Abstract
Introduction and hypothesis
We aimed to compare anal and urinary incontinence symptoms and anal manometry between women with undiagnosed obstetric anal sphincter injuries (OASIS) and women who had OASIS diagnosed and repaired.
Methods
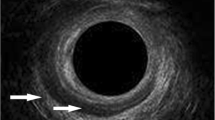
This was a matched retrospective cohort study. Each missed OASI was matched with a diagnosed OASI for severity [minor (3a/b) or major (3c)], parity and length of follow-up. Women completed the modified St Mark’s Incontinence Score and International Consultation on Incontinence Questionnaire. Women with OASIS or those without OASIS but with anal incontinence symptoms were seen in perineal clinic for perineal examinations, anorectal manometry and three-dimensional endoanal ultrasound 8–12 weeks postnatally or in a subsequent pregnancy.
Results
Forty missed OASIS were matched with 40 recognised OASIS (16 3a/b; 24 3c). The median modified St Mark’s scores were higher for missed tears [11 (4, 15) vs. 1 (0, 4), p < 0.001] as well as the urinary incontinence scores [4 (0, 6) vs. 0 (0, 2), p = 0.01] than for the control group. Missed OASIS patients had a shorter perineal body [1.6 ± 1.3 vs. 2.4 ± 0.8, p = 0.009]. All missed OASIS had larger defects on endoanal ultrasound. One in four missed OASIS required further surgery [aOR 4.1 (95% CI 1.0–16.3), p = 0.04] and almost all needed colorectal input [aOR 24.1 (95% CI 7.3–80.0), p < 0.0001]. There were no differences in anal manometry.
Conclusions
Women with symptomatic missed OASIS are compromised in terms of anal and urinary incontinence symptoms, sphincter defect size and perineal body size requiring additional colorectal input. This highlights the importance of preventing OASIS and perseverance with training to diagnose OASIS.

Similar content being viewed by others
References
Harvey MA, Pierce M. Obstetric anal sphincter injuries (OASIS): prevention, recognition and repair. J Obstet Gynaecol Can. 2015;37(12):1131–48.
Thiagamoorthy G, Johnson A, Thakar R, Sultan AH. National survey of perineal trauma and its subsequent management in the United Kingdom. Int Urogynecol J. 2014;25:1621–7.
Gurol-Urganci I, Cromwell DA, Edozien LC, Mahmood TA, Adams EJ, Richmond DH, et al. Third- and fourth-degree perineal tears among primiparous women in England between 2000 and 2012: time trends and risk factors. BJOG. 2013;120(12):1516–25.
Andrews V, Thakar R, Sultan AH. Structured hands-on training in repair of obstetric anal sphincter injuries (OASIS): an audit of clinical practice. Int Urogynecol J. 2009;20:1397.
Sultan AH, Thakar R. Third and fourth degree tears. In: Sultan AH, Thakar R, Fenner D, editors. Perineal and anal sphincter trauma. London: Springer; 2007. p. 33–51.
Sultan AH, Kamm MA, Hudson CN, Thomas JM, Bartram CI. Anal-sphincter disruption during vaginal delivery. N Engl J Med. 1993;329(26):1905–11.
Andrews V, Sultan AH, Thakar R, Jones PW. Occult anal sphincter injuries: myth or reality? BJOG. 2006;113:195–200.
Reid AR, Beggs AD, Sultan AH, Roos A-M, Thakar R. Outcome of repair of obstetric anal sphincter injuries (OASIS) at three years. Int J Gynecol Obstet. 2014;127:47–50.
Ness W. Faecal incontinence: what influences care and management options? Br J Nurs. 2008;17(18):1148–52.
Jordan PA, Naidu M, Thakar R, Sultan AH. Effect of subsequent vaginal delivery on bowel symptoms and anorectal function in women who sustained a previous obstetric anal sphincter injury. Int Urogynecol J. 2018;29(11):1579–88.
The management of third- and fourth- degree perineal tears. Green-top Guideline No. 29 Royal College of Obstetricians & Gynaecologists (2015) https://www.rcog.org.uk/globalassets/documents/guidelines/gtg-29.pdf Accessed 25th February 2018.
Roos AM, Sultan AH, Thakar R. St. Mark's incontinence score for assessment of anal incontinence following obstetric anal sphincter injuries (OASIS). Int Urogynecol J. 2009;20(4):407–10.
Avery K, Donovan J, Peters TJ, Shaw C, Gotoh M, Abrams P. ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn. 2004;23(4):322–30.
Roos AM, Thakar R, Sultan AH. Outcome of primary repair of obstetric anal sphincter injuries (OASIS): does the grade of tear matter? Ultrasound Obstet Gynecol. 2010;36(3):368–74.
Starck M, Bohe M, Valentin L. Results of endosonographic imaging of the anal sphincter 2–7 days after primary repair of third- or fourth-degree obstetric sphincter tears. Ultrasound Obstet Gynecol. 2003;22:609–15.
Groom KM, Palerson-Brown S. Can we improve on the diagnosis of third-degree tears? Eur J Obstet Gynecol Reprod Biol. 2002;101:19–21.
Andrews V, Sultan AH, Thakar R, Jones PW. Risk factors for obstetric anal sphincter injury: a prospective study. Birth. 2006;33(2):117–22.
Ozyurt S, Aksoy H, Gedikbasi A, Yildririm G, Aksoy U, Acmaz G, et al. Screening occult anal sphincter injuries in primigravid women after vaginal delivery with transperineal use of vaginal probe: a prospective, randomized controlled trial. Arch Gynecol Obstet. 2015;292:853–9.
Jango H, Langhoff-Roos J, Rosthoj S, Sakse A. Modifiable risk factors of obstetric anal sphincter injury in primiparous women: a population-based cohort study. Am J Obstet Gynecol. 2014;210(1):59e1–59 e6.
Ramage L, Yen C, Qiu S, Simillis C, Kontovounisios C, Tan E, et al. Does a missed obstetric anal sphincter injury at time of delivery affect short-term functional outcome? Ann R Coll Surg Engl. 2018;100:26–32.
van Roon Y, Vinayakarao L, Melson L, Percival R, Pathak S, Pradhan A. Comparative study of episiotomy angles achieved by cutting with straight Mayo scissors and the EPISCISSORS-60 in a birth simulation model. Int Urogynecol J. 2017;28(7):1063–6.
Siddiqui NY, Ammarell N, Wu JM, Sandaval JS, Bosworth HB. Urinary incontinence and health-seeking behaviour among white, black and Latina women. Female Pelvic Med Reconstr Surg. 2016;22(5):340–5.
Oberwald M, Connor J, Wener SD. Meta-analysis to determine the incidence of obstetric anal sphincter damage. Br J Surg. 2003;90:1333–7.
Fornell EU, Mathiesen L, Sjodahl R, Berg G. Obstetric anal sphincter injury ten years after: subjective and objective long-term effects. BJOG. 2005;112:312–6.
Kapoor DS, Thakar R, Sultan AH. Obstetric anal sphincter injuries: review of anatomical factors and modifiable second stage interventions. Int Urogynecol J. 2015;26(12):1725–34.
Mathe M, Valancogne G, Atallah A, Sciard C, Doret M, Gaucherand P, et al. Early pelvic floor muscle training after obstetrical anal sphincter injuries for the reduction of anal incontinence. Eur J Obstet Gynecol Reprod Biol. 2016;199:201–6.
Scheer I, Andrews V, Thakar R, Sultan AH. Urinary incontinence after obstetric anal sphincter injuries (OASIS) – is there a relationship? Int Urogynecol J. 2008;19(2):179–83.
Volloyhaug I, Taithongchai A, van Gruting I, Sultan AH, Thakar R. Levator ani morphology and function in women who have sustained obstetric anal sphincter injuries. Ultrasound Obstet Gynecol. 2018. https://doi.org/10.1002/uog.20115.
Jha S, Sultan AH. Obstetric anal sphincter injury: the changing landscape. BJOG. 2015;122(7):931.
Taithongchai A, van Gruting IMA, Volloyhaug I, Arendsen LP, Sultan AH, Thakar R. Comparing the diagnostic accuracy of three ultrasound modalities for diagnosing obstetric anal sphincter injuries. Am J Obstet Gynecol. 2019. https://doi.org/10.1016/j.ajog.2019.04.009.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Ranee Thakar is currently the President of the International Urogynecology Association. The other authors have no financial disclaimers or conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Conference Presentations
Annual Meeting of the British Society of Urogynaecology, Royal College of Obstetricians and Gynaecologists, London 9 November 2018
Rights and permissions
About this article
Cite this article
Taithongchai, A., Veiga, S.I., Sultan, A.H. et al. The consequences of undiagnosed obstetric anal sphincter injuries (OASIS) following vaginal delivery. Int Urogynecol J 31, 635–641 (2020). https://doi.org/10.1007/s00192-019-04033-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-019-04033-5