Collection
Equity and Diversity in Palliative Care
- Submission status
- Closed
Editors
-
Jonathan Koffman: Hull York Medical School, United Kingdom
Jonathan Koffman, BA (Hons), MSc, Ph.D., is a medical sociologist who has conducted studies examining social inequity and palliative care experiences and outcomes for over 20 years. Recent world events, including the Empire Windrush scandal, Black Lives Matter, and COVID-19 pandemic, with their disproportionate impact on those from minoritized communities and low socioeconomic positions, have radically changed his views on the experience of those dying in the margins, questioning previous research on the manner in which study questions have been constructed, methods chosen to address those questions, and the way findings have been reported.
-
Christian Schulz-Quach: Princess Margaret Cancer Centre, Canada
Dr. Christian Schulz-Quach, MD, MSc, MA, MRCPSych, is a staff psychiatrist at the Department of Supportive Care, Princess Margaret Cancer Centre, University Health Network, Toronto, Canada. He is a Clinician Educator and Assistant Professor at the Department of Psychiatry at the University of Toronto, Canada, and a board-certified Psychiatrist and Psychotherapist with work experience in Germany, UK, US, and Canada. He has specialty training in Psychosomatic Medicine, Medical Psychotherapy, and Palliative Medicine and is a candidate at the Toronto Institute for Contemporary Psychoanalysis. His special interest is Existential Psychoanalysis.
-
Gilla Shapiro: Princess Margaret Cancer Centre, Canada
Gilla Shapiro, MA (Cantab), MPP/MPA, Ph.D., is a Psychologist and Clinician-Scientist in the Department of Supportive Care at the Princess Margaret Cancer Centre in Toronto. Gilla completed her Ph.D. in clinical psychology at McGill University and her dual-degree MPA/MPP at the London School of Economics and Political Science and the Hertie School of Governance. Gilla’s clinical and research interests include psychosocial oncology, palliative care, health behavior, the social determinants of health, health equity, and policy analysis.
Articles (10 in this collection)
-
-
Patshitinikutau Natukunisha Tshishennuat Uitshuau (a place for Elders to spend their last days in life): a qualitative study about Innu perspectives on end-of-life care
Authors (first, second and last of 11)
- Russell Dawe
- Jack Penashue
- Nathaniel Pollock
- Content type: Research
- Open Access
- Published: 17 May 2024
- Article: 121

-
Measuring palliative care integration in Malawi through service provision, access, and training indicators: the Waterloo Coalition Initiative
Authors (first, second and last of 9)
- Fatia Kiyange
- Mackuline Atieno
- William E. Rosa
- Content type: Research
- Open Access
- Published: 16 January 2024
- Article: 17

-
“You can’t die here”: an exploration of the barriers to dying-in-place for structurally vulnerable populations in an urban centre in British Columbia, Canada
Authors (first, second and last of 9)
- Kelli I. Stajduhar
- Melissa Giesbrecht
- Simon Colgan
- Content type: Research
- Open Access
- Published: 10 January 2024
- Article: 12
-
Increasing access to palliative care for patients with advanced cancer of African and Latin American descent: a patient-oriented community-based study protocol
Authors (first, second and last of 20)
- Anna Santos Salas
- Sharon M. Watanabe
- the Patient Advisory Council
- Content type: Study Protocol
- Open Access
- Published: 20 December 2023
- Article: 204
-
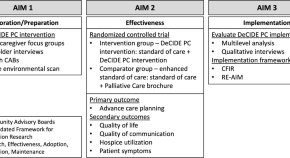
Dissemination and Implementation of a Community Health Worker Intervention for Disparities in Palliative Care (DeCIDE PC): a study protocol for a hybrid type 1 randomized controlled trial
Authors (first, second and last of 15)
- Amn Siddiqi
- Olivia Monton
- Fabian M. Johnston
- Content type: Study Protocol
- Open Access
- Published: 18 September 2023
- Article: 139
-
Participatory development of a manual for the implementation of diversity-sensitive palliative and hospice care in Germany: a mixed-methods study protocol
Authors
- Fabian Erdsiek
- Yüce Yılmaz-Aslan
- Patrick Brzoska
- Content type: Study Protocol
- Open Access
- Published: 05 September 2023
- Article: 128

-
Comparison of home-based palliative care delivered by community health workers versus usual care: research protocol for a pilot randomized controlled trial
Authors (first, second and last of 8)
- Suparna Qanungo
- Kathleen B. Cartmell
- Gaurav Kumar
- Content type: Study Protocol
- Open Access
- Published: 02 September 2023
- Article: 125

-
A qualitative exploration of allied health providers’ perspectives on cultural humility in palliative and end-of-life care
Authors (first, second and last of 7)
- Hardeep Singh
- Arta Taghavi Haghayegh
- Ruheena Sangrar
- Content type: Research
- Open Access
- Published: 12 July 2023
- Article: 92
-
Enhancing equity and diversity in palliative care clinical practice, research and education
Authors
- Jonathan Koffman
- Gilla K. Shapiro
- Christian Schulz-Quach
- Content type: Editorial
- Open Access
- Published: 05 June 2023
- Article: 64





