Abstract
Summary
Ibandronate reduces the risk of vertebral and non-vertebral fractures versus placebo in postmenopausal women with osteoporosis. This analysis, in which fractures were reported as safety events, showed that long-term use of ibandronate was associated with low fracture rates over 5 years of treatment.
Introduction
A previous post-hoc meta-analysis of 2–3 year studies found that ibandronate regimens with annual cumulative exposure (ACE) of ≥10.8 mg reduced the risk of vertebral and nonvertebral fractures (NVFs) versus placebo in postmenopausal women. This post-hoc analysis used individual patient data from the 2-year monthly oral ibandronate in ladies (MOBILE) and dosing intravenous administration (DIVA) studies, including the 3-year long-term extensions (LTEs), to assess fracture risk in patients treated with ibandronate for 5 years.
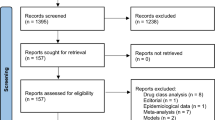
Methods
Patients treated for 2 years in MOBILE with monthly oral ibandronate 150 mg (n = 176) and in DIVA with IV ibandronate every 2 months 2 mg (n = 253) or quarterly 3 mg (n = 263) who continued on the same regimens for 3 additional years in the LTEs were included. Three-year placebo data (n = 1,924) were obtained from the ibandronate osteoporosis vertebral fracture trial in North America and Europe (BONE) and IV Fracture Prevention trials. The primary endpoint was clinical fracture rate; clinical fracture data were collected as adverse events. Time to fracture was analyzed using Kaplan–Meier and statistical analysis was conducted using the log-rank test. All clinical fractures included all NVFs and symptomatic vertebral fractures.
Results
For ibandronate regimens with ACE ≥10.8 mg, time to fracture was significantly longer for all clinical fractures, NVFs, and clinical vertebral fractures versus placebo (P = 0.005). For all fracture types, the rate of fracture appeared stable during the 5-year treatment period.
Conclusion
In women with postmenopausal osteoporosis, continuous treatment with ibandronate over 5 years results in low sustained clinical fracture rate.




Similar content being viewed by others
References
McClung MR (2000) Bisphosphonates in osteoporosis: recent clinical experience. Expert Opin Pharmacother 1:225–238
Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR (2009) Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA 301:513–521
Ioannidis G, Papaioannou A, Hopman WM, Akhtar-Danesh N, Anastassiades T, Pickard L, Kennedy CC, Prior JC, Olszynski WP, Davison KS, Goltzman D, Thabane L, Gafni A, Papadimitropoulos EA, Brown JP, Josse RG, Hanley DA, Adachi JD (2009) Relation between fractures and mortality: results from the Canadian Multicentre Osteoporosis Study. Cmaj 181:265–271
Sweet MG, Sweet JM, Jeremiah MP, Galazka SS (2009) Diagnosis and treatment of osteoporosis. Am Fam Physician 79:193–200
US Food and Drug Administration (1994) Guidelines for preclinical and clinical evaluation of agents used in the prevention or treatment of postmenopausal osteoporosis, Silver Spring
Boonen S, Orwoll ES, Wenderoth D, Stoner KJ, Eusebio R, Delmas PD (2009) Once-weekly risedronate in men with osteoporosis: results of a 2-year, placebo-controlled, double-blind, multicenter study. J Bone Miner Res 24:719–725
Delmas PD, McClung MR, Zanchetta JR, Racewicz A, Roux C, Benhamou CL, Man Z, Eusebio RA, Beary JF, Burgio DE, Matzkin E, Boonen S (2008) Efficacy and safety of risedronate 150 mg once a month in the treatment of postmenopausal osteoporosis. Bone 42:36–42
Schnitzer T, Bone HG, Crepaldi G, Adami S, McClung M, Kiel D, Felsenberg D, Recker RR, Tonino RP, Roux C, Pinchera A, Foldes AJ, Greenspan SL, Levine MA, Emkey R, Santora AC 2nd, Kaur A, Thompson DE, Yates J, Orloff JJ (2000) Therapeutic equivalence of alendronate 70 mg once-weekly and alendronate 10 mg daily in the treatment of osteoporosis. Alendronate Once-Weekly Study Group. Aging (Milano) 12:1–12
Eisman JA, Garcia-Hernandez PA, Ortiz-Luna G, Ste-Marie LG, Hughes C, Mairon N, Masanauskaite D, Delmas PD (2006) Intermittent intravenous ibandronate injections are an effective treatment option in postmenopausal osteoporosis: 2-year results from DIVA [abstract P316SA]. Osteoporos Int 17:S212
Bonnick SL, Shulman L (2006) Monitoring osteoporosis therapy: bone mineral density, bone turnover markers, or both? Am J Med 119:S25–S31
Hochberg MC, Greenspan S, Wasnich RD, Miller P, Thompson DE, Ross PD (2002) Changes in bone density and turnover explain the reductions in incidence of nonvertebral fractures that occur during treatment with antiresorptive agents. J Clin Endocrinol Metab 87:1586–1592
Miller PD (2005) Bone density and markers of bone turnover in predicting fracture risk and how changes in these measures predict fracture risk reduction. Curr Osteoporos Rep 3:103–110
Miller PD (2007) Monitoring osteoporosis therapies. Curr Osteoporos Rep 5:38–43
Miller PD, Zapalowski C, Kulak CA, Bilezikian JP (1999) Bone densitometry: the best way to detect osteoporosis and to monitor therapy. J Clin Endocrinol Metab 84:1867–1871
Wasnich RD, Miller PD (2000) Antifracture efficacy of antiresorptive agents are related to changes in bone density. J Clin Endocrinol Metab 85:231–236
Miller PD (2012) Bone strength and surrogate markers: the first, second, and third fiddle. J Bone Miner Res 27:1623–1626
Chesnut CH, Ettinger MP, Miller PD, Baylink DJ, Emkey R, Harris ST, Wasnich RD, Watts NB, Schimmer RC, Recker RR (2005) Ibandronate produces significant, similar antifracture efficacy in North American and European women: new clinical findings from BONE. Curr Med Res Opin 21:391–401
Chesnut CH, Skag A, Christiansen C, Recker R, Stakkestad JA, Hoiseth A, Felsenberg D, Huss H, Gilbride J, Schimmer RC, Delmas PD (2004) Effects of oral ibandronate administered daily or intermittently on fracture risk in postmenopausal osteoporosis. J Bone Miner Res 19:1241–1249
Reginster JY, Adami S, Lakatos P, Greenwald M, Stepan JJ, Silverman SL, Christiansen C, Rowell L, Mairon N, Bonvoisin B, Drezner MK, Emkey R, Felsenberg D, Cooper C, Delmas PD, Miller PD (2006) Efficacy and tolerability of once-monthly oral ibandronate in postmenopausal osteoporosis: 2 year results from the MOBILE study. Ann Rheum Dis 65:654–661
Eisman JA, Civitelli R, Adami S, Czerwinski E, Recknor C, Prince R, Reginster JY, Zaidi M, Felsenberg D, Hughes C, Mairon N, Masanauskaite D, Reid DM, Delmas PD, Recker RR (2008) Efficacy and tolerability of intravenous ibandronate injections in postmenopausal osteoporosis: 2-year results from the DIVA study. J Rheumatol 35:488–497
Harris ST, Blumentals WA, Miller PD (2008) Ibandronate and the risk of non-vertebral and clinical fractures in women with postmenopausal osteoporosis: results of a meta-analysis of phase III studies. Curr Med Res Opin 24:237–245
Miller PD, McClung MR, Macovei L, Stakkestad JA, Luckey M, Bonvoisin B, Reginster JY, Recker RR, Hughes C, Lewiecki EM, Felsenberg D, Delmas PD, Kendler DL, Bolognese MA, Mairon N, Cooper C (2005) Monthly oral ibandronate therapy in postmenopausal osteoporosis: 1-year results from the MOBILE study. J Bone Miner Res 20:1315–1322
Delmas PD, Adami S, Strugala C, Stakkestad JA, Reginster JY, Felsenberg D, Christiansen C, Civitelli R, Drezner MK, Recker RR, Bolognese M, Hughes C, Masanauskaite D, Ward P, Sambrook P, Reid DM (2006) Intravenous ibandronate injections in postmenopausal women with osteoporosis: one-year results from the dosing intravenous administration study. Arthritis Rheum 54:1838–1846
Cranney A, Wells G, Adachi R (2007) Non-vertebral fracture reduction with high- versus low-dose ibandronate: a meta-analysis of individual patient data. Ann Rheum Dis 66:681
Harris ST, Reginster JY, Harley C, Blumentals WA, Poston SA, Barr CE, Silverman SL (2009) Risk of fracture in women treated with monthly oral ibandronate or weekly bisphosphonates: the eValuation of IBandronate Efficacy (VIBE) database fracture study. Bone 44:758–765
Silverman SL (2010) Osteoporosis therapies: evidence from health-care databases and observational population studies. Calcif Tissue Int 87:375–384
Miller PD, Recker RR, Felsenberg D, Reginster JY, Riis BJ, Czerwinski E, Lorenc RS, Stakkestad JA, Dasic G, Barr CE, Lakatos P (2009) 5-year efficacy and safety of monthly oral ibandronate: results of the MOBILE long-term extension study. Osteoporos Int 20:S191–S229
Stakkestad JA, Lakatos P, Lorenc R, Sedarati F, Neate C, Reginster JY (2008) Monthly oral ibandronate is effective and well tolerated after 3 years: the MOBILE long-term extension. Clin Rheumatol 27:955–960
Recker R, Stakkestad JA, Chesnut CH 3rd, Christiansen C, Skag A, Hoiseth A, Ettinger M, Mahoney P, Schimmer RC, Delmas PD (2004) Insufficiently dosed intravenous ibandronate injections are associated with suboptimal antifracture efficacy in postmenopausal osteoporosis. Bone 34:890–899
Cranney A, Tugwell P, Adachi J, Weaver B, Zytaruk N, Papaioannou A, Robinson V, Shea B, Wells G, Guyatt G (2002) Meta-analyses of therapies for postmenopausal osteoporosis. III. Meta-analysis of risedronate for the treatment of postmenopausal osteoporosis. Endocr Rev 23:517–523
Cranney A, Wells GA, Yetisir E, Adami S, Cooper C, Delmas PD, Miller PD, Papapoulos S, Reginster JY, Sambrook PN, Silverman S, Siris E, Adachi JD (2009) Ibandronate for the prevention of nonvertebral fractures: a pooled analysis of individual patient data. Osteoporos Int 20:291–297
National Osteoporosis Foundation (2008) Clinician's guide to prevention and treatment of osteoporosis. Washington, 1–37
Bone HG, Hosking D, Devogelaer JP, Tucci JR, Emkey RD, Tonino RP, Rodriguez-Portales JA, Downs RW, Gupta J, Santora AC, Liberman UA (2004) Ten years' experience with alendronate for osteoporosis in postmenopausal women. N Engl J Med 350:1189–1199
Devogelaer JP, Brown JP, Burckhardt P, Meunier PJ, Goemaere S, Lippuner K, Body JJ, Samsioe G, Felsenberg D, Fashola T, Sanna L, Ortmann CE, Trechsel U, Krasnow J, Eriksen EF, Garnero P (2007) Zoledronic acid efficacy and safety over five years in postmenopausal osteoporosis. Osteoporos Int 18:1211–1218
Boonen S, Ferrari S, Miller PD, Eriksen EF, Sambrook PN, Compston J, Reid IR, Vanderschueren D, Cosman F (2012) Postmenopausal osteoporosis treatment with antiresorptives: effects of discontinuation or long-term continuation on bone turnover and fracture risk–a perspective. J Bone Miner Res 27:963–974
Khosla S, Bilezikian JP, Dempster DW, Lewiecki EM, Miller PD, Neer RM, Recker RR, Shane E, Shoback D, Potts JT (2012) Benefits and risks of bisphosphonate therapy for osteoporosis. J Clin Endocrinol Metab 97:2272–2282
McClung M, Harris ST, Miller PD, Bauer DC, Davison KS, Dian L, Hanley DA, Kendler DL, Yuen CK, Lewiecki EM (2013) Bisphosphonate therapy for osteoporosis: benefits, risks, and drug holiday. Am J Med 126:13–20
Whitaker M, Guo J, Kehoe T, Benson G (2012) Bisphosphonates for osteoporosis–where do we go from here? N Engl J Med 366:2048–2051
Reginster J, Minne HW, Sorensen OH, Hooper M, Roux C, Brandi ML, Lund B, Ethgen D, Pack S, Roumagnac I, Eastell R (2000) Randomized trial of the effects of risedronate on vertebral fractures in women with established postmenopausal osteoporosis. Vertebral Efficacy with Risedronate Therapy (VERT) Study Group. Osteoporos Int 11:83–91
Black DM, Delmas PD, Eastell R, Reid IR, Boonen S, Cauley JA, Cosman F, Lakatos P, Leung PC, Man Z, Mautalen C, Mesenbrink P, Hu H, Caminis J, Tong K, Rosario-Jansen T, Krasnow J, Hue TF, Sellmeyer D, Eriksen EF, Cummings SR (2007) Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med 356:1809–1822
Cummings SR, Black DM, Thompson DE, Applegate WB, Barrett-Connor E, Musliner TA, Palermo L, Prineas R, Rubin SM, Scott JC, Vogt T, Wallace R, Yates AJ, LaCroix AZ (1998) Effect of alendronate on risk of fracture in women with low bone density but without vertebral fractures: results from the Fracture Intervention Trial. JAMA 280:2077–2082
McClung MR, Geusens P, Miller PD, Zippel H, Bensen WG, Roux C, Adami S, Fogelman I, Diamond T, Eastell R, Meunier PJ, Reginster JY (2001) Effect of risedronate on the risk of hip fracture in elderly women. Hip Intervention Program Study Group. N Engl J Med 344:333–340
Black DM, Reid IR, Boonen S, Bucci-Rechtweg C, Cauley JA, Cosman F, Cummings SR, Hue TF, Lippuner K, Lakatos P, Leung PC, Man Z, Martinez RL, Tan M, Ruzycky ME, Su G, Eastell R (2012) The effect of 3 versus 6 years of zoledronic acid treatment of osteoporosis: a randomized extension to the HORIZON-Pivotal Fracture Trial (PFT). J Bone Miner Res 27:243–254
Sorensen OH, Crawford GM, Mulder H, Hosking DJ, Gennari C, Mellstrom D, Pack S, Wenderoth D, Cooper C, Reginster JY (2003) Long-term efficacy of risedronate: a 5-year placebo-controlled clinical experience. Bone 32:120–126
Black DM, Schwartz AV, Ensrud KE, Cauley JA, Levis S, Quandt SA, Satterfield S, Wallace RB, Bauer DC, Palermo L, Wehren LE, Lombardi A, Santora AC, Cummings SR (2006) Effects of continuing or stop** alendronate after 5 years of treatment: the Fracture Intervention Trial Long-term Extension (FLEX): a randomized trial. JAMA 296:2927–2938
Schwartz AV, Bauer DC, Cummings SR, Cauley JA, Ensrud KE, Palermo L, Wallace RB, Hochberg MC, Feldstein AC, Lombardi A, Black DM (2010) Efficacy of continued alendronate for fractures in women with and without prevalent vertebral fracture: the FLEX trial. J Bone Miner Res 25:976–982
Kwek EB, Koh JS, Howe TS (2008) More on atypical fractures of the femoral diaphysis. N Engl J Med 359:316–317, author reply 317–318
Lee P, Seibel MJ (2008) More on atypical fractures of the femoral diaphysis. N Engl J Med 359:317, author reply 317–318
Lenart BA, Lorich DG, Lane JM (2008) Atypical fractures of the femoral diaphysis in postmenopausal women taking alendronate. N Engl J Med 358:1304–1306
Odvina CV, Zerwekh JE, Rao DS, Maalouf N, Gottschalk FA, Pak CY (2005) Severely suppressed bone turnover: a potential complication of alendronate therapy. J Clin Endocrinol Metab 90:1294–1301
Visekruna M, Wilson D, McKiernan FE (2008) Severely suppressed bone turnover and atypical skeletal fragility. J Clin Endocrinol Metab 93:2948–2952
Dell RM, Adams AL, Greene DF, Funahashi TT, Silverman SL, Eisemon EO, Zhou H, Burchette RJ, Ott SM (2012) Incidence of atypical nontraumatic diaphyseal fractures of the femur. J Bone Miner Res 27:2544–2550
Schilcher J, Koeppen V, Ranstam J, Skripitz R, Michaelsson K, Aspenberg P (2013) Atypical femoral fractures are a separate entity, characterized by highly specific radiographic features. A comparison of 59 cases and 218 controls. Bone 52:389–392
Shane E, Burr D, Ebeling PR, Abrahamsen B, Adler RA, Brown TD, Cheung AM, Cosman F, Curtis JR, Dell R, Dempster D, Einhorn TA, Genant HK, Geusens P, Klaushofer K, Koval K, Lane JM, McKiernan F, McKinney R, Ng A, Nieves J, O'Keefe R, Papapoulos S, Sen HT, van der Meulen MC, Weinstein RS, Whyte M (2010) Atypical subtrochanteric and diaphyseal femoral fractures: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 25:2267–2294
Berlin JA, Santanna J, Schmid CH, Szczech LA, Feldman HI (2002) Individual patient- versus group-level data meta-regressions for the investigation of treatment effect modifiers: ecological bias rears its ugly head. Stat Med 21:371–387
Li Z, Meredith MP (2003) Exploring the relationship between surrogates and clinical outcomes: analysis of individual patient data vs. meta-regression on group-level summary statistics. J Biopharm Stat 13:777–792
Acknowledgments
This study was funded by Genentech and GlaxoSmithKline. Medical writing assistance was provided by Gill Sperrin CBiol MSB CMPP and Andrew Cooper PhD CMPP of Envision Scientific Solutions and funded by Genentech and GlaxoSmithKline. The authors received no financial support for this work and had complete control of the data.
Conflicts of interest
Dr Miller’s institution has received payment for consultancy from Amgen, Merck & Lilly, expert testimony from Novartis, and grants from Amgen, Merck & Lilly. Dr. Robert R. Recker is a paid consultant for Merck, Lilly, Wyeth, Procter and Gamble, Amgen, Roche, GlaxoSmithKline, Novartis, and NPS Allelix and has received grant/research support from Merck, Lilly, Wyeth, Procter and Gamble, Amgen, Roche, GlaxoSmithKline, Novartis, NPS Allelix, and Sanofi‐Aventis through grants to his institution. Dr. Jean‐Yves Reginster is a paid consultant for/has received payment for advisory boards from Servier, Novartis, Negma, Lilly, Wyeth, Amgen, GlaxoSmithKline, Roche, Merckle, Nycomed, NPS, Theramex, and UCB. He has received lecture fees when speaking at the invitation of a commercial sponsor for Merck Sharp and Dohme, Lilly, Rottapharm, IBSA, Genevrier, Novartis, Servier, Roche, GlaxoSmithKline, Tei**, Teva, Ebewee Pharma, Zodiac, Analis, Theramex, Nycomed, and Novo‐Nordisk. He has also received grant support from Bristol Myers Squibb, Merck Sharp & Dohme, Rottapharm, Teva, Lilly, Novartis, Roche, GlaxoSmithKline, Amgen, and Servier. Dr Harris has served as a Board member for Eli Lilly & Company, Merck; received consultancy fees from Amgen, Eli Lilly & Company, Merck, and Roche; has served as an expert advisor for Roche; and has received honoraria for Speakers Bureax from Amgen, Eli Lilly & Company, Genentech, GlaxoSmithKline, Procter & Gamble, Roche, Novartis, Warner Chilcott. De Silverman has received consultancy fees from The Alliance for Better Bone Health (Procter & Gamble Pharmaceuticals and Sanofi Aventis). Dr Felsenberg has received consulting fees or paid advisory board fees from Amgen, Chugai, GlaxoSmithKline, Lilly, MSD, Novartis, Nycomed, Roche, Servier, and TEVA; lecture fees from Amgen, Chugai, GE, GlaxoSmithKline, Lilly, MSD, Novartis, Nycomed, Roche, Servier, Teva, and WC; and grant support from Amgen, Chugai, Lilly, MSD, Novartis, Nycomed, Roche, Teva, Servier. Drs Bann‐Mo Day and Charles Barr are full‐time employees of Genentech. Dr. Daiva Masanauskaite is a full‐time employee of F. Hoffmann-La Roche.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miller, P.D., Recker, R.R., Harris, S. et al. Long-term fracture rates seen with continued ibandronate treatment: pooled analysis of DIVA and MOBILE long-term extension studies. Osteoporos Int 25, 349–357 (2014). https://doi.org/10.1007/s00198-013-2518-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-013-2518-z