Abstract
Introduction and hypothesis
The objective was to evaluate the diagnostic potential of digital rectal examination in the identification of a true rectocele.
Methods
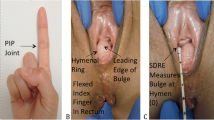
This is a retrospective observational study utilising 187 archived data sets of women presenting with lower urinary tract symptoms and/or pelvic organ prolapse between August 2012 and November 2013. Evaluation included a standardised interview, ICS-POPQ, rectal examination and 4D translabial ultrasound. The main outcome measure was the diagnosis of rectocele by digital rectal palpation on Valsalva manoeuvre. This diagnosis correlated with the sonographic diagnosis of rectocele to determine agreement between digital examination and ultrasound findings.
Results
Complete data sets were available for 180 participants. On imaging, the mean position of the rectal ampulla was 11.07 (−36.3 to 44.3) mm below the symphysis pubis; 42.8% (77) had a rectocele of a depth of ≥10 mm. On palpation, a rectocele was detected in 60 women (33%). Agreement between palpation and imaging was observed in 77%; the kappa was 0.52 (CI 0.39–0.65). On receiver operator characteristic analysis, the area under the curve was 0.854 for the relationship between rectocele pocket depth and the detection of rectocele on palpation.
Conclusion
Moderate agreement was found between digital rectal examination for rectocele and translabial ultrasound findings of a “true rectocele”. Digital rectal examination may be used to identify these defects in clinical practice. Extending the clinical examination of prolapse to include rectal examination to palpate defects in the rectovaginal septum may reduce the need for defecatory proctograms for the assessment of obstructive defecation and may help triage patients in the management of posterior compartment prolapse.


Similar content being viewed by others
References
Dietz HP, Steensma AB. Posterior compartment prolapse on two-dimensional and three-dimensional pelvic floor ultrasound: the distinction between true rectocele, perineal hypermobility and enterocele. Ultrasound Obstet Gynecol. 2005;26(1):73–7.
Dietz HP, Korda A. Which bowel symptoms are most strongly associated with a true rectocele? Aust N Z J Obstet Gynaecol. 2005;45(6):505–8.
Dietz HP, Clarke B. Prevalence of rectocele in young nulliparous women. Aust N Z J Obstet Gynaecol. 2005;45(5):391–4.
Guzman Rojas R, Quintero C, Shek KL, Dietz HP. Does childbirth play a role in the etiology of rectocele? Int Urogynecol J. 2015;26(5):737–41.
Guzman Rojas R, Kamisan Atan I, Shek KL, Dietz HP. The prevalence of abnormal posterior compartment anatomy in urogynecological patients. Int Urogynecol J. 2016;27(6):939–44.
Guzman Rojas R, Kamisan Atan I, Shek KL, Dietz HP. Defect-specific rectocele repair: medium-term anatomical, functional and subjective outcomes. Aust N Z J Obstet Gynaecol. 2015;55(5):487–92.
Perniola G, Shek C, Chong CC, Chew S, Cartmill J, Dietz HP. Defecation proctography and translabial ultrasound in the investigation of defecatory disorders. Ultrasound Obstet Gynecol. 2008;31(5):567–71.
Dietz HP. Pelvic floor ultrasound: a review. Am J Obstet Gynecol. 2010;202(4):321–34.
Steensma AB, Oom DM, Burger CW, Schouten WR. Assessment of posterior compartment prolapse: a comparison of evacuation proctography and 3D transperineal ultrasound. Colorectal Dis. 2010;12(6):533–9.
Pannu HK, Kaufman HS, Cundiff GW, Genadry R, Bluemke DA, Fishman EK. Dynamic MR imaging of pelvic organ prolapse: spectrum of abnormalities. Radiographics. 2000;20(6):1567–82.
Beer-Gabel M, Carter D. Comparison of dynamic transperineal ultrasound and defecography for the evaluation of pelvic floor disorders. Int J Colorectal Dis. 2015;30(6):835–41.
Dietz HP. Translabial ultrasound in the assessment of pelvic floor and anorectal function in women with defecatory disorders. Tech Coloproctol. 2014;18(5):481–94.
Martellucci J, Naldini G. Clinical relevance of transperineal ultrasound compared with evacuation proctography for the evaluation of patients with obstructed defaecation. Colorectal Dis. 2011;13(10):1167–72.
Alam P, Guzman Rojas R, Kamisan Atan I, Mann K, Dietz HP. The ‘bother’ of obstructed defecation. Ultrasound Obstet Gynecol. 2015; doi: 10.1002/uog.15828.
Dietz HP, Rojas RG, Shek KL. Postprocessing of pelvic floor ultrasound data: how repeatable is it? Aust N Z J Obstet Gynaecol. 2014;54(6):553–7.
Tan L, Shek KL, Atan IK, Rojas RG, Dietz HP. The repeatability of sonographic measures of functional pelvic floor anatomy. Int Urogynecol J. 2015;26(11):1667–72.
Martellucci J, Naldini G. Assessment of posterior compartment prolapse; a comparison of evacuation proctography and 3D transperineal ultrasound. Colorectal Dis. 2010;12(8):834.
Richardson AC. The rectovaginal septum revisited: its relationship to rectocele and its importance in rectocele repair. Clin Obstet Gynecol. 1993;36(4):976–83.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Source of funding
IUGA observership grant award, 2013, to S. Rachaneni.
Conflicts of interest
The authors declare that they have no conflicts of interest with regard to this manuscript.
Disclosures
HP Dietz and KL Shek have received unrestricted educational grants from GE.
Ethics approval
Not required as it is a retrospective study.
Rights and permissions
About this article
Cite this article
Rachaneni, S., Atan, I.K., Shek, K.L. et al. Digital rectal examination in the evaluation of rectovaginal septal defects. Int Urogynecol J 28, 1401–1405 (2017). https://doi.org/10.1007/s00192-017-3285-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-017-3285-8