Abstract
Purpose
Transcardiopulmonary thermodilution (TPTD, SVTD) as well as calibrated (SVPC CAL) and uncalibrated (SVPC UNCAL) arterial pulse contour analysis (PC) are increasingly promoted as less-invasive technologies to measure stroke volume (SV) but their reliability in aortic valve disease was unknown. The objective of this prospective study was to investigate the validity of three less-invasive techniques to assess SV in conditions involving aortic stenosis (AS) and valvuloplasty-induced aortic insufficiency (AI) compared with transesophageal echocardiography.
Methods
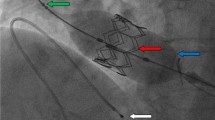
In 18 patients undergoing transcatheter aortic valve implantation, SVTD and SVPC CAL were determined using a central pressure signal via the brachial artery and SVPC UNCAL using a peripheral radial signal.
Results
In aortic valve dysfunction TPTD achieved adequate reproducibility (concordance correlation coefficient (CCC): AS 0.84; AI 0.82) and agreement (percentage error (PE): AS 26.3 %; AI 26.2 %) with the reference technique. In severe AS, SVPC CAL (PE 25.7 %; CCC 0.85) but not SVPC UNCAL (PE 50.4 %; CCC 0.38) was reliable. Neither calibrated nor uncalibrated PC (SVPC CAL: PE 51.5 %; CCC 0.49; SVPC UNCAL: PE 61.9 %; CCC 0.22) was valid in AI. Trending ability to hemodynamic changes, quantified by the ΔSV vector and the angle θ, was acceptable for each measurement modality.
Conclusions
Transcardiopulmonary thermodilution is valid in aortic valve dysfunction. Calibration of PC substantially improves reliability in aortic valve disease. Calibrated PC is valid in severe AS. Valvuloplasty-induced AI seriously confounds PC measurements. In uncalibrated PC approaches, the relative SV trend is superior to single absolute values.




Similar content being viewed by others
References
Gan TJ, Soppitt A, Maroof M, el-Moalem H, Robertson KM, Moretti E, Dwane P, Glass PS (2002) Goal-directed intraoperative fluid administration reduces length of hospital stay after major surgery. Anesthesiology 97:820–826
Goepfert MS, Reuter DA, Akyol D, Lamm P, Kilger E, Goetz AE (2007) Goal-directed fluid management reduces vasopressor and catecholamine use in cardiac surgery patients. Intensive Care Med 33:96–103
Hamilton MA, Cecconi M, Rhodes A (2011) A systematic review and meta-analysis on the use of preemptive hemodynamic intervention to improve postoperative outcomes in moderate and high-risk surgical patients. Anesth Analg 112:1392–1402
Rhodes A, Cecconi M, Hamilton M, Poloniecki J, Woods J, Boyd O, Bennett D, Grounds RM (2010) Goal-directed therapy in high-risk surgical patients: a 15-year follow-up study. Intensive Care Med 36:1327–1332
Harvey S, Young D, Brampton W, Cooper AB, Doig G, Sibbald W, Rowan K (2006) Pulmonary artery catheters for adult patients in intensive care. Cochrane Database Syst Rev 3:CD003408
Alhashemi JA, Cecconi M, Hofer CK (2011) Cardiac output monitoring: an integrative perspective. Crit Care 15:214
Reuter DA, Huang C, Edrich T, Shernan SK, Eltzschig HK (2010) Cardiac output monitoring using indicator-dilution techniques: basics, limits, and perspectives. Anesth Analg 110:799–811
Goedje O, Hoke K, Goetz AE, Felbinger TW, Reuter DA, Reichart B, Friedl R, Hannekum A, Pfeiffer UJ (2002) Reliability of a new algorithm for continuous cardiac output determination by pulse-contour analysis during hemodynamic instability. Crit Care Med 30:52–58
Reuter DA, Goetz AE (2005) Measurement of cardiac output. Anaesthesist 54:1135–1151; quiz 1152–1133
Felbinger TW, Reuter DA, Eltzschig HK, Moerstedt K, Goedje O, Goetz AE (2002) Comparison of pulmonary arterial thermodilution and arterial pulse contour analysis: evaluation of a new algorithm. J Clin Anesth 14:296–301
Goedje O, Hoeke K, Lichtwarck-Aschoff M, Faltchauser A, Lamm P, Reichart B (1999) Continuous cardiac output by femoral arterial thermodilution calibrated pulse contour analysis: comparison with pulmonary arterial thermodilution. Crit Care Med 27:2407–2412
Rauch H, Muller M, Fleischer F, Bauer H, Martin E, Bottiger BW (2002) Pulse contour analysis versus thermodilution in cardiac surgery patients. Acta Anaesthesiol Scand 46:424–429
Rodig G, Prasser C, Keyl C, Liebold A, Hobbhahn J (1999) Continuous cardiac output measurement: pulse contour analysis vs thermodilution technique in cardiac surgical patients. Br J Anaesth 82:525–530
Sander M, von Heymann C, Foer A, von Dossow V, Grosse J, Dushe S, Konertz WF, Spies CD (2005) Pulse contour analysis after normothermic cardiopulmonary bypass in cardiac surgery patients. Crit Care 9:R729–R734
Zollner C, Haller M, Weis M, Morstedt K, Lamm P, Kilger E, Goetz AE (2000) Beat-to-beat measurement of cardiac output by intravascular pulse contour analysis: a prospective criterion standard study in patients after cardiac surgery. J Cardiothorac Vasc Anesth 14:125–129
Breukers RM, Groeneveld AB, de Wilde RB, Jansen JR (2009) Transpulmonary versus continuous thermodilution cardiac output after valvular and coronary artery surgery. Interact Cardiovasc Thorac Surg 9:4–8
Compton FD, Zukunft B, Hoffmann C, Zidek W, Schaefer JH (2008) Performance of a minimally invasive uncalibrated cardiac output monitoring system (Flotrac/Vigileo) in haemodynamically unstable patients. Br J Anaesth 100:451–456
De Backer D, Marx G, Tan A, Junker C, Van Nuffelen M, Huter L, Ching W, Michard F, Vincent JL (2011) Arterial pressure-based cardiac output monitoring: a multicenter validation of the third-generation software in septic patients. Intensive Care Med 37:233–240
Lorsomradee S, Cromheecke S, De Hert SG (2007) Uncalibrated arterial pulse contour analysis versus continuous thermodilution technique: effects of alterations in arterial waveform. J Cardiothorac Vasc Anesth 21:636–643
Meng L, Tran NP, Alexander BS, Laning K, Chen G, Kain ZN, Cannesson M (2011) The impact of phenylephrine, ephedrine, and increased preload on third-generation Vigileo-FloTrac and esophageal Doppler cardiac output measurements. Anesth Analg 113:751–757
Monnet X, Anguel N, Jozwiak M, Richard C, Teboul JL (2012) Third-generation FloTrac/Vigileo does not reliably track changes in cardiac output induced by norepinephrine in critically ill patients. Br J Anaesth 108:615–622
Sander M, Spies CD, Grubitzsch H, Foer A, Muller M, von Heymann C (2006) Comparison of uncalibrated arterial waveform analysis in cardiac surgery patients with thermodilution cardiac output measurements. Crit Care 10:R164
Staier K, Wiesenack C, Gunkel L, Keyl C (2008) Cardiac output determination by thermodilution and arterial pulse waveform analysis in patients undergoing aortic valve replacement. Can J Anaesth 55:22–28
Rosengart TK, Feldman T, Borger MA, Vassiliades TA Jr, Gillinov AM, Hoercher KJ, Vahanian A, Bonow RO, O’Neill W (2008) Percutaneous and minimally invasive valve procedures: a scientific statement from the American Heart Association Council on Cardiovascular Surgery and Anesthesia, Council on Clinical Cardiology, Functional Genomics and Translational Biology Interdisciplinary Working Group, and Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation 117:1750–1767
Vahanian A, Alfieri O, Al-Attar N, Antunes M, Bax J, Cormier B, Cribier A, De JP, Fournial G, Kappetein AP, Kovac J, Ludgate S, Maisano F, Moat N, Mohr F, Nataf P, Pierard L, Pomar JL, Schofer J, Tornos P, Tuzcu M, van HB, Von Segesser LK, Walther T (2008) Transcatheter valve implantation for patients with aortic stenosis: a position statement from the European Association of Cardio-Thoracic Surgery (EACTS) and the European Society of Cardiology (ESC), in collaboration with the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 29:1463–1470
Huter L, Schwarzkopf KR, Preussler NP, Schubert H, Schreiber T (2007) The level of cardiac output affects the relationship and agreement between pulmonary artery and transpulmonary aortic thermodilution measurements in an animal model. J Cardiothorac Vasc Anesth 21:659–663
Critchley LA, Critchley JA (1999) A meta-analysis of studies using bias and precision statistics to compare cardiac output measurement techniques. J Clin Monit Comput 15:85–91
Cecconi M, Rhodes A, Poloniecki J, Della Rocca G, Grounds RM (2009) Bench-to-bedside review: the importance of the precision of the reference technique in method comparison studies–with specific reference to the measurement of cardiac output. Crit Care 13:201
Squara P, Cecconi M, Rhodes A, Singer M, Chiche JD (2009) Tracking changes in cardiac output: methodological considerations for the validation of monitoring devices. Intensive Care Med 35:1801–1808
Cecconi M, Dawson D, Grounds RM, Rhodes A (2009) Lithium dilution cardiac output measurement in the critically ill patient: determination of precision of the technique. Intensive Care Med 35:498–504
Lin LI (1989) A concordance correlation coefficient to evaluate reproducibility. Biometrics 45:255–268
Critchley LA, Lee A, Ho AM (2010) A critical review of the ability of continuous cardiac output monitors to measure trends in cardiac output. Anesth Analg 111:1180–1192
Malbrain ML, De Potter TJ, Dits H, Reuter DA (2010) Global and right ventricular end-diastolic volumes correlate better with preload after correction for ejection fraction. Acta Anaesthesiol Scand 54:622–631
Heerdt PM, Blessios GA, Beach ML, Hogue CW (2001) Flow dependency of error in thermodilution measurement of cardiac output during acute tricuspid regurgitation. J Cardiothorac Vasc Anesth 15:183–187
Hillis LD, Firth BG, Winniford MD (1986) Comparison of thermodilution and indocyanine green dye in low cardiac output or left-sided regurgitation. Am J Cardiol 57:1201–1202
Wouters PF, Quaghebeur B, Sergeant P, Van Hemelrijck J, Vandermeersch E (2005) Cardiac output monitoring using a brachial arterial catheter during off-pump coronary artery bypass grafting. J Cardiothorac Vasc Anesth 19:160–164
Schramm S, Albrecht E, Frascarolo P, Chassot PG, Spahn DR (2010) Validity of an arterial pressure waveform analysis device: does the puncture site play a role in the agreement with intermittent pulmonary artery catheter thermodilution measurements? J Cardiothorac Vasc Anesth 24:250–256
Orme RM, Pigott DW, Mihm FG (2004) Measurement of cardiac output by transpulmonary arterial thermodilution using a long radial artery catheter. A comparison with intermittent pulmonary artery thermodilution. Anaesthesia 59(6):590–594
Parra V, Fita G, Rovira I, Matute P, Gomar C, Pare C (2008) Transoesophageal echocardiography accurately detects cardiac output variation: a prospective comparison with thermodilution in cardiac surgery. Eur J Anaesthesiol 25:135–143
Nowak M, Rosenberger P, Felbinger TW, Goetz AE, Shernan SK, Unertl K, Eltzschig HK (2006) Perioperative echocardiography: basic principles. Anaesthesist 55:337–361
Conflicts of interest
AEG and DAR are members of the Medical Advisory Board of Pulsion Medical Systems. DAR has received honoraria for lectures from Edwards Lifesciences. The study was financed solely by institutional sources.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is discussed in the editorial available at: doi:10.1007/s00134-012-2802-y.
Electronic supplementary material
Below is the link to the electronic supplementary material.
134_2012_2786_MOESM1_ESM.tif
Supplementary material 1 (TIFF 375 kb) Online Resource 1 Regression and correlation analysis, scatter plots, X-axis SV measured with transesophageal echocardiography (SVTEE), Y-axis SV calculated with transcardiopulmonary thermodilution (SVTD, top), calibrated (SVPC CAL, middle), and uncalibrated arterial pulse contour analysis (SVPC UNCAL, bottom) at predefined measurement times from the left to the right with normal prosthetic valve function (post-interventional), with severe aortic stenosis (pre-interventional), and with aortic insufficiency (post-valvuloplasty)
Rights and permissions
About this article
Cite this article
Petzoldt, M., Riedel, C., Braeunig, J. et al. Stroke volume determination using transcardiopulmonary thermodilution and arterial pulse contour analysis in severe aortic valve disease. Intensive Care Med 39, 601–611 (2013). https://doi.org/10.1007/s00134-012-2786-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-012-2786-7