Abstract
Background
The position of the tip of a peripherally inserted central catheter (PICC) is crucial; malposition can lead to malfunction of the line or life-threatening events (e.g., arrhythmias, perforation).
Objective
To determine what factors other than arm position and accessed vein might influence the tip position of a PICC.
Materials and methods
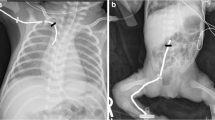
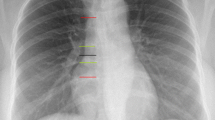
Inclusion criteria were upper limb PICC placement, body weight <20 kg, intraoperative imaging with the arm in 0°, 45° and 90° abduction and an arm view marking the skin entry site relative to the shoulder. Evaluated variables included patient demographics, and PICC and insertion site characteristics. We measured central tip movement in rib units.
Results
We included 112 children who received a PICC (42 girls/70 boys, mean age 31±13 months, mean weight 6.5±4.9 kg). The overall range of central tip movement was -1 to +4 rib units (mean +0.8±0.7 rib units). Silicone PICCs moved significantly less than polyurethane PICCs (P<0.05). PICCs placed in the cephalic vein moved significantly less than those placed in other veins (P<0.05). Patient demographics and PICC characteristics (size, number of lumens, left or right arm accessed, length of the line) did not influence the range of central tip movement of a PICC (P>0.05).
Conclusion
Silicone PICCs and PICCs inserted into the cephalic vein move less than PICCs made of polyurethane and PICCs inserted into the brachial and basilic veins. These findings might assist operators in deciding which PICC to place in children in a given clinical context.



Similar content being viewed by others
References
Connolly B, Mawson JB, MacDonald CE et al (2000) Fluoroscopic landmark for SVC-RA junction for central venous catheter placement in children. Pediatr Radiol 30:692–695
NAoVA Networks (1998) NAVAN position statement. J Vasc Access Devices 3:8–10
Baskin KM, Jimenez RM, Cahill AM et al (2008) Cavoatrial junction and central venous anatomy: implications for central venous access tip position. J Vasc Interv Radiol 19:359–365
Darling JC, Newell SJ, Mohamdee O et al (2001) Central venous catheter tip in the right atrium: a risk factor for neonatal cardiac tamponade. J Perinatol 21:461–464
Murray BH, Cohle SD, Davison P (1996) Pericardial tamponade and death from Hickman catheter perforation. Am Surg 62:994–997
Puel V, Caudry M, Le Métayer P et al (1993) Superior vena cava thrombosis related to catheter malposition in cancer chemotherapy given through implanted ports. Cancer 72:2248–2252
Racadio JM, Doellman DA, Johnson ND et al (2001) Pediatric peripherally inserted central catheters: complication rates related to catheter tip location. Pediatrics 107:E28
Nadroo AM, Glass RB, Lin J et al (2002) Changes in upper extremity position cause migration of peripherally inserted central catheters in neonates. Pediatrics 110:131–136
Connolly B, Amaral J, Walsh S et al (2006) Influence of arm movement on central tip location of peripherally inserted central catheters (PICCs). Pediatr Radiol 36:845–850
Crnich CJ, Halfmann JA, Crone WC et al (2005) The effects of prolonged ethanol exposure on the mechanical properties of polyurethane and silicone catheters used for intravascular access. Infect Control Hosp Epidemiol 26:708–714
Walder T (2013) Thermoplastic polyurethanes as medical grade thermoplastic elastomer. 1–7. http://files.eventsential.org/61198b3c-1544-484a-a2b1-01ec6810ec04/event-58/29265646-Walder%20Paper%20Material%20101513[1]-thermoplastic.pdf. Accessed 5 May 2016
Moran BJ, Sutton GL, Karran SJ (1992) Clinical evaluation of percutaneous insertion and long-term usage of a new cuffed polyurethane catheter for central venous access. Ann R Coll Surg Engl 74:426–429
Young MD, Streicher MC, Beck RJ et al (2012) Simulation of lower limb axial arterial length change during locomotion. J Biomech 45:1485–1490
Dubois J, Rypens F, Garel L et al (2007) Incidence of deep vein thrombosis related to peripherally inserted central catheters in children and adolescents. CMAJ 177:1185–1190
Collins JL, Lutz RJ (1991) In vitro study of simultaneous infusion of incompatible drugs in multilumen catheters. Heart Lung 20:271–277
Gravenstein N, Blackshear RH (1991) In vitro evaluation of relative perforating potential of central venous catheters: comparison of materials, selected models, number of lumens, and angles of incidence to simulated membrane. J Clin Monit 7:1–6
Forauer AR, Alonzo M (2000) Change in peripherally inserted central catheter tip position with abduction and adduction of the upper extremity. J Vasc Interv Radiol 11:1315–1318
Acknowledgments
Author Ralph Gnannt was supported by EMDO (Emily Dorothy Lageman) Foundation and Helmut-Hartweg Funds. We thank the Image-Guided Therapy team at the Hospital for Sick Children for assisting with recording and labeling of all the images used for our data analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Gnannt, R., Connolly, B.L., Parra, D.A. et al. Variables decreasing tip movement of peripherally inserted central catheters in pediatric patients. Pediatr Radiol 46, 1532–1538 (2016). https://doi.org/10.1007/s00247-016-3648-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-016-3648-1