditions of the scrotum. Acute epididymitis, acute epididymo-orchitis, torsion of the spermatic cord (TSC), and other acute scrotal abnormalities may have similar findings at clinical examination. Pain and swelling make the clinical examination difficult, sometimes practically impossible, potentially resulting in management delays. The objective of this review is to summarize the main clinical signs of the TSC and to illustrate and briefly discuss the US features of this entity, including gray-scale imaging, color Doppler with spectral analysis, and power Doppler sonography. Although TSC can occur at any age, it is most common in adolescent boys. The intensity of the symptoms and the US findings vary with the duration of the torsion, number of twists in the spermatic cord (degree of rotation), and how tightly the vessels of the cord are compressed. An enlarged, more spherical, and diffusely hypoechogenic testis without detectable arterial and venous testicular flow at color and power Doppler US is considered diagnostic of acute testicular ischemia. The presence of a color or power Doppler signal in one part of the testis does not exclude TSC. Positive blood flow but significantly diminished, usually near or inside the mediastinum, may be found, mainly in the partial or incomplete TSC. Identification of a large echogenic extratesticular mass distal to the site of the torsion, frequently misinterpreted as a chronic epididymitis, can be the key to the diagnosis of TSC. When a small arterial sign is found a low amplitude waveform is present with an increased resistive index on the affected side due to a diminished, absent, or reversed diastolic flow. Gray-scale imaging, color Doppler, power Doppler and pulsed Doppler with spectral analysis are very effective to make or exclude the diagnosis of TSC.





















Similar content being viewed by others
References
Süzer O, Özcan H, Küpeli S, et al. Color Doppler imaging in the diagnosis of the acute scrotum. Eur Urol 1997;32: 457–461
Dubinsky TJ, Chen P, Maklad N Color-flow and power Doppler imaging of the testes. World J Urol 1998;16:35–40
Kadish HA, Bolfe RG A retrospective review of pediatric patients with epididymitis, testicular torsion, and torsion of testicular appendages. Pediatrics 1998;102:73–76
Kass EJ, Lundak B The acute scrotum. Pediatr Clin North Am 1997;44: 1251–1266
Lin EP, Bhatt S, Rubens DJ, et al. Testicular torsion: twists and turns. Semin Ultrasound CT MRI 2007;28:317–328
Dogra VS, Gottlieb RH, Oka M, et al. Sonography of the scrotum. Radiology 2003; 227:18–36
Siegel MJ The acute scrotum. Radiol Clin North Am 1997;35: 959–976
Hörmann M, Balassy C, Philipp MO, et al. Imaging of the scrotum in children. Eur Radiol 2004;14:974–983
Oyen RH Scrotal ultrasound. Eur Radiol 2002;12:19–34
Favorito LA, Cavalcante AG, Costa WS Anatomic aspects of epididymis and tunica vaginalis in patients with testicular torsion. Int Braz J Urol 2004;30:420–424
Ringdhal E, Teague L Testicular torsion. Am Fam Physician 2006;74:1739–1743
Pavlica P, Barozzi L Imaging of the acute scrotum. Eur Radiol 2001;11:220–228
Frush DP, Sheldon CA Diagnostic Imaging for pediatric scrotal disorders. Radiographics 1998;18:969–985
Prando D Torsion of the spermatic cord: sonographic diagnosis. Ultrasound Quart 2002;18:41–57
Noske HD, Kraus SW, Altinkilic BM et al. Historical milestones regarding torsion of the scrotal organs. J Urol 1998;159:13–16
Schulsinger D, Glassberg K, Strashun A Intermittent torsion: association with horizontal lie of the testicle. J Urol 1991;145:1053
Albrecht T, Lotzof K, Hussain HK et al. Power Doppler US of the normal prepubertal testis: does it live up to its promises? Radiology 1997;203:227–231
Dogra VS, Sessions A, Mevorach RA, et al. Reversal of diastolic plateau in partial testicular torsion. J Clin Ultrasound 2001;29:105–108
Hernanz-Shulman M, Yenicesu F, Heller RM, et al. Sonographic identification of perinatal testicular torsion. J Ultrasound Med 1997;16:65–67
Zinn HL, Cohen HL, Horowitz M Testicular torsion in neonates: importance of power Doppler imaging. J Ultrasound Med 1998;17:385–388
Paltiel HJ, Connolly LP, Atala A et al. Acute scrotal symptoms in boys with an indeterminate clinical presentation: comparison of color Doppler sonography and scintigraphy. Radiology 1998;207:223–231
Sanelli PC, Burke BJ, Lee L Color and spectral Doppler sonography of partial torsion of the spermatic cord. AJR 1999;172:45–51
Aso C, Enríquez G, Fité M, et al. Gray-scale and color Doppler sonography of scrotal disorders in children: an update. Radiographics 2005;25:1197–1214
Prando D. Diagnostico por imagem. Ultra-sonografia escrotal. In: Hering FLO, Srougi M, eds. Urologia. Diagnóstico e tratamento. São Paulo, Roca, 1998; 35–66
Prando D. Escroto. In: Prando A, Prando D, Caserta NMG, Bauab Jr. T, eds. Urologia. Diagnóstico por Imagem. São Paulo: Sarvier, 1997:349–381
Dijk van R, Karthaus HFM Ultrasonography of the spermatic cord in testicular torsion. Eur J Radiol 1994;18:220–223
Baud C, Veyrac C, Couture A, et al. Spiral twists of the spermatic cord: a reliable sign of testicular torsion. Pediatr Radiol 1998;28:950–954
Vijayaraghavan SB Sonographic differential diagnosis of acute scrotum: real time whirlpool sign, a key sign of torsion. J Ultrasound Med 2006;25:563–574
Kalfa N, Veyrac C, Baud C, et al. Ultrasonography of the spermatic cord in children with testicular torsion: impact on the surgical strategy. J Urol 2004;172:1692–1695
Middleton WD, Middleton MA, Dierks M, et al. Sonographic prediction of viability in testicular torsion. J Ultrasound Med 1997;16:23–27
Dogra VS, Bhatt S, Rubens DJ Sonographic evaluation of testicular torsion. Ultrasound Clin 2006;1:55–66
Dogra VS, Bhatt S Acute painful scrotum. Radiol Clin North Am 2004;42 (9):349–363
Galejs LE, Kass EJ Color Doppler ultrasound of the acute scrotum. Tech Urol 1998;4:182–184
Arce JD, Cortes M, Vargas JC Sonographic diagnosis of acute spermatic cord torsion. Rotation of the cord: a key to diagnosis. Pediatr Radiol 2002;32:485–491
Jee WH, Choe BY, Byun JY et al. Resistive index of the intrascrotal artery in scrotal inflammatory disease. Acta Radiol 1997;38:1026–1029
Lucker GD, Siegel MJ Scrotal US in pediatric patients: comparison of power and standard color Doppler US. Radiology 1996;198:381–385
Barth RA, Shortliffe LD Normal pediatric testis: comparison of power Doppler and color Doppler US in the detection of blood flow. Radiology 1997;204:389–393
Bader TR, Kammerhuber F, Herneth AM Testicular blood flow in boys as assessed at color Doppler and power Doppler sonography. Radiology 1997;202:559–564
Babcock DS, Patriquin H, LaFortune M et al. Power Doppler sonography: basic principles and clinical applications in children. Pediatric Radiol 1996;26:109–115
Liao L, Dogra VS, Oka M, et al. (2000) Torsion and beyond: new twists in spectral Doppler evaluation of the scrotum (abstr.). RSNA Scientific program
Sanders LM, Haber S, Dembner A, et al. Significance of reversal of diastolic flow in the acute scrotum. J Ultrasound Med 1994;13:137–139
Dogra VS, Rubens DJ, Gottlieb RH, et al. Torsion and beyond: new twists in spectral Doppler evaluation of the scrotum. J Ultrasound Med 2004;23:1077–1085
Williamson RCN (1976) Torsion of the testis and allied conditions. Br J Sur 63:465–476
Skoglund RW, McRoberts JW, Radge H (1970) Torsion of the spermatic cord: A review of the literature and an analysis of 70 new cases. J Urol 104:604–607
Dogra VS, Bhatt S (2006) Acute scrotal pain: imaging evaluation for a more specific diagnosis. RSNA Categorical course in Diagnostic radiology, pp 255–269
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Prando, D. Torsion of the spermatic cord: the main gray-scale and doppler sonographic signs. Abdom Imaging 34, 648–661 (2009). https://doi.org/10.1007/s00261-008-9449-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-008-9449-8