Abstract
Purpose
We hypothesized that non-invasively determined work of breathing per minute (WOBN/min) (esophageal balloon not required) may be useful for predicting extubation outcome, i.e., appropriate work of breathing values may be associated with extubation success, while inappropriately increased values may be associated with failure.
Methods
Adult candidates for extubation were divided into a training set (n = 38) to determine threshold values of indices for assessing extubation and a prospective validation set (n = 59) to determine the predictive power of the threshold values for patients successfully extubated and those who failed extubation. All were evaluated for extubation during a spontaneous breathing trial (5 cmH2O pressure support ventilation, 5 cmH2O positive end expiratory pressure) using routine clinical practice standards. WOBN/min data were blinded to attending physicians. Area under the receiver operating characteristic curves (AUC), sensitivity, specificity, and positive and negative predictive values of all extubation indices were determined.
Results
AUC for WOBN/min was 0.96 and significantly greater (p < 0.05) than AUC for breathing frequency at 0.81, tidal volume at 0.61, breathing frequency-to-tidal volume ratio at 0.73, and other traditionally used indices. WOBN/min had a specificity of 0.83, the highest sensitivity at 0.96, positive predictive value at 0.84, and negative predictive value at 0.96 compared to all indices. For 95% of those successfully extubated, WOBN/min was ≤10 J/min.
Conclusions
WOBN/min had the greatest overall predictive accuracy for extubation compared to traditional indices. WOBN/min warrants consideration for use in a complementary manner with spontaneous breathing pattern data for predicting extubation outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Predicting when patients can be extubated successfully from ventilatory support has, in part, been based on traditionally measured breathing pattern and arterial blood gas data [1, 2]. Tolerance of the breathing load on the inspiratory muscles to spontaneously inhale has been assessed using breathing frequency (f), tidal volume (V T), index of rapid shallow breathing, i.e., f/V T ratio, and minute ventilation (MV) [3]. Loads on inspiratory muscles to spontaneously inhale, secondary to increased elastic (lung and chest wall compliance) and/or resistive loads (physiologic airways resistance and imposed resistance of endotracheal tube and ventilator apparatus), have been inferred by observing and palpating sternocleidomastoid accessory inspiratory muscle contractions [4]. Another approach is observing the contour of the inspiratory pressure waveform, as during flow/volume controlled mechanical ventilation, i.e., the greater the concavity of the pressure waveform, the greater load and vice versa [5]. Although potentially useful, shortcomings of these methods are that they are qualitative, subjective inferences of load. Clinicians would be better served with quantitative, objective, real-time measurements of load when making patient assessments for extubation.
Loads on the inspiratory muscles to spontaneously inhale are reflected by work of breathing, which requires insertion of an esophageal balloon catheter to measure changes in esophageal pressure, an estimate of changes in intrapleural pressure during spontaneous breathing [6]. Recent advances in the application of artificial neural network (ANN) technology to critical care medicine [7–9] allow work of breathing per minute or power of breathing to be determined noninvasively (WOBN/min), accurately, and in real time, obviating the need to insert an esophageal balloon catheter [10]. This approach greatly simplifies measurement of inspiratory muscle loads, allowing practical, clinical use of work of breathing data at the bedside.
Work of breathing has been suggested as a parameter for assessing and withdrawing ventilatory support, possibly for extubation as well. It has been shown that there is a level of work of breathing per minute at a range 1.34–1.8 kg m/min (equivalent to ≥13 J/min) above which patients cannot sustain spontaneous ventilation and be successfully extubated [11–13]. We hypothesized that inappropriately increased values of WOBN/min during a spontaneous breathing trial at minimal levels of pressure support ventilation (PSV) and positive end expiratory pressure (PEEP) may be associated with respiratory distress and be useful for predicting extubation failure. Conversely, appropriate values of WOBN/min under the same conditions may predict extubation success. The purpose of this study was to determine the potential usefulness of WOBN/min as a predictor of extubation in adults. We compared WOBN/min to traditional indices used for assessing the readiness of extubation.
Methods
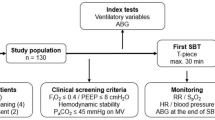
In this IRB-approved study, a waiver of informed consent was granted to record breathing pattern and related data in 97 adults (Table 1) in a surgical ICU at a university medical center who were considered candidates for extubation based on routinely used inclusion and exclusion criteria (Table 2). Patients had received ventilatory support for 9 ± 3 days (Model 840 ventilator, Puritan Bennett, Pleasanton, CA). The first 38 or approximately 40% of patients were designated as a training set to determine threshold values for indices that best differentiated patients who were successfully extubated (n = 31) or who failed extubation (n = 7), a 22% failure rate. The predictive power of the threshold values for each index was assessed in the subsequent 59 or 60% of patients in a prospective validation set who were successfully extubated (n = 47) or who failed extubation (n = 12), a 25% failure rate. The reported incidence of extubation failure ranges between 6 and 47% [14]. Failure rates for our two patient sets are comparable and near the middle of this range.
As routinely used, a spontaneous breathing trial (SBT) of PSV 5 cmH20 with PEEP 5 cmH2O (FIO2 ≤ 0.40) was performed with sedation/analgesia temporarily removed or reduced to obtain a Riker Sedation-Agitation Score of 4 [15]. During the SBT all indices were measured after 30 and 90 min; measurements at 90 min were used for statistical analysis. An arterial blood gas was obtained 5 min prior to and 30 min after extubation. The decision to extubate was made by the attending physician based on routinely used criteria (Table 2). For both patient sets and during all phases of the study, WOBN/min data were blinded to attending physicians and did not influence the decision to extubate. Following extubation, all patients breathed spontaneously through an aerosol facemask (FIO2 0.40). Successful extubation was defined using routine standards as the ability to sustain appropriate spontaneous breathing (f ≤ 30/min) and blood gas exchange, i.e., pulse oximeter oxygen saturation (SpO2) > 92%, PaO2/FIO2 ≥ 150–300, PaCO2 ≤ 50 mmHg for non-chronic obstructive pulmonary disease (COPD) patients, ≤55–60 mmHg for COPD patients, pH ≥ 7.30, and ability to cough and protect airway for greater than 24 h after extubation. Objective criteria for extubation failure were PaCO2 > 50 mmHg for non-COPD patients and >55–60 mmHg for COPD patients, PaO2 < 60 mmHg (FIO2 ≤ 0.40), f > 35/min, inability to cough and/or protect airway, and a worsening of hemodynamic or neurological conditions. Patients failing extubation were reintubated and provided with ventilatory support at the direction of the attending physician.
A combined pressure/flow/carbon dioxide sensor, positioned between the endotracheal tube and Y piece of the ventilator breathing circuit, directed data to a respiratory monitor (NICO, Respironics) for measurements including PSV, PEEP, f, V T, f/V T, MV, inspiratory flow rate, partial pressure end-tidal CO2 (PetCO2), SpO2, CO2 min production (VCO2), and physiologic dead space volume-to-tidal volume ratio (V D/V T). All data from the monitor were, in turn, directed to a laptop computer containing software (Convergent Engineering, Gainesville, FL) for calculating respiratory system compliance (Crs) and resistance (Rrs) using the least squares method [16], and operating an ANN to determine WOBN/min. The training of this ANN and validation of WOBN/min data compared to conventional measurements of work of breathing per minute using an esophageal balloon in a similar group of adults receiving PSV have been described [10].
Data were analyzed using ANOVA and receiver-operator characteristic (ROC) curves [17]. Two sets of ROC curves were constructed. For the training set, ROC curves allowed threshold values for each index to be identified (values with the fewest false classifications [2]) that discriminated between patients successfully extubated and those who failed extubation. For the prospective validation set, the predictive performance of the threshold value for each index was assessed with ROC curves by evaluating the area under the curve (AUC). The AUC assesses and validates the performance of an index for predicting extubation outcome (greater AUC, greater accuracy for predicting). The AUC for all indices were compared using the StAR method [18]. The predictive performance of each index was assessed with sensitivity, specificity, and positive and negative predictive values [19]. Also, to assess the complementary relationship between work of breathing and breathing pattern data, a multiple regression model using the predictors WOBN/min and f/V T was developed to predict extubation outcome. Alpha was set at 0.05 for statistical significance.
Results
One (WOBN/min = 10.7 J/min) of the 7 extubation failure patients in the training set and 2 (WOBN/min = 8.4 and 12.6 J/min, respectively) of the 12 patients in the prospective validation set were unable to cough and clear secretions adequately to protect the airway, which contributed to failing extubation, requiring reintubation. Other reasons for failing extubation and reintubation for the remaining patients in both sets was the appearance of labored, rapid breathing and use of accessory muscles, and acute hypoxemia associated with an altered level of consciousness and disorientation.
For the training set, threshold values of 11 indices were identified (Table 3). Nine were indices used traditionally for assessing readiness for extubation including f, V T, f/V T ratio, MV, PaO2/FIO2 ratio, SaO2, PaCO2, V D/V T ratio, and Crs. The two remaining indices were WOBN/min and VCO2. For example, the threshold value identified for WOBN/min was ≤10 J/min.
These threshold values were applied to the prospective validation set to determine the predictive accuracy of each index (Table 4). The AUC for WOBN/min was 0.96 and significantly greater (p < 0.05) than all other indices (Fig. 1; Table 4). The AUCs for f and the PaO2/FIO2 ratio were 0.81 and 0.79, respectively, were comparable to each other, and were significantly greater than the remaining indices (Table 4). AUCs for V T, f/V T ratio, MV, SaO2, PaCO2, Crs, and VCO2 were lower, ranging from 0.52 to 0.76. WOBN/min had the highest sensitivity at 0.96, positive predictive value at 0.84, and negative predictive value at 0.96 compared to all indices (Table 4). Specificity for WOBN/min and f were high and comparable at 0.83 and 0.89, respectively, and greater than other indices. However, f had a sensitivity of only 0.54, positive predictive value of 0.54, and negative predictive value of 0.89. The indices V T, f/V T ratio, PaO2/FIO2 ratio, and SaO2 had substantially greater sensitivity but lower specificity than f, and all had comparable negative predictive values. Positive predictive values for these indices were ≤0.54. For PaCO2 and VCO2, AUC, sensitivity, specificity, and positive predictive values were low, and negative predictive values were in the 0.75 range. MV and Crs had the lowest sensitivity and low negative predictive values.
ROC curves for non-invasively determined work of breathing per min (WOBN/min) in J/min and some traditional indices used to predict extubation from ventilatory support such as spontaneous breathing frequency in breaths/min (f), spontaneous tidal volume in ml (V T), and the ratio of spontaneous breathing frequency to tidal volume or index of rapid shallow breathing (f/V T) in breaths/min/l are shown for the prospective validation set of patients. The area under the curve (AUC) is generated by plotting the true positive rate or sensitivity against the false-positive rate or 1-specificity. AUC for WOBN/min was significantly greater (i.e., a better model for predicting) than AUCs for f, V T, and f/V T ratio, as well as other indices used to predict extubation, as shown in Table 4 (p < 0.05)
For the prospective validation set of patients, WOBN/min for those successfully extubated was 5 ± 2.3 J/min compared to 13.2 ± 4.6 J/min (p < 0.05) for those failing extubation (Table 5). For 95% of patients who were successfully extubated, WOBN/min was less than or equal to 10 J/min, while 83% of patients who failed extubation had a WOBN/min greater than 10 J/min. Those patients who were successfully extubated had significantly lower values for f, f/V T ratio, MV, and V D/V T ratio and higher values for Crs, PaO2, and PaO2/FIO2 ratio than those who failed (Table 5). WOBN/min and f/V T were significant predictors in a multiple regression model to predict extubation outcome, r 2 = 0.86 (p < 0.002).
Discussion
WOBN/min had the greatest overall predictive accuracy (AUC), and the greatest sensitivity and positive and negative predictive values compared to other indices. Regarding f/V T, compared to Yang and Tobin [2] who also used training and prospective validation sets, we observed lower sensitivity (0.80 compared to 0.97), specificity (0.57 compared to 0.64), and positive predictive values (0.33 compared to 0.78), while negative predictive values were comparable (0.91 compared to 0.95). Possible reasons for the aforementioned differences may, in part, be patient types and methods of ventilation. Our patients had blunt trauma and complex abdominal and neurologic surgeries requiring large fluid resuscitation. A relatively small percentage had concurrent pneumonia (12%), congestive heart failure (10%), or known COPD with a history of previous respiratory insufficiency (5%). We acknowledge that our surgical ICU has less representation of the patients described in Yang and Tobin’s medical ICU where pneumonia, COPD exacerbation, central nervous system disorders, congestive heart failure, and pulmonary fibrosis represent the bulk of the patients. SBTs for our patients employed low-level PSV and PEEP, while Yang and Tobin’s patients breathed spontaneously on ambient pressure and room air. Our patients received a slight positive pressure assist during inhalation from PSV, predisposing to larger V T, which is associated with lower f (thus, lower f/V T ratio), and may also have had larger functional residual capacities secondary to PEEP. The f/V T threshold as posited by Yang and Tobin may not apply during PSV [20].
This is not meant to impugn f/V T ratio data, for it reflects a patient’s response and tolerance for the breathing load. The pathophysiologic basis of rapid shallow breathing patterns may be a stress response reflecting an imbalance between inspiratory muscle capacity and load [2, 21]. WOBN/min used in association with the f/V T ratio reflects different and clinically useful physiologic information about a patient’s ability to breathe spontaneously; both are important. The combination of WOBN/min and f/V T predicted or explained 86% of the variance in predicting extubation outcome, a very good predictor. It may be reasonable to consider using WOBN/min and f/V T ratio data in a complementary manner when considering extubation.
Patients who were extubated successfully showed work of breathing values in the normal adult range [6], i.e., 5 ± 2.3 J/min, or in a few cases >10 J/min. For those who were extubated successfully, 95% of that group had a WOBN/min less than or equal to 10 J/min. For those failing extubation, 83% of that group had a WOBN/min >10 J/min. For the 5% of successfully extubated patients who had a WOBN/min in the 10–15 J/min range, it is speculated that such patients may be more physically fit, appropriately nourished, younger, and capable of tolerating moderately higher inspiratory muscle loads. For the 17% of failure patients who had a WOBN/min in the 5–10 J/min range, it is speculated that these patients may be weaker, emaciated, malnourished, elderly, and unable to tolerate normal to slightly increased inspiratory muscle loads. Another study may be needed to explore work of breathing and load tolerance relationships with respect to age, nutritional status, physical condition, and comorbidities, vis-à-vis predicting extubation.
Teixeira et al. [22] evaluated the predictive ability of work of breathing on extubation outcome in 51 adults in a surgical ICU over a 120-min SBT (T piece). For those failing extubation, work of breathing gradually increased to significantly higher values (>60% compared to starting value) over the SBT and was predictive of extubation failures. For work of breathing, the ROC area was 0.87, sensitivity was 0.91, specificity was 0.88, positive predictive value was 0.90, and negative predictive value was 0.89, congruent with our findings (Table 4). Patients in their study may be compared with our patients because the optimum pre-extubation mode of ventilation and duration of the SBT has not yet been identified [23]. SBT (30–120 min) using low-level PSV compared with T piece [24, 25], low-level PEEP compared with a T piece [26, 27], and PSV 5 cmH2O with PEEP 5 cmH2O for a timed trial [28] (as used in our study) were found to be equally effective, suitable methods for assessing readiness for extubation.
Fiastro et al. [29] compared work of breathing during SBT through a T piece to traditional indices like V T, MV, negative inspiratory pressure (NIP), and vital capacity for extubation in adults in a combined medical and surgical ICU. In one group who required mechanical ventilation for longer than 24 h, extubation was successful at a mean work of breathing of 1.09 kg m/min, equivalent to 10.6 J/min. This value corresponds to our threshold value for predicting extubation (Table 3). The authors concluded that for patients requiring prolonged ventilation, work of breathing may be a better indicator of successful extubation than traditional indices.
Because NIP can misrepresent inspiratory muscle strength [30] and was found to be a poor predictor of extubation outcome [5, 30, 31], we did not collect these data. It is unclear whether work of breathing referenced to a patient’s capabilities (inspiratory muscle strength) can be a predictor of extubation. Although not evaluated in this study, inspiratory muscle strength referenced to work of breathing (load), i.e., a strength–load ratio, may need to be evaluated in future studies.
There is growing awareness of the need to assess inspiratory muscle loads when considering extubation [5, 32–34]. Tobin et al. [5] contended that the main reason weaning attempts fail is because work of breathing is high consequent to abnormally increased respiratory system elastance and resistance and inspiratory muscles are unable to cope with the increased load, and that ventilator settings need to be monitored and adjusted to navigate a course between excessive work of breathing and excessive inspiratory muscle rest when considering extubation.
One study limitation is that our patients were from a surgical ICU (post-operative trauma, and complex abdominal, thoracic, and neurologic surgery). A few had COPD, as typically found in a medical ICU. None had severe forms of pulmonary dysfunction. It is unclear if our findings can be generalized to these types of patients. Another potential limitation concerns WOBN/min determinations, which reflect the total load on the inspiratory muscles to inhale, i.e., physiologic elastic and flow resistive work and imposed flow resistive work (resistive work on endotracheal tube, ventilator breathing circuit, and ventilator) [35]. These component loads cannot be differentiated using WOBN/min determinations. A third potential limitation is that WOBN/min determinations were validated for PSV only, a commonly used ventilator support mode. Another potential limitation is that it was not a purpose of our study to compare a 2-h SBT while breathing on ambient pressure through a T piece to using WOBN/min as a predictor of extubation during an SBT with the patient receiving 5 cmH2O PSV with 5 cmH2O PEEP. It is unclear if our method is superior. Lastly, excluded from the study were patients, who in the judgment of experienced attending physicians, were not considered as candidates for extubation due to poor cough strength, inadequate gag reflex, and increased frequency of suctioning due to increased sputum volume. These patients have a high risk of extubation failure.
In summary, inspiratory muscle loads during spontaneous inhalation as reflected by WOBN/min is a more accurate predictor of extubation than traditional indices. WOBN/min ≤10 J/min was observed for 95% of patients successfully extubated and may be a threshold value to be considered in adults for predicting extubation. Clinical outcome studies over a wider range of patient conditions to further evaluate the predictive ability of WOBN/min for extubation may be needed.
References
Epstein SK, Ciubotaru RL, Wong JB (1997) Effect of failed extubation on the outcome of mechanical ventilation. Chest 112:186–192
Yang KL, Tobin MJ (1991) A prospective study of indexes predicting the outcome of trials of weaning from mechanical ventilation. New Engl J Med 324:1445–1450
MacIntyre NR (1986) Respiratory function during pressure support ventilation. Chest 89:677–681
Brochard L, Harf A, Lorino H, Lemaire F (1989) Inspiratory pressure support prevents diaphragmatic fatigue during weaning from mechanical ventilation. Am Rev Respir Dis 139:513–521
Tobin MJ, Laghi F, Jubran A (2010) Narrative review: ventilator-induced respiratory muscle weakness. Ann Intern Med 153:240–245
Millic-Emilli J (1991) Work of breathing. In: Crystal RG, West JB (eds) The lung. Raven Press, New York, pp 1065–1075
Baxt WG (1995) Application of artificial neural networks to clinical medicine. Lancet 346:1135–1138
Rodvold DM, McLoad DG, Brandt JM, Snow PB, Murphy GP (2001) Introduction to artificial neural networks for physicians: taking the lid off the blackbox. Prostate 46:39–44
Leon MA, Lorini FL (1997) Ventilation mode recognition using artificial neural networks. Comp Biomed Res 30:373–378
Banner MJ, Euliano NR, Brennan V, Peters C, Layon AJ, Gabrielli A (2006) Power of breathing determined non-invasively with use of an artificial neural network in patients with respiratory failure. Crit Care Med 34:1052–1059
Proctor HJ, Woolsen R (1973) Prediction of respiratory muscle fatigue by measurements of work of breathing. Surg Gynecol Obstet 136:367–370
Peters RM, Hilberman M, Hogan JS, Crawford DA (1972) Objective indications for respiratory therapy in post-trauma and post-operative patients. Am J Surg 124:262–269
Henning RJ, Shubin H, Weil MH (1977) The measurement of work of breathing for clinical assessment of ventilator dependence. Crit Care Med 5:264–268
Kulkarni AP, Agarwal V (2008) Extubation failure in intensive care unit: predictors and management. Indian J Crit Care Med 12:1–9
Riker RR, Fraser GL, Simmons LE, Wilkins ML (2001) Validating the sedation–agitation scale with the bispectral index and visual analog scale in adult ICU patients after cardiac surgery. Intensive Care Med 27:853–858
Volta CA, Marangoni E, Alvisi V, Capuzzo M, Ragazzi R, Pavanelli L, Alvist R et al (2002) Respiratory mechanics by least squares fitting in mechanically ventilated patients: application on flow-limited COPD patients. Intensive Care Med 28:48–52
Mokhlesi B, Tulaimat A, Gluckman TJ, Wang Y, Evans AT, Corbridge TC (2007) Predicting extubation failure after successful completion of a spontaneous breathing trial. Resp Care 52:1710–1717
Vergara IA, Norambuena T, Ferrada E, Slater AW, Melo F (2008) StAR: a simple tool for the statistical comparison of ROC curves. Bioinformatics 9:265–272
Griner PF, Mayewski RJ, Mushlin A, Greenland P (1981) Selection and interpretation of diagnostic tests and procedures: principles and applications. Ann Intern Med 94:553–600
El-Khatib MF, Bou-Khalil P (2008) Clinical review: liberation from mechanical ventilation. Critical Care 12:221–232
Vassilakopoulos T, Zakynthinos S, Roussos C (1998) The tension-time index and frequency/tidal volume ratio are the major pathophysiological determinents of weaning failure and success. Am J Crit Care Med 158:378–385
Teixeira C, Teixeria PJZ, Pickersgill de Leon P, Oliveira ES (2009) Work of breathing during successful spontaneous breathing trial. J Crit Care 24:508–514
Epstein SK (2001) Predicting extubation failure. Chest 120:1061–1063
Estaban A, Alia I, Gordo F, Fernandez R, Solsona JF, Vallverdu I, Macias S, Allegue JM, Blanco J, Carriedo D, León M, de la Cal MA, Taboada F, Gonzalez de Velasco J, Palazón E, Carrizosa F, Tomás R, Suarez J, Goldwasser RS (1997) Extubation outcome after spontaneous breathing trials with T tube or pressure support ventilation. Amer J Resp Crit Care Med 156:459–465
Perren A, Domenighetti G, Mauri S, Genini F, Vizzardi N (2002) Protocol-directed weaning from mechanical ventilation: clinical outcome in patients randomized for a 30 min or 120 min trial with pressure support ventilation. Intensive Care Med 28:1058–1063
Jones DP, Byrne P, Morgan C, Fraser I, Hyland R (1991) Positive end expiratory pressure vs T piece. Chest 100:1655–1659
Bailey CR, Jones RM, Kelleher AA (1995) The role of continuous positive airway pressure during weaning from mechanical ventilation in cardiac surgical patients. Anaesthesia 50:677–681
Robertson E, Mann HJ, Hyzy R, Rogers A, Douglas I, Waxman AB, Weinert C, Alapat P, Guntupalli KK, Buchman TG et al (2008) Partnership for excellence in critical care. Multicenter implementation of a consensus-developed, evidenced-based, spontaneous breathing trial protocol. Crit Care Med 36:2753–2762
Fiastro JF, Habib MP, Shon BY, Campbell SC (1998) Comparison of standard weaning parameters and the mechanical work of breathing in mechanically ventilated patients. Chest 94:232–238
Laghi F, Tobin MJ (2003) Disorders of the respiratory muscles. Am J Respir Crit Care Med 168:10–48
Nemer SN, Barbas CSV, Calderia JB, Guimarães B, Azeredo LM, Gago R, Souza PC (2009) Evaluation of maximal inspiratory pressure, tracheal airway pressure, and its ratio in weaning outcome. J Crit Care 24:441–446
Tobin MJ, Laghi F, Brochard L (2009) Role of respiratory muscles in acute respiratory failure of COPD: lessons from weaning failure. J Appl Physiol 107:962–970
Goldstone J (2002) The pulmonary physician in critical care: difficult weaning. Thorax 57:986–991
Schultz M (2010) Weaning from mechanical ventilation: stay poised between load and strength. Anesthesiology 113:273–275
Banner MJ, Jaeger MJ, Kirby RR (1994) Components of work of breathing and implications for ventilator-dependent patients. Crit Care Med 22:515–523
Su WL, Chen YH, Chen CW, Yang SH, Su CL, Perng WC, Wu CP, Chen JH (2010) Involuntary cough strength and extubation outcomes for patients in an ICU. Chest 137:777–782
Smina M, Salam A, Khamiees M, Gada P, Amoateng-Adjepong Y, Manthous CA (2003) Cough, peak flows and extubation outcomes. Chest 124:262–268
Salam A, Tilluckdharry L, Amoateng-Adjepong Y, Manthous CA (2004) Neurologic status, cough, secretions and extubation outcomes. Inten Care Med 30:1334–1339
Acknowledgments
This research was supported by grants from Respironics Inc. Dr. Banner is a consultant for Convergent Engineering. Dr. Euliano is President and CEO of Convergent Engineering. Drs. Gabrielli, Layon, Al-Rawas, and Martin are employees of the University of Florida.
Conflict of interest
The authors have a US patent describing the application of an artificial neural network to a mechanical ventilator for determining work of breathing.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Banner, M.J., Euliano, N.R., Martin, A.D. et al. Noninvasive work of breathing improves prediction of post-extubation outcome. Intensive Care Med 38, 248–255 (2012). https://doi.org/10.1007/s00134-011-2402-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-011-2402-2