Abstract
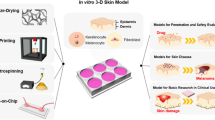
In the last few decades, skin bioengineering has undergone several advancements. The need, understanding, and importance of develo** artificial skin, i.e. in vitro human skin models (HSMs) such as static and dynamic perfusion-based skin-on-chip (SOC) models for studying the effect of cosmetics, skin diseases, and drug discovery, have started budding in recent years. SOCs are shown to be more realistic, high throughput, and less expensive alternatives to animal models for pre-clinical testing. Thus, fabrication, development, characterization, and validation of various in vitro HSMs like SOC came into the subject of skin tissue engineering, regenerative medicine, and diagnostics. The ideology of SOC proves the basic principle of 3Rs, i.e. replace, reduce, and refine (RRR). It satisfies the morphological, biomechanical, and functional resemblance to human skin. It has been validated by applications of cosmetics and pharmaceutical products, significantly demonstrating its efficacy, delivery, and toxicity. In this book chapter, all the mentioned parameters are discussed sequentially. An outlook on SOC impact, regulations, IPR followed by challenges, and current and future perspectives is also presented in the later section of this chapter.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Abaci HE, Guo Z, Doucet Y, Jacków J, Christiano A (2017) Next generation human skin constructs as advanced tools for drug development. Exp Biol Med (Maywood) 242(17):1657–1668. https://doi.org/10.1177/1535370217712690
Effects of air pollution on the skin: a review. Indian J Dermatol Venereol Leprol. June 30, 2017. https://ijdvl.com/effects-of-air-pollution-on-the-skin-a-review/. Accessed 31 Oct 2021
Svobodová A, Vostálová J (2010) Solar radiation induced skin damage: review of protective and preventive options. Int J Radiat Biol 86(12):999–1030. https://doi.org/10.3109/09553002.2010.501842
Karimkhani C et al (2017) Global skin disease morbidity and mortality. JAMA Dermatol 153(5):406–412. https://doi.org/10.1001/jamadermatol.2016.5538
Karimkhani C et al (2017) Global skin disease morbidity and mortality: an update from the global burden of disease study 2013. JAMA Dermatol 153(5):406–412. https://doi.org/10.1001/jamadermatol.2016.5538
Prausnitz MR, Langer R (2008) Transdermal drug delivery. Nat Biotechnol 26(11):11. https://doi.org/10.1038/nbt.1504
Eungdamrong NJ et al (2014) Challenges and promises in modeling dermatologic disorders with bioengineered skin. Exp Biol Med (Maywood) 239(9):1215–1224. https://doi.org/10.1177/1535370214538747
Yun Y, Jung YJ, Choi Y, Choi JS, Cho YW (2018) Artificial skin models for animal-free testing. J Pharm Investig 48. https://doi.org/10.1007/s40005-018-0389-1
Zhang Q, Sito L, Mao M, He J, Zhang YS, Zhao X (2018) Current advances in skin-on-a-chip models for drug testing. Microphysiol Syst 2. https://doi.org/10.21037/mps.2018.08.01
Esch MB, King TL, Shuler ML (2011) The role of body-on-a-chip devices in drug and toxicity studies. Annu Rev Biomed Eng 13(1):55–72. https://doi.org/10.1146/annurev-bioeng-071910-124629
Esch EW, Bahinski A, Huh D (2015) Organs-on-chips at the frontiers of drug discovery. Nat Rev Drug Discov 14(4):248–260. https://doi.org/10.1038/nrd4539
Ferdowsian HR, Beck N (2011) Ethical and scientific considerations regarding animal testing and research. PLoS One. https://doi.org/10.1371/journal.pone.0024059
Von Aulock S (2019) Is there an end in sight for animal testing? Can organ-on-a-chip replace animal use in safety testing with advanced human-focused approaches? ALTEX. https://doi.org/10.14573/altex.1812121
Lilienblum W et al (2008) Alternative methods to safety studies in experimental animals: role in the risk assessment of chemicals under the new European Chemicals Legislation (REACH). Arch Toxicol. https://doi.org/10.1007/s00204-008-0279-9
Almeida A, Sarmento B, Rodrigues F (2017) Insights on in vitro models for safety and toxicity assessment of cosmetic ingredients. Int J Pharm. https://doi.org/10.1016/j.ijpharm.2017.01.024
Hewitt NJ et al (2013) Use of human in vitro skin models for accurate and ethical risk assessment: metabolic considerations. Toxicol Sci. https://doi.org/10.1093/toxsci/kft080
Astashkina A, Grainger DW (2014) Critical analysis of 3-D organoid in vitro cell culture models for high-throughput drug candidate toxicity assessments. Adv Drug Deliv Rev. https://doi.org/10.1016/j.addr.2014.02.008
Bhatia SN, Ingber DE (2014) Microfluidic organs-on-chips. Nat Biotechnol 32(8):760–772. https://doi.org/10.1038/nbt.2989
Mohammadi MH et al (2016) Skin diseases modeling using combined tissue engineering and microfluidic technologies. Adv Healthc Mater 5(19):2459–2480. https://doi.org/10.1002/adhm.201600439
Abaci HE, Gledhill K, Guo Z, Christiano AM, Shuler ML (2015) Pumpless microfluidic platform for drug testing on human skin equivalents. Lab Chip 15(3):882–888. https://doi.org/10.1039/c4lc00999a
Sriram G et al (2018) Full-thickness human skin-on-chip with enhanced epidermal morphogenesis and barrier function. Mater Today 21(4):326–340. https://doi.org/10.1016/j.mattod.2017.11.002
Zhang YS et al (2017) Multisensor-integrated organs-on-chips platform for automated and continual in situ monitoring of organoid behaviors. Proc Natl Acad Sci U S A. https://doi.org/10.1073/pnas.1612906114
Kilic T, Navaee F, Stradolini F, Renaud P, Carrara S (2018) Organs-on-chip monitoring: sensors and other strategies. Microphysiol Syst. https://doi.org/10.21037/mps.2018.01.01
Seok J et al (2013) Genomic responses in mouse models poorly mimic human inflammatory diseases. Proc Natl Acad Sci U S A. https://doi.org/10.1073/pnas.1222878110
Mak IWY, Evaniew N, Ghert M (2014) Lost in translation: animal models and clinical trials in cancer treatment. Am J Transl Res 6:114–118
Wufuer M et al (2016) Skin-on-a-chip model simulating inflammation, edema and drug-based treatment. Sci Rep 6(August):1–12. https://doi.org/10.1038/srep37471
Ramadan Q, Ting FCW (2016) In vitro micro-physiological immune-competent model of the human skin. Lab Chip. https://doi.org/10.1039/c6lc00229c
Ghaemmaghami AM, Hancock MJ, Harrington H, Kaji H, Khademhosseini A (2012) Biomimetic tissues on a chip for drug discovery. Drug Discov Today 17(3–4):173–181. https://doi.org/10.1016/j.drudis.2011.10.029
Pati F, Gantelius J, Svahn HA (2016) 3D bioprinting of tissue/organ models. Angew Chem Int Ed 55(15):4650–4665. https://doi.org/10.1002/anie.201505062
Au AK, Lee W, Folch A (2014) Mail-order microfluidics: evaluation of stereolithography for the production of microfluidic devices. Lab Chip 14(7):1294–1301. https://doi.org/10.1039/C3LC51360B
Selimović S, Dokmeci MR, Khademhosseini A (2013) Organs-on-a-chip for drug discovery. Curr Opin Pharmacol 13(5):829–833. https://doi.org/10.1016/j.coph.2013.06.005
Zheng F, Fu F, Cheng Y, Wang C, Zhao Y, Gu Z (2016) Organ-on-a-chip systems: microengineering to biomimic living systems. Small 12(17):2253–2282. https://doi.org/10.1002/smll.201503208
Organs-on-chip monitoring: sensors and other strategies - Kilic - Microphysiological Systems. https://mps.amegroups.com/article/view/4689/5479. Accessed 20 June 2021
Schulz JT III, Tompkins RG, Burke JF (2000) Artificial skin. Annu Rev Med 51(1):231–244. https://doi.org/10.1146/annurev.med.51.1.231
Sorrell JM, Caterson B, Caplan AI, Davis B, Schafer IA (1990) Human keratinocytes contain carbohydrates that are recognized by keratan sulfate-specific monoclonal antibodies. J Invest Dermatol 95(3):347–352. https://doi.org/10.1111/1523-1747.ep12485110
Vijayavenkataraman S, Lu WF, Fuh JYH (2016) 3D bioprinting of skin: a state-of-the-art review on modelling, materials, and processes. Biofabrication 8(3):032001. https://doi.org/10.1088/1758-5090/8/3/032001
Elsevier Enhanced Reader. https://doi.org/10.1016/j.bbamem.2006.06.021. https://reader.elsevier.com/reader/sd/pii/S0005273606002410?token=C6DA4EC4BF5B7A11B86ACF3128CA110E6258177FD1ADC7578F27243DEFF07B0FC40E0EF30B9F2266E3B8AE9CB8C9BF4A&originRegion=eu-west-1&originCreation=20210722094219. Accessed 22 July 2021
Lin JY, Fisher DE (2007) Melanocyte biology and skin pigmentation. Nature 445(7130):843–850. https://doi.org/10.1038/nature05660
Choi H-I et al (2014) Melanosome uptake is associated with the proliferation and differentiation of keratinocytes. Arch Dermatol Res 306(1):59–66. https://doi.org/10.1007/s00403-013-1422-x
Doebel T, Voisin B, Nagao K (2017) Langerhans cells – the macrophage in dendritic cell clothing. Trends Immunol 38(11):817–828. https://doi.org/10.1016/j.it.2017.06.008
Lumpkin EA, Caterina MJ (2007) Mechanisms of sensory transduction in the skin. Nature 445(7130):858–865. https://doi.org/10.1038/nature05662
Woo S-H, Lumpkin EA, Patapoutian A (2015) Merkel cells and neurons keep in touch. Trends Cell Biol 25(2):74–81. https://doi.org/10.1016/j.tcb.2014.10.003
Pereira RF, Barrias CC, Granja PL, Bartolo PJ (2013) Advanced biofabrication strategies for skin regeneration and repair. Nanomedicine (Lond) 8(4):603–621. https://doi.org/10.2217/nnm.13.50
Dias J, Granja P, Bártolo P (2016) Advances in electrospun skin substitutes. Prog Mater Sci 84:314–334. https://doi.org/10.1016/j.pmatsci.2016.09.006
Planz V, Lehr C-M, Windbergs M (2016) In vitro models for evaluating safety and efficacy of novel technologies for skin drug delivery. J Control Release 242:89–104. https://doi.org/10.1016/j.jconrel.2016.09.002
Kahan V, Andersen ML, Tomimori J, Tufik S (2009) Stress, immunity and skin collagen integrity: evidence from animal models and clinical conditions. Brain Behav Immun 23(8):1089–1095. https://doi.org/10.1016/j.bbi.2009.06.002
Casey G (2002) Physiology of the skin. Nurs Stand 16(34):47–51.; quiz 53, 55. https://doi.org/10.7748/ns2002.05.16.34.47.c3193
Papakonstantinou E, Roth M, Karakiulakis G (2012) Hyaluronic acid: a key molecule in skin aging. Dermatoendocrinology 4(3):253–258. https://doi.org/10.4161/derm.21923
Freundlich B, Bomalaski JS, Neilson E, Jimenez SA (1986) Regulation of fibroblast proliferation and collagen synthesis by cytokines. Immunol Today 7(10):303–307. https://doi.org/10.1016/0167-5699(86)90067-8
Krishnaswamy G, Ajitawi O, Chi DS (2006) The human mast cell: an overview. Methods Mol Biol 315:13–34. https://doi.org/10.1385/1-59259-967-2:013
Lai-Cheong JE, McGrath JA (2017) Structure and function of skin, hair and nails. Medicine 45(6):347–351. https://doi.org/10.1016/j.mpmed.2017.03.004
Lee S, ** SP, Kim YK, Sung GY, Chung JH, Sung JH (2017) Construction of 3D multicellular microfluidic chip for an in vitro skin model. Biomed Microdevices. https://doi.org/10.1007/s10544-017-0156-5
Nishimura SI, Ueda M, Sasai M (2009) Cortical factor feedback model for cellular locomotion and cytofission. PLoS Comput Biol. https://doi.org/10.1371/journal.pcbi.1000310
Liang CC, Park AY, Guan JL (2007) In vitro scratch assay: a convenient and inexpensive method for analysis of cell migration in vitro. Nat Protoc. https://doi.org/10.1038/nprot.2007.30
Vedel S, Tay S, Johnston DM, Bruus H, Quake SR (2013) Migration of cells in a social context. Proc Natl Acad Sci U S A. https://doi.org/10.1073/pnas.1204291110
Polini A, Prodanov L, Bhise NS, Manoharan V, Dokmeci MR, Khademhosseini A (2014) Organs-on-a-chip: a new tool for drug discovery. Expert Opin Drug Discovery 9(4):335–352. https://doi.org/10.1517/17460441.2014.886562
van den Broek LJ, Bergers LIJC, Reijnders CMA, Gibbs S (2017) Progress and future prospectives in skin-on-chip development with emphasis on the use of different cell types and technical challenges. Stem Cell Rev Rep 13(3):418–429. https://doi.org/10.1007/s12015-017-9737-1
Duval K et al (2017) Modeling physiological events in 2D vs. 3D Cell Culture. Physiology (Bethesda) 32(4):266–277. https://doi.org/10.1152/physiol.00036.2016
Hinz B, Gabbiani G (2003) Cell-matrix and cell-cell contacts of myofibroblasts: role in connective tissue remodeling. Thromb Haemost 90(12):993–1002. https://doi.org/10.1160/TH03-05-0328
Bhatia SN, Ingber DE (2014) Microfluidic organs-on-chips. Nat Biotechnol 32(8):8. https://doi.org/10.1038/nbt.2989
Parmaksiz M, Dogan A, Odabas S, Elçin AE, Elçin YM (2016) Clinical applications of decellularized extracellular matrices for tissue engineering and regenerative medicine. Biomed Mater 11(2):022003. https://doi.org/10.1088/1748-6041/11/2/022003
Smola H, Thiekötter G, Fusenig NE (1993) Mutual induction of growth factor gene expression by epidermal-dermal cell interaction. J Cell Biol 122(2):417–429. https://doi.org/10.1083/jcb.122.2.417
Schmidt BA, Horsley V (2013) Intradermal adipocytes mediate fibroblast recruitment during skin wound healing. Development 140(7):1517–1527. https://doi.org/10.1242/dev.087593
Nie J et al (2018) Vessel-on-a-chip with hydrogel-based microfluidics. Small 14(45):e1802368. https://doi.org/10.1002/smll.201802368
Kim BS, Lee J-S, Gao G, Cho D-W (2017) Direct 3D cell-printing of human skin with functional transwell system. Biofabrication 9(2):025034. https://doi.org/10.1088/1758-5090/aa71c8
Sano E et al (2019) Tetrafluoroethylene-propylene elastomer for fabrication of microfluidic organs-on-chips resistant to drug absorption. Micromachines 10(11):11. https://doi.org/10.3390/mi10110793
Fentem JH, Botham PA (2002) ECVAM’s activities in validating alternative tests for skin corrosion and irritation. https://journals.sagepub.com/doi/abs/10.1177/026119290203002S09. Accessed 08 July 2021
Pellevoisin C et al (2018) SkinEthic™ RHE for in vitro evaluation of skin irritation of medical device extracts. Toxicol In Vitro 50:418–425. https://doi.org/10.1016/j.tiv.2018.01.008
Asbill C, Kim N, El-Kattan A, Creek K, Wertz P, Michniak B (2000) Evaluation of a human bio-engineered skin equivalent for drug permeation studies. Pharm Res 17(9):1092–1097. https://doi.org/10.1023/a:1026405712870
Ouwehand K, Spiekstra SW, Waaijman T, Scheper RJ, de Gruijl TD, Gibbs S (2011) Technical advance: Langerhans cells derived from a human cell line in a full-thickness skin equivalent undergo allergen-induced maturation and migration. J Leukoc Biol 90(5):1027–1033. https://doi.org/10.1189/jlb.0610374
Tremblay P-L, Berthod F, Germain L, Auger FA (2005) In vitro evaluation of the angiostatic potential of drugs using an endothelialized tissue-engineered connective tissue. J Pharmacol Exp Ther 315(2):510–516
Characterization of a human skin equivalent model to study the effects of ultraviolet B radiation on keratinocytes. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4074762/. Accessed 08 July 2021
Portes P, Pygmalion MJ, Popovic E, Cottin M, Mariani M (2002) Use of human reconstituted epidermis Episkin for assessment of weak phototoxic potential of chemical compounds. Photodermatol Photoimmunol Photomed 18(2):96–102. https://doi.org/10.1034/j.1600-0781.2002.180207.x
Dreher F, Fouchard F, Patouillet C, Andrian M, Simonnet J-T, Benech-Kieffer F (2002) Comparison of cutaneous bioavailability of cosmetic preparations containing caffeine or alpha-tocopherol applied on human skin models or human skin ex vivo at finite doses. Skin Pharmacol Appl Ski Physiol 15(Suppl 1):40–58. https://doi.org/10.1159/000066680
Dreher F et al (2002) Improvement of the experimental setup to assess cutaneous bioavailability on human skin models: dynamic protocol. Skin Pharmacol Appl Ski Physiol 15(Suppl 1):31–39. https://doi.org/10.1159/000066683
Gibbs S, Vietsch H, Meier U, Ponec M (2002) Effect of skin barrier competence on SLS and water-induced IL-1alpha expression. Exp Dermatol 11(3):217–223. https://doi.org/10.1034/j.1600-0625.2001.110304.x
Schmook FP, Meingassner JG, Billich A (2001) Comparison of human skin or epidermis models with human and animal skin in in-vitro percutaneous absorption. Int J Pharm 215(1):51–56. https://doi.org/10.1016/S0378-5173(00)00665-7
Guth K, Schäfer-Korting M, Fabian E, Landsiedel R, van Ravenzwaay B (2015) Suitability of skin integrity tests for dermal absorption studies in vitro. Toxicol In Vitro 29(1):113–123. https://doi.org/10.1016/j.tiv.2014.09.007
Groeber F, Holeiter M, Hampel M, Hinderer S, Schenke-Layland K (2011) Skin tissue engineering--in vivo and in vitro applications. Adv Drug Deliv Rev 63(4–5):352–366. https://doi.org/10.1016/j.addr.2011.01.005
Werner S, Krieg T, Smola H (2007) Keratinocyte–fibroblast interactions in wound healing. J Investig Dermatol 127(5):998–1008. https://doi.org/10.1038/sj.jid.5700786
Schumacher M et al (2014) Efficient keratinocyte differentiation strictly depends on JNK-induced soluble factors in fibroblasts. J Invest Dermatol 134(5):1332–1341. https://doi.org/10.1038/jid.2013.535
Catarino CM et al (2018) Skin corrosion test: a comparison between reconstructed human epidermis and full thickness skin models. Eur J Pharm Biopharm 125:51–57. https://doi.org/10.1016/j.ejpb.2018.01.002
Thakoersing VS, Ponec M, Bouwstra JA (2010) Generation of human skin equivalents under submerged conditions—mimicking the in utero environment. Tissue Eng A 16(4):1433–1441. https://doi.org/10.1089/ten.tea.2009.0358
Mallampati R et al (2010) Evaluation of EpiDerm full thickness-300 (EFT-300) as an in vitro model for skin irritation: Studies on aliphatic hydrocarbons. Toxicol In Vitro 24(2):669–676. https://doi.org/10.1016/j.tiv.2009.08.019
Heisler E, Hoffmann JJ, Peters P, Ahr HJ, Vohr H-W (2003) 155 Advanced skin test 2000 (AST-2000) as a potent in vitro tool for the characterization of skin reactions by protein fingerprinting. Toxicol Lett 144:s44–s45. https://doi.org/10.1016/S0378-4274(03)90154-8
Rasmussen C et al (2010) The StrataTest® human skin model, a consistent in vitro alternative for toxicological testing. Toxicol In Vitro 24:2021–2029. https://doi.org/10.1016/j.tiv.2010.07.027
Kumar R, Parsad D, Kanwar A, Kaul D (2012) Development of melanocye-keratinocyte co-culture model for controls and vitiligo to assess regulators of pigmentation and melanocytes. Indian J Dermatol Venereol Leprol 78(5):599–604. https://doi.org/10.4103/0378-6323.100567
Kosten IJ, Spiekstra SW, de Gruijl TD, Gibbs S (2015) MUTZ-3 derived Langerhans cells in human skin equivalents show differential migration and phenotypic plasticity after allergen or irritant exposure. Toxicol Appl Pharmacol 287(1):35–42. https://doi.org/10.1016/j.taap.2015.05.017
Chau DYS, Johnson C, MacNeil S, Haycock JW, Ghaemmaghami AM (2013) The development of a 3D immunocompetent model of human skin. Biofabrication 5(3):035011. https://doi.org/10.1088/1758-5082/5/3/035011
van den Bogaard EH et al (2014) Crosstalk between keratinocytes and T cells in a 3D microenvironment: a model to study inflammatory skin diseases. J Investig Dermatol 134(3):719–727. https://doi.org/10.1038/jid.2013.417
Monfort A, Soriano-Navarro M, García-Verdugo JM, Izeta A (2013) Production of human tissue-engineered skin trilayer on a plasma-based hypodermis. J Tissue Eng Regen Med 7(6):479–490. https://doi.org/10.1002/term.548
Trottier V, Marceau-Fortier G, Germain L, Vincent C, Fradette J (2008) IFATS collection: using human adipose-derived stem/stromal cells for the production of new skin substitutes. Stem Cells 26(10):2713–2723. https://doi.org/10.1634/stemcells.2008-0031
Abaci HE et al (2016) Human skin constructs with spatially controlled vasculature using primary and iPSC-derived endothelial cells. Adv Healthc Mater 5(14):1800–1807. https://doi.org/10.1002/adhm.201500936
Wufuer M et al (2016) Skin-on-a-chip model simulating inflammation, edema and drug-based treatment. Sci Rep 6(1):37471. https://doi.org/10.1038/srep37471
Dhanwada KR, Garrett L, Smith P, Thompson KD, Doster A, Jones C (1993) Characterization of human keratinocytes transformed by high risk human papillomavirus types 16 or 18 and herpes simplex virus type 2. J Gen Virol 74(Pt 6):955–963. https://doi.org/10.1099/0022-1317-74-6-955
Schoop VM, Mirancea N, Fusenig NE (1999) Epidermal organization and differentiation of HaCaT keratinocytes in organotypic coculture with human dermal fibroblasts. J Invest Dermatol 112(3):343–353. https://doi.org/10.1046/j.1523-1747.1999.00524.x
Reijnders CMA, van Lier A, Roffel S, Kramer D, Scheper RJ, Gibbs S (2015) Development of a full-thickness human skin equivalent in vitro model derived from TERT-immortalized keratinocytes and fibroblasts. Tissue Eng Part A 21(17–18):2448–2459. https://doi.org/10.1089/ten.TEA.2015.0139
Okugawa Y, Hirai Y (2008) Overexpression of extracellular epimorphin leads to impaired epidermal differentiation in HaCaT keratinocytes. J Invest Dermatol 128(8):1884–1893. https://doi.org/10.1038/jid.2008.22
Ataç B et al (2013) Skin and hair on-a-chip: in vitro skin models versus ex vivo tissue maintenance with dynamic perfusion. Lab Chip 13(18):3555. https://doi.org/10.1039/c3lc50227a
Mori N, Morimoto Y, Takeuchi S (2017) Skin integrated with perfusable vascular channels on a chip. Biomaterials 116:48–56. https://doi.org/10.1016/j.biomaterials.2016.11.031
Sandby-Møller J, Poulsen T, Wulf HC (2003) Epidermal thickness at different body sites: relationship to age, gender, pigmentation, blood content, skin type and smoking habits. Acta Derm Venereol 83(6):410–413. https://doi.org/10.1080/00015550310015419
Hwa C, Bauer EA, Cohen DE (2011) Skin biology: systems that enhance drug delivery - skin biology. Dermatol Ther 24(5):464–470. https://doi.org/10.1111/j.1529-8019.2012.01460.x
Oltulu P, Ince B, Kokbudak N, Findik S, Kilinc F (2018) Measurement of epidermis, dermis, and total skin thicknesses from six different body regions with a new ethical histometric technique. Turk J Plast Surg 26(2):56. https://doi.org/10.4103/tjps.TJPS_2_17
Gangatirkar P, Paquet-Fifield S, Li A, Rossi R, Kaur P (2007) Establishment of 3D organotypic cultures using human neonatal epidermal cells. Nat Protoc 2(1):178–186. https://doi.org/10.1038/nprot.2006.448
Itoh M, Umegaki-Arao N, Guo Z, Liu L, Higgins CA, Christiano AM (2013) Generation of 3D skin equivalents fully reconstituted from human induced pluripotent stem cells (iPSCs). PLoS One 8(10):e77673. https://doi.org/10.1371/journal.pone.0077673
Liu Y, Ma L, Gao C (2012) Facile fabrication of the glutaraldehyde cross-linked collagen/chitosan porous scaffold for skin tissue engineering. Mater Sci Eng C 32(8):2361–2366. https://doi.org/10.1016/j.msec.2012.07.008
Sheikh F et al (2014) 3D electrospun silk fibroin nanofibers for fabrication of artificial skin. Nanomed Nanotechnol, Biol Med 11. https://doi.org/10.1016/j.nano.2014.11.007
Cheung HY, Lau KT, Lu TP, Hui D (2007) A critical review on polymer-based bio-engineered materials for scaffold development. Compos B Eng. https://doi.org/10.1016/j.compositesb.2006.06.014
Golas AR, Hernandez KA, Spector JA (2014) Tissue engineering for plastic surgeons: a primer. Aesth Plast Surg 38(1):207–221. https://doi.org/10.1007/s00266-013-0255-5
Pereira RF, Barrias CC, Granja PL, Bartolo PJ (2013) Advanced biofabrication strategies for skin regeneration and repair. Nanomedicine 8(4):603–621. https://doi.org/10.2217/nnm.13.50
Hudecki A, Kiryczyński G, Łos MJ (2019) Biomaterials, definition, overview. In: Stem cells and biomaterials for regenerative medicine. Elsevier, Amsterdam, pp 85–98. https://doi.org/10.1016/B978-0-12-812258-7.00007-1
Bhardwaj N, Chouhan D, Mandal BB (2018) 3D functional scaffolds for skin tissue engineering. In: Functional 3D tissue engineering scaffolds. Elsevier, Amsterdam, pp 345–365. https://doi.org/10.1016/B978-0-08-100979-6.00014-8
O’Brien FJ (2011) Biomaterials & scaffolds for tissue engineering. Mater Today 14(3):88–95. https://doi.org/10.1016/S1369-7021(11)70058-X
Balint R, Cassidy NJ, Cartmell SH (2014) Conductive polymers: towards a smart biomaterial for tissue engineering. Acta Biomater 10(6):2341–2353. https://doi.org/10.1016/j.actbio.2014.02.015
Gupta P et al (2016) Mimicking form and function of native small diameter vascular conduits using mulberry and non-mulberry patterned silk films. ACS Appl Mater Interfaces 8(25):15874–15888. https://doi.org/10.1021/acsami.6b00783
Chan BP, Leong KW (2008) Scaffolding in tissue engineering: general approaches and tissue-specific considerations. Eur Spine J 17(S4):467–479. https://doi.org/10.1007/s00586-008-0745-3
Rahmati M, Blaker JJ, Lyngstadaas SP, Mano JF, Haugen HJ (2020) Designing multigradient biomaterials for skin regeneration. Mater Today Adv 5:100051. https://doi.org/10.1016/j.mtadv.2019.100051
Jeong K-H, Park D, Lee Y-C (2017) Polymer-based hydrogel scaffolds for skin tissue engineering applications: a mini-review. J Polym Res 24(7):112. https://doi.org/10.1007/s10965-017-1278-4
Bernard A, Renault JP, Michel B, Bosshard HR, Delamarche E (2000) Microcontact printing of proteins. Adv Mater. https://doi.org/10.1002/1521-4095(200007)12:14<1067::AID-ADMA1067>3.0.CO;2-M
Therriault D, White SR, Lewis JA (2003) Chaotic mixing in three-dimensional microvascular networks fabricated by direct-write assembly. Nat Mater. https://doi.org/10.1038/nmat863
Wang Z, Samanipour R, Koo KI, Kim K (2015) Organ-on-a-chip platforms for drug delivery and cell characterization: a review. Sens Mater. https://doi.org/10.18494/SAM.2015.1086
Sticker D, Rothbauer M, Lechner S, Hehenberger MT, Ertl P (2015) Multi-layered, membrane-integrated microfluidics based on replica molding of a thiol-ene epoxy thermoset for organ-on-a-chip applications. Lab Chip. https://doi.org/10.1039/c5lc01028d
Lee J, Cuddihy MJ, Kotov NA (2008) Three-dimensional cell culture matrices: state of the art. Tissue Eng B Rev. https://doi.org/10.1089/teb.2007.0150
Okugawa Y, Hirai Y (2013) Extracellular epimorphin modulates epidermal differentiation signals mediated by epidermal growth factor receptor. J Dermatol Sci. https://doi.org/10.1016/j.jdermsci.2012.11.006
Hern DL, Hubbell JA (1998) Incorporation of adhesion peptides into nonadhesive hydrogels useful for tissue resurfacing. J Biomed Mater Res. https://doi.org/10.1002/(SICI)1097-4636(199802)39:2<266::AID-JBM14>3.0.CO;2-B
Hosseinkhani H et al (2013) Engineering three-dimensional collagen-IKVAV matrix to mimic neural microenvironment. ACS Chem Neurosci. https://doi.org/10.1021/cn400075h
Zhao X et al (2016) Photocrosslinkable gelatin hydrogel for epidermal tissue engineering. Adv Healthc Mater. https://doi.org/10.1002/adhm.201500005
Fu L, **e J, Carlson MA, Reilly DA (2017) Three-dimensional nanofiber scaffolds with arrayed holes for engineering skin tissue constructs. MRS Commun. https://doi.org/10.1557/mrc.2017.49
Pan H, Jiang H, Chen W (2006) Interaction of dermal fibroblasts with electrospun composite polymer scaffolds prepared from dextran and poly lactide-co-glycolide. Biomaterials. https://doi.org/10.1016/j.biomaterials.2006.01.032
Plaza C, Meyrignac C, Botto J-M, Capallere C (2021) Characterization of a new full-thickness in vitro skin model. Tissue Eng Part C Methods 27(7):411–420. https://doi.org/10.1089/ten.tec.2021.0035
**a Y, Whitesides GM (1998) Soft lithography. Annu Rev Mater Sci. https://doi.org/10.1146/annurev.matsci.28.1.153
Qin D, **a Y, Whitesides GM (2010) Soft lithography for micro- and nanoscale patterning. Nat Protoc 5(3):491–502. https://doi.org/10.1038/nprot.2009.234
Kim JJ et al (2019) A microscale, full-thickness, human skin on a chip assay simulating neutrophil responses to skin infection and antibiotic treatments. Lab Chip 19(18):3094–3103. https://doi.org/10.1039/C9LC00399A
Kwak BS, ** SP, Kim SJ, Kim EJ, Chung JH, Sung JH (2020) Microfluidic skin chip with vasculature for recapitulating the immune response of the skin tissue. Biotechnol Bioeng 117(6):1853–1863. https://doi.org/10.1002/bit.27320
Warrick J, Meyvantsson I, Ju J, Beebe DJ (2007) High-throughput microfluidics: improved sample treatment and washing over standard wells. Lab Chip. https://doi.org/10.1039/b613350a
Dittrich PS, Manz A (2006) Lab-on-a-chip: microfluidics in drug discovery. Nat Rev Drug Discov. https://doi.org/10.1038/nrd1985
Valencia L et al (2021) A new microfluidic method enabling the generation of multi-layered tissues-on-chips using skin cells as a proof of concept. Sci Rep 11(1):13160. https://doi.org/10.1038/s41598-021-91875-z
Jeon HM, Kim K, Choi KC, Sung GY (2020) Side-effect test of sorafenib using 3-D skin equivalent based on microfluidic skin-on-a-chip. J Ind Eng Chem 82:71–80. https://doi.org/10.1016/j.jiec.2019.09.044
Kim K, Jeon HM, Choi KC, Sung GY (2020) Testing the effectiveness of curcuma longa leaf extract on a skin equivalent using a pumpless skin-on-a-chip model. IJMS 21(11):3898. https://doi.org/10.3390/ijms21113898
Sasaki N, Tsuchiya K, Kobayashi H (2019) Photolithography-free skin-on-a-chip for parallel permeation assays. Sens Mater 31(1):9
Lim HY et al (2018) Development of wrinkled skin-on-a-chip (WSOC) by cyclic uniaxial stretching. J Ind Eng Chem 68:238–245. https://doi.org/10.1016/j.jiec.2018.07.050
Song HJ et al (2018) Development of 3D skin-equivalent in a pump-less microfluidic chip. J Ind Eng Chem 60:355–359. https://doi.org/10.1016/j.jiec.2017.11.022
Song HJ, Lim HY, Chun W, Choi KC, Sung JH, Sung GY (2017) Fabrication of a pumpless, microfluidic skin chip from different collagen sources. J Ind Eng Chem 56:375–381. https://doi.org/10.1016/j.jiec.2017.07.034
Alexander F, Eggert S, Wiest J (2018) Skin-on-a-chip: transepithelial electrical resistance and extracellular acidification measurements through an automated air-liquid interface. Genes 9(2):114. https://doi.org/10.3390/genes9020114
Maschmeyer I et al (2015) Chip-based human liver–intestine and liver–skin co-cultures – a first step toward systemic repeated dose substance testing in vitro. Eur J Pharm Biopharm 95:77–87. https://doi.org/10.1016/j.ejpb.2015.03.002
Wagner I et al (2013) A dynamic multi-organ-chip for long-term cultivation and substance testing proven by 3D human liver and skin tissue co-culture. Lab Chip 13(18):3538. https://doi.org/10.1039/c3lc50234a
Calcein Am - an overview. ScienceDirect Topics. https://www.sciencedirect.com/topics/chemistry/calcein-am. Accessed 07 Nov 2021
Ethidium Homodimer - an overview. ScienceDirect Topics. https://www.sciencedirect.com/topics/chemistry/ethidium-homodimer. Accessed 07 Nov 2021
Crowley LC, Scott AP, Marfell BJ, Boughaba JA, Chojnowski G, Waterhouse NJ (2016) Measuring cell death by propidium iodide uptake and flow cytometry. Cold Spring Harb Protoc 2016(7). https://doi.org/10.1101/pdb.prot087163
Viability Assay - an overview. ScienceDirect Topics. https://www.sciencedirect.com/topics/pharmacology-toxicology-and-pharmaceutical-science/viability-assay. Accessed 07 Nov 2021
Moniz T, Lima SAC, Reis S (2020) Human skin models: from healthy to disease-mimetic systems; characteristics and applications. Br J Pharmacol 177(19):4314–4329. https://doi.org/10.1111/bph.15184
Souto LRM, Vassallo J, Rehder J, Pinto GA, Puzzi MB (2009) Immunoarchitectural characterization of a human skin model reconstructed in vitro. Sao Paulo Med J 127(1):28–33. https://doi.org/10.1590/S1516-31802009000100007
Barker CL et al (2004) The development and characterization of an in vitro model of psoriasis. J Investig Dermatol 123(5):892–901. https://doi.org/10.1111/j.0022-202X.2004.23435.x
Grimm J, Kircher MF, Weissleder R (2007) Cell tracking. Principles and applications. Radiologe 47(1):25–33. https://doi.org/10.1007/s00117-006-1449-5
Halabi EA, Arasa J, Püntener S, Collado-Diaz V, Halin C, Rivera-Fuentes P (2020) Dual-activatable cell tracker for controlled and prolonged single-cell labeling. ACS Chem Biol 15(6):1613–1620. https://doi.org/10.1021/acschembio.0c00208
Liang X, Graf BW, Boppart SA (2011) In vivo multiphoton microscopy for investigating biomechanical properties of human skin. Cell Mol Bioeng 4(2):231–238. https://doi.org/10.1007/s12195-010-0147-6
Pawlaczyk M, Lelonkiewicz M, Wieczorowski M (2013) Age-dependent biomechanical properties of the skin. Postepy Dermatol Allergol 30(5):302–306. https://doi.org/10.5114/pdia.2013.38359
Joodaki H, Panzer MB (2018) Skin mechanical properties and modeling: a review. https://journals.sagepub.com/doi/10.1177/0954411918759801. Accessed 07 Nov 2021
Jachowicz J, McMullen R, Prettypaul D (2007) Indentometric analysis of in vivo skin and comparison with artificial skin models. Skin Res Technol 13(3):299–309. https://doi.org/10.1111/j.1600-0846.2007.00229.x
Sutterby E, Thurgood P, Baratchi S, Khoshmanesh K, Pirogova E (2020) Microfluidic skin-on-a-chip models: toward biomimetic artificial skin. Small 16(39):2002515. https://doi.org/10.1002/smll.202002515
Mechanical properties and Young’s modulus of human skin in vivo. SpringerLink. https://springer.longhoe.net/article/10.1007/BF00406415. Accessed 07 Nov 2021
Kalra A, Lowe A (2016) Mechanical behaviour of skin: a review. J Mater Sci Eng 5. https://doi.org/10.4172/2169-0022.1000254
Dimitrow E et al (2009) Sensitivity and specificity of multiphoton laser tomography for in vivo and ex vivo diagnosis of malignant melanoma. J Invest Dermatol 129(7):1752–1758. https://doi.org/10.1038/jid.2008.439
Koehler MJ, König K, Elsner P, Bückle R, Kaatz M (2006) In vivo assessment of human skin aging by multiphoton laser scanning tomography. Opt Lett 31(19):2879–2881. https://doi.org/10.1364/ol.31.002879
Konig K, Ehlers A, Stracke F, Riemann I (2006) In vivo drug screening in human skin using femtosecond laser multiphoton tomography. Skin Pharmacol Physiol 19(2):78–88. https://doi.org/10.1159/000091974
Srinivasan B, Kolli AR, Esch MB, Abaci HE, Shuler ML, Hickman JJ (2015) TEER measurement techniques for in vitro barrier model systems. J Lab Autom 20(2):107–126. https://doi.org/10.1177/2211068214561025
Alberti M et al (2017) Multi-chamber microfluidic platform for high-precision skin permeation testing. Lab Chip 17(9):1625–1634. https://doi.org/10.1039/c6lc01574c
Netzlaff F, Lehr C-M, Wertz PW, Schaefer UF (2005) The human epidermis models EpiSkin, SkinEthic and EpiDerm: an evaluation of morphology and their suitability for testing phototoxicity, irritancy, corrosivity, and substance transport. Eur J Pharm Biopharm 60(2):167–178. https://doi.org/10.1016/j.ejpb.2005.03.004
Alexander FA, Eggert S, Wiest J (2018) Skin-on-a-chip: transepithelial electrical resistance and extracellular acidification measurements through an automated air-liquid interface. Genes (Basel) 9(2):E114. https://doi.org/10.3390/genes9020114
Niehues H, Bouwstra JA, Ghalbzouri AE, Brandner JM, Zeeuwen PLJM, van den Bogaard EH (2018) 3D skin models for 3R research: the potential of 3D reconstructed skin models to study skin barrier function. Exp Dermatol 27(5):501–511. https://doi.org/10.1111/exd.13531
Pauty J et al (2017) A vascular permeability assay using an in vitro human microvessel model mimicking the inflammatory condition. Nano 1(1):103–113. https://doi.org/10.7150/ntno.18303
Lukács B et al (2019) Skin-on-a-chip device for ex vivo monitoring of transdermal delivery of drugs—design, fabrication, and testing. Pharmaceutics 11(9):445. https://doi.org/10.3390/pharmaceutics11090445
Bajza Á et al (2020) Verification of p-glycoprotein function at the dermal barrier in diffusion cells and dynamic ‘skin-on-a-chip’ microfluidic device. Pharmaceutics 12(9):1–16. https://doi.org/10.3390/pharmaceutics12090804
Rousselle P, Gentilhomme E, Neveux Y (2017) Markers of Epidermal Proliferation and Differentiation. In: Humbert P, Fanian F, Maibach HI, Agache P (eds) Agache’s measuring the skin: non-invasive investigations, physiology, normal constants. Springer, Cham, pp 407–415. https://doi.org/10.1007/978-3-319-32383-1_37
Ponec M, Boelsma E, Weerheim A, Mulder A, Bouwstra J, Mommaas M (2000) Lipid and ultrastructural characterization of reconstructed skin models. Int J Pharm 203(1):211–225. https://doi.org/10.1016/S0378-5173(00)00459-2
Poumay Y, Coquette A (2006) Modelling the human epidermis in vitro: tools for basic and applied research. Arch Dermatol Res 298(8):361–369. https://doi.org/10.1007/s00403-006-0709-6
Kuempel D, Swartzendruber DC, Squier CA, Wertz PW (1998) In vitro reconstitution of stratum corneum lipid lamellae. Biochim Biophys Acta Biomembr 1372(1):135–140. https://doi.org/10.1016/S0005-2736(98)00053-4
Bataillon M et al (2019) Characterization of a new reconstructed full thickness skin model, T-Skin™, and its application for investigations of anti-aging compounds. Int J Mol Sci 20(9):9. https://doi.org/10.3390/ijms20092240
Marionnet C, Pierrard C, Vioux-Chagnoleau C, Sok J, Asselineau D, Bernerd F (2006) Interactions between fibroblasts and keratinocytes in morphogenesis of dermal epidermal junction in a model of reconstructed skin. J Investig Dermatol 126(5):971–979. https://doi.org/10.1038/sj.jid.5700230
Krieg T, Aumailley M (2011) The extracellular matrix of the dermis: flexible structures with dynamic functions. Exp Dermatol 20(8):689–695. https://doi.org/10.1111/j.1600-0625.2011.01313.x
Supp DM et al (2019) Collagen VII expression is required in both keratinocytes and fibroblasts for anchoring fibril formation in bilayer engineered skin substitutes. Cell Transplant 28(9–10):1242–1256. https://doi.org/10.1177/0963689719857657
Lippens S et al (2004) Vitamin D3 induces caspase-14 expression in psoriatic lesions and enhances caspase-14 processing in organotypic skin cultures. Am J Pathol 165(3):833–841. https://doi.org/10.1016/S0002-9440(10)63346-9
Chiricozzi A et al (2014) IL-17 induces an expanded range of downstream genes in reconstituted human epidermis model. PLoS One 9(2):e90284. https://doi.org/10.1371/journal.pone.0090284
Yin X, Zhang S, Li B, Zhang Y, Zhang X (2019) IL28RA inhibits human epidermal keratinocyte proliferation by inhibiting cell cycle progression. Mol Biol Rep 46(1):1189–1197. https://doi.org/10.1007/s11033-019-04586-0
Gibbs S et al (2013) An epidermal equivalent assay for identification and ranking potency of contact sensitizers. Toxicol Appl Pharmacol 272(2):529–541. https://doi.org/10.1016/j.taap.2013.07.003
Saito K, Takenouchi O, Nukada Y, Miyazawa M, Sakaguchi H (2017) An in vitro skin sensitization assay termed EpiSensA for broad sets of chemicals including lipophilic chemicals and pre/pro-haptens. Toxicol In Vitro 40:11–25. https://doi.org/10.1016/j.tiv.2016.12.005
Facy V, Flouret V, Régnier M, Schmidt R (2005) Reactivity of Langerhans cells in human reconstructed epidermis to known allergens and UV radiation. Toxicol In Vitro 19(6):787–795. https://doi.org/10.1016/j.tiv.2005.03.018
De Vuyst É et al (2018) Methyl-β-cyclodextrin concurs with interleukin (IL)-4, IL-13 and IL-25 to induce alterations reminiscent of atopic dermatitis in reconstructed human epidermis. Exp Dermatol 27(4):435–437. https://doi.org/10.1111/exd.13113
TNF-α and Th2 cytokines induce atopic dermatitis–like features on epidermal differentiation proteins and stratum corneum lipids in human skin equivalents. J Invest Dermatol. https://www.jidonline.org/article/S0022-202X(15)36873-1/fulltext. Accessed 20 Feb 2021
Boukhedouni N et al (2020) Type-1 cytokines regulate MMP-9 production and E-cadherin disruption to promote melanocyte loss in vitiligo. JCI Insight 5(11). https://doi.org/10.1172/jci.insight.133772
Matei A-E et al (2019) Vascularised human skin equivalents as a novel in vitro model of skin fibrosis and platform for testing of antifibrotic drugs. Ann Rheum Dis 78(12):1686–1692. https://doi.org/10.1136/annrheumdis-2019-216108
Hill DS et al (2015) A novel fully humanized 3D skin equivalent to model early melanoma invasion. Mol Cancer Ther 14(11):2665–2673. https://doi.org/10.1158/1535-7163.MCT-15-0394
Vörsmann H et al (2013) Development of a human three-dimensional organotypic skin-melanoma spheroid model for in vitro drug testing. Cell Death Dis 4(7):7. https://doi.org/10.1038/cddis.2013.249
Browning JR et al (2020) A 3D biofabricated cutaneous squamous cell carcinoma tissue model with multi-channel confocal microscopy imaging biomarkers to quantify antitumor effects of chemotherapeutics in tissue. Oncotarget 11(27):2587–2596. https://doi.org/10.18632/oncotarget.27570
Linde N, Gutschalk CM, Hoffmann C, Yilmaz D, Mueller MM (2012) Integrating macrophages into organotypic co-cultures: a 3D in vitro model to study tumor-associated macrophages. PLoS One 7(7):e40058. https://doi.org/10.1371/journal.pone.0040058
Obrigkeit DH et al (2009) Effects of photodynamic therapy evaluated in a novel three-dimensional squamous cell carcinoma organ construct of the skin. Photochem Photobiol 85(1):272–278. https://doi.org/10.1111/j.1751-1097.2008.00432.x
Tan JJY, Common JE, Wu C, Ho PCL, Kang L (2019) Keratinocytes maintain compartmentalization between dermal papilla and fibroblasts in 3D heterotypic tri-cultures. Cell Prolif 52(5):e12668. https://doi.org/10.1111/cpr.12668
Lin B et al (2016) Surface tension guided hanging-drop: producing controllable 3D spheroid of high-passaged human dermal papilla cells and forming inductive microtissues for hair-follicle regeneration. ACS Appl Mater Interfaces 8(9):5906–5916. https://doi.org/10.1021/acsami.6b00202
Gupta AC et al (2018) Establishment of an in vitro organoid model of dermal papilla of human hair follicle. J Cell Physiol 233(11):9015–9030. https://doi.org/10.1002/jcp.26853
de Breij A et al (2012) Three-dimensional human skin equivalent as a tool to study Acinetobacter baumannii colonization. Antimicrob Agents Chemother 56(5):2459–2464. https://doi.org/10.1128/AAC.05975-11
Havlikova J, May RC, Styles IB, Cooper HJ (2020) Direct identification of bacterial and human proteins from infected wounds in living 3D skin models. Sci Rep 10(1):1. https://doi.org/10.1038/s41598-020-68233-6
Liang P-P et al (2016) A trichophyton rubrum infection model based on the reconstructed human epidermis - Episkin®. Chin Med J 129(1):54–58. https://doi.org/10.4103/0366-6999.172573
Faway É, Cambier L, Mignon B, Poumay Y, Lambert de Rouvroit C (2017) Modeling dermatophytosis in reconstructed human epidermis: a new tool to study infection mechanisms and to test antifungal agents. Med Mycol 55(5):485–494. https://doi.org/10.1093/mmy/myw111
Coolen NA, Vlig M, Bogaerdt AJVD, Middelkoop E, Ulrich MMW (2008) Development of an in vitro burn wound model. Wound Repair Regen 16(4):559–567. https://doi.org/10.1111/j.1524-475X.2008.00403.x
Weinmüllner R et al (2020) Organotypic human skin culture models constructed with senescent fibroblasts show hallmarks of skin aging. NPJ Aging Mech Dis 6(1):1–7. https://doi.org/10.1038/s41514-020-0042-x
Dos Santos M, Metral E, Boher A, Rousselle P, Thepot A, Damour O (2015) In vitro 3-D model based on extending time of culture for studying chronological epidermis aging. Matrix Biol 47:85–97. https://doi.org/10.1016/j.matbio.2015.03.009
Bernerd F, Asselineau D (1998) UVA exposure of human skin reconstructed in vitro induces apoptosis of dermal fibroblasts: subsequent connective tissue repair and implications in photoaging. Cell Death Differ 5(9):9. https://doi.org/10.1038/sj.cdd.4400413
Meloni M, Farina A, de Servi B (2010) Molecular modifications of dermal and epidermal biomarkers following UVA exposures on reconstructed full-thickness human skin. Photochem Photobiol Sci 9(4):439–447. https://doi.org/10.1039/B9PP00164F
Karapetsas A et al (2020) Honey extracts exhibit cytoprotective properties against UVB-induced photodamage in human experimental skin models. Antioxidants 9(7):7. https://doi.org/10.3390/antiox9070566
Verdin A et al (2019) An in vitro model to evaluate the impact of environmental fine particles (PM0.3-2.5) on skin damage. Toxicol Lett 305:94–102. https://doi.org/10.1016/j.toxlet.2019.01.016
McKenzie NE (2005) The drug development process. Fundament Cancer Prev:131–138. https://doi.org/10.1007/3-540-26337-3_7
Drews J (2000) Drug discovery: a historical perspective. Science. https://doi.org/10.1126/science.287.5460.1960
Sung JH et al (2013) Microfabricated mammalian organ systems and their integration into models of whole animals and humans. Lab Chip. https://doi.org/10.1039/c3lc41017j
Luni C, Serena E, Elvassore N (2014) Human-on-chip for therapy development and fundamental science. Curr Opin Biotechnol. https://doi.org/10.1016/j.copbio.2013.08.015
** H, Yu Y (2016) A review of the application of body-on-a-chip for drug test and its latest trend of incorporating barrier tissue. J Lab Autom. https://doi.org/10.1177/2211068215619126
Biglari S et al (2019) Simulating inflammation in a wound microenvironment using a dermal wound-on-a-chip model. Adv Healthc Mater. https://doi.org/10.1002/adhm.201801307
Ray TR et al (2021) Soft, skin-interfaced sweat stickers for cystic fibrosis diagnosis and management. Sci Transl Med. https://doi.org/10.1126/scitranslmed.abd8109
Can sweat shed a light on disease severity in atopic dermatitis? [Online]. Available: https://www.dermatologytimes.com/view/can-sweat-shed-light-disease-severity-atopic-dermatitis. Accessed 30 July 2021
Sheibani S et al (2021) Extended gate field-effect-transistor for sensing cortisol stress hormone. Commun Mater. https://doi.org/10.1038/s43246-020-00114-x
Kim S et al (2020) Soft, skin-interfaced microfluidic systems with integrated immunoassays, fluorometric sensors, and impedance measurement capabilities. Proc Natl Acad Sci U S A. https://doi.org/10.1073/pnas.2012700117
Gentag Announces Lab-on-a-Chip (LOC) Patent For Diagnostics With Cell Phones (NFC) | Gentag. [Online]. Available: https://gentag.com/gentags-lab-chip-loc-patent-diagnostics-cell-phones-issues/. Accessed 30 July 2021
Gorjikhah F et al (2016) Improving ‘lab-on-a-chip’ techniques using biomedical nanotechnology: a review. Artif Cells Nanomed Biotechnol 44(7):1609–1614. https://doi.org/10.3109/21691401.2015.1129619
Researchers are develo** a ‘Lab-on-skin’ to monitor biomarkers • healthcare-in-europe.com. [Online]. Available: https://healthcare-in-europe.com/en/news/researchers-are-develo**-a-lab-on-skin-to-monitor-biomarkers.html. Accessed 30 July 2021
Tavares RSN et al (2020) Skin irritation testing beyond tissue viability: fucoxanthin effects on inflammation, homeostasis, and metabolism. Pharmaceutics. https://doi.org/10.3390/pharmaceutics12020136
Wang XP et al (2004) The interleukin-6 cytokine system regulates epidermal permeability barrier homeostasis. J Investig Dermatol. https://doi.org/10.1111/j.0022-202X.2004.22736.x
Jensen JM, Schütze S, Förl M, Krönke M, Proksch E (1999) Roles for tumor necrosis factor receptor p55 and sphingomyelinase in repairing the cutaneous permeability barrier. J Clin Investig. https://doi.org/10.1172/JCI5307
Kim J, Kim K, Sung GY (2020) Coenzyme q10 efficacy test for human skin equivalents using a pumpless skin-on-a-chip system. Int J Mol Sci. https://doi.org/10.3390/ijms21228475
Kim K, Jeon HM, Choi KC, Sung GY (2020) Testing the effectiveness of curcuma longa leaf extract on a skin equivalent using a pumpless skin-on-a-chip model. Int J Mol Sci 21(11):1–15. https://doi.org/10.3390/ijms21113898
Pauty J et al (2021) A 3D tissue model-on-a-chip for studying the effects of human senescent fibroblasts on blood vessels. Biomater Sci. https://doi.org/10.1039/d0bm01297a
Ruze A et al (2018) Low shear stress upregulates the expression of fractalkine through the activation of mitogen-activated protein kinases in endothelial cells. Blood Coagul Fibrinolysis. https://doi.org/10.1097/MBC.0000000000000701
Lin JY, Lo KY, Sun YS (2019) A microfluidics-based wound-healing assay for studying the effects of shear stresses, wound widths, and chemicals on the wound-healing process. Sci Rep. https://doi.org/10.1038/s41598-019-56753-9
Lawrence BJ, Madihally SV (2008) Cell colonization in degradable 3D porous matrices. Cell Adhes Migr. https://doi.org/10.4161/cam.2.1.5884
Suwannaphan T et al (2016) Investigation of shear stress and cell survival in a microfluidic chip for a single cell study. https://doi.org/10.1109/BMEiCON.2015.7399541
Agarwal T, Narayana GH, Banerjee I (2019) Keratinocytes are mechanoresponsive to the microflow-induced shear stress. Cytoskeleton. https://doi.org/10.1002/cm.21521
Allwardt V et al (2020) Translational roadmap for the organs-on-a-chip industry toward broad adoption. Bioengineering 7(3):3. https://doi.org/10.3390/bioengineering7030112
How to improve R&D productivity: the pharmaceutical industry’s grand challenge. Nat Rev Drug Discov. https://www.nature.com/articles/nrd3078. Accessed 09 July 2021
Harrison RK (2016) Phase II and phase III failures: 2013–2015. Nat Rev Drug Discov 15(12):817–818. https://doi.org/10.1038/nrd.2016.184
Arrowsmith J, Miller P (2013) Phase II and Phase III attrition rates 2011–2012. Nat Rev Drug Discov 12(8):569–569. https://doi.org/10.1038/nrd4090
Probst C, Schneider S, Loskill P (2018) High-throughput organ-on-a-chip systems: current status and remaining challenges. Curr Opin Biomed Eng 6:33–41. https://doi.org/10.1016/j.cobme.2018.02.004
Reardon S (2015) ‘Organs-on-chips’ go mainstream. Nature 523(7560):266–266. https://doi.org/10.1038/523266a
DiMasi JA, Grabowski HG, Hansen RW (2016) Innovation in the pharmaceutical industry: new estimates of R&D costs. J Health Econ 47:20–33. https://doi.org/10.1016/j.jhealeco.2016.01.012
Prasad V, Mailankody S (2017) Research and development spending to bring a single cancer drug to market and revenues after approval. JAMA Intern Med 177(11):1569–1575. https://doi.org/10.1001/jamainternmed.2017.3601
Impact of organ-on-a-chip technology on pharmaceutical R&D costs. Elsevier Enhanced Reader. https://reader.elsevier.com/reader/sd/pii/S135964461930042X?token=9AC2BDA79D1EAD5E80268995FCBD5A3FE36048296F31BCBD44426678C8AFBDDC501CAF4B652426D61A2B3300A7670A7F&originRegion=eu-west-1&originCreation=20210708174208. Accessed 09 July 2021
C. for D. E. and Research. Office of Clinical Pharmacology, FDA, 31 Mar 2021. https://www.fda.gov/about-fda/center-drug-evaluation-and-research-cder/office-clinical-pharmacology. Accessed 09 July 2021
C. for D. E. and Research. Product Development Under the Animal Rule. U.S. Food and Drug Administration, 14 Apr 2020. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/product-development-under-animal-rule. Accessed 09 July 2021
OECD (2019) Test No. 431: In vitro skin corrosion: reconstructed human epidermis (RHE) test method. Organisation for Economic Co-operation and Development, Paris. Available: https://www.oecd-ilibrary.org/environment/test-no-431-in-vitro-skin-corrosion-reconstructed-human-epidermis-rhe-test-method_9789264264618-en. Accessed 07 Nov 2021
OECD (2010) Test No. 439: In vitro skin irritation: reconstructed human epidermis test method. Organisation for Economic Co-operation and Development, Paris. Available: https://www.oecd-ilibrary.org/environment/test-no-439-in-vitro-skin-irritation_9789264090958-en. Accessed 07 Nov 2021
OECD (2021) Test No. 498: In vitro phototoxicity - Reconstructed Human Epidermis Phototoxicity test method. Organisation for Economic Co-operation and Development, Paris. Available: https://www.oecd-ilibrary.org/environment/test-no-498-in-vitro-phototoxicity-reconstructed-human-epidermis-phototoxicity-test-method_7b2f9ea0-en. Accessed 07 Nov 2021
Pasman T, Grijpma D, Stamatialis D, Poot A (2018) Flat and microstructured polymeric membranes in organs-on-chips. J R Soc Interface. https://doi.org/10.1098/rsif.2018.0351
Huh D (2015) A human breathing lung-on-a-chip. Ann Am Thorac Soc. https://doi.org/10.1513/AnnalsATS.201410-442MG
Gumuscu B, Albers HJ, Van Den Berg A, Eijkel JCT, Van Der Meer AD (2017) Compartmentalized 3D tissue culture arrays under controlled microfluidic delivery. Sci Rep. https://doi.org/10.1038/s41598-017-01944-5
Richardson L, Jeong S, Kim S, Hart A, Menon R (2019) Amnion membrane organ-on-chip: an innovative approach to study cellular interactions. FASEB J. https://doi.org/10.1096/fj.201900020RR
van Meer BJ et al (2017) Small molecule absorption by PDMS in the context of drug response bioassays. Biochem Biophys Res Commun. https://doi.org/10.1016/j.bbrc.2016.11.062
Toepke MW, Beebe DJ (2006) PDMS absorption of small molecules and consequences in microfluidic applications. Lab Chip 6(12):12. https://doi.org/10.1039/B612140C
Berthier E, Young EWK, Beebe D (2012) Engineers are from PDMS-land, biologists are from polystyrenia. Lab Chip. https://doi.org/10.1039/c2lc20982a
Eddington DT, Puccinelli JP, Beebe DJ (2006) Thermal aging and reduced hydrophobic recovery of polydimethylsiloxane. Sensors Actuators B Chem. https://doi.org/10.1016/j.snb.2005.04.037
Agarwal A, Farouz Y, Nesmith AP, Deravi LF, McCain ML, Parker KK (2013) Micropatterning alginate substrates for in vitro cardiovascular muscle on a chip. Adv Funct Mater. https://doi.org/10.1002/adfm.201203319
Ren K, Zhou J, Wu H (2013) Materials for microfluidic chip fabrication. Acc Chem Res. https://doi.org/10.1021/ar300314s
Borysiak MD, Bielawski KS, Sniadecki NJ, Jenkel CF, Vogt BD, Posner JD (2013) Simple replica micromolding of biocompatible styrenic elastomers. Lab Chip. https://doi.org/10.1039/c3lc50426c
Wikswo JP (2017) Looking to the future of organs-on-chips: interview with professor John Wikswo. Future Sci OA. https://doi.org/10.4155/fsoa-2016-0085
Henry OYF, Villenave R, Cronce MJ, Leineweber WD, Benz MA, Ingber DE (2017) Organs-on-chips with integrated electrodes for trans-epithelial electrical resistance (TEER) measurements of human epithelial barrier function. Lab Chip. https://doi.org/10.1039/c7lc00155j
Rennert K et al (2015) A microfluidically perfused three dimensional human liver model. Biomaterials. https://doi.org/10.1016/j.biomaterials.2015.08.043
Gruber P, Marques MPC, Szita N, Mayr T (2017) Integration and application of optical chemical sensors in microbioreactors. Lab Chip. https://doi.org/10.1039/c7lc00538e
Wikswo JP et al (2013) Engineering challenges for instrumenting and controlling integrated organ-on-chip systems. IEEE Trans Biomed Eng. https://doi.org/10.1109/TBME.2013.2244891
Gordon S et al (2015) Non-animal models of epithelial barriers (skin, intestine and lung) in research, industrial applications and regulatory toxicology. ALTEX 32(4):327–378. https://doi.org/10.14573/altex.1510051
Wainwright DJ (1995) Use of an acellular allograft dermal matrix (AlloDerm) in the management of full-thickness burns. Burns 21(4):243–248. https://doi.org/10.1016/0305-4179(95)93866-i
Boyce ST, Kagan RJ, Meyer NA, Yakuboff KP, Warden GD (1999) The 1999 clinical research award. Cultured skin substitutes combined with Integra Artificial Skin to replace native skin autograft and allograft for the closure of excised full-thickness burns. J Burn Care Rehabil 20(6):453–461. https://doi.org/10.1097/00004630-199920060-00006
Eaglstein WH, Falanga V (1997) Tissue engineering and the development of Apligraf, a human skin equivalent. Clin Ther 19(5):894–905. https://doi.org/10.1016/s0149-2918(97)80043-4
Hansbrough JF, Mozingo DW, Kealey GP, Davis M, Gidner A, Gentzkow GD (1997) Clinical trials of a biosynthetic temporary skin replacement, dermagraft-transitional covering, compared with cryopreserved human cadaver skin for temporary coverage of excised burn wounds. J Burn Care Rehabil 18(1 Pt 1):43–51. https://doi.org/10.1097/00004630-199701000-00008
Vig K et al (2017) Advances in skin regeneration using tissue engineering. Int J Mol Sci 18(4):E789. https://doi.org/10.3390/ijms18040789
Centanni JM et al (2011) StrataGraft skin substitute is well-tolerated and is not acutely immunogenic in patients with traumatic wounds: results from a prospective, randomized, controlled dose escalation trial. Ann Surg 253(4):672–683. https://doi.org/10.1097/SLA.0b013e318210f3bd
Allen-Hoffmann B, Rooney P (2016) Current innovations for the treatment of chronic wounds, pp 265–287. https://doi.org/10.1016/B978-0-12-801654-1.00013-9
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Chaturvedi, D., Mukherjee, S., Sawant, P., Jain, P.D., Majumder, A. (2022). Skin-on-Chip. In: Mohanan, P.V. (eds) Microfluidics and Multi Organs on Chip . Springer, Singapore. https://doi.org/10.1007/978-981-19-1379-2_22
Download citation
DOI: https://doi.org/10.1007/978-981-19-1379-2_22
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-19-1378-5
Online ISBN: 978-981-19-1379-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)