Abstract
Summary
This study aims to analyze the impact of participation in vigorous physical activity as it can promote a healthy bone development. Adolescents who increased their participation in vigorous physical activity showed higher improvements in bone parameters compared to those who did not, which highlights the relevance of vigorous physical activity engagement.
Introduction
The main purpose of the study was to analyze the effects of different patterns of vigorous physical activity (VPA) on bone development.
Methods
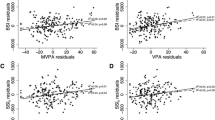
One-week accelerometry registers and dual-energy X-ray absorptiometry scans at the whole body, hip, and lumbar spine of 140 healthy male adolescents (11–13 years, at baseline) were performed twice with a 1-year interval between measurements. Four patterns of VPA evolution (“low–low,” “low–high,” “high–low,” and “high–high”) and three patterns of bone growth (“optimal,” “mean,” and “reduced”) were defined according to the median participation in VPA and a cluster analysis of the longitudinal changes in BMC and BMD in all sites measured, respectively. Bone mineral parameters were adjusted for skeletal age and body weight prior to statistical comparison among groups.
Results
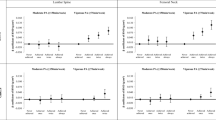
Participants in the “low–high” group had greater adjusted BMD increases at both the femoral neck and lumbar spine when compared to the “low–low” group (estimated mean (95% CI) 0.066 (0.047–0.085) vs. 0.034 (0.021–0.047) g/cm2 and 0.074 (0.054–0.093) vs. 0.049 (0.035–0.062) g/cm2 respectively, both p < 0.05). Femoral neck BMD adjusted increase was also different between the “high–high” and the “high–low” groups (0.053 (0.041–0.066) vs. 0.030 (0.011–0.049) g/cm2, p < 0.05). Additionally, a higher percentage of “optimal” growth was found in the “low–high” group than in the “low–low” and “high–low” categories (36.3, 12.5 and 13.6% respectively, p < 0.05).
Conclusions
Engaging in VPA as well as maintaining high levels of VPA during puberty is associated with greater gains in bone mass, which can have an impact in future bone health.


Similar content being viewed by others
References
Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jönsson B, Kanis JA (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden: a report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8(136):136. https://doi.org/10.1007/s11657-013-0136-1
Wright NC, Looker AC, Saag KG, Curtis JR, Delzell ES, Randall S, Dawson-Hughes B (2014) The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res 29:2520–2526. https://doi.org/10.1002/jbmr.2269
Peck WA, Burckhardt P, Christiansen C et al (1993) Consensus development conference: diagnosis, prophylaxis, and treatment of osteoporosis. American Journal of Medicine, In, pp 646–650
Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR (2009) Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA 301:513–521. https://doi.org/10.1001/jama.2009.50
Cooper C, Cole ZA, Holroyd CR et al (2011) Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos Int 22:1277–1288
Rizzoli R, Bianchi ML, Garabédian M, McKay HA, Moreno LA (2010) Maximizing bone mineral mass gain during growth for the prevention of fractures in the adolescents and the elderly. Bone 46:294–305. https://doi.org/10.1016/j.bone.2009.10.005
Pocock NA, Eisman JA, Hopper JL, Yeates MG, Sambrook PN, Eberl S (1987) Genetic determinants of bone mass in adults: a twin study. J Clin Invest 80:706–710. https://doi.org/10.1172/jci113125
Vicente-Rodríguez G (2006) How does exercise affect bone development during growth? Sport Med 36:561–569
Baxter-Jones ADG, Faulkner RA, Forwood MR, Mirwald RL, Bailey DA (2011) Bone mineral accrual from 8 to 30 years of age: an estimation of peak bone mass. J Bone Miner Res 26:1729–1739. https://doi.org/10.1002/jbmr.412
Bonjour JP, Chevalley T, Ferrari S, Rizzoli R (2009) The importance and relevance of peak bone mass in the prevalence of osteoporosis. Salud Publica Mex 51:5–17. https://doi.org/10.1590/S0036-36342009000700004
Weaver CM, Gordon CM, Janz KF, Kalkwarf HJ, Lappe JM, Lewis R, O’Karma M, Wallace TC, Zemel BS (2016) The National Osteoporosis Foundation’s position statement on peak bone mass development and lifestyle factors: a systematic review and implementation recommendations. Osteoporos Int 27:1281–1386. https://doi.org/10.1007/s00198-015-3440-3
Poitras VJ, Gray CE, Borghese MM, Carson V, Chaput JP, Janssen I, Katzmarzyk PT, Pate RR, Connor Gorber S, Kho ME, Sampson M, Tremblay MS (2016) Systematic review of the relationships between objectively measured physical activity and health indicators in school-aged children and youth. Appl Physiol Nutr Metab 6:S197–S239. https://doi.org/10.1139/apnm-2015-0663
Lappe JM, Watson P, Gilsanz V, Hangartner T, Kalkwarf HJ, Oberfield S, Shepherd J, Winer KK, Zemel B (2015) The longitudinal effects of physical activity and dietary calcium on bone mass accrual across stages of pubertal development. J Bone Miner Res 30:156–164. https://doi.org/10.1002/jbmr.2319
Gunter KB, Almstedt HC, Janz KF (2012) Physical activity in childhood may be the key to optimizing lifespan skeletal health. Exerc Sport Sci Rev 40:13–21. https://doi.org/10.1097/JES.0b013e318236e5ee.Physical
Robling AG (2009) Is bone’s response to mechanical signals dominated by muscle forces? Med Sci Sports Exerc 41:2044–2049. https://doi.org/10.1249/MSS.0b013e3181a8c702
Borer KT (2005) Physical activity in the prevention and amelioration of osteoporosis in women: interaction of mechanical, hormonal and dietary factors. Sports Med 35:779–830
Holroyd C, Harvey N, Dennison E, Cooper C (2012) Epigenetic influences in the developmental origins of osteoporosis. Osteoporos Int 23:401–410. https://doi.org/10.1007/s00198-011-1671-5
Daly RM (2007) The effect of exercise on bone mass and structural geometry during growth. Med Sport Sci 51:33–49. https://doi.org/10.1159/0000103003
Gunter K, Baxter-Jones AD, Mirwald RL et al (2007) Impact exercise increases BMC during growth: an 8-year longitudinal study. J Bone Miner Res 23:986–993. https://doi.org/10.1359/jbmr.071201
Janz KF, Letuchy EM, Francis SL, Metcalf KM, Burns TL, Levy SM (2014) Objectively measured physical activity predicts hip and spine bone mineral content in children and adolescents ages 5-15 years: Iowa bone development study. Front Endocrinol (Lausanne) 5:1–7. https://doi.org/10.3389/fendo.2014.00112
Gracia-Marco L, Moreno LA, Ortega FB, León F, Sioen I, Kafatos A, Martinez-Gomez D, Widhalm K, Castillo MJ, Vicente-Rodríguez G, HELENA Study Group (2011) Levels of physical activity that predict optimal bone mass in adolescents: The HELENA study. Am J Prev Med 40:599–607. https://doi.org/10.1016/j.amepre.2011.03.001
Janz KF, Letuchy EM, Burns TL et al (2014) Objectively measured physical activity trajectories predict adolescent bone strength: Iowa Bone Development Study. Br J Sports Med 48:1032–1036. https://doi.org/10.1249/MSS.0000000000000648
Cardadeiro G, Baptista F, Ornelas R, Janz KF, Sardinha LB (2012) Sex specific association of physical activity on proximal femur BMD in 9 to 10 year-old children. PLoS One 7:e50657. https://doi.org/10.1371/journal.pone.0050657
Hasselstrøm H, Karlsson KM, Hansen SE, Grønfeldt V, Froberg K, Andersen LB (2007) Peripheral bone mineral density and different intensities of physical activity in children 6-8 years old: the Copenhagen School Child Intervention Study. Calcif Tissue Int 80:31–38. https://doi.org/10.1007/s00223-006-0137-9
Katzman DK, Bachrach LK, Carter DR, Marcus R (1991) Clinical and anthropometric correlates of bone mineral acquisition in healthy adolescent girls*. J Clin Endocrinol Metab 73:1332–1339. https://doi.org/10.1210/jcem-73-6-1332
Carter DR, Bouxsein ML, Marcus R (2009) New approaches for interpreting projected bone densitometry data. J Bone Miner Res 7:137–145. https://doi.org/10.1002/jbmr.5650070204
Greulich WW, Pyle SI (1959) Radiographic atlas of skeletal development of the hand and wrist. Am J Med Sci 238:393
Groell R, Lindbichler F, Riepl T, Gherra L, Roposch A, Fotter R (1999) The reliability of bone age determination in central European children using the Greulich and Pyle method. Br J Radiol 72:461–464. https://doi.org/10.1259/bjr.72.857.10505010
Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG (2008) Calibration of two objective measures of physical activity for children. J Sports Sci 26:1557–1565
Trost SG, Loprinzi PD, Moore R, Pfeiffer KA (2011) Comparison of accelerometer cut points for predicting activity intensity in youth. Med Sci Sports Exerc 43:1360–1368. https://doi.org/10.1249/MSS.0b013e318206476e
Holman RM, Carson V, Janssen I (2011) Does the fractionalization of daily physical activity (sporadic vs. bouts) impact cardiometabolic risk factors in children and youth? PLoS One 6:1–7. https://doi.org/10.1371/journal.pone.0025733
Gore PA (2000) Cluster analysis. In: Tinsley HEA, Brown SD (eds) Handbook of Applied Multivariate Statistics and Mathematical Modeling. Academic Press, San Diego, pp 297–321
Ivuškāns A, Mäestu J, Jürimäe T, Lätt E, Purge P, Saar M, Maasalu K, Jürimäe J (2015) Sedentary time has a negative influence on bone mineral parameters in peripubertal boys: a 1-year prospective study. J Bone Miner Metab 33:85–92. https://doi.org/10.1007/s00774-013-0556-4
Francis SL, Letuchy EM, Levy SM, Janz KF (2014) Sustained effects of physical activity on bone health: Iowa Bone Development Study. Bone 63:95–100. https://doi.org/10.1016/j.bone.2014.03.004
Christoffersen T, Winther A, Nilsen OA, Ahmed LA, Furberg AS, Grimnes G, Dennison E, Emaus N (2015) Does the frequency and intensity of physical activity in adolescence have an impact on bone? The Tromsø Study, Fit Futures. BMC Sports Sci Med Rehabil 7:26. https://doi.org/10.1186/s13102-015-0020-y
Sayers A, Mattocks C, Deere K, Ness A, Riddoch C, Tobias JH (2011) Habitual levels of vigorous, but not moderate or light, physical activity is positively related to cortical bone mass in adolescents. J Clin Endocrinol Metab 96:793–802. https://doi.org/10.1210/jc.2010-2550
Deere K, Sayers A, Rittweger J, Tobias JH (2012) Habitual levels of high, but not moderate or low, impact activity are positively related to hip BMD and geometry: results from a population-based study of adolescents. J Bone Miner Res 27:1887–1895. https://doi.org/10.1002/jbmr.1631
Frost HM (2003) Bone’s mechanostat: a 2003 update. Anat Rec Part A Discov Mol Cell Evol Biol 275:1081–1101
Bakker I, Twisk JWR, Van Mechelen W, Kemper HCG (2003) Fat-free body mass is the most important body composition determinant of 10-yr longitudinal development of lumbar bone in adult men and women. J Clin Endocrinol Metab 88:2607–2613. https://doi.org/10.1210/jc.2002-021538
Kriemler S, Zahner L, Puder JJ, Braun-Fahrländer C, Schindler C, Farpour-Lambert NJ, Kränzlin M, Rizzoli R (2008) Weight-bearing bones are more sensitive to physical exercise in boys than in girls during pre- and early puberty: a cross-sectional study. Osteoporos Int 19:1749–1758. https://doi.org/10.1007/s00198-008-0611-5
Marcus R (1996) Mechanisms of exercise effects on bone. Princ bone Biol 151:1135–1146
MacKelvie KJ, Khan KM, McKay HA (2002) Is there a critical period for bone response to weight-bearing exercise in children and adolescents? A systematic review. Br J Sports Med 36:250–257. https://doi.org/10.1136/bjsm.36.4.250
Klein-Nulend J, Bacabac RG, Bakker AD (2012) Mechanical loading and how it affects bone cells: the role of the osteocyte cytoskeleton in maintaining our skeleton. Eur Cell Mater 24:278–291
Funding
JMP received a grant from ‘Ministerio de Educación Cultura y Deportes’ (FPU014/04302). This study was funded by the Estonian Ministry of Education and Science (IUT 20-58).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study protocol followed the ethical guidelines of the Declaration of Helisinki and was approved by the Human Ethical Committee of the University of Tartu, Estonia (179/T-4). Signed informed consent was retrieved from all the participants and their parents prior to the beginning of the tests. They were also given a full written description of the study characteristics before signing the informed consent.
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Marin-Puyalto, J., Mäestu, J., Gomez-Cabello, A. et al. Vigorous physical activity patterns affect bone growth during early puberty in boys. Osteoporos Int 29, 2693–2701 (2018). https://doi.org/10.1007/s00198-018-4731-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-018-4731-2