Abstract
Purpose
The aims of the present analysis were to determine prevalence of transaminase elevation in placebo-treated healthy volunteers in our historical phase I clinical trials and to assess which factors were associated with it.
Methods
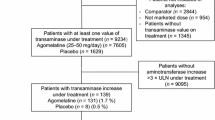
We performed a retrospective analysis of alanine transaminase (ALT) levels in 481 placebo-treated healthy volunteers from 20 phase I trials by examining ALT elevation rates using the upper limit of normal values (ULN) as the cutoff as well as changes from baseline in actual ALT values.
Results
The ULN for ALT ranged from 32 to 72 IU/L across the studies. Although the overall ALT elevation rate (4.4%) from pooled datasets was low, the elevation rates were higher in more recent studies than in earlier ones. While elevation rates at baseline and during placebo treatment did not differ significantly, ALT maximal levels during placebo treatment were significantly higher than baseline levels. Moreover, baseline ALT levels were found to be more important in predicting ALT elevation during placebo treatment than demographic and study design factors.
Conclusion
Baseline level and changes from baseline in transaminase are important variables to examine in addition to elevation above ULN for more reliably interpreting liver signals in Phase I clinical trials.





Similar content being viewed by others
References
Narjes H, Nehmiz G (2000) Effect of hospitalisation on transaminases in healthy subjects. Eur J Clin Pharmacol 56:329–333
Rosenzweig P, Miget N, Brohier S (1999) Transaminase elevation on placebo during phase I trials: prevalence and significance. Br J Clin Pharmacol 48:19–23
Kobayashi M, Yamada N, Shibata H, Nishikawa T (1993) Elevated serum transaminase values in volunteers after ad- ministration of placebo in a phase I study. Jpn J Clin Pharmacol Ther 24:493–496
Kanamaru M, Nagashima S, Uematsu T, Nakashima M (1989) Influence of 7-day hospitalisation for phase I study on the biochemical laboratory tests of healthy volunteers. Jpn J Clin Pharmacol Ther 20:493–503
Cutler NR, Sramek JJ, Greenblatt DJ, Chaikin P, Ford N, Lesko JL (1997) Defining the maximum tolerated dose: investigator, academic, industry and regulatory perspectives. J Clin Pharmacol 37:767–783
Golik A, Rubio A, Weibtraub M, Byrne L (1991) Elevated serum liver enzymes in obesity: a dilemma during clinical trials. Int J Obes 15:797–801
Azuma J, Seto Y, Mochizuki N, Maruyama K, Ogura M (1993) Changes in the serum enzyme levels and the predicting factors during 2 weeks hospitalisation in healthy volunteers: a retrospective study. Jpn J Clin Pharmacol Ther 24:385–396
Porikos KP, van Itallie TB (1983) Diet-induced changes in serum transaminase and triglyceride levels in healthy adult men. Am J Med 75:624–630
Irwin MI, Staton AJ (1969) Dietary wheat starch and sucrose. Effect on levels of five enzymes in blood serum of young adults. Am J Clin Nutr 22:701–709
CDISC Study Data Tabulation Model SDTM Implementation Guide V3.1.1. Available at: http://www.cdisc.org/models/sdtm/v1.1/index.html. Accessed 12 Feb 2009
Spotfire, Inc (1996–2007) Spotfire DecisionSite 9.0 (SP2). Available at: http://spotfire.tibco.com/,
Breiman L (2001) Random forests. Mach Learning 45:5–32
Quinn PG, Johnston DE (1997) Detection of chronic liver disease: costs and benefits. Gastroenterologist 5:58–77
Sherman KE (1991) Alanine transaminase in clinical practice. Arch Intern Med 151:260–265
Brinkmann T, Dreier J, Diekmann J, Götting C, Klauke R, Schumann G et al (2003) Alanine aminotransferase cut-off values for blood donor screening using the new International Federation of Clinical Chemistry reference method at 37°C. Vox Sanguinis 85:159–164
Piton A, Poynard T, Imbert-Bismut F, Khalil L, Delattre J, Pelissier E et al (1998) Factors associated with serum alanine transaminase activity in healthy subjects: consequences for the definition of normal values, for selection of blood donors, and for patients with chronic hepatitis C. Hepatology 27:1213–1219
Ruhl CE, Everhart JE (2003) Determinants of the association of overweight with elevated serum alanine aminotransferase activity in the United States. Gastroenterology 124:71–79
Carter-Pokras OD, Najjar MF, Billhymer BF, Shulman IA (1993) Alanine aminotransferase levels in Hispanics. Ethn Dis 3:176–180
Manolio TA, Burke GL, Savage PJ, Jacobs DR Jr, Sidney S, Wagenknecht LE et al (1992) Sex- and race-related differences in liver-associated serum chemistry tests in young adults in the CARDIA study. Clin Chem 38:1853–1859
Kariv R, Leshno M, Beth-Or A, Strul H, Blendis L, Kokia E et al (2006) Re-evaluation of serum alanine aminotransferase upper normal limit and its modulating factors in a large-scale population study. Liver Int 26:445–450
Prati D, Taioli E, Zanella A, Della Torre E, Butelli S, Del Vecchio E et al (2002) Updated definitions of healthy ranges for serum alanine aminotransferase levels. Ann Intern Med 137:1–10
Sibille M, Deigat N, Durieu I et al (1999) Laboratory data in healthy volunteers: reference values, reference changes, screening and laboratory adverse event limits in Phase I clinical trials. Eur J Clin Pharmacol 55:13–19
Stromme JH, Rustad P, Steensland H et al (2004) Reference intervals for eight enzymes in blood of adult females and males measured in accordance with the International Federation of Clinical Chemistry reference system at 37 degrees C: part of the Nordic Reference Interval Project. Scand J Clin Lab Invest 64:371–384
Kechagias S, Ernersson A, Dahlqvist O, Lundberg P, Lindström T, Nystrom FH et al (2008) Fast-food-based hyper-alimentation can induce rapid and profound elevation of serum alanine aminotransferase in healthy subjects. Gut 57:568–670
Clark JM, Brancati FL, Diehl AM (2003) The prevalence and etiology of elevated transaminase levels in the United States. Am J Gastroenterol 98:960–967
Hay JE, Czaja AJ, Rakela J, Ludwig J (1989) The nature of unexplained chronic aminotransferase elevations of a mild to moderate degree in asymptomatic patients. Hepatology 9:193–197
Daniel S, Ben-Menachem T, Vasudevan G, Ma CK, Blumenkehl M (1999) Prospective evaluation of unexplained chronic liver transaminase abnormalities in asymptomatic and symptomatic patients. Am J Gastroenterol 94:3010–3014
Browning JD, Szczepaniak LS, Dobbins R et al (2004) Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology 40:1387–1395
Friedman LS, Dienstag JL, Watkins E et al (1987) Evaluation of blood donors with elevated serum alanine aminotransferase levels. Ann Intern Med 107:137–144
Kundrotas LW, Clement DJ (1993) Serum alanine aminotransferase (ALT) elevation in asymptomatic US Air Force basic trainee blood donors. Dig Dis Sci 38:2145–2150
Yu AS, Keeffe EB (2003) Elevated AST or ALT to nonalcoholic fatty liver disease: accurate predictor of disease prevalence? Am J Gastroenterol 98:955–956
Mathiesen UL, Franzen LE, Fryden A et al (1999) The clinical significance of slightly to moderately increased liver transaminase values in asymptomatic patients. Scand J Gastroenterol 34:85–91
Skelly MM, James PD, Ryder SD (2001) Findings on liver biopsy to investigate abnormal liver function tests in the absence of diagnostic serology. J Hepatol 35:195–199
Acknowledgments
We thank the following people for their input to this analysis: Brian Bryzinski, Susan Harris, Ulf Hindorf, Stuart Oliver, John Pears, Debra Silberg, and Harry Southworth
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cai, Z., Christianson, A.M., Ståhle, L. et al. Reexamining transaminase elevation in Phase I clinical trials: the importance of baseline and change from baseline. Eur J Clin Pharmacol 65, 1025–1035 (2009). https://doi.org/10.1007/s00228-009-0684-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-009-0684-x