Abstract
Aims/hypothesis
Cardiovascular risk in diabetes is at least in part attributable to defective angiogenesis. Since diabetes negatively affects blood cells involved in angiogenesis, we herein evaluated whether diabetes impairs proangiogenic granulocytes (PAGs).
Methods
We characterised and quantified PAGs as CD49d+ granulocytes in peripheral blood of participants with type 2 or type 1 diabetes and in non-diabetic control participants. We evaluated PAG antigenic profile and assessed in vitro functional properties of CD49d+ granulocytes using 2D and 3D angiogenesis assays. We also quantified PAGs before and after glucose control with a sodium–glucose cotransporter 2 (SGLT2) inhibitor, dapagliflozin. In parallel, we measured Ly6G+CD49d+ PAGs in streptozotocin-induced type 1-like diabetic mice vs non-diabetic control mice.
Results
PAGs were composed of eosinophils (>80%) and neutrophils (<20%). Within both populations, CD49d identified CXCR4high/VEGFR1high cells. CD49d+ granulocytes supported in vitro angiogenesis by endothelial cells significantly more than CD49d− control granulocytes, and physically interacted with endothelial cells. Granulocytes from type 2 diabetic participants had a profoundly impaired capacity to stimulate endothelial cell tubule formation compared with those from non-diabetic control participants. CD49d+ PAGs were reduced by 30–40% and were functionally impaired in diabetic vs control individuals. PAG levels inversely correlated with plasma glucose (r = −0.25; p = 0.025) and significantly increased 1.8-times after glucose control with dapagliflozin, which reduced HbA1c by 1.0% (11 mmol/mol). Levels of Ly6G+CD49d+ PAGs were also significantly reduced also in type 1 diabetic mice vs control mice.
Conclusions/interpretation
We illustrate a significant impairment of PAGs in diabetes and provide evidence for a direct role of hyperglycaemia. These findings add mechanistic information to explain the defective angiogenesis in diabetes.

Graphical abstract
Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
People with diabetes have a reduced life expectancy, with most excess mortality due to cardiovascular causes [1]. The mechanisms driving excess cardiovascular risk in diabetes are manifold and still incompletely understood. In addition to accelerating the onset of vascular occlusive diseases, diabetes worsens the outcome after acute myocardial infarction and stroke [2,3,4]. It has been hypothesised that responses to ischaemia are compromised in patients with diabetes, at least in part because of defective angiogenesis [5, 6]. The well-established blockade of angiogenesis in diabetes has multiple mechanisms [7], including alterations of hypoxia-related pathways, chronic inflammation, and reduction of bone marrow (BM)-derived proangiogenic cells. Among these, we have extensively characterised the defect of endothelial progenitor cells (EPCs) in individuals with diabetes and how reduction of BM-derived stem/progenitor cells predicted adverse cardiovascular outcomes [8, 9]. Besides EPCs, other blood cell types can be involved in the proangiogenic response to tissue ischaemia, including monocyte-macrophages. Interestingly, diabetes is associated with reductions in the levels of so-called M2 (anti-inflammatory) macrophages [10], which exhibit a distinctive proangiogenic capacity [11]. Among inflammatory cells, neutrophils have also been shown to modulate angiogenesis, especially in the setting of cancer [12], for instance through secretion of vascular endothelial growth factor (VEGF) [13]. Recently, a specific population of CD49d+ proangiogenic granulocytes (PAGs) in the murine neutrophil population has been characterised, with a similar population being observed in the human blood [14]. Given that diabetes im**es upon neutrophil levels and function, we hypothesised that this population of cells could be affected.
In the present study, we first characterised PAGs in the human blood and then explored whether diabetes is associated with changes in the levels and function of PAGs. Finally, we evaluated the role of hyperglycaemia in modulating PAGs.
Methods
Participants
Diabetic and non-diabetic control participants were recruited at the University Hospital of Padova. The study was approved by the local ethics committee and all participants provided written informed consent. For the cross-sectional study, we included participants with diabetes (type 2 or type 1) for at least 1 year and non-diabetic control participants, who were male or female, aged 18–80 years. Exclusion criteria were: acute disease or infection, haematological disorders, immunological disorders (such as rheumatoid arthritis, but excluding type 1 diabetes and autoimmune thyroid disease), immunosuppression or organ transplantation, pregnancy or lactation, and inability to provide informed consent. For all participants, we collected the following information: age, sex, disease duration (for individuals with diabetes), height and weight for the calculation of BMI, current smoking habit, prevalence of hypertension, and values for fasting plasma glucose, HbA1c, plasma total cholesterol, HDL-cholesterol, triacylglycerol (LDL-cholesterol was calculated using the Friedewald formula [15]), serum creatinine, and urinary albumin excretion rate (as urinary albumin/creatinine ratio [ACR] in mg/mmol). We also collected information on current glucose-lowering medications and other concomitant medications. Diabetic complications were defined as follows. Retinopathy was defined based on digital funduscopic examination and scored according to ETDRS (early treatment of diabetic retinopathy study) [16]. Neuropathy was defined as a history of symptoms suggestive of peripheral polyneuropathy confirmed by nerve conduction velocity or in the presence of pathologic autonomic neuropathy tests. Nephropathy was defined as an ACR > 30 mg/g (3.39 mg/mmol) or eGFR (using Chronic Kidney Disease-Epidemiology Collaboration [CKD-EPI] equation [17]) <60 ml min−1 (1.73 m)−2. Coronary artery disease was defined as a past history of myocardial infarction, coronary revascularisation or angiographic evidence of haemodynamically significant coronary stenosis. Peripheral arterial disease was defined as a history of claudication or rest pain, confirmed by angiographic or ultrasonographic evidence of haemodynamically significant stenosis of leg arteries, or as a history of peripheral revascularisation. Cerebrovascular disease was defined as a history of stroke or transient ischaemic attack or as evidence of asymptomatic carotid atherosclerosis. The metabolic syndrome and its components were defined based on the revised ATP-III definition [18].
To examine the effects of glucose control with sodium–glucose cotransporter 2 (SGLT2) inhibition, we measured PAGs in a subgroup of type 2 diabetic patients enrolled in a trial of dapagliflozin therapy (NCT02327039, for details see [9]).
Animals
All animal protocols were approved by the local and national ethics committee and were conducted in compliance with the Guide for the care and use of laboratory animals, Eighth edition (2011). C57Bl/6J mice from an in-house colony (at the Veneto Institute of Molecular Medicine) were rendered diabetic by a single intraperitoneal injection of streptozotocin (STZ) at 175 mg/kg in 100 mmol/l sodium citrate buffer, pH 4.5. Blood glucose was measured using a point-of-care glucometer (FreeStyle Optium, Abbott, Rome, Italy). Only animals with persistently elevated glucose levels (>16.7 mmol/l) were considered diabetic and retained in the study. Experiments were performed 4 weeks after confirming hyperglycaemia. C57Bl/6J mice treated with vehicle and observed for 4 weeks were used as controls. Mice were randomly assigned to STZ or vehicle using the coin toss method and personnel in charge of assessing endpoints were blind to the treatment received by each mouse. Body weight was monitored weekly. In all animals we measured blood glucose, HbA1c, total cholesterol, triacylglycerol and creatinine using a point-of-care system (Allegro, Nova Biomedicals, Milan, Italy).
Flow cytometry
Identification and quantification of PAGs was performed using fresh peripheral blood. Antibodies are listed in electronic supplementary material (ESM) Table 1. Cells were labelled with CD45, CD16, CD49d, C-X-C chemokine receptor type 4 (CXCR4) and VEGF receptor (VEGFR)1. After erythrocyte lysis, cells were analysed on a FACSCanto II instrument and scored using FACS Diva (both from Becton Dickinson [BD], Milan, Italy). We gated granulocytes in the morphologic side scatter area (SSC-A) vs forward scatter area (FSC-A) gate based on size and complexity. Then, we identified and scored the population of CD49d+ cells in the morphologic granulocyte gate. Contamination of the granulocytic CD49d+ population was ruled out by staining with CD9, CD3, CD56, CD10, CD19, CD14, CD24, CD15, CD66b and CD11b; we examined expression of such markers on CD49d+ cells in the granulocytic vs the mononuclear (lymphomonocytic) cell gate. From the morphologic granulocyte population, we identified neutrophils and eosinophils in the CD45 vs CD16 plot. In separate experiments, granulocyte identity in the CD45/CD16 plot was confirmed using intracellular staining with the neutrophil-specific marker myeloperoxidase (MPO), and the eosinophil-specific markers C-C motif chemokine receptor 3 (CCR3) and sialic acid-binding immunoglobulin-type lectin (SIGLEC)8. Per cent expression of CD49d was then evaluated separately in the neutrophil and eosinophil populations. We compared mean fluorescence intensity (MFI) of CXCR4 and VEGFR1 on gated CD49d+ and CD49d− granulocytes, and then separated for neutrophils and eosinophils.
For quantification of murine PAGs, mice were killed and blood was collected by cardiac puncture. PAGs were identified and scored using a strategy similar to that developed in humans. Cells in the morphologically defined granulocyte population were stained for lymphocyte antigen 6 complex locus G6D (Ly6G) (eBioscience, Thermo Fisher Scientific, Monza, Italy) and CD49d (cat no. 564394, BD) in order to identify CD49d+ neutrophils (Ly6G+) and CD49d+ eosinophils (Ly6G−). Eosinophil vs neutrophil identity of gated Ly6G+/− granulocytes was confirmed by SIGLEC-F staining. CD115 was used to rule out contamination with CD49d+ mononuclear cells. Then, by co-staining cells for CXCR4 and VEGFR1, we examined MFI on CD49d+ neutrophils or eosinophils, relative to the respective CD49d− control. Absolute cell counts were obtained multiplying relative cell counts by the number of white blood cells/μl of blood, obtained on a Sysmex XE-series haematology analyser (Sysmex Sverige, Kungsbacka, Sweden), which also yielded the automated differential cell counts. The same trained operator performed the analysis throughout the study.
Cell isolation
Granulocytes were isolated from anticoagulated whole blood of healthy blood donors. Non-target cells were removed by immunomagnetic depletion (MACSxpress Human Neutrophil Isolation Kit, Miltenyi Biotec, Bologna, Italy) and erythrocytes were sedimented, yielding a granulocyte population with the same representation of neutrophils and eosinophils observed in whole blood.
In other experiments, CD49d+ granulocytes were separated from fresh peripheral blood using FACSAria (BD). We either sorted CD49d+ cells from the entire morphologically defined (SSC-A and FSC-A) granulocyte population or within the CD16+ (neutrophil) or CD16− (eosinophil) subset of granulocytes. Elevated autofluorescence was also used to differentiate eosinophils from neutrophils [19]. To have definite confirmation that CD16+CD49d+ granulocytes were neutrophils, whereas CD16−CD49d+ granulocytes were eosinophils, we spotted freshly sorted cells onto glass slides that were stained with May–Grünwald–Giemsa.
Preparation of conditioned medium
Peripheral blood from healthy donors was lysed and stained with APC-labelled anti-CD45 antibody (BD). Then, 100,000 cells of each population were seeded in 1 ml of supplemented Endothelial Cell Growth Medium (PromoCell) and cultured in standard conditions (5% CO2; 37°C) for 16 h. Conditioned medium samples were collected and centrifuged at 1000 g for 10 min to remove cell debris, and supernatants were collected to perform the tube formation assay.
Tubule formation assay
HUVECs, passages 2–4, were cultured in supplemented endothelial growth medium (EGM, Lonza, Basel, Switzerland) on plastic and then transferred to 96-well plates coated with Matrigel. In this condition, within a few hours, cells organise in longitudinal tubes connected to each other. To test in vitro the activity of CD49d+ and CD49d− granulocytes, cells were freshly sorted with FACSAria (BD) based on the expression of CD49d in the granulocyte gate, labelled with PKH67 and co-incubated at a ratio of 1:12 (1250 CD49d+/− cells and 15,000 HUVECs) with HUVECs for the tubule formation assay. After 24 h of incubation, cells were visualised under an inverted fluorescence microscope (IX71; Olympus, Tokyo, Japan). Tubule numbers, intersections and tubule length were quantified using ImageJ (Bethesda, MD, USA). In separated experiments, HUVECs were co-incubated at the same 1:12 ratio with granulocytes isolated from patients with diabetes or non-diabetic control individuals.
Spheroid sprouting assay
For preparation of methocoel, 6 g of methylcellulose together with a magnetic stir bar were autoclaved in a 500 ml flask. Then, 250 μl of 60°C endothelial basal medium (EBM) was added under sterile conditions and the suspension was stirred at 60°C for 40 min. Additional 250 ml of EBM medium were added and the solution was stirred at 4°C overnight. Portions of 50 ml of the solution were centrifuged for 2 h at 2500 g at room temperature. The highly viscose soluble fraction was separated from insoluble residue and was stored at 4°C. For the spheroid assay, 48,000 HUVECs were mixed with 6 ml of methocoel and seeded as 100 μl drops in a 96-well U-bottomed dish using a multipette. The cells were incubated for 24 h in an incubator to form spheroids. The following day, spheroids were collected and centrifuged and the spheroid pellet was mixed with methocoel mix. The collagen gel was prepared on ice and 500 μl of collagen gel were added to the spheroid/methocoel solution, mixed by pipetting and seeded on a 24-well culture dish for 30 min in an incubator. The spheroids were cultured for 24 h at 37°C and 5% CO2 with 1500 CD49d+ or CD49d− granulocytes labelled with PKH67 (green). Spheroids were finally fixed with formaldehyde. The sprouting area was quantified using ImageJ.
Gene expression in haematopoietic colonies
During a previous study [20], we collected blood samples from diabetic and non-diabetic individuals before and 8 h after stimulation with the stem cell mobilising agent plerixafor. CD34+ stem cells from these samples were purified using the Diamond human CD34 isolation kit (Miltenyi Biotec) and 500 cells were plated on the Methocult colony forming assay (Stem Cells). At the end of the culture period, white colonies were manually picked-up and resuspended in QIAzol Lysis reagent for RNA isolation. cDNA was synthesised using SensiFAST cDNA Synthesis Kit (Bioline, London, UK) and qPCR was performed using SensiFAST SYBR Lo-ROX Kit (Bioline) via a QuantStudio 5 Real-Time PCR System (Thermo Fisher Scientific, MA, USA). PRG2 primers were: forward CCTGGTTTCCATCCACAACTTCAA; reverse TGCCGTCAACCCACTGAA.
Statistical analysis
Continuous variables were reported as mean ± SD if normal, unless otherwise specified, or as median (interquartile range) if not normal. Normality was checked using the Kolmogorov–Smirnov test. Non-normal variables were log-transformed (base 10) before statistical analysis with parametric tests. Categorical variables were reported as percentage. Comparison between two or more groups was performed using unpaired two-tailed Student’s t test or ANOVA, respectively. Categorical variables were compared using the χ2 test. The post hoc Bonferroni correction was applied. Intragroup comparisons (before/after) were performed using the paired two-tailed Student’s t test. Linear correlations were checked using the Pearson’s r coefficient. A multiple linear regression analysis was performed to evaluate the association between covariates, entered as a single block, and levels of PAGs as the dependent variable. Statistical significance was accepted for p < 0.05. SPSS version 23.0 (IBM, USA) was used.
Results
Characterisation of human CD49d+ granulocytes
We first characterised the phenotype of CD49d+ granulocytes in humans (Fig. 1). We found that, among 46 healthy individuals, a discrete population of CD49d+ granulocytes was always present (Fig. 1a,b), which represented 7.6 ± 0.8% of the granulocyte gate, and was higher in men than in women (9.3 ± 1.3% vs 6.2 ± 0.8%; p = 0.046; Fig. 1c). CD49d+ cells in the polymorphonuclear cell gate, compared with CD49d+ in the mononuclear cell gate, were positive for CD24, CD10, CD15, CD66b, CD11b and negative for CD3 (T cells), CD19 (B cells), CD56 (NK cells) and CD14 (monocytes). Therefore, CD49d+ granulocytes were not contaminated by lympho-monocytes (ESM Fig. 1).
Identification and quantification of PAGs by flow cytometry. We first gated granulocytes in the morphologic FSC-A vs SSC-A plot (a) and then examined the resulting population for expression of CD49d (b). Quantification of CD49d+ granulocytes in non-diabetic individuals is shown in (c), stratified by sex (*p < 0.05). Within the granulocyte gate shown in (a), we then distinguished neutrophils from eosinophils in the CD16 vs CD45 gate (d). CD16−CD45bright eosinophils and CD16+CD45+ neutrophils defined antigenically were examined for intracellular expression of MPO (e) and for other markers: CXCR4, VEGFR1, CD49d, CCR3 and SIGLEC8 (f). Quantitative expression of CD49d was determined on CD16− (g, eosinophils) and CD16+ (h, neutrophils) granulocytes; CXCR4 and VEGFR1 expression on CD49d+ and CD49d− fractions within the eosinophil and neutrophil populations is shown in the histograms in (g) and (h), respectively. (i) Identification of CD49d+ eosinophils (CD16−) and neutrophils (CD16+) in the gate used to sort cells for subsequent May–Grünwald–Giemsa staining (j; scale bar 10 μm): the typical bi-/tri-lobulated nucleus and pink cytoplasm confirmed eosinophil identity compared with the multi-lobulated nucleus and pale cytoplasm of neutrophils. (k) Intracellular MPO content was examined in gated CD16−CD49d+ eosinophils and CD16+CD49d+ neutrophils: although eosinophils showed the typical high autofluorescence, MPO-labelled cells showed no signal compared with the negative control, whereas neutrophils showed bright MPO signal compared with control. Histograms show mean and SEM, while circles indicate individual data points. Eo, eosinophils; Neu, neutrophils
Since CD49d has long been considered a marker of eosinophils [19], we checked whether CD49d+ granulocytes were eosinophils or neutrophils. Neutrophils and eosinophils were distinguished as being CD16+CD45+ and CD16−CD45bright, respectively (Fig. 1d). As a confirmation of this immune-phenotype, we found intracellular expression of MPO in gated neutrophils but not in eosinophils (Fig. 1e), whereas expression of CCR3 and SIGLEC8 confirmed the identity of CD16−CD45bright as eosinophils (Fig. 1f). CD49d was expressed by the vast majority of eosinophils (94.2 ± 1.0%; Fig. 1g) and by a small fraction of neutrophils (1.1 ± 0.3%; Fig. 1h) Taking into account that eosinophils represented ~5% of granulocytes, it appeared that the total CD49d+ granulocyte population was composed of >80% eosinophils and <20% neutrophils (Fig. 1i). Analysis of May–Grünwald–Giemsa staining (Fig. 1j) and MPO intracellular content (Fig. 1k) confirmed that CD16− granulocytes were eosinophils whereas CD16+ granulocytes were neutrophils and that both subpopulations could be distinguished in CD49d+ and CD49d− cells.
We then compared CXCR4 and VEGFR1 expression on CD49d+ vs CD49d− cells separately in the CD16− eosinophil and CD16+ neutrophil gates (Fig. 1g,h). Within the small fraction of CD49d+ neutrophils, both CXCR4 and VEGFR1 expression was higher than in CD49d− neutrophils. Expression of CXCR4 and VEGFR1 was also higher in CD49d+ vs CD49d− eosinophils. In general, expression of CXCR4 and VEGFR1 were higher in eosinophils (~94% of which were CD49d+) than in neutrophils (~98% of which were CD49d−) (Fig. 1f). These data highlight that, within the granulocyte population, CD49d identified cells with distinctive eosinophil or neutrophil characteristics, both of which expressed high levels of the proangiogenic markers CXCR4 and VEGFR1. Interestingly, the association between CD49d and CXCR4/VEGFR1 expression was not found in the mononuclear cell gate (ESM Fig. 2), suggesting that the proangiogenic antigenic phenotype associated with CD49d expression is specific for granulocytes.
In vitro angiogenic activity of human CD49d+ granulocytes
We employed two in vitro assays to evaluate the capacity of CD49d+ granulocytes to support angiogenesis by human endothelial cells. CD49d+ or CD49d− granulocytes freshly sorted from healthy donors were mixed with endothelial cells in 2D Matrigel for tubule formation assay. Presence of CD49d+ vs CD49d− granulocytes significantly increased total tubule length, total number of tubules and tubule intersections (Fig. 2a,b; additional representative images in ESM Fig. 3a), while not affecting mean tube length. In separate experiments, CD49d+ or CD49d− granulocytes were stained with the green fluorescent dye PKH67 to visualise their physical interactions with endothelial cells in the tubules (Fig. 2c; additional representative images in ESM Fig. 3b). While CD49d− granulocytes were mainly interspersed in the Matrigel or located at tube intersections, CD49d+ neutrophils were mainly located within tubules (Fig. 2d). This finding suggested that contact of CD49d+ cells with endothelial cells was needed for the proangiogenic effect. To support this hypothesis, we performed experiments with conditioned media from unselected granulocytes and CD49d+ and CD49d− granulocytes, as illustrated in Fig. 2e. While tube length increased with a soluble positive control stimulus (VEGF), it did not change with any of the conditioned media (Fig. 2f). These data confirm that contact of granulocytes with endothelial cells is needed to exert the proangiogenic activity, possibly mediated by the adhesion molecule CD49d.
Functional characterisation of CD49d+ granulocytes. (a, b) Effects of co-incubation of CD49d+ or CD49d− granulocytes with HUVECs on total tubule length, number of tubules and intersections (a; *p < 0.05 vs CD49d−; the horizontal dashed line represents the negative control with unstimulated HUVECs). Representative images reconstructed from multiple fields are shown in (b) (additional replicates from the same experiment are shown in ESM Fig. 3a). (c, d) In separate experiments, CD49d+ or CD49d− granulocytes were labelled in green with PKH67 (c) and the proportion of green cells in the tubules, intersections or interspersed in the Matrigel were quantified (d; *p < 0.05 post-ANOVA; additional replicates from the same experiment are shown in ESM Fig. 3b). (e) Schematic representation of the experiment performed with conditioned media. (f) Total tube length formed by HUVECs in the presence of VEGF (as a positive control) or conditioned medium from unselected polymorphonuclear (PMN) granulocytes, CD49d+ or CD49d− granulocytes (*p < 0.05 vs the negative control of unstimulated HUVECs, represented by the dashed line). (g) Tube formation by HUVECs co-incubated with CD49d+ or CD49d− cells from the CD16+ neutrophil or CD16− eosinophil population (*p < 0.05 vs CD49d−; the negative control with unstimulated HUVECs is represented by the dashed line). (h) Effects of co-incubation of CD49d+ or CD49d− granulocytes with HUVECs on spheroid sprouting area; *p < 0.05. In representative microphotographs, the sprouting area contour is shown. (i) In separate experiments, CD49d+ or CD49d− granulocytes were labelled in green with PKH67 and the ratio of green fluorescence in the core spheroid vs the sprouting area was compared (*p < 0.05). Histograms show mean and SEM, while circles indicate individual data points. In (a, b, f) the horizontal dashed lines represent the negative control with unstimulated HUVECS
We then performed experiments to compare the in vitro proangiogenic potential of human CD49d+ neutrophils vs CD49d+ eosinophils. Cells were freshly sorted into CD16+CD49d+/− neutrophils and CD16−CD49d+/− eosinophils. Both within the CD16+ neutrophil and the CD16− eosinophil populations, CD49d+ cells supported tubule growth more than did CD49d− cells (Fig. 2g).
As a second in vitro angiogenesis model, we used the spheroid sprouting assay. CD49d+ or CD49d− granulocytes freshly sorted from healthy donors were mixed with endothelial cells, cultured as hanging drops to form spheroids, and embedded in a 3D collagen matrix. The sprouting area at 24 h was significantly higher when endothelial cells were co-cultured with CD49d+ than with CD49d− granulocytes (Fig. 2h). In separate experiments, CD49d+ or CD49d− granulocytes were stained with the fluorescent dye PKH67 to visualise physical interactions with endothelial cells in the sprouts. While the majority of CD49d− granulocytes remained trapped in the endothelial cell spheroid, CD49d+ granulocytes were often located in the sprouting area. As a result, the ratio between the fluorescence found in the sprouting over that found in the spheroid was significantly higher for CD49d+ vs CD49d− granulocytes (Fig. 2i).
These assays suggest that CD49d+ granulocytes support in vitro angiogenesis possibly by physically interacting with endothelial cells. Altogether, antigenic and functional characterisation identified CD49d+ in the polymorphonuclear gate as PAGs.
PAGs in type 2 diabetes
We evaluated whether in vitro endothelial cell tubule formation was differentially affected by the presence of granulocytes isolated from male participants with or without type 2 diabetes. Isolated granulocytes contained PAGs normally distributed in CD16+CD49d+ neutrophils and CD16−CD49d+ eosinophils (ESM Fig. 4). In the presence of granulocytes from diabetic individuals, endothelial cells formed significantly fewer tubules, with a reduced total tubule length (Fig. 3a,b; additional representative images in ESM Fig. 3c). This suggested that granulocytes from diabetic individuals were less able to support angiogenesis. Since the proangiogenic activity of granulocytes was confined to the CD49d+ fraction (Fig. 3), we hypothesised that reduced support of angiogenesis by diabetic granulocytes could be due to a quantitative defect in CD49d+ cells. We thus compared the levels of CD49d+ PAGs in diabetic vs non-diabetic participants (Fig. 3d,e; cohort baseline data in Table 1). The percentage of CD49d+ granulocytes was significantly lower in diabetic than in non-diabetic patients (5.5 ± 0.5% vs 7.6 ± 0.8%; p = 0.021; Fig. 3d). CD49d+ cells were reduced proportionally within the neutrophil and eosinophil populations relative to the total granulocyte gate, but it was statistically significant only within eosinophils (Fig. 3e). CD49d+ PAG levels were also reduced in diabetic vs control participants when expressed in absolute terms, (186 ± 11 vs 239 ± 14 cells/μl; p = 0.046). However, the profoundly impaired tube forming capacity of diabetic granulocytes could only be partially explained by quantitative PAG reduction. Thus, we compared tube forming capacity of endothelial cells incubated with CD49d+ neutrophils or CD49d+ eosinophils freshly isolated from the blood of sex-matched diabetic and non-diabetic participants. Within both neutrophils and eosinophils, diabetic CD49d+ PAGs were unable to increase endothelial cell tube formation (Fig. 3f), suggesting that diabetes induces both quantitative and functional impairment of PAGs.
PAGs in type 2 diabetes. (a, b) Tubule formation (total tubule length and tubule numbers) by endothelial cells co-incubated with granulocytes isolated from patients with (T2D) and without (Ctrl) type 2 diabetes; *p < 0.05. (c) Representative images reconstructed from multiple fields of the tubule formation assay in the two conditions (additional replicates from the same experiment are shown in ESM Fig. 3c). (d) Levels of CD49d+ PAGs in T2D vs Ctrl (*p < 0.05). (e) Levels of CD49d+ expression in T2D vs Ctrl in the eosinophil and neutrophil populations; *p < 0.05. (f) Tubule formation assay by endothelial cells co-incubated with CD49d+ neutrophils or eosinophils freshly sorted from diabetic and non-diabetic patients (*p < 0.05). (g) Levels of CD49d+ PAGs in the entire cohort of T2D and Ctrl participants stratified by the number of metabolic syndrome (MS) components: in addition to confirming significance of the linear tendency, we tested the difference between patients with and without the metabolic syndrome (*p < 0.05). (h) Study participants were also stratified according to the presence or absence of each metabolic syndrome component (Glucose, fasting plasma glucose >5.5 mmol/l; Waist, waist circumference >102 cm for men or >88 cm for women; BP, raised BP; HDL, low HDL-cholesterol; TG, high triacylglycerol); *p < 0.05. Histograms show mean and SEM, while circles indicate individual data points. In (a, b, f) the horizontal dashed lines represent the negative control with unstimulated HUVECs
As expected, type 2 diabetic patients had a higher BMI, lower HDL-cholesterol, and higher prevalence of hypertension than non-diabetic control individuals (Table 1). Upon a multiple regression analysis adjusted for significant differences between the two groups, the inverse association between type 2 diabetes and level of CD49d+ granulocytes remained significant but was attenuated (Table 2). Thus, we hypothesised that part of the reduction in PAGs observed in type 2 diabetes may be attributable to concomitant risk factors that define the metabolic syndrome. Indeed, the level of PAGs progressively and linearly declined with increasing number of metabolic syndrome components (Fig. 3g) and there were significant reductions in the levels of CD49d+ granulocytes with the glucose and blood pressure component of the metabolic syndrome (Fig. 3h).
Since most eosinophils express CD49d and diabetes reduced total CD49d+ granulocytes, a reduction in the total eosinophil population was expected. The total white blood cell count was mildly elevated in type 2 diabetes (ESM Fig. 5a), with an imbalance in the granulocyte-to-lymphocyte ratio (ESM Fig. 5b,c), typical of enhanced myelopoiesis [21]. Data obtained using an automated cell counter showed that diabetic participants had a significant relative increase in neutrophils and no significant difference in eosinophils. Using flow cytometry (ESM Fig. 5d,e), diabetic patients displayed an increase in the percentage of CD16+CD45+ neutrophils and a decrease in CD16−CD45bright eosinophils (which were CCR3+ and SIGLEC8+, Fig. 1f).
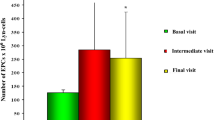
Impact of hyperglycaemia on PAGs
In type 2 diabetes, an inverse correlation was observed between PAG levels and fasting plasma glucose (Fig. 4a) but not HbA1c, which was not surprising in view of the short half-life of human granulocytes (from hours to a few days). To better understand the direct effect of hyperglycaemia on PAGs, we quantified CD49d+ granulocytes in ten type 2 diabetic patients before and after 12 weeks of treatment with the SGLT2 inhibitor dapagliflozin. Clinical characteristics of enrolled patients are shown in ESM Table 2. HbA1c declined from 67 ± 2 mmol/mol (8.3 ± 0.2%) to 56 ± 2 mmol/mol (7.3 ± 0.3%); 8 of 10 patients displayed an increase in their levels of PAGs and the mean cell level significantly increased 1.8-times from baseline to 12 weeks (Fig. 4b). Next, we examined levels of PAGs in 15 patients with type 1 diabetes, and in 15 healthy controls of similar age and sex (ESM Table 3). Similarly to what was observed in patients with type 2 diabetes, type 1 diabetes was also associated with a significant reduction of CD49d+ granulocytes (Fig. 4c). Finally, to address an even cleaner model, we quantified CD49d+ granulocytes in STZ-induced type 1-like diabetic mice vs non-diabetic control mice. This model is characterised by marked hyperglycaemia in the absence of dyslipidaemia (ESM Table 4) and is ideally suitable to evaluate the isolated effects of high glucose. Murine neutrophils and eosinophils were distinguished by expression of Ly6G and SIGLEC-F (Fig. 4d–i), ruling out monocyte contamination by CD115 staining (Fig. 4f,j). As observed in humans, CD49d labelled a small fraction of neutrophils and the majority of eosinophils (Fig. 4f,j). Within both neutrophils (Fig. 4g) and eosinophils (Fig. 4k), CD49d+ cells had higher MFI of VEGFR1 and CXCR4 (Fig. 4l,m), consistent with a proangiogenic capacity. Type 1-like diabetes in mice led to a significant reduction in CD49d expression among both neutrophils and eosinophils, which was significant for eosinophils compared with non-diabetic control mice (Fig. 4n).
Effects of hyperglycaemia on PAGs. (a) Levels of CD49d+ PAGs were correlated with fasting plasma glucose; the regression coefficient r and the corresponding p values are shown. (b) Levels of CD49d+ PAGs were quantified at baseline and after 12 weeks of treatment with the SGLT2 inhibitor (SGLT2i) dapagliflozin. The box shows median and interquartile range, whereas whiskers indicate full range and lines indicate individual patients; *p < 0.05. (c) Levels of CD49d+ PAGs were compared in type 1 diabetic (T1D) participants vs non-diabetic control (Ctrl) participants (*p < 0.05). (d–k) Identification and characterisation of murine PAGs: granulocytes were first gated in the morphologic FSC-A vs SSC-A plot (d) and the resulting population was analysed for expression of the granulocyte marker Ly6G (h); expression of CD49d was analysed on the Ly6G+ neutrophil and Ly6G− eosinophil population (e), both excluding monocytic contamination using CD115 (f, j). Eosinophil identity of Ly6G− granulocytes was confirmed by SIGLEC-F staining (i). Resulting Ly6G+CD49d+ neutrophils (f, g) and Ly6G−CD49d+ eosinophils (j, k) were examined for expression of CXCR4 and VEGFR1, relative to the respective CD49d− controls. (l, m) Quantification of VEGFR1 and CXCR4 MFI, respectively, on CD49d+ vs CD49d− neutrophils and eosinophils (*p < 0.05 vs CD49d−; †p = 0.08 vs CD49d−). (n) Comparison of the levels of total CD49d+ PAGs in diabetic (T1D) mice vs non-diabetic control (Ctrl) mice; *p < 0.05. Histograms show mean and SEM, while circles indicate individual data points. Eo, eosinophils; Neu, neutrophils
Potential mechanisms of CD49d+ cell defect in diabetes
Since a general CD49d downregulation was observed in diabetes and in view of the emerging effect of hyperglycaemia on PAGs, we examined whether exposing granulocytes to high glucose ex vivo resulted in a reduction of CD49d expression. We performed a short-term experiment in high glucose and high-mannitol (osmotic control) because granulocytes are short-lived. Exposure to 20 mmol/l glucose or mannitol for 18 h, compared with the control unstimulated condition, did not significantly modify CD49d expression (ESM Fig. 6), thereby ruling out that high glucose directly reduced CD49d expression on granulocytes.
To explore whether defective generation of CD49d+ cells, most of which are eosinophils, is part of the disturbed myelopoiesis associated with diabetes [21], we analysed gene expression of haematopoietic colonies generated in a previous study before and after CD34+ stem cell mobilisation with plerixafor [20]. Colonies from diabetic participants, compared with control participants, expressed lower levels of the PRG2 gene, which encodes the eosinophil-specific marker major basic protein (ESM Fig. 7).
Discussion
In this study, we describe shortage and dysfunction of circulating PAGs in patients with diabetes, reflecting a diminished activity of granulocytes in support of angiogenesis. Solid data also point to a direct role of hyperglycaemia in the reduction of PAGs observed in diabetic patients.
Proangiogenic neutrophils have been previously described in mice as Ly6G+ neutrophils expressing CD49d and enriched in surface VEGFR1 and CXCR4 [14]. In vivo, expression of VEGFR1 on neutrophils and of VEGFR2 on endothelial cells was required for recruitment of neutrophils to tissues stimulated with VEGF-A [14]. Neutrophil emigration was completely abolished by neutralisation of the adhesion molecule CD49d, suggesting that cell adhesion by CD49d was required for the proangiogenic function. A similar population of CD49d+ neutrophils in the human peripheral blood accounted for ~3.2% of neutrophils [14]. We herein confirmed existence of human CD16+CD49d+ neutrophils, accounting for ~1% of neutrophils, and characterised by high expression of CXCR4 and VEGFR1. Intriguingly, however, based on immune-phenotype, granule content and cytology, most (>80%) CD49d+ granulocytes proved to be eosinophils. Similar to CD49d+ neutrophils, CD49d+ eosinophils also expressed high levels of CXCR4 and VEGFR1. Since CD49d+ eosinophils and neutrophils were equally supportive of endothelial cell tube formation, the proangiogenic activity of CD49d+ granulocytes was not confined to the neutrophil population. Eosinophils have long been implicated in angiogenesis, especially in cancer [22] and in allergic asthma [23, 24]. Thereafter, we focused on the total population of CD49d+ granulocytes, including both eosinophils and neutrophils. Using 2D and 3D angiogenesis assays, we demonstrate the in vitro functional properties of human CD49d+ granulocytes, allowing us to use the term proangiogenic granulocytes (PAGs). Cell-tracking experiments revealed location of CD49d+ granulocytes close to endothelial cells in the tubules and in the sprouts, suggesting that physical interactions between granulocytes and endothelial cells are important in driving the proangiogenic effect. This is in agreement with the role of CD49d in adhesion of leucocytes to the endothelium and is supported by our observation that conditioned medium did not recapitulate the tube-supporting effect of CD49d+ granulocytes.
On the basis of the established notion that diabetes impairs angiogenesis [25], we explored PAGs in diabetic patients. First, we found that granulocytes from type 2 diabetic patients were less able to support in vitro tubule formation by endothelial cells, when compared with granulocytes from non-diabetic control individuals. Since we had noted that CD49d+ granulocytes stimulated tubule formation more than CD49d− granulocytes, we hypothesised that the proangiogenic defect of granulocytes from diabetic individuals could be attributed to reductions in CD49d+ cells. Indeed, levels of PAGs were ~30% lower in type 2 diabetic vs control participants. Quantitative reduction of diabetic PAGs, together with their inability to support endothelial tube formation, explained the profoundly impaired proangiogenic function of diabetic granulocytes.
An inverse correlation was observed between glucose and PAG levels, implying a possible role of glucotoxicity. However, the effects of hyperglycaemia in type 2 diabetes could hardly be dissected from those of concomitant risk factors. Adjusting for variables that differed between the two groups, diabetes remained associated with lower PAGs. To better evaluate the direct impact of hyperglycaemia, we quantified PAGs in a subgroup of type 2 diabetic patients before and after a 12-week therapy with the SGLT2 inhibitor dapagliflozin. Interestingly, glucose control achieved with dapagliflozin was associated with a rise in the levels of PAGs. Since SGLT2 inhibitors exert their glucose-lowering action independently from insulin and exclusively by inducing urinary glucose excretion [26], this setting is ideal to demonstrate the impact of glucotoxicity. In further support of a role for hyperglycaemia in PAG reduction, we found that type 1 diabetic patients without cardiovascular or renal complications had lower levels of PAGs when compared with control individuals of similar age and sex. Finally, we quantified PAG levels in STZ-induced type 1-like diabetic mice, the prototypical murine model of hyperglycaemia. PAGs were significantly lower in diabetic vs non-diabetic control mice. While experimental data suggest that high glucose does not accelerate atherogenesis independently from other risk factors [27], people with type 1 diabetes experience an increased risk of cardiovascular events compared with non-diabetic people [28] and intensive glucose control exerts cardiovascular protection against CVD in type 1 diabetes [29]. Altogether, our results point to a direct role for hyperglycaemia in the reduction of PAGs observed in type 1 and type 2 diabetes, which is, however, not mediated by downregulation of CD49d in high glucose. Pauperisation of CD49d+ granulocytes in diabetic patients was associated with significantly reduced levels of the total immune-defined eosinophil pool. Since hyperglycaemia has been shown to induce myeloid bias [21, 30], we speculated that a reduction of PAGs and eosinophils resulted from a skewed differentiation of haematopoietic precursors. Preliminary results showed an impaired generation of eosinophils from diabetic haematopoietic stem cells. Interestingly, since eosinophils belong to Th2 innate immune function [31], a general imbalance between Th1 (neutrophils and M1 macrophages) and Th2 (eosinophils and M2 macrophages) may mark a disturbed immuno-metabolic crosstalk.
In conclusion, our data add mechanistic information to explain the impairment of angiogenesis in diabetes and broaden the variety of blood cell types involved in diabetic vascular disease. Future studies will enable us to expand our knowledge on the role of PAGs in chronic diabetic vascular complications.
Data availability
Original data are available from the corresponding author at a reasonable request.
Abbreviations
- ACR:
-
Albumin/creatinine ratio
- BM:
-
Bone marrow
- CCR3:
-
C-C motif chemokine receptor 3
- CXCR4:
-
C-X-C chemokine receptor type 4
- EPC:
-
Endothelial progenitor cell
- FSC-A:
-
Forward scatter area
- Ly6G:
-
Lymphocyte antigen 6 complex locus G6D
- MFI:
-
Mean fluorescence intensity
- MPO:
-
Myeloperoxidase
- PAG:
-
Proangiogenic granulocyte
- SGLT2:
-
Sodium–glucose cotransporter 2
- SSC-A:
-
Side scatter area
- SIGLEC:
-
Sialic acid-binding immunoglobulin-type lectin
- STZ:
-
Streptozotocin
- VEGF:
-
Vascular endothelial growth factor
- VEGFR:
-
VEGF receptor
References
Rao Kondapally Seshasai S, Kaptoge S, Thompson A et al (2011) Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med 364(9):829–841. https://doi.org/10.1056/NEJMoa1008862
Fadini GP, Cosentino F (2018) Diabetes and ischaemic stroke: a deadly association. Eur Heart J 39(25):2387–2389. https://doi.org/10.1093/eurheartj/ehy033
Capes SE, Hunt D, Malmberg K, Gerstein HC (2000) Stress hyperglycaemia and increased risk of death after myocardial infarction in patients with and without diabetes: a systematic overview. Lancet 355(9206):773–778. https://doi.org/10.1016/S0140-6736(99)08415-9
Aguilar D, Solomon SD, Kober L et al (2004) Newly diagnosed and previously known diabetes mellitus and 1-year outcomes of acute myocardial infarction: the VALsartan In Acute myocardial iNfarcTion (VALIANT) trial. Circulation 110(12):1572–1578. https://doi.org/10.1161/01.CIR.0000142047.28024.F2
Fadini GP, Spinetti G, Santopaolo M, Madeddu P (2019) Impaired regeneration contributes to poor outcomes in diabetic peripheral artery disease. Arterioscler Thromb Vasc Biol 40(1):34–44
Fadini GP, Albiero M, Bonora BM, Avogaro A (2019) Angiogenic abnormalities in diabetes mellitus: mechanistic and clinical aspects. J Clin Endocrinol Metab 104(11):5431–5444. https://doi.org/10.1210/jc.2019-00980
Howangyin KY, Silvestre JS (2014) Diabetes mellitus and ischemic diseases: molecular mechanisms of vascular repair dysfunction. Arterioscler Thromb Vasc Biol 34(6):1126–1135. https://doi.org/10.1161/ATVBAHA.114.303090
Fadini GP, Rigato M, Cappellari R, Bonora BM, Avogaro A (2017) Long-term prediction of cardiovascular outcomes by circulating CD34+ and CD34+CD133+ stem cells in patients with type 2 diabetes. Diabetes Care 40(1):125–131. https://doi.org/10.2337/dc16-1755
Fadini GP, Ciciliot S, Albiero M (2017) Concise review: perspectives and clinical implications of bone marrow and circulating stem cell defects in diabetes. Stem Cells 35(1):106–116. https://doi.org/10.1002/stem.2445
Fadini GP, de Kreutzenberg SV, Boscaro E et al (2013) An unbalanced monocyte polarisation in peripheral blood and bone marrow of patients with type 2 diabetes has an impact on microangiopathy. Diabetologia 56(8):1856–1866. https://doi.org/10.1007/s00125-013-2918-9
Jetten N, Verbruggen S, Gijbels MJ, Post MJ, De Winther MP, Donners MM (2014) Anti-inflammatory M2, but not pro-inflammatory M1 macrophages promote angiogenesis in vivo. Angiogenesis 17(1):109–118. https://doi.org/10.1007/s10456-013-9381-6
Nozawa H, Chiu C, Hanahan D (2006) Infiltrating neutrophils mediate the initial angiogenic switch in a mouse model of multistage carcinogenesis. Proc Natl Acad Sci U S A 103(33):12493–12498. https://doi.org/10.1073/pnas.0601807103
Gaudry M, Bregerie O, Andrieu V, El Benna J, Pocidalo MA, Hakim J (1997) Intracellular pool of vascular endothelial growth factor in human neutrophils. Blood 90(10):4153–4161
Massena S, Christoffersson G, Vagesjo E et al (2015) Identification and characterization of VEGF-A-responsive neutrophils expressing CD49d, VEGFR1, and CXCR4 in mice and humans. Blood 126(17):2016–2026. https://doi.org/10.1182/blood-2015-03-631572
Friedewald WT, Levy RI, Fredrickson DS (1972) Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 18(6):499–502
Early Treatment Diabetic Retinopathy Study Research Group (1991) Grading diabetic retinopathy from stereoscopic color fundus photographs--an extension of the modified Airlie House classification. ETDRS report number 10. Ophthalmology 98:786–806
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612. https://doi.org/10.7326/0003-4819-150-9-200905050-00006
Ardern CI, Katzmarzyk PT, Janssen I, Church TS, Blair SN (2005) Revised adult treatment panel III guidelines and cardiovascular disease mortality in men attending a preventive medical clinic. Circulation 112(10):1478–1485. https://doi.org/10.1161/CIRCULATIONAHA.105.548198
Ethier C, Lacy P, Davoine F (2014) Identification of human eosinophils in whole blood by flow cytometry. Methods Mol Biol 1178:81–92. https://doi.org/10.1007/978-1-4939-1016-8_8
Fadini GP, Fiala M, Cappellari R et al (2015) Diabetes limits stem cell mobilization following G-CSF but not plerixafor. Diabetes 64(8):2969–2977. https://doi.org/10.2337/db15-0077
Albiero M, Ciciliot S, Tedesco S et al (2019) Diabetes-associated myelopoiesis drives stem cell mobilopathy through an OSM-p66Shc signaling pathway. Diabetes 68(6):1303–1314. https://doi.org/10.2337/db19-0080
De Palma M, Biziato D, Petrova TV (2017) Microenvironmental regulation of tumour angiogenesis. Nat Rev Cancer 17(8):457–474. https://doi.org/10.1038/nrc.2017.51
Asosingh K, Vasanji A, Tipton A et al (2016) Eotaxin-rich proangiogenic hematopoietic progenitor cells and CCR3+ endothelium in the atopic asthmatic response. J Immunol 196(5):2377–2387. https://doi.org/10.4049/jimmunol.1500770
Puxeddu I, Ribatti D, Crivellato E, Levi-Schaffer F (2005) Mast cells and eosinophils: a novel link between inflammation and angiogenesis in allergic diseases. J Allergy Clin Immunol 116(3):531–536. https://doi.org/10.1016/j.jaci.2005.06.007
Martin A, Komada MR, Sane DC (2003) Abnormal angiogenesis in diabetes mellitus. Med Res Rev 23(2):117–145. https://doi.org/10.1002/med.10024
Ferrannini E, Muscelli E, Frascerra S et al (2014) Metabolic response to sodium-glucose cotransporter 2 inhibition in type 2 diabetic patients. J Clin Invest 124(2):499–508. https://doi.org/10.1172/JCI72227
Al-Mashhadi RH, Bjorklund MM, Mortensen MB et al (2015) Diabetes with poor glycaemic control does not promote atherosclerosis in genetically modified hypercholesterolaemic minipigs. Diabetologia 58(8):1926–1936. https://doi.org/10.1007/s00125-015-3637-1
Soedamah-Muthu SS, Fuller JH, Mulnier HE, Raleigh VS, Lawrenson RA, Colhoun HM (2006) High risk of cardiovascular disease in patients with type 1 diabetes in the U.K.: a cohort study using the general practice research database. Diabetes Care 29(4):798–804. https://doi.org/10.2337/diacare.29.04.06.dc05-1433
Nathan DM, Cleary PA, Backlund JY et al (2005) Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med 353(25):2643–2653. https://doi.org/10.1056/NEJMoa052187
Nagareddy PR, Murphy AJ, Stirzaker RA et al (2013) Hyperglycemia promotes myelopoiesis and impairs the resolution of atherosclerosis. Cell Metab 17(5):695–708. https://doi.org/10.1016/j.cmet.2013.04.001
Wynn TA (2015) Type 2 cytokines: mechanisms and therapeutic strategies. Nat Rev Immunol 15(5):271–282. https://doi.org/10.1038/nri3831
Funding
The study was supported by grants from: the Italian Ministry of University and Education to GPF (PRIN 2015ZTT5KB); the European Foundation for the Study of Diabetes (EFSD) / Lilly 2016 grant to GPF; the Italian Diabetes Society / Lilly 2017 grant to GPF; the Italian Ministry of Health (RF-2013-02358024) to MA. The study funders were not involved in the design of the study; the collection, analysis, and interpretation of data; writing the report; and did not impose any restrictions regarding the publication of the report.
Author information
Authors and Affiliations
Contributions
RC, MDA, MA, AA and GPF designed the study, RC, MDA, LM, BMB, MA acquired the data, RC, MDA, LM and GPF drafted the manuscript. BMB, MA and AA revised the manuscript. All authors approved the final version of the manuscript. GPF is the guarantor of this work.
Corresponding author
Ethics declarations
The authors declare that there are no relationships or activities that might bias, or be perceived to bias, their work.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM
(PDF 764 kb)
Rights and permissions
About this article
Cite this article
Cappellari, R., D’Anna, M., Menegazzo, L. et al. Diabetes mellitus impairs circulating proangiogenic granulocytes. Diabetologia 63, 1872–1884 (2020). https://doi.org/10.1007/s00125-020-05142-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-020-05142-3