Abstract
Background
While a number of studies in the western countries have provided estimates of prevalence for child psychiatric morbidity and associated risk factors, relatively little is known about child psychiatric problems and risk factors in develo** countries like Pakistan.
Method
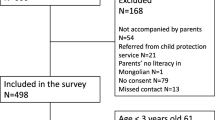
A cross sectional survey of 5–11-year-old children attending main stream private and community schools in Karachi was conducted. Seven private and eight community schools agreed to participate. About 1488 consent forms were sent to 700 parents of private school and 788 parents of community school children. A total of 675 parents agreed to participate in the study. The response rate was 45.4%. Assessment of children’s mental health was conducted using Strength and difficulties questionnaire (SDQ) by parents based on cut-off provided by Goodman.
Results
About 47% children were rated as normal, 19% as borderline and 34% as abnormal by the parents. Ordinal regression was used to identify factors associated with parent’s rating. The odds of female children of being normal was 1.5 times relative to male children, adjusting for school type and mother’s education (ORadj = 1.5, 95% CI: 1.1–2.0). Children attending private schools were more likely to be normal as compared to community school children, adjusting for child’s gender and mother’s education (ORadj = 2.3, 95% CI: 1.3–4.0).
Conclusion
In the present study, prevalence of child mental health problems was higher than reported in studies from other countries. Prevalence was higher amongst children attending community schools. Consistent with most studies, male children were at a higher risk than females. There is a need for develo** programs to train, sensitise and mobilize teachers and parents regarding child’s psychological, emotional and behavioural problems with special attention to community schools. Since the male child is at a greater risk we should be cognizant of this while evaluating children for psychopathology.

Similar content being viewed by others
References
Bird HR, Gould MS, Yager T, Staghezza B, Canino G (1989) Risk factors for maladjustment in Puerto Rican children. J Am Acad Child Adolesc Psychaitry 28:847–850
Brown GW, Harris TO, Bifulco A (1985) Long-term effects of early loss of parent. In: Rutter M, Izard CE, Read PB (eds) Depression in young people: developmental and clinical perspectives. Guilford Press, New York, pp 251–296
Eapen V, Abou-Saleh M (2003) Children with psychiatric disorders: the Al Ain community psychiatric survey. Can J Psychiatry 48:402–407
Farrington DP, Loeber RG, van Kammen WB (1990) Long-term criminal outcomes of hyperactivityimpulsivity-attention deficit and conduct in childhood. In: Robins LN, Rutter M (eds) Straight and devious pathways from childhood to adulthood. Cambridge: Cambridge University Press, pp 62–81
Federal Bureau of statistics (FBS). Government of Pakistan (April, 2001) http://www.statpak.gov.pk
Fleitlich B, Goodman R (2001) Social factors associated with child mental health problems in Brazil—a cross-sectional survey. BMJ 323:599–600
Fleitlich B, Goodman R (2004) Prevalence of child and adolescent psychiatric disorders in southeast Brazil. J Am Acad Child Adolesc Psychiatry 43:727–734
Goodman R (1997) The Strengths and Difficulties Questionnaire: A research note. J Child Psychol Psychiatry 38:581–586
Goodman R (1999) The extended version of the Strengths and Difficulties Questionnaire as a guide to child psychiatric caseness and consequent burden. J Child Psychol Psychiatry 40:791–799
Goodman R, Scott S (1999) Comparing the strengths and difficulties questionnaire and child behaviour checklist: is small beautiful? J Abnormal Child Psychol 27:17–24
Goodman R, Slobodskaya H, Knyazev G (2005) Russian child mental health: a cross-sectional study of prevalence and risk factors. Eur Child Adolesc Psychiatry 14:28–33
Gureje O, Omigbodun O (1995) Children with mental disorders in primary care: functional status and risk factors. Acta Psychitr Scand 92:310–314
Hackett R, Hackett L, Bakta P, Gowers S (1999) The prevalence and association of psychiatric disorder in children in Kerala, South India. J Child Psychol Psychiatry 40:801–807
Harrington R (1993) Depression disorder in childhood and adolescence. Wiley, Chichester
Javad AM, Kundi MZ, Khan AP (1992) Emotional and behavioural problems among school children in Pakistan. J Pakistan Med Assoc 42:181–184
Margot P, Shanya V, Diana S (2005) Behavioural problems in Sri Lankan schoolchildren : Associations with socio-economic status, age, gender, academic progress, ethnicity and religion. Soc Psychiatry Psychiatr Epidemiol 40:654–662
Meltzer H, Gatward R, Goodman R, Ford T (2000) Mental health of children and adolescents in Great Britain. London: The Stationery Office
Mullick MS, Goodman R (2005) The prevalence of psychiatric disorders among 5–10 year-olds in rural, urban and slum areas in Bangladesh: an exploratory study. Soc Psychiatry Psychiatr Epidemiol 40:663–671
Mumford DB, Minhas F, Akhter F, et al. (2000) Stress and psychiatric disorder in urban Rawalpindi. Brit J Psychiatry 177:557–562
Nikapota AD (1991) Child psychiatry in develo** countries. Brit J Psychiatry 158:743–751
Patel V, Kleinman A (2003) Poverty and common mental disorders in develo** countries. Bull World Health Organ 81:609–615
Roberts RE, Attkinson CC, Rosenblatt A (1998) Prevalence of psychopathology among children and adolescents. Am J Psychiatry 155:715–725
Rutter M (ed) (1988) Studies of psychosocial risk. Cambridge University Press, Cambridge
Rutter M (1989) Pathways from childhood to adult life. J Child Psychol Psychiatry 30:23–51
Samad L, Hollis C, Prince M, Goodman R (2005) Child and adolescent psychopathology in a develo** country: testing the validity of the Strength and Difficulty Questionnaire (Urdu Version). Int J Methods Psychiatr Res 14(3):158–166
Srinath S, Girimaji SC, Gururaj G, Seshadri S, Subbakrishna DK, Bhola P, Kumar N (2005) Epidemiological study of child & adolescent psychiatric disorders in urban and rural areas of Bangalore, India. Indian J Med Res 122:67–79
Verhulst FC, Koot HM (eds) (1995) The epidemiology of child and adolescent sychopathology. Oxford University Press, Oxford
Acknowledgement
The study was generously supported by grants form Sindh Education Foundation (SEF) and Aga Khan University Hospital (AKUH) Karachi, Pakistan. We are grateful for the guidance and support provided by Dr Panos Vostanis, (Professor of Child and Adolescent Psychiatry), Greenwood Institute of Child Health, University of Leicester.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Syed, E.U., Hussein, S.A. & Mahmud, S. Screening for emotional and behavioural problems amongst 5–11-year-old school children in Karachi, Pakistan. Soc Psychiat Epidemiol 42, 421–427 (2007). https://doi.org/10.1007/s00127-007-0188-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-007-0188-x