Abstract
In recent years, there has been an increase in the incidence of foodborne diseases worldwide, with viruses now being recognized as a major cause of these illnesses. The most common viruses implicated in foodborne disease are enteric viruses, which are found in the human gastrointestinal tract, excreted in human feces and transmitted by the fecal-oral route. Many different viruses are found in the gastrointestinal tract but not all are recognized as foodborne pathogens. The diseases caused by enteric viruses fall into three main types: gastroenteritis, enterically transmitted hepatitis, and illnesses that can affect other parts of the body such as the eye, the respiratory system and the central nervous system leading to conjunctivitis, poliomyelitis, meningitis and encephalitis. Viral pathogens excreted in human feces include noroviruses, sapoviruses, enteroviruses, adenoviruses, hepatitis A virus (HAV), hepatitis E virus (HEV), rotaviruses, and astroviruses. Most of these viruses have been associated with foodborne disease outbreaks. Noroviruses and HAV are commonly identified as foodborne causes of gastroenteritis and acute hepatitis, respectively.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Foodborne viruses
- Enteric viruses
- Epidemiology
- Taxonomy
- Biological propterties
- Foodborne disease
- Zoonotic transmission
1 Introduction
In recent years, there has been an increase in the incidence of foodborne diseases worldwide, with viruses now being recognized as a major cause of these illnesses. The most common viruses implicated in foodborne disease are enteric viruses, which are found in the human gastrointestinal tract, excreted in human feces and transmitted by the fecal-oral route. Many different viruses are found in the gastrointestinal tract but not all are recognized as foodborne pathogens. The diseases caused by enteric viruses fall into three main types: gastroenteritis, enterically transmitted hepatitis, and illnesses that can affect other parts of the body such as the eye, the respiratory system and the central nervous system leading to conjunctivitis, poliomyelitis, meningitis and encephalitis. Viral pathogens excreted in human feces include noroviruses, sapoviruses, enteroviruses, adenoviruses, hepatitis A virus (HAV), hepatitis E virus (HEV), rotaviruses, and astroviruses. Most of these viruses have been associated with foodborne disease outbreaks. Noroviruses and HAV are commonly identified as foodborne causes of gastroenteritis and acute hepatitis, respectively.
Other human- and animal-derived viruses, which have the potential to be transmitted by food, do not always infect the gastrointestinal tract . For example, HAV and HEV infect the liver; enterovirus, poliovirus, Nipah virus and tick-borne encephalitis virus infect the nervous system; and the SARS (severe acute respiratory syndrome) and the MERS (Middle East respiratory syndrome) coronaviruses and avian influenza virus H5N1 infect the respiratory system (FAO/WHO 2008). Members of several virus families (including Birnaviridae, Circoviridae, Papillomaviridae, Parvoviridae and Polyomaviridae) can survive for a prolonged period outside the host, a suitable characteristic for foodborne transmission (Koopmans et al. 2008).
Five of the enteric viruses, namely norovirus, HAV, sapovirus, rotavirus and astrovirus, are included in the 31 major foodborne pathogens identified by the Centers for Disease Control and Prevention (CDC) (Scallan et al. 2011). Of the estimated 37 million foodborne illnesses that occur annually in the United States, viruses cause 59 % of illnesses with noroviruses being the greatest contributor, causing an estimated 5.5 million cases per year (Scallan et al. 2011). The European Food Safety Authority (EFSA) identified norovirus (NoV) and HAV as the major foodborne viruses of public health significance. The HEV was also included because of its high prevalence in pigs and the potential for zoonotic transmission (EFSA 2011). Several virus-commodity combinations were identified as high priority for implementation of prevention and control measures :
-
NoV and HAV in bivalve molluscan shellfish
-
NoV and HAV in fresh produce
-
NoV and HAV in prepared (ready-to-eat) foods
-
Rotaviruses in water for food preparation
-
Emerging viruses in selected commodities
With the exception of shellfish, which are most often contaminated by sewage infiltration of harvesting waters, food handlers are the most significant source of viral foodborne illnesses. Foods most often implicated include salads, fresh produce and bakery or delicatessen items that are prepared or handled raw or after the foods have been cooked. The EFSA now recommends a focus on measures such as encouraging good hand hygiene and sanitation to prevent viral contamination of foods rather than virus removal or inactivation after foods have become contaminated (EFSA 2011).
All enteric viruses except the adenoviruses contain RNA, have a protein capsid that protects the nucleic acid, and are non-enveloped. In the environment and in food, the enteric viruses are inert particles and do not replicate or metabolize because, like all other viruses, they are obligate pathogens and require living cells to multiply. Cell cultures are generally used for the growth and analysis of culturable viruses. Using culture methods , infectious viruses can be identified through their ability to produce cell changes or cytopathic effects (CPE), or through expression of viral antigens that may be detected serologically. The advantage of culture-based methodology is that it can be either quantitative or qualitative and produces unambiguous results with respect to virus presence and infectivity. Many of the enteric viruses such as astroviruses, enteric adenoviruses, HAV and rotaviruses are fastidious in their in vitro growth requirements but can still be grown in cell cultures with some effort. Despite numerous attempts to grow human norovirus (HuNoV) in vitro in traditional cell lines, primary cell cultures, or differentiated tissues grown in three-dimensional cultures (Duizer et al. 2004; Lay et al. 2010; Papafragkou et al. 2013), they have until recently remained recalitrant. Low-level HuNoV infection in cultured B-cells was recently reported (Jones et al. 2014). Such findings are exciting and promising, but the model awaits optimization and validation before it can be routinely applied. In addition, no animal model for Human NoV infection has been validated, although recent reports on replication of this virus in immunocompromised mice and gnotobiotic animals suggest that this task is not out of reach (Tan and Jiang 2010; Bok et al. 2011). In the meantime, surrogate viruses that are closely related to HuNoV and are easily cultured in the laboratory, are used to conduct studies on the disinfection and environmental persistence of HuNoV.
Until the introduction of molecular methods, enteric viruses were mainly identified by electron microscopy (EM) including solid phase immune electron microscopy (SPIEM) . The SPIEM is more sensitive than direct EM because, in the presence of specific antibodies, the virus particles are aggregated together making them more easily distinguishable from the background matrix. Many of the ‘small round viruses’, which include astroviruses, noroviruses, sapoviruses and parvoviruses, were first discovered through the use of EM. Molecular methods , especially real-time quantitative PCR, are now the most commonly used techniques for the identification of enteric viruses in foods. Other methods for identification of enteric viruses in human specimens include enzyme-linked immunosorbent assay (ELISA), radioimmunoassay (RIA) and culture-PCR, which is a combination of cell culture and PCR methods. The latter technique detects only the infectious virus and is preferable to direct PCR, which currently detects both infectious and non-infectious viruses.
The enteric viruses are generally resistant to environmental stressors, including moderate heat and acid extremes. Most resist freezing and drying and are stable in the presence of organic solvents. It is not clear whether pasteurization at 60 °C for 30 min inactivates all enteric viruses in all food types. Many enteric viruses show resistance to high hydrostatic pressure, which is now widely used as a food processing treatment for shellfish, jams, jellies and dairy products (Kingsley 2013). The resistance of enteric viruses to environmental stressors allows them to survive both the acidic environment of the mammalian gastrointestinal tract and also the proteolytic and alkaline activities of the duodenum, so that infection can be established in the small intestine. Thus, enteric viruses can survive in acidic foods, marinated and pickled foods, frozen foods and lightly cooked foods such as gently steamed shellfish. Most enteric viruses are believed to have a low infectious dose of 10–100 particles or possibly even less. Hence, although they do not multiply in food, enough infectious viruses may survive in food to cause infection.
Enteric viruses have been shown to retain infectivity in shellfish and in fresh, estuarine and marine waters for several weeks to months at 4 °C (Bae and Schwab 2008). The length of virus survival appears to be inversely related to temperature. They may survive longer if attached to particulate matter or sediments, where they can present a greater potential risk to human health (Jaykus et al. 1994). Numerous studies have been published in recent years assessing the fate of foodborne viruses in the environment and their transfer to foods during preparation and handling (Kotwal and Cannon 2014).
Viral contamination of foods can occur before, during or after harvest at any stage in the food harvesting, processing, distribution and retail chain, or by food handlers in the home or restaurant setting. The key factors influencing the risk of contamination of fresh produce are water quality and food worker hand hygiene. Thus sewage contamination and poor hygiene practices play a major role in the contamination of produce.
Numerous opportunities exist for both pre- and post-harvest viral contamination of food. The quality of shellfish growing waters is important; pre-harvest virus contamination occurs when filter-feeding bivalve shellfish grow in waters contaminated with sewage or fecal material. Shellfish filter between four and 20 L of water every hour, sieving out and accumulating food particles, including bacteria, viruses and heavy metals. Feeding rates depend upon water temperature and salinity and availability of food and particulate matter. Bacteria and viruses become trapped in the mucus of the gills, which is then pushed into the digestive gland where viruses concentrate. Shellfish can accumulate high concentrations of viruses within a few hours e.g., they may contain virus levels that are 100–1000 times greater than in the surrounding waters.
Different species of oysters take up enteric viruses at different rates (Nappier et al. 2008, 2010). In winter, the shellfish are physiologically less active and do not accumulate viruses as fast as in warmer seasons. In clean waters, shellfish depurate or cleanse themselves of bacteria and particulate matter. However, studies have shown that depuration does not remove viruses efficiently and that there is no correlation between the removal of bacteria and viruses (Lees 2000). This was demonstrated in a large hepatitis A outbreak in Australia where oysters were depurated for 36 h before consumption but still retained infectious HAV (Conaty et al. 2000). Recent laboratory-based depuration experiments have shown that poliovirus, HAV and norovirus are eliminated at different rates from Pacific oysters over a 48 h period; most of the poliovirus was inactivated but HAV remained infectious over the 48 h period (McLeod et al. 2009). Human noroviruses are particularly recalcitrant to removal by depuration due to specific carbohydrate moieties expressed in the digestive diverticula of some filter-feeding bivalves that bind and retain the viruses (Le Guyader 2006; Maalouf et al. 2010; Tian et al. 2007).
The globalization of the food supply means that the source of fresh produce may not always be known and the quality may not always be controlled. Although it is presumed that fresh produce is “clean, green and healthy”, it may not be so, especially when it is imported from countries where general hygiene practices do not meet international standards. In recent years, there have been numerous outbreaks of HuNoV and HAV associated with contaminated fresh produce imported into Europe, Australia and North America (Anonymous 2013; Carvalho et al. 2012; Cotterelle et al. 2005; Donnan et al. 2012; Ethelberg et al. 2010; Falkenhorst et al. 2005; Fournet et al. 2012; Korsager et al. 2005; Le Guyader et al. 2004; Made et al. 2013; Maunula et al. 2009). Confirming the sources of contamination during these outbreaks has proven to be very difficult. In some cases, more than one pathogen or strain of virus was associated with the outbreak, suggesting that sewage-impacted irrigation or produce-wash water may have been involved.
Fresh produce may become contaminated with disease-causing enteric viruses if irrigated with or washed in water containing human fecal material or if handled by field-workers or food-handlers with poor hygiene practices. Foods at the greatest risk of virus contamination at the pre-harvest, harvest or post-harvest processing stage are shellfish, soft berry fruits, herbs and salad greens. Foods that are subject to much handling and are subsequently consumed cold or uncooked are at risk of contamination from food handlers. Such foods include bread and bakery goods, lightly cooked or raw shellfish, sandwiches, salads, herbs, fresh fruits, cold meats and cold desserts. It is probable that the current trend for the consumption of raw or lightly cooked ready-to-eat (RTE) foods, especially salads and sandwiches, has increased the risk of foodborne viral disease. Poor food handling was shown to be a key risk factor in the transmission of HuNoV in New Zealand and of HuNoV and rotaviruses in the Netherlands (de Wit et al. 2003; Thornley et al. 2013). In the U.S., infected food handlers are the source of over 50 % of all foodborne HuNoV outbreaks, and may even play a contributing role in over 80 % of them (Hall et al. 2012).
Viruses are frequently host specific, preferring to grow in the tissue of one species rather than a range of species. Both animal and human strains exist in all of the enteric viral genera. A key question still to be answered is whether animal viruses can infect humans and vice versa. The pathogenic strains of astrovirus, adenovirus and enterovirus that infect animals appear to be distinct from those infecting humans. Thus, although noroviruses have been isolated from animal feces and antibodies to animal noroviruses have been detected in humans, so far they have not been implicated in human disease.
Zoonotic infections are generally not transmitted by food. However, the risk of zoonotic viral disease from meat products contaminated with animal viruses has been identified in some countries, with tick-borne encephalitis virus (TBE) and hepatitis E virus (HEV) being two examples. The HEV is possibly the first virus reported to cause zoonotic foodborne viral disease. Non-viral infectious proteinaceous agents or prions, that cause diseases such as bovine spongiform encephalopathy (BSE), scrapie and Creuzfeldt-Jacob disease, also transmit disease from animals to humans via the foodborne route but are not discussed in this review.
As a result of the advances in methodology for detection of viruses in foods, the extent and role of viruses in foodborne disease has been clarified in recent years. New molecular methods , including real-time quantitative PCR for the detection of non-culturable or difficult to culture viruses, have shown their frequent presence in the environment and foods, especially shellfish. These methods have also allowed investigation of virus responses to environmental stressors and have contributed to increased knowledge of enteric virus behavior in the foods and the environment.
2 Hepatitis A Virus
2.1 Distribution and Transmission
Several different viruses cause hepatitis but only two, namely HAV and HEV, are transmitted by the fecal-oral route. The hepatitis viruses are so named because they infect the liver. These viruses do not share phylogenetic or morphological similarities and each of the five different hepatitis viruses is classified in distinct virus families. The HAV causes hepatitis A, a severe food and waterborn e disease primarily transmitted by the fecal-oral route, which was formerly known as infectious hepatitis or jaundice. Hepatitis A infection occurs worldwide and is especially common in develo** countries where over 90–100 % of children are infected by 6 years of age (Cliver 1997; Cromeans et al. 2001; Franco et al. 2012). The infection is often asymptomatic in children.
In recent years, the incidence of HAV infection in many countries has decreased as sewage treatment and hygiene practices have improved, but this has also led to an overall lowering of immunity in these populations with consequent increase in susceptibility to the disease. As a result, there is an increasing risk of contracting HAV infection from fresh foods imported from regions of the world where HAV is endemic and general hygiene standards are poor. Hepatitis A is a serious foodborne infection and hence is a notifiable disease in most of the developed countries. In the United States, HAV is reported as the most common cause of hepatitis with an estimated death rate of 2.4 % for laboratory confirmed cases (Scallan et al. 2011). The majority of illnesses (41 %) are related to travel but approximately 1500 cases (7 %) each year in the US are due to domestically acquired foodborne illnesses. In 2010, 1670 illnesses were reported to the CDC in the US. Taking into account asymptomatic infections and underreporting, it is estimated that there were 17,000 cases, an 88 % decline from the past decade (CDC 2010).
No seasonal distribution of HAV has been observed, with infection occurring throughout the year, but the disease has been reported to have a cyclic occurrence in endemic areas. This cyclic pattern has been observed in the United States, particularly among low socio-economic Native American and Hispanic populations. Large increases in HAV infections occur approximately every 10 years when a new cohort of susceptible children within these communities reach an age when they can become clinically symptomatic. However, the main transmission route is generally believed to be person-to-person rather than foodborne (Cromeans et al. 2001; Fiore 2004).
2.2 Taxonomy and Morphology
The HAV is a 27–32 nm non-enveloped, positive-sense, single-stranded RNA virus with a 7.5 kb genome, icosohedral capsid symmetry, and a buoyant density in cesium chloride of 1.33–1.34 g/ml. The virus is classified in the Picornaviridae family in its own distinct genus, Hepatovirus (Table 2.1). Hepatoviruses do not exhibit the “canyon-like” cellular receptor binding sites on their capsid surface causing differences in cell interaction, which sets them apart from other picornaviruses (Cristina and Costa-Mattioli 2007). The single species of HAV was previously classified into seven genotypes based on partial sequences of VP1 and VP3 genes that code for surface proteins (Robertson et al. 1992; Robertson et al. 1991). However, full-length VP1 sequencing has now revealed similarities between genogroup II and IV strains, sub-grou** of genogroup II and the elimination of genogroup VII. Genogroups I-III contain A and B sub-genogroups (Hollinger and Emerson 2007).
The HAV genotypes are phylogenetically distinct and have different preferred hosts. For example, genotypes, I-III and IV-VI infect humans and simians, respectively. Human genotypes infect all species of primates including humans, chimpanzees, owl monkeys and marmosets, whereas simian genotypes infect non-human primates including green monkeys and cynomolgus monkeys (Aggarwal and Naik 2008). Characterization of these genotypes has been useful in outbreak investigations for tracing infection sources; virus strains within these genotypes have over 85 % genetic similarity (Cromeans et al. 2001; Niu et al. 1992). There is a single serotype for all HAV genotypes. Mutation rates for HAV are much lower than those reported for other picornaviruses, due mostly to constraints of the viral capsid being unfavorable to amino acid substitutions (Cristina and Costa-Mattioli 2007).
2.3 Growth and Biological Properties
The HAV can be cultured in several different primate cell lines including African green monkey kidney cells (BSC-1), fetal rhesus monkey kidney cells (FRhK-4 and FRhK-6) and human fibroblasts (HF), but wild type strains are difficult to culture and generally do not produce CPE in cell cultures. Immunofluorescence is often used for detection of HAV antigen in infected cells because of the lack of CPE. The virus is usually slow-growing and the yield in cell cultures is low compared to most other picornaviruses. Consequently it is difficult to identify the virus in clinical, food or environmental sources by culture alone. Under normal conditions, the virus requires 3 weeks for in vitro growth. Laboratory-adapted strains such as HM 175 are able to produce CPE and have been used extensively in research studies. These strains require less time for in vitro growth and produce visible CPE or plaques. Molecular techniques, including culture-PCR, have become the method of choice for detection of HAV in non-human samples. In humans, clinical diagnosis is usually based on the patient’s immune response. The HAV antigens are conserved and antibodies are generated against a single antigenic site comprised of amino acid residues of VP3 and VP1 proteins on the virus surface.
The virus is very stable, showing high resistance to chemical and physical agents such as drying, heat, low pH and solvents and has been shown to survive for over 3 months in the environment, including seawater and marine sediments (Sobsey et al. 1988). The virus exhibits greater thermal stability at high temperatures when compared to norovirus surrogates. The resistance of HAV to heat is greater in foods and shellfish due to reduced heat transfer and protection by the shellfish tissue. Under refrigeration and freezing conditions the virus remains intact and infectious for several years. It is also resistant to drying, remaining infectious for over 1 month at 25 °C and 42 % humidity, and shows even greater resistance at low humidity and low temperatures. The survival of HAV on fresh and semi-dried tomato (SDT) surfaces was investigated following a recent outbreak of HAV. Results showed that inactivation of HAV on SDT using chemicals or heat was difficult and that it was important to inactivate HAV prior to or during the manufacture of SDT because, following manufacture, any HAV remaining on SDT could retain infectivity at both room temperature and at 5 °C for periods beyond the shelf life of the product (Greening and Hewitt 2012).
In other studies, 2–5 log10 of virus were inactivated following exposure to 70 % alcohol for 3 min; however, it was resistant to several preservatives and solvents including chloroform, Freon, Arklone and 20 % ether. In addition, HAV was not inactivated by 300 mg/L perchloroacetic acid or 1 g/L chloramine at 20 °C for 15 min (Hollinger and Emerson 2007) although it was susceptible to formalin (3 % for 5 min or 8 % for 1 min at 25 °C), iodine (3 mg/L for 5 min) and ß-propiolactone (0.03 % for 72 h at 4 °C) (Hollinger and Emerson 2007). The virus is stable at pH 1.0 and survives acid marination at pH 3.75 in mussels for at least 4 weeks (Hewitt and Greening 2004; Hollinger and Emerson 2007). Gamma irradiation is not effective for inactivation of HAV on fresh fruits and vegetables and high doses of ultraviolet radiation are required for inactivation (Hollinger and Emerson 2007). Hydrostatic pressure, now used as an isothermal preservation method for perishable foods, inactivated HAV following 5 min exposure at 400 MPa (Kingsley 2013). Free chlorine concentrations of less than 10 ppm inactivate HAV at room temperature when sufficient exposure times are provided (5–15 min) and organic solids contribute minimally to chlorine demand (Hollinger and Emerson 2007). Like many enteric viruses, fecal material and virus aggregation provide protection to HAV against chemical and physical assaults. Overall HAV exhibits greater resistance to stressors than other picornaviruses.
2.4 Infection and Disease
The HAV infects the epithelial cells of small intestine and hepatocytes causing elevation of liver enzymes and inflammation of the liver. Cytotoxic T-cell immune response destroys infected liver cells releasing the virus particles into the bile duct from where they are excreted in the feces. The virus is believed to initially enter the liver via the bloodstream and it is not clear if intestinal replication occurs. The disease has an incubation period of 2–6 weeks with an average of 28 days. Initially the symptoms are non-specific and include fever, headache, fatigue, anorexia, dark urine, light stools, and nausea and vomiting with occasional diarrhea. One to two weeks later, characteristic symptoms of hepatitis such as viremia and jaundice appear. Peak infectivity occurs in 2 weeks preceding the onset of jaundice and the virus is present in the blood at 2–4 weeks. The virus is shed in large numbers (>106 particles/g) in feces from the latter 2 weeks of the incubation period and for up to 5 weeks. Jaundice is usually evident from week 4–7 and virus shedding generally continues throughout this period.
Diagnosis is based on the detection of anti-HAV IgM antibody, which can be detected before the onset of symptoms but becomes undetectable within 6 months of recovery. Acute hepatitis is usually self-limiting, but overall debility lasting several weeks is common and relapses may occur. The HAV has not been associated with development of chronic liver disease but on rare occasions, fulminant disease that results in death may occur. Because the onset of symptoms occurs several weeks after infection, it is rare to have the suspected food available for analysis. A killed vaccine that provides long-lasting immunity has been commercially available since 1995 and is commonly given to travelers at high risk. It is now a part of the childhood vaccination schedule in the US, as recommended by the CDC. This vaccine could be used in the food industry to immunize food workers to reduce the risk of food contamination by these workers.
2.5 Foodborne Disease
The HAV has been associated with many outbreaks of foodborne disease; contamination generally occurring either pre-harvest or during food handling. There are a number of documented outbreaks of disease resulting from consumption of HAV-contaminated shellfish, the largest of which occurred in China in 1988 when approximately 300,000 people were infected following consumption of partially cooked clams harvested from a growing area impacted by raw sewage (Halliday et al. 1991). Other shellfish-associated outbreaks include oysters in Australia (Conaty et al. 2000), oysters in Brazil (Coelho et al. 2003), mussels in Italy (Croci et al. 2000) and clams in Spain (Bosch et al. 2001). In most of these outbreaks sewage was generally the source of pollution. Contamination of shellfish with HAV is still common in Italy, Spain and other European countries. Pre-harvest contamination of fruits and vegetables, including strawberries (Niu et al. 1992), raspberries (Ramsay and Upton 1989; Reid and Robinson 1987), blueberries (Calder et al. 2003), frozen pomegranate seeds (Anonymous 2013), lettuce (Pebody et al. 1998), semi-dried tomatoes (Donnan et al. 2012; Petrignani et al. 2010) and green onions (CDC 2003), has also been reported and has resulted in outbreaks of disease in countries such as Finland, the Netherlands, the United States, Australia and New Zealand, where populations have low or no immunity to the disease (Calder et al. 2003; Donnan et al. 2012; Pebody et al. 1998). The source of contamination in these outbreaks was reported to be either infected food handlers or contaminated irrigation waters.
The other main source of HAV infection is from food handlers and food processors . Since HAV is shed before symptoms become apparent (as much as >106 infectious virus particles can be excreted per gram of feces), HAV-infected produce harvesters and food handlers, without knowing, may become a source of contamination. In areas with poor hygiene practices, this can present a very high risk to human health. Foodborne outbreaks of HAV are relatively uncommon in develo** countries where there are high levels of immunity in the local population, but tourists in these regions can be susceptible if they are not vaccinated.
3 Hepatitis E Virus
3.1 Distribution and Transmission
The hepatitis E virus (HEV) is a major etiologic agent of enterically transmitted hepatitis in humans and domestic swine worldwide. In endemic regions of the world, Global Burden of Disease estimates are 20 million infections, 3.4 million symptomatic illnesses, 70,000 deaths and 3000 stillbirths (Dalton et al. 2013). In India, mortality estimates among pregnant women reach 1000 per year (Dalton et al. 2013). Waterborne outbreaks and secondary person-to-person spread involving thousands and even tens of thousands of persons have been reported in China, India, and Africa (CDC 2013; Kamar et al. 2012). In developed countries, sources of HEV infection in humans are largely unrecognized but evidence for zoonotic and foodborne transmission is emerging. In fact, HEV is now regarded as a significant emerging zoonotic and potential foodborne pathogen by the European Food Safety Authority (EFSA 2011). Seroprevalence rates of 16–29 %, and as high as 52 % in a hyperendemic region of Southern France, have been reported among adults in Europe. Discrepancies between seroprevalence and clinically confirmed cases suggest that asymptomatic infections and underreporting are common.
3.2 Taxonomy and Morphology
The HEV was first isolated and identified by Balayan et al. (1983) in acute and convalescent specimens collected from a case of non-A, non-B hepatitis (Balayan et al. 1983). The HEV is 27–34 nm, non-enveloped virus with positive-sense, single-stranded RNA (linear genome of 7.2 kb) (Table 2.1). The capsid symmetry is icosohedral and the buoyant density in potassium tartrate—glycerol gradient is 1.29 g/ml. Virus particles isolated from serum associate with lipids and therefore have a lower density (1.15–1.16 g/ml) in sucrose fractions than do HEV isolated from feces (1.27–1.28 g/ml) (Kamar et al. 2012). The HEV was originally classified in the Caliciviridae family because of similarities in structural morphology and genome organization but was later reclassified under Togaviridae because of similarities between the replicative enzymes of HEV and the togaviruses. Until very recently, the International Committee on Taxonomy of Viruses (ICTV) classification placed HEV under a new family Hepeviridae under the single genus Hepevirus (Van Regenmortel 2000). The family has since been divided into two genera; Orthohepevirus, which infects mammalian and avian species and Piscihepevirus, which includes only the cutthroat trout virus (Smith et al. 2014). While there are four groups of orthohepevirus (groups A-D), only group A is known to infect humans (Smith et al. 2014). Within group A, there are four HEV genotypes (HEV1-HEV4) that infect humans and other mammals but only a single serotype (Dalton et al. 2013).
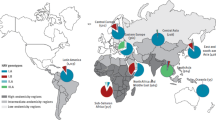
The HEV1, HEV2, HEV3 and HEV4 can be further divided into at least 5, 2, 3 and 7 subgenotypes, respectively (Kamar et al. 2012). The HEV1 and HEV2 primarily cause disease in areas of the world where water quality and sanitation are inadequate; HEV1 primarily circulates in Southeast Asia and Africa while HEV2 has been detected in Mexico and parts of Africa. The HEV3 is detected worldwide but HEV4 has primarily been detected in Southeast Asia and recently in Europe. Historical evidence suggests HEV1 and/or HEV2 circulated in Europe and the United States at the turn of the twentieth century, but disappeared with water and sanitation improvements after World War II (Dalton et al. 2013).
The HEV3 primarily circulates in swine and wild boars worldwide but occurs mainly in China and Japan. Swine and human strains of HEV share close sequence homology. Both HEV3 and HEV4 strains have been detected in retail pork products (Berto et al. 2013; Berto et al. 2012; Colson et al. 2010) and epidemiological investigations strongly point to human infections caused by consumption of pork products and game meat (Li et al. 2005; Masuda et al. 2005; Matsubayashi et al. 2008; Matsuda et al. 2003) and deer (Mushahwar 2008; Takahashi et al. 2003; Tei et al. 2003). Other mammals such as rats, bats, rabbits and ferrets are known to harbor HEV, but no cases of human disease have been associated with these animals. Contamination of water, shellfish and fresh produce with HEV has also been documented, suggesting the occurrence of non-zoonotic sources of foodborne infections and/or water and crop contamination with swine or other animal waste (Meng 2011). Blood transfusions and organ transplants are another significant source of HEV infection in the developed world (Mushahwar 2008). Secondary person-to-person transmission is relatively uncommon and is estimated at 0.7–8.0 % (Cromeans et al. 2001).
3.3 Growth and Biological Properties
In vitro growth in cell c ulture has only recently been possible for HEV1, HEV3 and HEV4. Hepatic carcinoma (PRC/PRF/5) and lung carcinoma (A549) cell lines support the growth of these genotypes of HEV (Kamar et al. 2012). An HEV3 strain from a chronically infected patient has been adapted to grow in HepG2/C3A hepatoma cells (Kamar et al. 2012).
3.4 Infection and Disease
The HEV produces Acute Jaundice Syndrome (AJS) that does not obviously differ from the disease caused by HAV. Asymptomatic infections exceed the number of clinical illnesses. Following a 2–8 week incubation period, symptoms of viremia, nausea, fever, abdominal pain, arthralgia, dark urine and general malaise may develop in addition to the classic appearance of jaundice. In develo** countries, where HEV1 and HEV2 predominate, case fatality rates during epidemics have been reported between 0.2 and 4 % for non-pregnant persons, with higher mortality in children under 2 years of age. Mortality rates for pregnant females are as high as 10 % and are more likely to occur in the third trimester.
In developed countries where HEV3 and HEV4 predominate, the majority of infections are asymptomatic. Clinical (icteric) infections are generally mild and self-limiting, lasting 4–6 weeks unless an underlying chronic liver disease is present. Excess fatalities among pregnant women have not been reported for HEV3 or HEV4 (Dalton et al. 2013). Symptomatic infection is reported to be 3 times more common in middle-aged and elderly men than women, even though seroprevalence rates in men and women are similar. Reasons for this discrepancy are not clear, but are probably linked to excessive alcohol consumption among a cohort of this population. Chronic infection occurs primarily among immunosuppressed patients, particularly solid organ transplant recipients. It is estimated that HEV prevalence among transplant patients is 1.0–2.3 % and although infection is usually asymptomatic, approximately 10 % of exposed patients develop cirrhosis within 2 years. Infrequently, neurological disorders, encephalitis and muscular impairments (including Guillain-Barré syndrome) have resulted from acute and chronic infection with HEV3 and possibly also HEV1. Viremia and virus excretion in feces through bile begins 2 weeks before the peak elevation of liver enzymes (and symptoms, if present) and continues until the enzyme levels return to normal (up to 2–3 weeks after symptoms appear). Diagnosis is generally by detection of IgM and IgG in patients’ sera or by molecular detection of the virus in feces or sera. A recombinant vaccine was licensed in China in 2012 but has not yet received WHO recommendation (Dalton et al. 2013).
3.5 Foodborne Disease
Water contaminated with human and/or swine waste can harbour HEV allowing it to enter the food chain if used for shellfish production or irrigation. Similarly, fecal contamination of run-off waters from pig farms or from lands spread with untreated pig manure could contaminate irrigation and surface waters with subsequent HEV contamination of fruits, vegetables and shellfish. The virus has been detected in raw sewage, river water, shellfish and seawater in Europe, Japan, Southeast Asia, New Zealand, UK and the U.S. (Clemente-Casares et al. 2003; Crossan et al. 2012; Ishida et al. 2012; Jothikumar et al. 1993; Masclaux et al. 2013; Pina et al. 2000; Pina et al. 1998; Williamson et al. 2011). Therefore, consumption of raw or undercooked shellfish is a risk factor for HEV infection and has been implicated as the source of sporadic cases occurring in Europe and Southeast Asia (Cacopardo et al. 1997; Koizumi et al. 2004). In addition, HEV has been detected on strawberries irrigated with river water under experimental conditions (Brassard et al. 2012), providing evidence for HEV contamination through irrigation water. In a study where enteric viruses were traced through a food production chain, 1 of 38 samples of frozen raspberry tested positive for HEV, but the source (water or human/animal contact) of viral contamination could not be definitively identified (Maunula et al. 2013).
3.6 Zoonotic Transmission
The HEV has now been established as a zoonotic pathogen. Swine are the primary reservoir for HEV3 and HEV4 strains but infections have been reported in a wide range of wild and domestic animals. Human HEV3 and HEV4 strains can easily infect pigs under experimental conditions indicating a zoonotic origin for these viruses, a property not shared by human HEV1 and HEV2 strains (Meng 2011). The virus replicates in the liver and intestine and is shed in the feces and bile of swine for 3–5 weeks following infection (Halbur et al. 2001). It is highly contagious and therefore can spread among herds of domestic pigs very efficiently (Dalton et al. 2013). Swine veterinarians and handlers are significantly more likely to be seropositive for anti-HEV antibodies (Meng 2011), a finding consistent with HEV transmission through contact or environmental exposure.
Animal meat can also be contaminated with HEV via infection of the liver or by contact with infected feces during animal dressing or meat processing. A recent study conducted in the United States showed that 11 % of pig livers tested positive for HEV RNA and the virus was infective (Feagins et al. 2007). In Japan, 2 % of commercial pig livers were HEV positive and the strains were closely related to those detected in HEV-infected humans (Yazaki et al. 2003). Consumption of raw or undercooked pig and wild boar livers was a risk factor for several sporadic HEV illnesses recently reported in southeast Asia and Europe (Colson et al. 2010; Li et al. 2005; Masuda et al. 2005; Matsubayashi et al. 2008; Matsuda et al. 2003). Zoonotic transmission of HEV was also reported after consumption of raw deer meat by two Japanese families (Takahashi et al. 2004; Tei et al. 2003). Tei et al. (2004) investigated the risks associated with consumption of uncooked deer meat in a case control study and found that, in the area studied, eating uncooked deer meat was a risk factor (Tei et al. 2004).
4 Norovirus
4.1 Distribution and Transmission
Noroviruses, previously known as small round structured viruses (SRSVs) and Norwalk-like viruses (NLVs) , are now the most widely recognized viral agents associated with food and waterborne outbreaks of non-bacterial gastroenteritis and probably the most common cause of foodborne disease worldwide. The prototype norovirus, the Norwalk virus, was first discovered by Kapikian et al. (1972) following an outbreak of gastroenteritis in a school in Norwalk, Ohio (Kapikian et al. 1972). Immune electron microscopy was used to examine feces from volunteers who consumed fecal filtrates from infected cases (Dolin et al. 1971; Kapikian et al. 1972). At that time, most cases of gastroenteritis that could not be attributed to a bacterial agent were termed as acute nonbacterial gastroenteritis of unknown etiology. The discovery of Norwalk virus provided the first evidence of a viral etiology for human diarrheal disease. Despite this discovery, noroviruses remained largely unrecognized until about 20 years ago because their detection was technically difficult and because the illness was generally thought to be mild and short-lived and so was frequently not reported to public health authorities.
Noroviruses are primarily transmitted by direct person-to-person spread, via the fecal-oral route, or by aerosolized vomit. Indirect transmission can also occur after consumption of fecally contaminated food or water, or after contact with contaminated surfaces, including high-touch surfaces (i.e. door handles, faucets, utensils) or those impacted by an ill person’s vomitus. Outbreaks commonly occur in closed community situations such as rest homes, schools, camps, hospitals, resorts and cruise ships where many high-touch surfaces and food and water sources are shared. Since norovirus infections are often not notifiable, the global burden of disease is not known and is generally grossly under-reported particularly in develo** countries. However, some of the disease burden is recorded in many developed countries through the notification of gastroenteritis outbreaks to the public health disease surveillance systems. Human noroviruses cause ~90 % of all outbreaks of non-bacterial gastroenteritis and ~50 % of all-cause outbreaks worldwide (Patel et al. 2009). The National Outbreak Reporting system (NORs), launched in 2009 by the CDC in the United States, determined that norovirus was responsible or suspected in 89 % of all outbreaks of gastroenteritis with a known etiology (Wikswo and Hall 2012).
Noroviruses are also responsible for approximately 58 % of foodborne disease in the US, including 5.5 million cases, 26 % of hospitalizations and 11 % of deaths related to foodborne disease each year (Scallan et al. 2011). In New Zealand, norovirus is the most frequently reported agent for gastroenteritis outbreaks. Between 2001 and 2007, 809 reported outbreaks of norovirus infection involving a total of 18,508 cases, were reported in annual surveillance reports (Greening et al. 2009). Norovirus was also confirmed as the cause of 1206 gastroenteritis outbreaks between 2002 and 2009, of which 64.6 % occurred in healthcare settings and 16.6 % were associated with catered settings and shellfish consumption (Greening et al. 2012). Recent estimates published by the Food-borne Viruses in Europe Network indicated that 21 % of all norovirus outbreaks are estimated to be due to foodborne transmission (Verhoef et al. 2010). Although noroviruses contribute significantly to foodborne disease, the primary means of norovirus transmission appears to be person-to-person worldwide.
4.2 Taxonomy and Morphology
There are five genera in the family Caliciviridae: Norovirus and Sapovirus are human pathogens while Lagovirus, Vesivirus, and the newly discovered Nebovirus infect animals and are not known to be pathogenic for humans. Two additional genera, Recovirus and Valovirus, have recently been proposed. The former includes the Tulane virus which was isolated from rhesus macaques (Farkas et al. 2008) and the latter, St-Valérien-like viruses, which have been isolated from swine (L’Homme et al. 2009). The ‘Norwalk-like viruses’ and ‘Sapporo-like viruses’ were renamed as Norovirus and Sapovirus in August 2002 by the ICTV (Van Regenmortel 2000). The noroviruses do not show the characteristic cup-shaped morphology of caliciviruses but instead show a “fuzzy” or ragged appearance by direct electron microscopy, which is why they were classified as a distinct group until 1995 (Fig. 2.1a).
The noroviruses are 28–35 nm non-enveloped, linear, positive sense, single-stranded RNA viruses with a genome of approximately 7.4–7.7 kb and icosohedral capsid symmetry (Table 2.1). The buoyant density in cesium chloride gradient is 1.36–1.41 g/ml. The genome is composed of three open reading frames (ORF), which code for the non-structural proteins, including the RNA polymerase in ORF1, the major capsid protein (VP1) in ORF2 and a minor structural protein (VP2) in ORF3. Currently, six norovirus genogroups (GI, GII, GIII, GIV, GV and GVI) have been identified. The majority of human infections are caused by genogroup I and II (GI & GII) strains but infections with GIV strains are sometimes reported. Genogroups I and II contain 9 (GI.1-9) and 22 genotypes (GII.1-22), respectively (Kroneman et al. 2013) (Fig. 2.2). Genogroup II includes three genotypes (GII.11, GII.18 and GII.19) that cause asymptomatic infection in swine. Two genotypes of genogroup III (GIII.1-2) are known to cause diarrhea in bovine calves. Genogroup IV noroviruses have been detected in humans (GIV.1), dogs, lions and cats (animal strains belong to GIV.2) (Martella et al. 2007; Martella et al. 2008b; Pinto et al. 2012). Genogroup V noroviruses are highly prevalent in laboratory mice but are not known to infect other animals (Wobus et al. 2006). The most recently established genogroup VI viruses infect canine species (Green 2013). An international norovirus working group established in 2008 recently published new parameters for norovirus genoty** and proposed a standard nomenclature for reporting purposes (Kroneman et al. 2013). In addition, an online ty** tool (http://www.rivm.nl/mpf/norovirus/ty**tool) is now available for public use.
4.3 Growth and Biological Properties
Most information on the biology and properties of noroviruses has been obtained through studies in human volunteers and laboratory animals with culturable animal caliciviruses. Human volunteer studies primarily conducted in the 1970s (Dolin et al. 1972; Dolin et al. 1971; Green 2007) and more recently in the 2000s (Atmar et al. 2011; Atmar et al. 2008; Hutson et al. 2002; Lindesmith et al. 2003) have almost exclusively been conducted with the prototype GI.1 Norwalk virus, although two studies were performed with GII.2 and GII.4 norovirus (Frenck et al. 2000). In a recent study, HuNoV remained infectious in groundwater for at least 61 days (last collection point for human challenge study) and viral RNA could be detected 3 years after inoculation (Seitz et al. 2011).
Fecal pollution from sewage discharges, septic tank leachates and boat discharges has caused contamination of shellfish beds, recreational water, irrigation water and drinking water. It is probable that noroviruses persist in these environments for extended periods (weeks or months). In infected live oysters, noroviruses were still detectable after 4–6 weeks in natural growing conditions (Greening et al. 2003). Fecal material associated with these viruses and their propensity to aggregate causes them to be more moderately resistant to chemical disinfectants, including free chlorine levels used in drinking water distribution systems. Noroviruses also retain at least partial infectivity after exposure to 20 % ether at 4 °C for 18 h (Dolin et al. 1972; Green 2007). It should be noted, however, that virus titer could not accurately be determined in the early human challenge experiments reviewed in Green (2007). If starting virus titers are high (i.e. ≥8 log per ml), incomplete virus inactivation may be observed even if a disinfectant produces 3–4 log10 reduction in the titers of infectious virus.
4.4 Infection and Disease
Noroviruses are extremely infectious; the 50 % infectious dose of Norwalk (GI.1 strain) virus in humans was recently calculated t o be as low as 18 (Teunis et al. 2008) and as high as 2800 virus particles (Atmar et al. 2014). Very high numbers (1010–1012 per g) of noroviruses can be shed in feces of symptomatic and even asymptomatic persons (Atmar et al. 2008). Symptoms normally include vomiting, diarrhea, nausea, abdominal pain and general malaise, but vomiting can be present without diarrhea and vice versa. Viruses are excreted in vomit and feces during illness and can continue to be shed in decreasing numbers for up to 28 days or longer in stools (Atmar et al. 2008). Symptoms normally develop within 12–48 h of exposure and resolve within 24–60 h. Dehydration is a common complication that can particularly affect the young and elderly, necessitating rehydration therapy. There is no evidence of any long-term sequelae following norovirus infection.
In the absence of reliable laboratory tests for norovirus, Kaplan et al. (1982) developed epidemiological and clinical criteria for the diagnosis of noroviral gastroenteritis outbreaks (Kaplan et al. 1982). These widely used criteria are: stools negative for bacterial pathogens, a mean or median duration of illness of 12–60 h, vomiting in ≥50 % of cases and a mean or median incubation period of 24–48 h. The mechanism of immunity to norovirus infection is not clear. Infection normally stimulates production of both gut and serum antibody and although immunity to the infecting norovirus strain may develop, it is generally short-lived, is strain-specific and does not confer protection against future infection. Re-infection with a different strain can occur soon after the initial infection. Thus, given the genetic variability of noroviruses, people are likely to be re-infected many times during their lifetimes.
Several reports over the last 10 years have revealed an association between histo-blood group antigen (HBGA) expression on a person’s gut mucosal cells and a susceptibility to norovirus infection (Atmar et al. 2011; Hutson et al. 2002; Lindesmith et al. 2003; Tan and Jiang 2010). Persons deemed to be “secretors” are capable of expressing HBGAs on their gastrointestinal cells and secretions, including saliva. Noroviruses are capable of binding to HBGAs and saliva from secretors and the role of HBGAs as receptors or co-receptors for virus attachment and entry into cells has been speculated. Evidence for this was derived from human challenge studies with Norwalk virus (GI.1 prototype) where “non-secretors”, individuals that do not express HBGAs on their GI mucosa, were resistant to symptomatic infection (Atmar et al. 2011; Hutson et al. 2002; Lindesmith et al. 2003; Tan and Jiang 2010). There also appears to be an association with HBGA expression and susceptibility to infection with GII.4 noroviruses (Frenck et al. 2012; Tan and Jiang 2010); although, this association is not as well defined as it is for Norwalk virus. There is also evidence that susceptibility to infection by other norovirus genotypes may not depend on the secretor status (Lindesmith et al. 2005). Considering the genetic diversity of noroviruses, this unfortunately means that there is likely a genotype capable of infecting almost everyone, regardless of their HBGA expression.
Projectile vomiting is a characteristic symptom that can contribute to secondary spread through droplet infection, where droplets containing virus may contaminate surfaces or be swallowed. Evidence that norovirus transmission occurs through aerosolization of vomit was clearly demonstrated at a UK hotel. During a meal, a guest vomited at the table and norovirus infection spread in a radial pattern through the restaurant, progressively decreasing from 91 % attack rate among those seated at the same table to an attack rate of 25 % in those patrons who were seated the furthest distance away from the guest who vomited (Marks et al. 2000). Norovirus infection characteristically has an attack rate of 50–70 % or even higher in some situations. High attack rate, low infectious dose, prolonged virus excretion, short-term immunity and, environmental stability of NoVs contribute to the epidemic nature of noroviral gastroenteritis.
Norovirus infection was historically termed ‘winter vomiting disease’ because outbreaks occurred most frequently in the winter months, especially in rest homes and institutions. This seasonality is still apparent, but NoV outbreaks are also reported throughout the year. Viruses belonging to GII.4 are by far the most frequently reported in outbreaks and sporadic illnesses worldwide. This topic will be discussed in greater detail in Chap. 4 of this book.
4.5 Foodborne Disease
Noroviruses are the main cause of foodborne viral gastroenteritis worldwide with foodborne transmission accounting for a large proportion of NoV outbreaks in many countries. Foodborne norovirus outbreaks resulting from pre-harvest contamination of foods such as shellfish and post-harvest contamination through food handling have been reported worldwide. Among these are several outbreaks resulting from consumption of norovirus-contaminated shellfish (Dowell et al. 1995; Christensen et al. 1998; Berg et al. 2000; Simmons et al. 2001; Bellou et al. 2013), bakery products (Kuritsky et al. 1984; de Wit et al. 2007), delicatessen and ready to eat meats (Schwab et al. 2000; Malek et al. 2009), sandwiches (Parashar et al. 1998; Daniels et al. 2000; CDC 2006), raspberries (Ponka et al. 1999; Hjertqvist et al. 2006; Maunula et al. 2009; Sarvikivi et al. 2012), and water and ice (Beller et al. 1997; Brugha et al. 1999; Beuret et al. 2002). Pre-symptomatic infection in food handlers has also been shown to cause outbreaks of foodborne norovirus infection (Lo et al. 1994; Gaulin et al. 1999; Thornley et al. 2013).
Among the 2922 confirmed or suspected outbreaks of foodborne norovirus illness reported to CDC from 2001 to 2008, the food vehicle could not be determined for 56 % of the outbreaks (Hall et al. 2012). Of the 886 outbreaks where the factors leading to food contamination were indicated, 82 % of outbreaks involved food handler contact and 13 % indicated contamination of the raw product (Hall et al. 2012). Determination of the original source of virus is often problematic because several modes of transmission frequently operate during norovirus gastroenteritis outbreaks. Although the initial transmission route may be through consumption of contaminated foods, secondary transmission via direct contamination of the environment or person-to-person contact also often occurs. This results in wide dissemination where infection quickly spreads through institutions, schools, camps and resorts and cruise ships leading to large-scale epidemics, often with over 50 % attack rates.
The use of DNA sequencing techniques for genoty** of noroviruses has greatly assisted the epidemiological investigation of gastroenteritis outbreaks. The comparison of norovirus sequences from fecal specimens and contaminated foods, such as oysters, can often indicate if it is a common source outbreak or if individual cases are somehow related, particularly when a strain is involved that is not common in the community. In 1993, 23 gastroenteritis outbreaks across six states in the United States were shown to be related to consumption of oysters harvested from a single area and contaminated with the same norovirus strain (Dowell et al. 1995). Validating the source of outbreaks caused by GII.4 strains is often more difficult because these strains can be highly prevalent in the community, particularly during pandemic years. Sequencing either the full capsid-encoding ORF2 or minimally the hypervariable region of ORF2 is needed for molecular epidemiologic investigations of these strains.
4.6 Zoonotic Transmission
To date, zoonotic transmission of noroviruses remains speculative. Despite the presence of GII norovirus strains in swine populations (0.2–25 % detection rate) globally, there is no evidence of human infection by these strains (Mathijs et al. 2012). Similarly, GIII bovine noroviruses have been detected in the stools of diarrheic calves with a 1.6–72 % detection rate (Mathijs et al. 2012). Despite serologic evidence of large animal veterinarians’ exposure to bovine noroviruses (Widdowson et al. 2005), no illnesses have been reported. GIV.1 noroviruses appear to infect only humans and animal strains of GIV norovirus have not been detected in humans. Recombination between strains within the same host species has been reported for human, bovine, canine and mouse noroviruses; however, recombination between strains of different host species has not been confirmed. In the laboratory, HuNoV infection in gnotobiotic pigs and calves (Cheetham et al. 2006; Souza et al. 2008; Takanashi et al. 2011) and non-human primates (Bok et al. 2011; Rockx et al. 2005) has been extensively studied as models for viral pathogenesis, immunology and response to vaccination (Tan and Jiang 2010). Only two reports to date provide evidence of animals as reservoirs for human noroviruses. In one study, human norovirus-like sequences were detected in the feces of livestock (cows and pigs) (Mattison et al. 2007). Human norovirus RNA was also detected in the feces of pet dogs from households where symptoms of gastroenteritis were reported, suggesting a potential role for dogs in HuNoV transmission (Summa et al. 2012). However, based on current evidence it seems more likely that dogs are the recipients of spill-over from the human population rather than being a reservoir.
5 Sapovirus
5.1 Distribution and Transmission
The sapoviruses, formerly described as the “Sapporo-like viruses” or SLVs , also belong to the Caliciviridae family and cause gastroenteritis among both children and adults. Sapoviruses were first identified in 1977 after a gastroenteritis outbreak in a children’s home in Sapporo, Japan. Sapoviruses were once thought to be primarily associated with pediatric diarrhea in infants since infections among adults were less frequently reported and were less severe than those caused by HuNoVs (Hansman et al. 2007a). Diagnostic testing for sapovirus is, therefore, infrequently performed during routine outbreak investigations or after emergency room visits. However, outbreaks of sapovirus gastroenteritis among adults and elderly persons are increasingly reported worldwide (Pang et al. 2009; Svraka et al. 2010). In addition, the emergence of specific sapovirus strains (GI.2 and GIV) has correlated with its increased occurrence (Gallimore et al. 2006; Khamrin et al. 2007; Lee et al. 2012; Svraka et al. 2010). Sapovirus infections occur throughout the year, but the frequency is higher during the winter and spring months. Person-to-person transmission is believed to be the most common route, although several foodborne outbreaks have been reported (Hansman et al. 2007b; Iizuka et al. 2010; Kobayashi et al. 2012; Nakagawa-Okamoto et al. 2009; Noel et al. 1997; Ueki et al. 2010; Yamashita et al. 2010).
5.2 Taxonomy and Morphology
Sapoviruses show a Star-of-David structure under EM, with distinct cup-shaped indentations typical of caliciviruses on the surface and/or ten spikes on the outline of the virions. The sapoviruses are 30–38 nm, non-enveloped, positive sense, single-stranded RNA viruses with a genome of approximately 7.1–7.7 kb and icosohedral capsid symmetry (Table 2.1) (Oka et al. 2015). ‘Sapporo-like viruses’ were renamed as Sapovirus in 2002 by the ICTV (Van Regenmortel 2000). There are currently five sapovirus genogroups (GI-GV), but eight additional genogroups (GVI-GXIV) have been proposed (Oka et al. 2015). GI, GII, GIV and GV viruses infect humans. Based on the nucleic acid sequence of the major capsid protein (VP1), human sapoviruses are further divided into at least seven GI and GII genotypes, one GIV genotype and two genotypes of GV (Oka et al. 2012; Oka et al. 2015). GV genotypes also have been detected in pigs and sea lions (Oka et al. 2015). Of the additional proposed genogroups, three infect swine (GVI, GVII and GVIII) (Scheuer et al. 2013). The other proposed genogroups of sapovirus have been detected in swine, mink, dogs, and bats (Scheuer et al. 2013).
5.3 Growth and Biological Properties
A majority of sapovirus strains are not capable of growth in cell culture. Detection and identification is generally by molecular methods, most c ommonly RT-PCR (Green 2007; Hansman et al. 2007a). However, the GIII-Cowden strain of porcine sapovirus (historically referred to as porcine enteric calicivirus or PEC) has been adapted to grow in a continuous swine kidney cell line (LLC-PK). Its culture depends on supplementation of media with glycochenodeoxycholic acid (GCDCA), a bile acid (Chang 2004). This strain has recently been proposed as a surrogate for HuNoVs to be used in disinfection and survival studies (Wang et al. 2012).
5.4 Infection and Disease
Although previously thought to cause primarily diarrhea, a high percentage (37–89 %) of vomiting among cases have recently been reported (Chhabra et al. 2013; Iizuka et al. 2010; Kobayashi et al. 2012; Lee et al. 2012; Yamashita et al. 2010; Yoshida et al. 2009). In fact, the clinical symptoms, virus shedding, and epidemiological features (incubation period, duration of illness) of epidemic sapovirus are nearly identical to those of noroviruses. It is hypothesized that using the Kaplan criteria alone for diagnosis of outbreaks may result in an overestimation of norovirus and an underestimation of sapovirus (Lee et al. 2012). Severe gastrointestinal illnesses and even deaths due to sapovirus do occur, but are infrequently reported. In a recent study, norovirus- and rotavirus- negative clinical specimens collected from children seeking medical attention for acute gastroenteritis were screened for less common agents of viral gastroenteritis; 5.4 % were positive for sapoviruses (Chhabra et al. 2013). However, determining sapovirus as the causative agent of gastroenteritis is sometimes difficult, particularly for sporadic cases, due to the common presence of other gastroenteritis-causing viruses in fecal specimens and high rates of asymptomatic carriage. In one study, 4.2 % of the healthy control specimens tested positive for sapovirus and mixed infections with rotavirus, norovirus, astrovirus and adenovirus were reported (Chhabra et al. 2013). High levels of sapovirus shedding (106–1011 per g) in stools from both symptomatic and asymptomatic persons have been reported (Yoshida et al. 2009). While the infectious dose is not known, it is thought to be low and similar to that for noroviruses.
5.5 Foodborne Disease
Food handler contamination of RTE foods and incidences of contaminated shellfish harvesting waters are increasingly being reported. One of the first food-related outbreaks of sapovirus gastroenteritis occurred among adults at a school in Parkville, Maryland, in 1997 (Noel et al. 1997). In Japan, there have been several reports of sapovirus outbreaks due to the consumption of oysters (Nakagawa-Okamoto et al. 2009; Ueki et al. 2010) and clams (Hansman et al. 2007b; Iizuka et al. 2010). A large food handler-associated outbreak was reported among 109 wedding guests served boxed lunches (Yamashita et al. 2010). In January 2010, the largest outbreak of sapovirus ever to be reported in Japan (655 persons; 17 % of persons served) was also caused by boxed lunches contaminated by food handlers (Kobayashi et al. 2012).
5.6 Zoonotic Transmission
There are no reports of zoonotic transmission of sapoviruses to date. However, the potential exists as intra- and inter-genogroup recombination has been reported (Hansman et al. 2007a; Wang et al. 2005). Porcine sapoviruses co-concentrated with other human enteric viruses have been detected in raw US oysters, revealing a potential vector for mixed infections and recombination (Costantini et al. 2006). In addition, closely related GVIII sapovirus strains have been detected in humans and swine indicating possible transmission of GVIII strains from humans to pigs or vice versa (Martella et al. 2008a; Scheuer et al. 2013).
6 Rotavirus
6.1 Distribution and Transmission
Acute gastroenteritis caused by rotaviruses is a common disease of infants and young children worldwide, which can lead to severe illness and deaths especially in locations where medical services are not readily accessible. Although the disease occurs in all age groups, it is generally considered to be a mild infection in adults; hence, the true extent of adult infections is not known. Since the licensing of two live, oral, second-generation rotavirus vaccines in 2006, there has been a marked decline in the number of diarrheal illnesses caused by rotaviruses in young children, particularly in the developed world. In the United States, where rotaviruses were estimated to cause about 3 million infections, 70,000 hospitalizations and nearly 100 deaths annually, the impact of routine childhood vaccination on the reduction of rotavirus infections is already apparent (Glass et al. 2011; Malek et al. 2006; Parashar et al. 2006a).
Vaccination of U.S. children with RV5 RotaTeq® (Merck and Company, Inc.) has decreased the number of hospitalizations due to rotaviruses by up to 89 % (Cortes et al. 2011). In addition, the annual number of diarrheal illnesses due to rotavirus has also been in steady decline (Glass et al. 2011; Tate et al. 2011). The pentavalent RV5 and monovalent RV1 Rotarix® (GlaxoSmithKline) vaccines have been recommended by WHO for all regions of the world since 2009 (WHO 2009) and have been licensed in more than 100 countries (Glass et al. 2011). In many regions of the world, rotaviruses are still a major cause of severe acute gastroenteritis, causing more than 100 million cases worldwide of childhood diarrhea, 2.4 million hospitalizations and 500,000 deaths in children under the age of 5 years in develo** countries at the time of vaccine release (Greenberg and Estes 2009; Malek et al. 2006; Parashar et al. 2006a; Parashar et al. 2006b). Although it is clear that second-generation vaccines have had a significant impact on several middle- and high-income countries, vaccine efficacy has generally not been as high as in low-income countries, for reasons not entirely known (Glass et al. 2011; Jiang et al. 2010; Yen et al. 2011). As the poorest regions of the world suffer the greatest numbers of severe illnesses and deaths due to rotavirus, there is a critical need to understand the underlying causes of this disparity and improve vaccination efficacy in these populations.
Rotaviruses are transmitted by the fecal-oral route and cause disease in both humans and animals, especially domestic animals, with subsequent serious economic loss. Although the animal and human strains are usually distinct, some human strains are closely related to animal strains and cross-species infections do occur (Sattar and Tetro 2001). Rotaviruses can be excreted in human stool at concentrations of up to 1012 virus particles per g of feces, making them highly transmissible through direct person-to-person contact and by contaminated fomites (Bishop 1996). Transmission of rotavirus via aerosolized droplets following a vomiting event has not been confirmed. As few as ten virus particles appear to be sufficient for causing infection in humans (Graham et al. 1987). Infection is generally not recognized as being foodborne but outbreaks associated with food and water have been reported from a number of countries (Sattar and Tetro 2001).
6.2 Taxonomy and Morphology
Rotaviruses are classified in the genus Rotavirus in the family Reoviridae, a large family comprised of two virus subfamilies, Spinareovirinae and Sedoreovirinae, which include nine and six genera, respectively (Carstens 2010). Rotaviruses belong to the Sedoreovirinae subfamily. Electron micrographs of rotaviruses show a characteristic wheel-like appearance, hence the name ‘rotavirus’, derived from the Latin meaning ‘wheel’ (Fig. 2.1b). These viruses are distinct in that they have a complex, segmented genome that undergoes reassortment during replication. There are eight groups (also termed species) within the Rotavirus genus, designated A-H (Desselberger 2014). Group A rotaviruses are most commonly associated with human disease; infection with Groups B and C is rarely reported. Group A rotaviruses are also common agents of disease in cattle and several other domestic animal species (equine, porcine, ovine, caprine, canine, feline (rare), and poultry (rare)) (Dhama et al. 2009). In addition, Groups C and E rotaviruses infect swine; Groups D, F and G affect poultry; and Group B viruses have been detected in young cattle, swine and sheep, although rarely (Dhama et al. 2009). Initially isolated from humans but unassigned to a rotavirus group until recently, Group H rotaviruses have been reported to infect both humans and piglets (Molinari et al. 2014).
Rotaviruses are 60–80 nm, non-enveloped viruses with icosohedral capsid symmetry and a linear, segmented, double stranded RNA genome. The 16–27 kb genome is enclosed in a triple layered capsid composed of a double protein shell and an inner core. The 11 segments of RNA code for 11 proteins (six structural and five non-structural). Their classification has been traditionally based on the antigenic properties of two structural proteins, VP7 (G-type glycoprotein) and VP4 (P-type protease-sensitive protein), which comprise the shell and spike proteins of the outer capsid, respectively, and are important in virus infectivity and immunogenicity. The proteins have been used to define P and G serotypes of rotaviruses (Estes and Kapikian 2007). However, seroty** is time consuming and immunological reagents are not always readily available. While there is good correlation between G serotypes and VP7 genotypes, P serotype and VP4 genoty** results are not always in agreement (Greenberg and Estes 2009), so classification is now mainly based on sequencing of these genes or a double nomenclature for P types, based on genotype and serotype information (Desselberger 2014). Genoty** by sequencing is based on identities between sequences of cognate gene segments. There are at least 27 G genotypes and 37 P genotypes within the Rotavirus A (RVA) species (Desselberger 2014). Predominant strains circulating globally include six G types (G1-4, G9, and G12) and two P types (P[4] and P[8]). The six G- and P-type combinations accounting for 80–90 % of all rotavirus infections in North America, Europe and Australia include, G1P[8], G2P[4], G3P[8], G4P[8] and G9P[8] and G12P[8] (Desselberger 2014). In Africa, G5, G6 and G8 types predominate (Desselberger 2014). A Rotavirus Classification Working Group (RCWG) charged with develo** a genome classification system for RVA was recently formed to address the lack of uniformity in the literature (Matthijnssens et al. 2008). In 2008, abbreviations for all 11 RNA segments were defined and percent cut-off values established for categorizing rotavirus strains using a common nomenclature (Matthijnssens et al. 2008). Furthermore, the RCWG proposed a standardized strain nomenclature system for reporting complete rotavirus genome sequences and for use in epidemiologic studies (RV group/species of origin/country of identification/common name/year of identification/G- and P-type). Since this time, 50 new genotypes have been reported and in several cases, a link between animal and human strains has been revealed (Greenberg and Estes 2009).
6.3 Growth and Biological Properties
Although many rotaviruses can be grown in cell cultures, they have proved difficult to cultivate in vitro and growth is restricted to a few cell lines derived mainly from monkey kidneys. Addition of trypsin to the culture medium is required to enhance viral growth in cell cultures. Rotaviruses do not show the same tolerance to extreme conditions as other enteric viruses although they are stable in the environment and can be stored for several months at 4 °C or even at 20 °C. They are resistant to drying and may survive on fomites and surfaces, but are labile under conditions of high relative humidity (approximately 80 %) (Estes and Kapikian 2007). Heating at 50 °C for 30 min reduces their infectivity by 99 % and infectivity is rapidly lost at pH <3.0 and >10.0. Repeated cycles of freeze-thaw can also destroy infectivity. The viruses are resistant to solvents such as ether and chloroform and to non-ionic detergents such as deoxycholate. Chelating agents such as EDTA disrupt the outer shell and inactivate rotaviruses. Treatment with disinfectants such as chlorine, phenol, formalin and 95 % ethanol is also effective against rotavirus (Estes and Kapikian 2007). Normal cooking temperatures are usually sufficient to inactivate rotaviruses. The viruses are found in water and sewage, are resistant to chlorine levels present in the drinking water distribution system and are persistent in the environment. Human rotavirus can survive for several weeks in river water at 4 and 20 °C.
6.4 Infection and Disease
The incubation period for rotavirus infection is 1–2 days. The characteristic symptoms of vomiting and watery diarrhea develop quickly and persist for 3–8 days, frequently accompanied by fever and abdominal pain. Dehydration is a key factor that contributes to the high infant death rate from rotavirus disease, especially in develo** countries where rehydration therapy is often not readily available. Virus is shed in feces for 5–7 days. The main transmission route is fecal-oral. Since rotaviruses most often infect young children, the major route of transmission is believed to be person-to-person through care-givers and the general adult population. Rotaviruses, particularly group B, can also infect adults and have been occasionally associated with food and water outbreaks. In the early 1980s, a large waterborne epidemic affecting nearly 1 million persons was reported in China (Hung et al. 1984). Waterborne outbreaks have also been reported from Germany, Israel, Sweden, Russia, Turkey and the US (Ansari et al. 1991; Koroglu et al. 2011; Sattar and Tetro 2001). Rotavirus infections are more common during the winter months in countries with a temperate climate. In tropical regions, outbreaks can occur in cool, dry months as well as throughout the year especially when transmission is related to contaminated water supplies or in the absence of sewage treatment systems (Ansari et al. 1991; Cook et al. 1990).
6.5 Foodborne Disease
A case–control study examining risk factors outside the home implicated contact with a person suffering from gastrointestinal illness and poor hygienic kitchen practices as major contributors to the likelihood of contracting rotavirus infections (de Wit et al. 2003). Cross-contamination of foods during preparation in the home may be an important source of infection for children, particularly for weaning infants (Motarjemi et al. 1993). Eleven foodborne outbreaks consisting of 460 cases of rotaviral gastroenteritis were reported in New York between 1985 and 1990. Seven of these outbreaks were associated with food-service premises and the implicated foods included salad, cold foods, shepherd’s pie, and water or ice (Sattar and Tetro 2001). In Japan, a foodborne rotavirus outbreak was reported among adults eating restaurant-prepared meals (Iizuka et al. 2000). College-age students in the United States became ill following consumption of tuna or chicken salad sandwiches prepared by food workers testing positive for the same P[4], G2 rotavirus strain that was detected in the stools of the students (CDC 2000).
Although no direct link between field-contaminated produce and outbreaks of rotavirus illness has been established as yet, several studies indicate that this route of transmission is possible. In Costa Rica, market lettuce was found to be contaminated with rotavirus and HAV at a time when there was a high incidence of rotaviral diarrhea in the community (Hernandez et al. 1997). Similarly, rotaviruses were detected on green onions and work surfaces within a packing house in Mexico (Felix-Valenzuela et al. 2012) and on strawberries irrigated with river water in Canada (Brassard et al. 2012). Sewage-impacted water has resulted in rotavirus contamination of shellfish in China (Ming et al. 2013) and was also the likely source of a gastroenteritis outbreak related to salad consumption on a cruise ship, where rotavirus, human norovirus and sapovirus were detected in the stools of ill persons (Gallimore et al. 2005).
6.6 Zoonotic Transmission
Rotaviruses are major pathogens of both humans and domestic animals. There is mounting evidence of zoonotic transmission between humans and animals, particularly when domestic animals are kept in close proximity to humans. Interspecies replication of rotaviruses occurs readily with many rotavirus strains, but is less commonly associated with disease. Exploitation of this fact was the basis for construction of live-attenuated rotavirus vaccine candidates. Due to the segmented nature of the viral genome, there is potential for genomic reassortment of human and animal rotaviruses. Close interspecies relationships between porcine-human and bovine-human strains have been identified by RNA-RNA hybridization and more recently by full genome sequencing. Several rotavirus strains that have caused illness in humans in Latin America, Asia, Europe and Africa have now been either confirmed or are highly suspected to have emerged after reassortment with animal rotaviruses (Martella et al. 2010). Continued efforts to generate full-length genome sequences for human and animal rotavirus strains will thus be important for further elucidation of the zoonotic potential of rotaviruses.
7 Astrovirus
7.1 Distribution and Transmission
Astroviruses are distributed worldwide and have been isolated from birds, cats, dogs, pigs, sheep, cows and man. The main feature of astrovirus infection in both humans and animals is a self-limiting gastroenteritis. Astroviruses are estimated to cause up to 20 % of all sporadic and 0.5–15 % of epidemic cases of non-bacterial gastroenteritis in humans, with most cases of infection being detected in young children under 2 years of age (De Benedictis et al. 2011). Although astroviruses cause a mild infection in adults, they have been associated with gastroenteritis in immunocompromised adults. Transmission is through the fecal-oral route via food, water and person-to-person contact, especially in nurseries, childcare centers and hospitals. Asymptomatic excretion is estimated to be approximately 10 % in most human populations but as high as 30 % prevalence rates have been reported in develo** countries (De Benedictis et al. 2011; De Grazia et al. 2011; Guix et al. 2002). Co-infections with other enteric pathogens are common and have been reported to be between 17 and 65 % (De Benedictis et al. 2011).
7.2 Taxonomy and Morphology
The astroviruses, named for the star-like appearance they exhibit under electron microscope (EM), were first recognized in 1975 (Madeley and Cosgrove 1975). The virus belongs to the family Astroviridae, which includes the genera Mamastrovirus and Avastrovirus that infect mammals and birds, respectively. Astroviruses are 28–30 nm icosohedral, non-enveloped positive-sense single-stranded RNA viruses with a genome of about 6.8–7.8 kb and a buoyant density of 1.32 g/ml in potassium tartrate-glycerol gradient (Table 2.1). Since only 10 % of astroviruses exhibit the typical 5 or 6 pointed star-like morphology by direct EM, the efficiency of detection was restricted until the introduction of molecular detection methods and improved culture techniques. Eight human astrovirus species (HAstVs 1-8) have been identified based on seroty** but new species continue to emerge through molecular studies. Currently there are 33 genotypes in the Mamastrovirus genus and 11 genotypes in the Avastrovirus genus (Bosch et al. 2014). Mamastrovirus species are also detected in bovine, feline, porcine, canine, ovine, mink, rodent, bat and marine mammal hosts. Avastroviruses include turkey, chicken and duck astroviruses as well as the avian nephritis virus (De Benedictis et al. 2011).
7.3 Growth and Biological Properties
Wild-type astroviruses are fastidious to grow in vitro. Human, porcine, bovine and avian astroviruses have been adapted to grow in established cell lines, but trypsin is required in the growth medium to boost infectivity for all astroviruses except chicken astroviruses. Propagation of reference strains and wild-type astroviruses from stool suspensions is most successful with the adenocarcinoma cell lines, Caco-2 and T-84, and the human liver hepatoma cell line, PLC/PRF/5 (Mendez and Arias 2007). Virus detection is carried out mainly by EM of stool specimens, diagnostic RT-PCR using broadly reactive primers, or by an integrated cell culture-RT-PCR (ICC-RT-PCR) procedure. Astroviruses are resistant to extreme environmental conditions. Their heat tolerance allows them to survive 50 °C for 1 h. At 60 °C, the virus titer falls by 3 log10 and 6 log10 after 5 and 15 min, respectively. Astroviruses are stable for years at ≤ −70 °C but repeated freeze/thawing cycles can lead to structural damage. The virus is stable at pH 3.0 and is resistant to chemicals, including chloroform, lipid solvents, and alcohols and to non-ionic, anionic and Zwitter ionic detergents. Astrovirus particles exhibit a range of buoyant densities in cesium chloride (CsCl), from 1.35 to 1.39 g/mL for complete virus particles, and from 1.28 to 1.33 g/mL for empty (no genome) capsids or VLPs. Divalent cations (Ca2+ and Mg2+) in CsCl facilitate virus and VLP stabilization (Mendez and Arias 2007).
7.4 Infection and Disease
Clinically, astroviruses cause symptoms similar to those of caliciviruses following an incubation period of 3–4 days although shorter incubation periods (24–36 h) have also been reported. Symptoms include diarrhea, fever, nausea, and general malaise with occasional vomiting. Normally, diarrhea persists for only 2–3 days but can be prolonged for up to 14 days with virus excretion in feces. High concentrations of astrovirus (up to 1010 or 1011 viruses per gram) can be shed in feces (Mendez and Arias 2007). Severe illnesses and death can occur but are rarely reported. Outbreaks commonly occur in institutional settings, especially pediatric wards. In temperate climates, a seasonal peak in winter and spring occurs, but infections may occur throughout the year, especially during the rainy season in tropical climates.
7.5 Foodborne Disease
Epidemiological evidence of transmission by foods is limited but infections via contaminated shellfish and water have been reported (Appleton 2001; Oishi et al. 1994). In 1991, a large outbreak of acute gastroenteritis occurred in Japan involving thousands of children and adults from 14 schools (Oishi et al. 1994). The outbreak was traced to food prepared by a common supplier for school lunches; astrovirus type 6 was identified by immune electron microscopy and confirmed by molecular and culture methods. There are several reports of astrovirus genomes identified in shellfish and evidence indicates that astroviruses may contribute to outbreaks of gastroenteritis through consumption of contaminated oysters (Kitahashi et al. 1999; Le Guyader et al. 2008; Ming et al. 2013). In a French shellfish-related gastroenteritis outbreak, astroviruses were among a range of enteric viruses identified in patient feces and related shellfish samples (Le Guyader et al. 2008). Given the wide range of animal astroviruses discovered in recent years and their capacity for genetic mutation and recombination, interspecies replication and zoonotic transmission is possible although, to date, no zoonotic astrovirus strains have been reported in humans (Bosch et al. 2014).
8 Other Viruses with Potential for Foodborne Transmission
Other viruses transmitted by the fecal-oral route and found in feces of humans and animals include the adenoviruses, enteroviruses, aichiviruses, parvoviruses, coronaviruses, toroviruses, picobirnaviruses, polyomaviruses and the tick borne encephalitis virus (Table 2.1). Some of these viruses have caused a small number of foodborne outbreaks in the past. While they are currently considered minor foodborne pathogens, there is a possibility that more virulent or transmissible strains of these viruses might emerge making them pathogens of significance. For some of these viruses, the ability to cause illness in humans and or animals is still unproven. Readers are referred to a published review providing more description on these viruses and their potential to cause foodborne disease (Duizer and Koopmans 2008). A brief description of these viruses is given below.
8.1 Adenoviruses
Adenoviruses belong to the Adenoviridae family and are classified into five genera, Mastedenovirus (infect mammals), Aviadenovirus (infect birds), Atadenovirus (infect sheep, cattle, ducks and possum), Ichtadenovirus (infects sturgeon) and Siadenovirus (infect reptiles and birds). Adenoviruses are 80–110 nm non-enveloped, linear double-stranded DNA viruses with icosahedral symmetry and a genome of 28–45 kb (Table 2.1, Fig. 2.1c). Most human adenovirus (HAdV) infections in normally healthy individuals are mild or subclinical but can be associated with respiratory, ocular and gastrointestinal disease. HAdV-F types 40 and 41 are generally associated with fecal-oral spread and cause gastroenteritis, although all types are shed in feces, often in large numbers (up to 1011 particles/g feces) for several months (Wold and Horwitz 2007). Over 60 human adenovirus types have been recognized that appear to be specific to humans as none have been detected in the stools of domestic and wild mammals (Jiang 2006). This feature makes them a good candidate for microbial source tracking to identify sources of fecal pollution (Wong et al. 2012).
The adenoviruses are capable of prolonged survival in the environment and are considered to be more stable than other enteric viruses and faecal indicator bacteria in many environmental situations. The A549 and 293 cell lines have been used successfully for the isolation of adenoviruses from food and environmental samples, although members of the F subgroup are more fastidious than other human adenoviruses. Adenoviruses can be transmitted person-to-person by direct contact or via fecal-oral, respiratory or environmental routes. Waterborne transmission of adenovirus has been associated with conjunctivitis in children. Enteric adenovirus infections are common all year round, whereas outbreaks of adenovirus-associated respiratory disease normally occur from late winter to early summer. Adenoviruses have been detected in a variety of environmental samples, including wastewater, sludge, shellfish, and marine, surface and drinking waters. No foodborne or waterborne outbreaks associated with the enteric adenoviruses have been reported but, as these viruses are common in the environment, it is possible that disease has occurred but the source of infection was not recognized. There are no reports of foodborne transmission or disease resulting from consumption of adenovirus-contaminated shellfish.
8.2 Enteroviruses
The enteroviruses are 28–30 nm non-enveloped, positive-sense single-stranded RNA viruses with icosohedral symmetry and a genome of 7.2–8.4 kb (Table 2.1). They are classified in the large Picornaviridae family and 12 species are currently designated within the Enterovirus genus, including Enterovirus A, B, C, D, E, F, G, H, and J (the letter I was skipped) and Rhinovirus A–C (ICTV 2012; Knowles et al. 2011b). Enteroviruses include polioviruses, coxsackie A and B viruses, echoviruses, and rhinoviruses, many of which are culturable. Enteroviruses cause a range of diseases, including viral meningitis and poliomyelitis. They multiply mainly in the gastrointestinal tract but can also multiply in other tissues such as nerve and muscle, as does the poliovirus. The incubation period is usually between 3 and 7 days with virus transmission occurring from 3 to 10 days after symptoms develop. Enteroviral infection is most common in summer and early autumn and many infections are asymptomatic. Only a few people (approximately 0.001 %) develop aseptic or viral meningitis and no long-term complications normally follow the mild illnesses or aseptic meningitis. On rare occasions, a person may develop myocarditis or encephalitis.
Many enteroviruses are transmitted by the fecal-oral route and are excreted in feces but do not generally cause gastroenteritis. Because they are easily cultured in vitro and are stable in the environment, live attenuated vaccine strains of poliovirus have been used as indicator viruses for the presence of other virulent enteric viruses in food and water. They have also been used extensively in environmental and food virology research for method development and to gather information on virus recovery, persistence and behavior in these settings. The first recorded outbreak associated with foodborne viruses was an outbreak of poliomyelitis linked to consumption of raw milk in 1914 (Jubb 1915). A further ten outbreaks associated with raw milk consumption were reported in the USA and United Kingdom over the following 35 years (Sattar and Tetro 2001). The widespread introduction of pasteurized milk in the 1950s decreased transmission by this route. There have been few recorded foodborne outbreaks associated with enterovirus infection despite the regular occurrence of enteroviruses in the environment. Enteroviruses, including echoviruses and coxsackie A and B viruses, have been isolated from sewage, raw and digested sludge, marine and fresh waters, and shellfish. In two reported foodborne outbreaks associated with echoviruses in the United States, the source of the virus was not identified (Cliver 1997). Although enteroviruses are often present in shellfish, other enteric viruses are also usually present and no shellfish—associated outbreaks have been reported specifically for enteroviruses.
8.3 Aichivirus
Aichivirus A (formerly Aichi virus) is a single stranded RNA virus classified in the Genus Kobuvirus, in the Family Picornaviridae. It was first discovered in 1989 in Japan by Yamashita et al. (1991) as the cause of oyster-associated gastroenteritis (Yamashita et al. 1991). It was later identified in gastroenteritis cases from several Asian countries and classified as a novel picornavirus (Yamashita et al. 1993; Yamashita et al. 1998). Aichiviruses have been detected in stools, human sewage and in shellfish worldwide, but seem to be more often detected in Asian countries. Aichivirus was identified in 33 % of 57 commercial packages of Japanese clams (Hansman et al. 2008). The first identifications of the virus outside Asia occurred in clinical specimens in Germany and Brazil (Oh et al. 2006). Aichiviruses were also among several enteric viruses identified in clinical specimens and oysters associated with a gastroenteritis outbreak in France (Le Guyader et al. 2008). Since it is often detected along with other viruses associated with gastrointestinal illness, its importance as a food- and water-borne pathogen is still unclear. The virus is culturable and produces cytopathic effects in B-SC 1 cells.
8.4 Parvovirus
Parvoviruses have been proposed as causal agents of human gastroenteritis but their role in viral gastroenteritis of some animal species has been well documented. They are single stranded DNA viruses classified in the family Parvoviridae, subfamily Parvovirinae, genus Erythrovirus, which includes type species human parvovirus B19. They are among the smallest known viruses at 18–26 nm in diameter. Parvoviruses have a smooth surface with no discernable features and were included under ‘small round viruses’ before definitive classification of these viruses was completed. Three possible serotypes known as the Parramatta agent, the cockle agent and the Wollan/Ditchling group have been identified by immune electron microscopy. There is limited evidence of parvovirus association with foodborne disease but it has been linked with consumption of contaminated shellfish (Appleton 2001; Appleton and Pereira 1977). The ‘cockle agent’ parvovirus was implicated in a large UK outbreak related to consumption of contaminated cockles (Appleton 2001). Over 800 confirmed cases of gastroenteritis occurred and parvovirus was identified in all stools examined from this large gastroenteritis outbreak.
Human bocaviruses (1, 2 a–c, 3 & 4) are also classified in the Parvoviridae family (subfamily Parvovirinae, Bocaparvovirus genus). Although they have been detected in feces and waters and may be transmitted by the fecal-oral route, bocavirus type 1 is mainly associated with pediatric respiratory diseases (Arthur et al. 2009) and the role of bocavirus type 2 in gastroenteritis is currently unclear (Chhabra et al. 2013; Chow et al. 2010).
8.5 Coronavirus
Coronaviruses are large (80–220 nm), pleomorphic, enveloped, positive sense single-stranded RNA viruses belonging to the Coronaviridae family (human strains reside in Alphacoronavirus and Betacoronavirus genera). They generally cause respiratory infections but can also cause gastroenteritis in animals and are excreted in feces. Their role in human gastroenteritis is unclear, although ‘coronavirus-like particles’ can be identified in human feces (Glass 1995). SARS (severe acute respiratory syndrome) and the MERS (Middle East respiratory syndrome) coronaviruses (CoVs ) have been associated with severe atypical pneumonia and numerous deaths since their emergence in 2002 and 2012, respectively. Bats appear to be the primary reservoir for both of these viruses. However, intermediate hosts appear to be responsible for zoonotic transmission to humans. SARS-CoV infections in humans have been linked to palm civets and raccoon dogs sold at Chinese exotic markets (Graham and Baric 2010). Dromedary camels may be associated with human infections by MERS-CoV in the Middle East, as evidenced by neutralizing antibodies and positive nasal swabs detected in these animals (Milne-Price et al. 2014); however, a direct evidence of zoonotic transmission has not been reported to date.
8.6 Torovirus
Toroviruses are 100–150 nm, enveloped, positive sense, single-stranded RNA viruses belonging to the Genus Torovirus in the Coronaviridae family. They were first discovered in 1979 and were named as Breda viruses (Glass 1995; Woode et al. 1982). When observed by EM they have a distinctive pleomorphic appearance with club-shaped projections extending from the capsid. Toroviruses are known to cause gastroenteritis in animals, especially dairy cattle, in which they cause a marked decrease in milk production. Although they have been isolated from feces of children and adults with diarrhea (Koopmans et al. 1991), their exact role in human gastroenteritis and foodborne disease is still unknown.
8.7 Picobirnavirus
The picobirnaviruses are small non-enveloped 33–41 nm positive sense double-stranded RNA viruses with a segmented genome and are classified in the family Picobirnaviridae, genus Picobirnavirus (Knowles et al. 2011a). These viruses have been detected in feces of many animals and birds and are known to cause gastroenteritis in a range of domestic animals. They have also been detected in humans with and without diarrhea and are now regarded as opportunistic pathogens which can cause gastroenteritis in immunocompromised patients. They have been detected in sewage and river waters (Hamza et al. 2011) and in humans from several countries, including Australia, Brazil, England and the USA. Their role as true human pathogens is unproven and although there is no documented evidence of foodborne transmission, it is likely that they can be transmitted by the fecal-oral route and possibly via food.
8.8 Tick-Borne Encephalitis Virus
Tick-borne encephalitis (TBE ) virus along with other closely related arboviruses that cause yellow fever, Japanese encephalitis, dengue fever and West Nile disease are enveloped, positive sense single- stranded RNA viruses classified in the Flaviviridae family under the Flavivirus genus. Tick-borne encephalitis is a zoonotic arbovirus infection endemic to Eastern and Central Europe and Russia. However, the distribution of these viruses can extend to Northern Europe, China, Japan and Korea. Three subtypes of TBE virus cause tick-borne encephalitis: the Eastern European subtype, the Western European subtype and the Siberian subtype. Most cases occur in spring and summer following bites of different species of Ixodes tick. Foodborne transmission is less common but can occur following consumption of unpasteurized dairy products such as milk, yogurt, butter and cheese from infected cattle and goats (Döbbecker et al. 2010). The disease is serious and can result in long-term neurological sequelae or death. Increased tourism to the endemic areas has extended the risk of travellers acquiring TBE. Vaccines are now available in several countries.
8.9 Other Foodborne Routes of Virus Transmission
Transmission of viral disease can occur through human breastfeeding especially some of the bloodborne viruses. There are reports of human immunodeficiency virus (HIV), human lymphotrophic virus -1 (HTLV-1), hepatitis B virus and cytomegalovirus (CMV) being transmitted to infants in milk from infected mothers during breast feeding (Pol et al. 2011; Sattar and Tetro 2001). This can present serious problems in less developed countries with a high incidence of HIV and few alternative options for feeding available to infected mothers.
9 Summary and Conclusions
Foodborne disease is increasing worldwide and has become a major public health problem. A majority of foodborne viral disease is caused by noroviruses and HAV. Foodborne transmission of other enteric viruses is less common. The HEV is the only virus that appears to be a likely candidate for direct zoonotic transmission from animals to man, although to date there have been few reports of its transmission by this route.
The overall contribution of viruses to global foodborne disease burden is unknown because accurate data on the prevalence of foodborne viral disease are not available for all countries. National epidemiological surveillance systems vary from country to country and a large proportion of viral infections are not notifiable and therefore not reported. However, from epidemiological data that has been collected in Europe, the USA and other countries, it is apparent that viruses play a significant role and that the economic burden of foodborne viral gastrointestinal disease can be substantial in terms of staff illness, time away from employment and disruption to services.
Over the last 20 years, the introduction of molecular methods for detection and identification of enteric viruses, many of which are not culturable or are difficult to grow in culture, has greatly increased our understanding of their role in foodborne disease. The development of techniques, such as PCR and real-time quantitative PCR, is rapidly increasing the knowledge base by facilitating studies on the behavior and persistence of these viruses in food matrices. However, it is important to recognize the limitations of these techniques. PCR-based methods currently detect both infectious and non-infectious viruses and are not able to measure viral infectivity, which is the key factor when assessing human health risks from foodborne pathogens.
Recently, several novel molecular—based methods have been developed to determine viral infectivity in non-culturable viruses, but none have yet been validated for regulatory or epidemiological use (Knight et al. 2013). The overall strategies used in these methods are either assessment of virus capsid integrity by receptor or antibody binding, or use of nucleic acid-intercalating chemicals or RNases to disrupt RNA such that only intact viral RNA is amplified by RT-PCR. Sometimes longer portions of the genome are targeted to better assess RNA damage. If the virus is no longer detectable in molecular assays after employing these methods, it is considered to be non-infectious.
It is important however that judicious interpretation of data generated solely from molecular-based assays is used when studying these viruses. Use of integrated cell culture combined with PCR methods (ICC-PCR) can overcome some of the problems associated with viruses that are difficult to grow. Unfortunately, the infectivity status of the main foodborne viral pathogen, norovirus, still cannot be determined routinely by in vitro methods. This has limited our knowledge of the natural history and biological properties of this pathogen and has also slowed progress in the development of effective control and intervention strategies.
References
Aggarwal R, Naik S (2008) Enterically transmitted hepatitis. In: Koopmans MPG, Cliver DO, Bosch A (eds) Food-borne viruses: progress and challenges. ASM (American Society for Microbiology) Press, Washington, pp 65–85
Anonymous (2013) Multistate outbreak of hepatitis A virus infections linked to pomegranate seeds from Turkey (final update). Centers for Disease Control and Prevention. Posted October 28, 2008. http://www.cdc.gov/hepatitis/outbreaks/2013/a1b-03-31/index.html. Accessed 13 March 2014
Ansari SA, Springthorpe VS, Sattar SA (1991) Survival and vehicular spread of human rotaviruses: possible relation to seasonality of outbreaks. Rev Infect Dis 13:448–461
Appleton H (2001) Norwalk virus and the small round viruses causing foodborne gastroenteritis. In: Hui YH, Gorham JR, Murrell KD, Cliver DOE (eds) Foodborne disease handbook: viruses, parasites, pathogens and HACCP, 2nd edn. Marcel Dekker, Inc., New York, pp 77–97
Appleton H, Pereira MS (1977) A possible virus aetiology in outbreaks of food-poisoning from cockles. Lancet 1:780–781
Arthur JL, Higgins GD, Davidson GP, Givney RC, Ratcliff RM (2009) A novel bocavirus associated with acute gastroenteritis in Australian children. PLoS Pathog 5, e1000391
Atmar RL, Opekun AR, Gilger MA, Estes MK, Crawford SE, Neill FH, Graham DY (2008) Norwalk virus shedding after experimental human infection. Emerg Infect Dis 14:1553–1557
Atmar RL, Bernstein DI, Harro CD, Al-Ibrahim MS, Chen WH, Ferreira J, Estes MK, Graham DY, Opekun AR, Richardson C, Mendelman PM (2011) Norovirus vaccine against experimental human Norwalk virus illness. N Engl J Med 365:2178–2187
Atmar RL, Opekun AR, Gilger MA, Estes MK, Crawford SE, Neill FH, Ramani S, Hill H, Ferreira J, Graham DY (2014) Determination of the 50% human infectious dose for Norwalk virus. J Infect Dis 209(7):1016–1022
Bae J, Schwab KJ (2008) Evaluation of murine norovirus, feline calicivirus, poliovirus, and MS2 as surrogates for human norovirus in a model of viral persistence in surface water and groundwater. Appl Environ Microbiol 74:477–484
Balayan MS, Andjaparidze AG, Savinskaya SS, Ketiladze ES, Braginsky DM, Savinov AP, Poleschuk VF (1983) Evidence for a virus in non-A, non-B hepatitis transmitted via the fecal-oral route. Intervirology 20:23–31
Beller M, Ellis A, Lee SH, Drebot MA, Jenkerson SA, Funk E, Sobsey MD, Simmons OD 3rd, Monroe SS, Ando T, Noel J, Petric M, Middaugh JP, Spika JS (1997) Outbreak of viral gastroenteritis due to a contaminated well: international consequences. JAMA 278:563–568
Bellou M, Kokkinos P, Vantarakis A (2013) Shellfish-borne viral outbreaks: a systematic review. Food Environ Virol 5:13–23
Berg DE, Kohn MA, Farley TA, McFarland LM (2000) Multi-state outbreaks of acute gastroenteritis traced to fecal-contaminated oysters harvested in Louisiana. J Infect Dis 181(Suppl 2):S381–S386
Berto A, Martelli F, Grierson S, Banks M (2012) Hepatitis E virus in pork food chain, United Kingdom, 2009–2010. Emerg Infect Dis 18:1358–1360
Berto A, Grierson S, Hakze-van der Honing R, Martelli F, Johne R, Reetz J, Ulrich RG, Pavio N, Van der Poel WH, Banks M (2013) Hepatitis E virus in pork liver sausage, France. Emerg Infect Dis 19:264–266
Beuret C, Kohler D, Baumgartner A, Luthi TM (2002) Norwalk-like virus sequences in mineral waters: one-year monitoring of three brands. Appl Environ Microbiol 68:1925–1931
Bishop RF (1996) Natural history of human rotavirus infection. Arch Virol Suppl 12:119–128
Bok K, Parra GI, Mitra T, Abente E, Shaver CK, Boon D, Engle R, Yu C, Kapikian AZ, Sosnovtsev SV, Purcell RH, Green KY (2011) Chimpanzees as an animal model for human norovirus infection and vaccine development. PNAS 108:325–330
Bosch A, Sanchez G, Le Guyader F, Vanaclocha H, Haugarreau L, Pinto RM (2001) Human enteric viruses in Coquina clams associated with a large hepatitis A outbreak. Water Sci Technol 43:61–65
Bosch A, Pintó RM, Guix S (2014) Human astroviruses. Clin Microbiol Rev 27:1048–1074
Bozkurt H, D’Souza DH, Davidson PM (2013) Determination of the thermal inactivation kinetics of the human norovirus surrogates, murine norovirus and feline calicivirus. J Food Prot 76:79–84
Brassard J, Gagne MJ, Genereux M, Cote C (2012) Detection of human food-borne and zoonotic viruses on irrigated, field-grown strawberries. Appl Environ Microbiol 78:3763–3766
Brugha R, Vipond I, Evans M, Sandifer Q, Roberts R, Salmon R, Caul E, Mukerjee A (1999) A community outbreak of food-borne small round-structured virus gastroenteritis caused by a contaminated water supply. Epidemiol Infect 122:145–154
Burton-MacLeod JA, Kane EM, Beard RS, Hadley LA, Glass RI, Ando T (2004) Evaluation and comparison of two commercial enzyme-linked immunosorbent assay kits for detection of antigenically diverse human noroviruses in stool samples. J Clin Microbiol 42:2587–2595
Cacopardo B, Russo R, Preiser W, Benanti F, Brancati G, Nunnari A (1997) Acute hepatitis E in Catania (Eastern Sicily) 1980–1994. The role of hepatitis E virus. Infection 25:313–316
Calder L, Simmons G, Thornley C, Taylor P, Pritchard K, Greening G, Bishop J (2003) An outbreak of hepatitis A associated with consumption of raw blueberries. Epidemiol Infect 131:745–751
Cannon JL, Papafragkou E, Park GW, Osborne J, Jaykus LA, Vinje J (2006) Surrogates for the study of norovirus stability and inactivation in the environment: a comparison of murine norovirus and feline calicivirus. J Food Prot 69:2761–2765
Carstens EB (2010) Ratification vote on taxonomic proposals to the international committee on taxonomy of viruses (2009). Arch Virol 155:133–146
Carvalho C, Thomas HL, Balogun K, Tedder R, Pebody R, Ramsay M, Ngui SL (2012) A possible outbreak of hepatitis A associated with semi-dried tomatoes, England, July-November 2011. Euro Surveill 17:14–17
Centers for Disease Control and Prevention (CDC) (2000) Foodborne outbreak of group A rotavirus gastroenteritis among college students--District of Columbia, March-April 2000. Morb Mortal Wkly Rep 49:1131–1133
Centers for Disease Control and Prevention (CDC) (2003) Hepatitis A outbreak associated with green onions at a restaurant --- Monaca, Pennsylvania, 2003. Morb Mortal Wkly Rep 52:1155–1157
Centers for Disease Control and Prevention (CDC) (2006) Multisite outbreak of norovirus associated with a franchise restaurant--Kent County, Michigan, May 2005. Morb Mortal Wkly Rep 55:395–397
Centers for Disease Control and Prevention (CDC) (2010) Viral hepatitis surveillance; United States, 2010. Centers for Disease Control and Prevention. Posted August 26, 2013. http://www.cdc.gov/hepatitis/Statistics/2010Surveillance. Accessed 13 March 2014
Centers for Disease Control and Prevention (CDC) (2011) Updated norovirus outbreak management and disease prevention guidelines. Morb Mortal Wkly Rep 60:1–18
Centers for Disease Control and Prevention (CDC) (2013) Investigation of hepatitis E outbreak among refugees - upper Nile, South Sudan, 2012–2013. Morb Mortal Wkly Rep 62:581–586
Chadwick PR, Beards G, Brown D, Caul EO, Cheesbrough J, Clarke I, Curry A, O’Brien S, Quigley K, Sellwood J, Westmoreland D (2000) Management of hospital outbreaks of gastro-enteritis due to small round-structured viruses. J Hosp Infect 45:1–10
Chang KO (2004) Bile acids are essential for porcine enteric calicivirus replication in association with down-regulation of signal transducer and activator of transcription 1. PNAS 101:8733–8738
Cheetham S, Souza M, Meulia T, Grimes S, Han MG, Saif LJ (2006) Pathogenesis of a genogroup II human norovirus in gnotobiotic pigs. J Virol 80:10372–10381
Chhabra P, Payne DC, Szilagyi PG, Edwards KM, Staat MA, Shirley SH, Wikswo M, Nix WA, Lu X, Parashar UD, Vinje J (2013) Etiology of viral gastroenteritis in children <5 years of age in the United States, 2008–2009. J Infect Dis 208:790–800
Chow BD, Ou Z, Esper FP (2010) Newly recognized bocaviruses (HBoV, HBoV2) in children and adults with gastrointestinal illness in the United States. J Clin Virol 47:143–147
Christensen BF, Lees D, Henshilwood K, Bjergskov T, Green J (1998) Human enteric viruses in oysters causing a large outbreak of human food borne infection in 1996/97. J Shellfish Res 17:1633–1635
Clemente-Casares P, Pina S, Buti M, Jardi R, MartIn M, Bofill-Mas S, Girones R (2003) Hepatitis E virus epidemiology in industrialized countries. Emerg Infect Dis 9:448–454
Cliver DO (1997) Virus transmission via food. World Health Stat Q 50:90–101
Coelho C, Heinert AP, Simoes CM, Barardi CR (2003) Hepatitis A virus detection in oysters (Crassostrea gigas) in Santa Catarina state, Brazil, by reverse transcription-polymerase chain reaction. J Food Prot 66:507–511
Colson P, Borentain P, Queyriaux B, Kaba M, Moal V, Gallian P, Heyries L, Raoult D, Gerolami R (2010) Pig liver sausage as a source of hepatitis E virus transmission to humans. J Infect Dis 202:825–834
Conaty S, Bird P, Bell G, Kraa E, Grohmann G, McAnulty JM (2000) Hepatitis A in New South Wales, Australia from consumption of oysters: the first reported outbreak. Epidemiol Infect 124:121–130
Cook SM, Glass RI, LeBaron CW, Ho MS (1990) Global seasonality of rotavirus infections. Bull World Health Organ 68:171–177
Cortes JE, Curns AT, Tate JE, Cortese MM, Patel MM, Zhou F, Parashar UD (2011) Rotavirus vaccine and health care utilization for diarrhea in U.S. children. NEJM 365:1108–1117
Costantini V, Loisy F, Joens L, Le Guyader FS, Saif LJ (2006) Human and animal enteric caliciviruses in oysters from different coastal regions of the United States. Appl Environ Microbiol 72:1800–1809
Cotterelle B, Drougard C, Rolland J, Becamel M, Boudon M, Pinede S, Traore O, Balay K, Pothier P, Espie E (2005) Outbreak of norovirus infection associated with the consumption of frozen raspberries, France, March 2005. Euro Surveill 10, E050428. 1
Cristina J, Costa-Mattioli M (2007) Genetic variability and molecular evolution of hepatitis A virus. Virus Res 127:151–157
Croci L, De Medici D, Scalfaro C, Fiore A, Divizia M, Donia D, Cosentino AM, Moretti P, Costantini G (2000) Determination of enteroviruses, hepatitis A virus, bacteriophages and Escherichia coli in Adriatic sea mussels. J Appl Microbiol 88:293–298
Cromeans T, Favorov MO, Nainan OV, Margolis HS (2001) Hepatitis A and E viruses. In: Hui YH, Sattar SA, Murrell KD, Nip W-K, Stanfield PS (eds) Foodborne disease handbook: viruses, parasites, pathogens and HACCP, 2nd edn. Marcel Dekker, Inc., New York, pp 23–76
Crossan C, Baker PJ, Craft J, Takeuchi Y, Dalton HR, Scobie L (2012) Hepatitis E virus genotype 3 in shellfish, United Kingdom. Emerg Infect Dis 18:2085–2087
Dalton HR, Hunter JG, Bendall RP (2013) Hepatitis E. Curr Opin Infect Dis 26:471–478
Daniels NA, Bergmire-Sweat DA, Schwab KJ, Hendricks KA, Reddy S, Rowe SM, Fankhauser RL, Monroe SS, Atmar RL, Glass RI, Mead P (2000) A foodborne outbreak of gastroenteritis associated with Norwalk-like viruses: first molecular traceback to deli sandwiches contaminated during preparation. J Infect Dis 181:1467–1470
De Benedictis P, Schultz-Cherry S, Burnham A, Cattoli G (2011) Astrovirus infections in humans and animals - molecular biology, genetic diversity, and interspecies transmissions. Infect Genet Evol 11:1529–1544
De Grazia S, Platia MA, Rotolo V, Colomba C, Martella V, Giammanco GM (2011) Surveillance of human astrovirus circulation in Italy 2002–2005: emergence of lineage 2c strains. Eur Soc Clin Microbiol Infect Dis 17:97–101
de Wit MA, Koopmans MP, van Duynhoven YT (2003) Risk factors for norovirus, sapporo-like virus, and group A rotavirus gastroenteritis. Emerg Infect Dis 9:1563–1570
de Wit MA, Widdowson MA, Vennema H, de Bruin E, Fernandes T, Koopmans M (2007) Large outbreak of norovirus: the baker who should have known better. J Infect 55:188–193
Desselberger U (2014) Rotoviruses. Virus Res 190:75–96
Dhama K, Chauhan RS, Mahendran M, Malik SV (2009) Rotavirus diarrhea in bovines and other domestic animals. Vet Res Commun 33:1–23
Döbbecker B, Dobler G, Spiegel M, Hufert FT (2010) Tick-borne encephalitis virus and the immune response of the mammalian host. Travel Med Infect Dis 8:213–222
Dolin R, Blacklow NR, DuPont H, Formal S, Buscho RF, Kasel JA, Chames RP, Hornick R, Chanock RM (1971) Transmission of acute infectious nonbacterial gastroenteritis to volunteers by oral administration of stool filtrates. J Infect Dis 123:307–312
Dolin R, Blacklow NR, DuPont H, Buscho RF, Wyatt RG, Kasel JA, Hornick R, Chanock RM (1972) Biological properties of Norwalk agent of acute infectious nonbacterial gastroenteritis. Proc Soc Exp Biol Med 140:578–583
Donnan EJ, Fielding JE, Gregory JE, Lalor K, Rowe S, Goldsmith P, Antoniou M, Fullerton KE, Knope K, Copland JG, Bowden DS, Tracy SL, Hogg GG, Tan A, Adamopoulos J, Gaston J, Vally H (2012) A multistate outbreak of hepatitis A associated with semidried tomatoes in Australia, 2009. Clin Infect Dis 54:775–781
Dowell SF, Groves C, Kirkland KB, Cicirello HG, Ando T, ** Q, Gentsch JR, Monroe SS, Humphrey CD, Slemp C et al (1995) A multistate outbreak of oyster-associated gastroenteritis: implications for interstate tracing of contaminated shellfish. J Infect Dis 171:1497–1503
Duizer E, Koopmans M (2008) Emerging food-borne viral diseases. In: Koopmans M, Cliver DO, Bosch A (eds) Food-borne viruses: progress and challenges. ASM Press, Washington, pp 117–145
Duizer E, Schwab KJ, Neill FH, Atmar RL, Koopmans MP, Estes MK (2004) Laboratory efforts to cultivate noroviruses. J Gen Virol 85:79–87
EFSA, Panel on Biological Hazards (2011) Scientific opinion on an update on the present knowledge on the occurrence and control of foodborne viruses. EFSA J 9:2190–2286
Estes MK, Kapikian AZ (2007) Rotaviruses. In: Knipe DM, Howley PM, Cohen JI, Griffin DE, Lamb RA, Martin MA, Racaniello VR, Roizman B (eds) Fields virology, 5th edn. Lippincott Williams & Wilkins, Philadelphia, pp 1917–1974
Estes MK, Ball JM, Guerrero RA, Opekun AR, Gilger MA, Pacheco SS, Graham DY (2000) Norwalk virus vaccines: challenges and progress. J Infect Dis 181(Suppl 2):S367–S373
Ethelberg S, Lisby M, Bottiger B, Schultz AC, Villif A, Jensen T, Olsen KE, Scheutz F, Kjelso C, Muller L (2010) Outbreaks of gastroenteritis linked to lettuce, Denmark, January 2010. Euro Surveill 15:2–4
Falkenhorst G, Krusell L, Lisby M, Madsen SB, Bottiger B, Molbak K (2005) Imported frozen raspberries cause a series of norovirus outbreaks in Denmark, 2005. Euro Surveill 10:E050922.2
Farkas T, Sestak K, Wei C, Jiang X (2008) Characterization of a Rhesus monkey calicivirus representing a new genus of Caliciviridae. J Virol 82:5408–5416
Feagins AR, Opriessnig T, Guenette DK, Halbur PG, Meng XJ (2007) Detection and characterization of infectious hepatitis E virus from commercial pig livers sold in local grocery stores in the USA. J Gen Virol 88:912–917
Felix-Valenzuela L, Resendiz-Sandoval M, Burgara-Estrella A, Hernandez J, Mata-Haro V (2012) Quantitative detection of hepatitis A, rotavirus and genogroup I norovirus by RT-qPCR in fresh produce from packinghouse facilities. J Food Saf 32:467–473
Fiore AE (2004) Hepatitis A transmitted by food. Clin Infect Dis 38:705–715
Food and Agriculture Organization of the United Nations/World Health Organization (FAO/WHO) (2008) Viruses in food: scientific advice to support risk management activities. Microbiological Risk Assessment Series 13. ISSN 1726–527. http://www.who.int/foodsafety/publications/micro/mra13/en/. Accessed 13 March 13 2014
Fournet N, Baas D, van Pelt W, Swaan C, Ober HJ, Isken L, Cremer J, Friesema I, Vennema H, Boxman I, Koopmans M, Verhoef L (2012) Another possible food-borne outbreak of hepatitis A in the Netherlands indicated by two closely related molecular sequences, July to October 2011. Euro Surveill 17:18–20
Franco E, Meleleo C, Serino L, Sorbara D, Zaratti L (2012) Hepatitis A: epidemiology and prevention in develo** countries. World J Hepatol 4:68–73
Frenck R, Bernstein DI, **a M, Huang P, Zhong W, Parker S, Dickey M, McNeal M, Jiang X (2012) Predicting susceptibility to norovirus GII.4 by use of a challenge model involving humans. J Infect Dis 206:1386–1393
Gallimore CI, Pipkin C, Shrimpton H, Green AD, Pickford Y, McCartney C, Sutherland G, Brown DW, Gray JJ (2005) Detection of multiple enteric virus strains within a foodborne outbreak of gastroenteritis: an indication of the source of contamination. Epidemiol Infect 133:41–47
Gallimore CI, Iturriza-Gomara M, Lewis D, Cubitt D, Cotterill H, Gray JJ (2006) Characterization of sapoviruses collected in the United Kingdom from 1989 to 2004. J Med Virol 78:673–682
Gaulin C, Frigon M, Poirier D, Fournier C (1999) Transmission of calicivirus by a foodhandler in the pre-symptomatic phase of illness. Epidemiol Infect 123:475–478
Glass R (1995) Other viral agents of gastroenteritis. In: Blaser MJ, Smith PD, Ravdin JI, Greenberg HB, Guerrant RL (eds) Infections of the gastrointestinal tract. Raven, New York, pp 1055–1063
Glass RI, Patel M, Parashar U (2011) Lessons from the US rotavirus vaccination program. JAMA 306:1701–1702
Graham RL, Baric RS (2010) Recombination, reservoirs, and the modular spike: mechanisms of coronavirus cross-species transmission. J Virol 84:3134–3146
Graham DY, Dufour GR, Estes MK (1987) Minimal infective dose of rotavirus. Arch Virol 92:261–271
Green KY (2007) Caliciviridae: the noroviruses. In: Knipe DM, Howley PM, Cohen JI, Griffin DE, Lamb RA, MartIn M, Roizman B, Straus SE (eds) Fields virology, 5th edn. Lippincott Williams & Wilkins, Phildelphia, pp 949–979
Green KY (2013) Caliciviridae: the noroviruses. In: Knipe DM, Howley PM, Griffin DE, Lamb RA, Martin MA, Racaniello VR, Roizman B (eds) Fields virology, 6th edn. Lippincott Williams & Wilkins, Philadelphia, pp 582–608
Greenberg HB, Estes MK (2009) Rotaviruses: from pathogenesis to vaccination. Gastroent 136:1939–1951
Greening GE, Hewitt J (2012) Evaluation of intervention strategies for hepatitis A virus on semi-dried tomatoes. In: 3rd Food and Environmental Virology Conference, Lisbon, 10 October 2012
Greening GE, Hewitt J, Hay BE, Grant CM (2003) Persistence of Norwalk-like viruses over time in pacific oysters grown in the natural environment. In: Villalba A, Reguera B, Romalde JL, Beiras R (eds) 4th International Conference on Molluscan Shellfish Safety. Consellería de Pesca e Asuntos Marítimos da Xunta de Galicia and Intergovernmental Oceanographic Commission of UNESCO, Santiago de Compostela, pp 367–377
Greening GE, Lake, RJ, Hudson JA, Cressey PC (2009) Risk profile: norovirus in mollusca (raw). New Zealand Food Safety Authority. October 2009. http://foodsafety.govt.nz/elibrary/industry/Risk_Profile_Norovirus-Science_Research.pdf. Accessed 13 March 2014
Greening GE, Hewitt J, Rivera-Aban M, Croucher D (2012) Molecular epidemiology of norovirus gastroenteritis outbreaks in New Zealand from 2002–2009. J Med Virol 84:1449–1458
Guix S, Caballero S, Villena C, Bartolome R, Latorre C, Rabella N, Simo M, Bosch A, Pinto RM (2002) Molecular epidemiology of astrovirus infection in Barcelona, Spain. J Clin Microbiol 40:133–139
Guix S, Asanaka M, Katayama K, Crawford SE, Neill FH, Atmar RL, Estes MK (2007) Norwalk virus RNA is infectious in mammalian cells. J Virol 81:12238–12248
Halbur PG, Kasorndorkbua C, Gilbert C, Guenette D, Potters MB, Purcell RH, Emerson SU, Toth TE, Meng XJ (2001) Comparative pathogenesis of infection of pigs with hepatitis E viruses recovered from a pig and a human. J Clin Microbiol 39:918–923
Hall AJ, Eisenbart VG, Etingue AL, Gould LH, Lopman BA, Parashar UD (2012) Epidemiology of foodborne norovirus outbreaks, United States, 2001–2008. Emerg Infect Dis 18:1566–1573
Halliday LM, Kang LY, Zhou TK, Hu MD, Pan QC, Fu TY, Huang YS, Hu SL (1991) An epidemic of hepatitis A attributable to the ingestion of raw clams in Shanghai, China. J Infect Dis 164:852–859
Hamza IA, Jurzik L, Uberla K, Wilhelm M (2011) Evaluation of pepper mild mottle virus, human picobirnavirus and torque teno virus as indicators of fecal contamination in river water. Water Res 45:1358–1368
Hansman GS, Oka T, Katayama K, Takeda N (2007a) Human sapoviruses: genetic diversity, recombination, and classification. Rev Med Virol 17:133–141
Hansman GS, Oka T, Okamoto R, Nishida T, Toda S, Noda M, Sano D, Ueki Y, Imai T, Omura T, Nishio O, Kimura H, Takeda N (2007b) Human sapovirus in clams, Japan. Emerg Infect Dis 13:620–622
Hansman GS, Oka T, Li TC, Nishio O, Noda M, Takeda N (2008) Detection of human enteric viruses in Japanese clams. J Food Prot 71:1689–1695
Hernandez F, Monge R, Jimenez C, Taylor L (1997) Rotavirus and hepatitis A virus in market lettuce (Latuca sativa) in Costa Rica. Int J Food Microbiol 37:221–223
Hewitt J, Greening GE (2004) Survival and persistence of norovirus, hepatitis A virus, and feline calicivirus in marinated mussels. J Food Prot 67:1743–1750
Hjertqvist M, Johansson A, Svensson N, Abom PE, Magnusson C, Olsson M, Hedlund KO, Andersson Y (2006) Four outbreaks of norovirus gastroenteritis after consuming raspberries, Sweden, June-August 2006. Euro Surveill 11, E060907.1
Hollinger FB, Emerson SU (2007) Hepatitis A virus. In: Knipe DM, Howley PM, Griffin DE, Lamb RA, Martin M, Roizman B, Straus SE (eds) Fields virology, 5th edn. Lippincott Williams & Wilkins, Philadelphia, pp 911–947
Hung T, Chen GM, Wang CG, Yao HL, Fang ZY, Chao TX, Chou ZY, Ye W, Chang XJ, Den SS, Chang WC (1984) Waterborne outbreak of rotavirus diarrhoea in adults in China caused by a novel rotavirus. Lancet 1:1139–1142
Hutson AM, Atmar RL, Graham DY, Estes MK (2002) Norwalk virus infection and disease is associated with ABO histo-blood group type. J Infect Dis 185:1335–1337
Iizuka S, Matsuda Y, Hoshina K, Itagaki A (2000) An outbreak of group A rotavirus infection among adults from eating meals prepared at a restaurant, April 2000, Shimane. In: IASR, Infectious Agents Surveillance Report, 21 ed. Shimane Prefectural Institute of Public Health and Environmental Science, pp 145–146
Iizuka S, Oka T, Tabara K, Omura T, Katayama K, Takeda N, Noda M (2010) Detection of sapoviruses and noroviruses in an outbreak of gastroenteritis linked genetically to shellfish. J Med Virol 82:1247–1254
International Committee on Taxonomy of Viruses (ICTV) (2012) Master species list. In: ICTV (ed) Version 4. https://talk.ictvonline.org/files/masterspecies-lists/m/msl/4910. Accessed 28 April 2016
Ishida S, Yoshizumi S, Ikeda T, Miyoshi M, Goto A, Matsubayashi K, Ikeda H (2012) Detection and molecular characterization of hepatitis E virus in clinical, environmental and putative animal sources. Arch Virol 157:2363–2368
Jaykus LA, Hemard MT, Sobsey MD (1994) Human enteric pathogenic viruses. In: Pierson MD, Hackney CR (eds) Environmental indicators and shellfish safety. Pierson Associates, Inc., Newport, pp 92–153
Jiang SC (2006) Human adenoviruses in water: occurrence and health implications: a critical review. Environ Sci Technol 40:7132–7140
Jiang V, Jiang B, Tate J, Parashar UD, Patel MM (2010) Performance of rotavirus vaccines in developed and develo** countries. Hum Vacci 6:532–542
Jones MK, Watanabe M, Zhu S, Graves CL, Keyes LR, Grau KR, Gonzalez-Hernandez MB, Iovine NM, Wobus CE, Vinjé J, Tibbetts SA, Wallet SM, Karst SM (2014) Enteric bacteria promote human and mouse norovirus infection of B cells. Science 346:755–759
Jothikumar N, Aparna K, Kamatchiammal S, Paulmurugan R, Saravanadevi S, Khanna P (1993) Detection of hepatitis E virus in raw and treated wastewater with the polymerase chain reaction. Appl Environ Microbiol 59:2558–2562
Jubb G (1915) A third outbreak of poliovirus at West Kirby. Lancet 1:67
Kamar N, Bendall R, Legrand-Abravanel F, **a NS, Ijaz S, Izopet J, Dalton HR (2012) Hepatitis E. Lancet 379:2477–2488
Kapikian AZ, Wyatt RG, Dolin R, Thornhill TS, Kalica AR, Chanock RM (1972) Visualization by immune electron microscopy of a 27-nm particle associated with acute infectious nonbacterial gastroenteritis. J Virol 10:1075–1081
Kaplan JE, Feldman R, Campbell DS, Lookabaugh C, Gary GW (1982) The frequency of a Norwalk-like pattern of illness in outbreaks of acute gastroenteritis. Am J Public Health 72:1329–1332
Khamrin P, Maneekarn N, Peerakome S, Tonusin S, Malasao R, Mizuguchi M, Okitsu S, Ushijima H (2007) Genetic diversity of noroviruses and sapoviruses in children hospitalized with acute gastroenteritis in Chiang Mai, Thailand. J Med Virol 79:1921–1926
Kingsley DH (2013) High pressure processing and its application to the challenge of virus-contaminated foods. Food Environ Virol 5:1–12
Kitahashi T, Tanaka T, Utagawa E (1999) Detection of HAV, SRSV and astrovirus genomes from native oysters in Chiba City, Japan. Kansenshogaku Zasshi 73:559–564
Knight A, Li D, Uyttendaele M, Jaykus LA (2013) A critical review of methods for detecting human noroviruses and predicting their infectivity. Crit Rev Microbiol 39:295–309
Knowles NJ, Hovi T, Hyypia T, King AMQ, Lindberg AM, Pallansch MA, Palmenberg AC, Simmonds P, Skern T, Stanway G, Yamashita T, Zell R (2011a) Family- Picobirnaviridae. In: King AMQ, Adams MJ, Carstens EB, Lefkowitz EJ (eds) Virus taxonomy: classification and nomenclature of viruses: ninth report of the International Committee on Taxonomy of Viruses. Elsevier, San Diego, pp 535–539
Knowles NJ, Hovi T, Hyypia T, King AMQ, Lindberg AM, Pallansch MA, Palmenberg AC, Simmonds P, Skern T, Stanway G, Yamashita T, Zell R (2011b) Family- Picornaviridae. In: King AMQ, Adams MJ, Carstens EB, Lefkowitz EJ (eds) Virus taxonomy: classification and nomenclature of viruses: ninth report of the International Committee on Taxonomy of Viruses. Elsevier, San Diego, pp 855–880
Kobayashi S, Fujiwara N, Yasui Y, Yamashita T, Hiramatsu R, Minagawa H (2012) A foodborne outbreak of sapovirus linked to catered box lunches in Japan. Arch Virol 157:1995–1997
Koizumi Y, Isoda N, Sato Y, Iwaki T, Ono K, Ido K, Sugano K, Takahashi M, Nishizawa T, Okamoto H (2004) Infection of a Japanese patient by genotype 4 hepatitis E virus while traveling in Vietnam. J Clin Microbiol 42:3883–3885
Koopmans M, van Wuijckhuise-Sjouke L, Schukken YH, Cremers H, Horzinek MC (1991) Association of diarrhea in cattle with torovirus infections on farms. Am J Vet Res 52:1769–1773
Koopmans MPG, Cliver DO, Bosch A (2008) Food-borne viruses: progress and challenges. ASM (American Society for Microbiology) Press, Washington
Koroglu M, Yakupogullari Y, Otlu B, Ozturk S, Ozden M, Ozer A, Sener K, Durmaz R (2011) A waterborne outbreak of epidemic diarrhea due to group A rotavirus in Malatya, Turkey. New Microbiol 34:17–24
Korsager B, Hede S, Boggild H, Bottiger BE, Molbak K (2005) Two outbreaks of norovirus infections associated with the consumption of imported frozen raspberries, Denmark, May-June 2005. Euro Surveill 10, E050623.1
Kotwal G, Cannon JL (2014) Environmental persistence and transfer of enteric viruses. Curr Opin Virol 4:37–43
Kroneman A, Vega E, Vennema H, Vinje J, White PA, Hansman G, Green K, Martella V, Katayama K, Koopmans M (2013) Proposal for a unified norovirus nomenclature and genoty**. Arch Virol 158:2059–2068
Kuritsky JN, Osterholm MT, Greenberg HB, Korlath JA, Godes JR, Hedberg CW, Forfang JC, Kapikian AZ, McCullough JC, White KE (1984) Norwalk gastroenteritis: a community outbreak associated with bakery product consumption. Ann Intern Med 100:519–521
L’Homme Y, Sansregret R, Plante-Fortier E, Lamontagne AM, Ouardani M, Lacroix G, Simard C (2009) Genomic characterization of swine caliciviruses representing a new genus of Caliciviridae. Virus Genes 39:66–75
Lay MK, Atmar RL, Guix S, Bharadwaj U, He H, Neill FH, Sastry KJ, Yao QZ, Estes MK (2010) Norwalk virus does not replicate in human macrophages or dendritic cells derived from the peripheral blood of susceptible humans. Virology 406:1–11
Le Guyader F (2006) Norwalk virus-specific binding to oyster digestive tissues. Emerg Infect Dis 12:931–936
Le Guyader FS, Mittelholzer C, Haugarreau L, Hedlund KO, Alsterlund R, Pommepuy M, Svensson L (2004) Detection of noroviruses in raspberries associated with a gastroenteritis outbreak. Int J Food Microbiol 97:179–186
Le Guyader FS, Le Saux JC, Ambert-Balay K, Krol J, Serais O, Parnaudeau S, Giraudon H, Delmas G, Pommepuy M, Pothier P, Atmar RL (2008) Aichi virus, norovirus, astrovirus, enterovirus, and rotavirus involved in clinical cases from a French oyster-related gastroenteritis outbreak. J Clin Microbiol 46:4011–4017
Lee LE, Cebelinski EA, Fuller C, Keene WE, Smith K, Vinje J, Besser JM (2012) Sapovirus outbreaks in long-term care facilities, Oregon and Minnesota, USA, 2002–2009. Emerg Infect Dis 18:873–876
Lees D (2000) Viruses and bivalve shellfish. Int J Food Microbiol 59:81–116
Li TC, Chijiwa K, Sera N, Ishibashi T, Etoh Y, Shinohara Y, Kurata Y, Ishida M, Sakamoto S, Takeda N, Miyamura T (2005) Hepatitis E virus transmission from wild boar meat. Emerg Infect Dis 11:1958–1960
Lindesmith L, Moe C, Marionneau S, Ruvoen N, Jiang X, Lindblad L, Stewart P, LePendu J, Baric R (2003) Human susceptibility and resistance to Norwalk virus infection. Nat Med 9:548–553
Lindesmith L, Moe C, Lependu J, Frelinger JA, Treanor J, Baric RS (2005) Cellular and humoral immunity following Snow Mountain virus challenge. J Virol 79:2900–2909
Lo SV, Connolly AM, Palmer SR, Wright D, Thomas PD, Joynson D (1994) The role of the pre-symptomatic food handler in a common source outbreak of food-borne SRSV gastroenteritis in a group of hospitals. Epidemiol Infect 113:513–521
Maalouf H, Zakhour M, Le Pendu J, Le Saux JC, Atmar RL, Le Guyader FS (2010) Distribution in tissue and seasonal variation of norovirus genogroup I and II ligands in oysters. Appl Environ Microbiol 76:5621–5630
Made D, Trubner K, Neubert E, Hohne M, Johne R (2013) Detection and ty** of norovirus from frozen strawberries involved in a large-scale gastroenteritis outbreak in Germany. Food Environ Virol 5:162–168
Madeley CR, Cosgrove BP (1975) Letter: 28 nm particles in faeces in infantile gastroenteritis. Lancet 2:451–452
Malek MA, Curns AT, Holman RC, Fischer TK, Bresee JS, Glass RI, Steiner CA, Parashar UD (2006) Diarrhea- and rotavirus-associated hospitalizations among children less than 5 years of age: United States, 1997 and 2000. Pediatrics 117:1887–1892
Malek M, Barzilay E, Kramer A, Camp B, Jaykus LA, Escudero-Abarca B, Derrick G, White P, Gerba C, Higgins C, Vinje J, Glass R, Lynch M, Widdowson MA (2009) Outbreak of norovirus infection among river rafters associated with packaged delicatessen meat, Grand Canyon, 2005. Clin Infect Dis 48:31–37
Marks PJ, Vipond IB, Carlisle D, Deakin D, Fey RE, Caul EO (2000) Evidence for airborne transmission of Norwalk-like virus (NLV) in a hotel restaurant. Epidemiol Infect 124:481–487
Martella V, Campolo M, Lorusso E, Cavicchio P, Camero M, Bellacicco AL, Decaro N, Elia G, Greco G, Corrente M, Desario C, Arista S, Banyai K, Koopmans M, Buonavoglia C (2007) Norovirus in captive lion cub (Panthera leo). Emerg Infect Dis 13:1071–1073
Martella V, Lorusso E, Banyai K, Decaro N, Corrente M, Elia G, Cavalli A, Radogna A, Costantini V, Saif LJ, Lavazza A, Di Trani L, Buonavoglia C (2008a) Identification of a porcine calicivirus related genetically to human sapoviruses. J Clin Microbiol 46:1907–1913
Martella V, Lorusso E, Decaro N, Elia G, Radogna A, D’Abramo M, Desario C, Cavalli A, Corrente M, Camero M, Germinario CA, Banyai K, Di Martino B, Marsilio F, Carmichael LE, Buonavoglia C (2008b) Detection and molecular characterization of a canine norovirus. Emerg Infect Dis 14:1306–1308
Martella V, Banyai K, Matthijnssens J, Buonavoglia C, Ciarlet M (2010) Zoonotic aspects of rotaviruses. Vet Microbiol 140:246–255
Masclaux FG, Hotz P, Friedli D, Savova-Bianchi D, Oppliger A (2013) High occurrence of hepatitis E virus in samples from wastewater treatment plants in Switzerland and comparison with other enteric viruses. Water Res 47:5101–5109
Masuda J, Yano K, Tamada Y, Takii Y, Ito M, Omagari K, Kohno S (2005) Acute hepatitis E of a man who consumed wild boar meat prior to the onset of illness in Nagasaki, Japan. J Jpn Soc Hepatol 31:178–183
Mathijs E, Stals A, Baert L, Botteldoorn N, Denayer S, Mauroy A, Scipioni A, Daube G, Dierick K, Herman L, Van Coillie E, Uyttendaele M, Thiry E (2012) A review of known and hypothetical transmission routes for noroviruses. Food Environ Virol 4:131–152
Matsubayashi K, Kang JH, Sakata H, Takahashi K, Shindo M, Kato M, Sato S, Kato T, Nishimori H, Tsuji K, Maguchi H, Yoshida J, Maekubo H, Mishiro S, Ikeda H (2008) A case of transfusion-transmitted hepatitis E caused by blood from a donor infected with hepatitis E virus via zoonotic food-borne route. Transfusion 48:1368–1375
Matsuda H, Okada K, Takahashi K, Mishiro S (2003) Severe hepatitis E virus infection after ingestion of uncooked liver from a wild boar. J Infect Dis 188:944
Matthijnssens J, Ciarlet M, Rahman M, Attoui H, Banyai K, Estes MK, Gentsch JR, Iturriza-Gomara M, Kirkwood CD, Martella V, Mertens PP, Nakagomi O, Patton JT, Ruggeri FM, Saif LJ, Santos N, Steyer A, Taniguchi K, Desselberger U, Van Ranst M (2008) Recommendations for the classification of group A rotaviruses using all 11 genomic RNA segments. Arch Virol 153:1621–1629
Mattison K, Shukla A, Cook A, Pollari F, Friendship R, Kelton D, Bidawid S, Farber JM (2007) Human noroviruses in swine and cattle. Emerg Infect Dis 13:1184–1188
Maunula L, Roivainen M, Keranen M, Makela S, Soderberg K, Summa M, von Bonsdorff CH, Lappalainen M, Korhonen T, Kuusi M, Niskanen T (2009) Detection of human norovirus from frozen raspberries in a cluster of gastroenteritis outbreaks. Euro Surveill 14:16–18
Maunula L, Kaupke A, Vasickova P, Soderberg K, Kozyra I, Lazic S, van der Poel WH, Bouwknegt M, Rutjes S, Willems KA, Moloney R, D’Agostino M, de Roda Husman AM, von Bonsdorff CH, Rzezutka A, Pavlik I, Petrovic T, Cook N (2013) Tracing enteric viruses in the European berry fruit supply chain. Int J Food Microbiol 167:177–185
McLeod C, Hay B, Grant C, Greening G, Day D (2009) Inactivation and elimination of human enteric viruses by pacific oysters. J Appl Microbiol 107:1809–1818
Mendez E, Arias CF (2007) Astroviruses. In: Knipe DM, Howley PM, Griffin DE, Lamb RA, Martin M, Roizman B, Straus SE (eds) Fields virology, 5th edn. Lippincott Williams & Wilkins, Philadelphia, pp 981–1000
Meng XJ (2011) From barnyard to food table: the omnipresence of hepatitis E virus and risk for zoonotic infection and food safety. Virus Res 161:23–30
Milne-Price S, Miazgowicz KL, Munster VJ (2014) The emergence of the Middle East respiratory syndrome coronavirus (MERS-CoV). Pathog Dis 71:119–134
Ming HX, Fan JF, Wu LJ, Liang YB (2013) Prevalence of human enteric viruses and a potential indicator of contamination in shellfish in China. J Food Saf 33:209–214
Molinari BLD, Lorenzetti E, Otonel RAA, Alfieri AF, Alfieri AA (2014) Species H rotavirus detected in piglets with diarrhea, Brazil, 2012. Emerg Infect Dis 20:1019–1022
Morillo SG, Luchs A, Cilli A, Ribeiro CD, Calux SJ, Carmona Rde C, Timenetsky Mdo C (2011) Norovirus 3rd generation kit: an improvement for rapid diagnosis of sporadic gastroenteritis cases and valuable for outbreak detection. J Virol Methods 173:13–16
Motarjemi Y, Kaferstein F, Moy G, Quevedo F (1993) Contaminated weaning food: a major risk factor for diarrheoea and associated malnutrition. Bull World Health Organ 71:79–92
Mushahwar IK (2008) Hepatitis E virus: molecular virology, clinical features, diagnosis, transmission, epidemiology, and prevention. J Med Virol 80:646–658
Nakagawa-Okamoto R, Arita-Nishida T, Toda S, Kato H, Iwata H, Akiyama M, Nishio O, Kimura H, Noda M, Takeda N, Oka T (2009) Detection of multiple sapovirus genotypes and genogroups in oyster-associated outbreaks. Jpn J Infect Dis 62:63–66
Nappier SP, Graczyk TK, Schwab KJ (2008) Bioaccumulation, retention, and depuration of enteric viruses by Crassostrea virginica and Crassostrea ariakensis oysters. Appl Environ Microbiol 74:6825–6831
Nappier SP, Graczyk TK, Tamang L, Schwab KJ (2010) Co-localized Crassostrea virginica and Crassostrea ariakensis oysters differ in bioaccumulation, retention and depuration of microbial indicators and human enteropathogens. J Appl Microbiol 108:736–744
Niu MT, Polish LB, Robertson BH, Khanna BK, Woodruff BA, Shapiro CN, Miller MA, Smith JD, Gedrose JK, Alter MJ, Margolis HS (1992) Multistate outbreak of hepatitis A associated with frozen strawberries. J Infect Dis 166:518–524
Noel JS, Liu BJ, Humphrey CD, Rodriguez EM, Lambden PR, Clarke IN, Dwyer DM, Ando T, Glass RI, Monroe SS (1997) Parkville virus: a novel genetic variant of human calicivirus in the sapporo virus clade, associated with an outbreak of gastroenteritis in adults. J Med Virol 52:173–178
Oh DY, Silva PA, Hauroeder B, Diedrich S, Cardoso DD, Schreier E (2006) Molecular characterization of the first aichi viruses isolated in Europe and in South America. Arch Virol 151:1199–1206
Oishi I, Yamazaki K, Kimoto T, Minekawa Y, Utagawa E, Yamazaki S, Inouye S, Grohmann GS, Monroe SS, Stine SE et al (1994) A large outbreak of acute gastroenteritis associated with astrovirus among students and teachers in Osaka, Japan. J Infect Dis 170:439–443
Oka T, Mori K, Iritani N, Harada S, Ueki Y, Iizuka S, Mise K, Murakami K, Wakita T, Katayama K (2012) Human sapovirus classification based on complete capsid nucleotide sequences. Arch Virol 157:349–352
Oka T, Wang Q, Katayama K, Saif LJ (2015) Comprehensive review of human sapoviruses. Clin Microbiol Rev 28:32–53
Pang XL, Lee BE, Tyrrell GJ, Preiksaitis JK (2009) Epidemiology and genotype analysis of sapovirus associated with gastroenteritis outbreaks in Alberta, Canada: 2004–2007. J Infect Dis 199:547–551
Papafragkou E, Hewitt J, Park GW, Greening G, Vinje J (2013) Challenges of culturing human norovirus in three-dimensional organoid intestinal cell culture models. PLoS One 8, e63485
Parashar UD, Dow L, Fankhauser RL, Humphrey CD, Miller J, Ando T, Williams KS, Eddy CR, Noel JS, Ingram T, Bresee JS, Monroe SS, Glass RI (1998) An outbreak of viral gastroenteritis associated with consumption of sandwiches: implications for the control of transmission by food handlers. Epidemiol Infect 121:615–621
Parashar UD, Alexander JP, Glass RI (2006a) Prevention of rotavirus gastroenteritis among infants and children: recommendations of the advisory committee on immunization practices (ACIP). MMWR Recomm Rep 55:1–13
Parashar UD, Gibson CJ, Bresee JS, Glass RI (2006b) Rotavirus and severe childhood diarrhea. Emerg Infect Dis 12:304–306
Patel MM, Hall AJ, Vinje J, Parashara UD (2009) Noroviruses: a comprehensive review. J Clin Virol 44:1–8
Pebody RG, Leino T, Ruutu P, Kinnunen L, Davidkin I, Nohynek H, Leinikki P (1998) Foodborne outbreaks of hepatitis A in a low endemic country: an emerging problem? Epidemiol Infect 120:55–59
Petrignani M, Harms M, Verhoef L, van Hunen R, Swaan C, van Steenbergen J, Boxman I, Peran ISR, Ober H, Vennema H, Koopmans M, van Pelt W (2010) Update: a food-borne outbreak of hepatitis A in the Netherlands related to semi-dried tomatoes in oil, January-February 2010. Euro Surveill 15, 19572
Pina S, Jofre J, Emerson SU, Purcell RH, Girones R (1998) Characterization of a strain of infectious hepatitis E virus isolated from sewage in an area where hepatitis E is not endemic. Appl Environ Microbiol 64:4485–4488
Pina S, Buti M, Cotrina M, Piella J, Girones R (2000) HEV identified in serum from humans with acute hepatitis and in sewage of animal origin in Spain. J Hepatol 33:826–833
Pinto P, Wang Q, Chen N, Dubovi EJ, Daniels JB, Millward LM, Buonavoglia C, Martella V, Saif LJ (2012) Discovery and genomic characterization of noroviruses from a gastroenteritis outbreak in domestic cats in the US. PLoS One 7, e32739
Pol S, Corouge M, Fontaine H (2011) Hepatitis B virus infection and pregnancy. Clin Res Hepatol Gastroenterol 35:618–622
Ponka A, Maunula L, von Bonsdorff CH, Lyytikainen O (1999) An outbreak of calicivirus associated with consumption of frozen raspberries. Epidemiol Infect 123:469–474
Ramsay CN, Upton PA (1989) Hepatitis A and frozen raspberries. Lancet 1:43–44
Reid TM, Robinson HG (1987) Frozen raspberries and hepatitis A. Epidemiol Infect 98:109–112
Richards AF, Lopman B, Gunn A, Curry A, Ellis D, Cotterill H, Ratcliffe S, Jenkins M, Appleton H, Gallimore CI, Gray JJ, Brown DW (2003) Evaluation of a commercial ELISA for detecting Norwalk-like virus antigen in faeces. J Clin Virol 26:109–115
Robertson BH, Khanna B, Nainan OV, Margolis HS (1991) Epidemiologic patterns of wild-type hepatitis A virus determined by genetic variation. J Infect Dis 163:286–292
Robertson BH, Jansen RW, Khanna B, Totsuka A, Nainan OV, Siegl G, Widell A, Margolis HS, Isomura S, Ito K, Ishizu T, Moritsugu Y, Lemon SM (1992) Genetic relatedness of hepatitis A virus strains recovered from different geographic regions. J Gen Virol 73:1365–1377
Rockx BH, Bogers WM, Heeney JL, van Amerongen G, Koopmans MP (2005) Experimental norovirus infections in non-human primates. J Med Virol 75:313–320
Sarvikivi E, Roivainen M, Maunula L, Niskanen T, Korhonen T, Lappalainen M, Kuusi M (2012) Multiple norovirus outbreaks linked to imported frozen raspberries. Epidemiol Infect 140:260–267
Sattar SA, Tetro JA (2001) Other foodborne viruses. In: Hui YH, Sattar SA, Murrell KD, Nip W-K, Stanfield PS (eds) Foodborne disease handbook: viruses, parasites, pathogens, and HACCP, 2nd edn. Marcel Dekker, New York, pp 127–136
Scallan E, Hoekstra RM, Angulo FJ, Tauxe RV, Widdowson MA, Roy SL, Jones JL, Griffin PM (2011) Foodborne illness acquired in the United States-major pathogens. Emerg Infect Dis 17:7–15
Scheuer KA, Oka T, Hoet AE, Gebreyes WA, Molla BZ, Saif LJ, Wang Q (2013) Prevalence of porcine noroviruses, molecular characterization of emerging porcine sapoviruses from finisher swine in the United States, and unified classification scheme for sapoviruses. J Clin Microbiol 51:2344–2353
Schwab KJ, Neill FH, Fankhauser RL, Daniels NA, Monroe SS, Bergmire-Sweat DA, Estes MK, Atmar RL (2000) Development of methods to detect “Norwalk-like viruses” (NLVs) and hepatitis A virus in delicatessen foods: application to a food-borne NLV outbreak. Appl Environ Microbiol 66:213–218
Seitz SR, Leon JS, Schwab KJ, Lyon GM, Dowd M, McDaniels M, Abdulhafid G, Fernandez ML, Lindesmith LC, Baric RS, Moe CL (2011) Norovirus infectivity in humans and persistence in water. Appl Environ Microbiol 77:6884–6888
Simmons G, Greening G, Gao W, Campbell D (2001) Raw oyster consumption and outbreaks of viral gastroenteritis in New Zealand: Evidence for risk to the public’s health. Aust N Z J Public Health 25:234–240
Smith DB, Simmonds P, members of the International Committee on Taxonomy of Viruses Hepeviridae Study Group, Jameel S, Emerson SU, Harrison TJ, Meng X-J, Okamoto H, Van der Poel WHM, Purdy MA (2014) Consensus proposals for classification of the family Hepeviridae. J Gen Virol 95:2223–2232
Sobsey MD, Shields PA, Hauchman F, Davis A, Rullman V, Bosch A (1988) Survival and persistence of hepatitis A virus in environmental samples. In: Zuckermann A (ed) Viral hepatitis and liver disease. Alan Liss, New York, pp 121–124
Souza M, Azevedo MS, Jung K, Cheetham S, Saif LJ (2008) Pathogenesis and immune responses in gnotobiotic calves after infection with the genogroup II.4-hs66 strain of human norovirus. J Virol 82:1777–1786
Summa M, von Bonsdorff CH, Maunula L (2012) Pet dogs--a transmission route for human noroviruses? J Clin Virol 53:244–247
Svraka S, Vennema H, van der Veer B, Hedlund KO, Thorhagen M, Siebenga J, Duizer E, Koopmans M (2010) Epidemiology and genotype analysis of emerging sapovirus-associated infections across Europe. J Clin Microbiol 48:2191–2198
Takahashi M, Nishizawa T, Okamoto H (2003) Identification of a genotype III swine hepatitis E virus that was isolated from a Japanese pig born in 1990 and that is most closely related to Japanese isolates of human hepatitis E virus. J Clin Microbiol 41:1342–1343
Takahashi K, Kitajima N, Abe N, Mishiro S (2004) Complete or near-complete nucleotide sequences of hepatitis E virus genome recovered from a wild boar, a deer, and four patients who ate the deer. Virology 330:501–505
Takanashi S, Wang Q, Chen N, Shen Q, Jung K, Zhang Z, Yokoyama M, Lindesmith LC, Baric RS, Saif LJ (2011) Characterization of emerging GII.g/GII.12 noroviruses from a gastroenteritis outbreak in the United States in 2010. J Clin Microbiol 49:3234–3244
Tan M, Jiang X (2010) Norovirus gastroenteritis, carbohydrate receptors, and animal models. PLoS Pathog 6, e1000983
Tate JE, Mutuc JD, Panozzo CA, Payne DC, Cortese MM, Cortes JE, Yen C, Esposito DH, Lopman BA, Patel MM, Parashar UD (2011) Sustained decline in rotavirus detections in the United States following the introduction of rotavirus vaccine in 2006. Pediatr Infect Dis J 30:S30–S34
Taube S, Kolawole AO, Hohne M, Wilkinson JE, Handley SA, Perry JW, Thackray LB, Akkina R, Wobus CE (2013) A mouse model for human norovirus. MBio 4, e00450-13
Tei S, Kitajima N, Takahashi K, Mishiro S (2003) Zoonotic transmission of hepatitis E virus from deer to human beings. Lancet 362:371–373
Tei S, Kitajima N, Ohara S, Inoue Y, Miki M, Yamatani T, Yamabe H, Mishiro S, Kinoshita Y (2004) Consumption of uncooked deer meat as a risk factor for hepatitis E virus infection: an age- and sex-matched case–control study. J Med Virol 74:67–70
Teunis PF, Moe CL, Liu P, Miller SE, Lindesmith L, Baric RS, Le Pendu J, Calderon RL (2008) Norwalk virus: how infectious is it? J Med Virol 80:1468–1476
Thornley CN, Hewitt J, Perumal L, Van Gessel SM, Wong J, David SA, Rapana JP, Li S, Marshall JC, Greening GE (2013) Multiple outbreaks of a novel norovirus GII.4 linked to an infected post-symptomatic food handler. Epidemiol Infect 141:1585–1597
Tian P, Engelbrektson AL, Jiang X, Zhong W, Mandrell RE (2007) Norovirus recognizes histo-blood group antigens on gastrointestinal cells of clams, mussels, and oysters: a possible mechanism of bioaccumulation. J Food Prot 70:2140–2147
Ueki Y, Shoji M, Okimura Y, Miyota Y, Masago Y, Oka T, Katayama K, Takeda N, Noda M, Miura T, Sano D, Omura T (2010) Detection of sapovirus in oysters. Microbiol Immunol 54:483–486
Van Regenmortel MHV (2000) Virus taxonomy: classification and nomenclature of viruses: seventh report of the International Committee on Taxonomy of Viruses. Academic, San Diego
Verhoef L, Vennema H, van Pelt W, Lees D, Boshuizen H, Henshilwood K, Koopmans M (2010) Use of norovirus genotype profiles to differentiate origins of foodborne outbreaks. Emerg Infect Dis 16:617–624
Wang QH, Han MG, Cheetham S, Souza M, Funk JA, Saif LJ (2005) Porcine noroviruses related to human noroviruses. Emerg Infect Dis 11:1874–1881
Wang Q, Zhang Z, Saif LJ (2012) Stability of and attachment to lettuce by a culturable porcine sapovirus surrogate for human caliciviruses. Appl Environ Microbiol 78:3932–3940
Widdowson MA, Rockx B, Schepp R, van der Poel WH, Vinje J, van Duynhoven YT, Koopmans MP (2005) Detection of serum antibodies to bovine norovirus in veterinarians and the general population in the Netherlands. J Med Virol 76:119–128
Wikswo ME, Hall AJ (2012) Outbreaks of acute gastroenteritis transmitted by person-to-person contact--United States, 2009–2010. MMWR Surveill Summ 61:1–12
Williamson WM, Ball A, Wolf S, Hewitt J, Lin S, Scholes P, Ambrose V, Robson B, Greening GE (2011) Enteric viruses in New Zealand drinking-water sources. Water Sci Technol 63:1744–1751
Wobus CE, Thackray LB, Virgin HW (2006) Murine norovirus: a model system to study norovirus biology and pathogenesis. J Virol 80:5104–5112
Wold WSM, Horwitz MS (2007) Adenoviruses. In: Knipe DM, Howley PM, Griffin DE, Lamb RA, Martin MA, Roizman B, Straus SE (eds) Fields virology, 5th edn. Lippincott Williams & Wilkins, Baltimore, pp 2395–2436
Wong K, Fong TT, Bibby K, Molina M (2012) Application of enteric viruses for fecal pollution source tracking in environmental waters. Environ Int 45:151–164
Woode GN, Reed DE, Runnels PL, Herrig MA, Hill HT (1982) Studies with an unclassified virus isolated from diarrheic calves. Vet Microbiol 7:221–240
World Health Organization (WHO) (2009) Meeting of the strategic advisory group of experts on immunization, October 2009—conclusions and recommendations. Wkly Epidemiol Rec 518
Yamashita T, Kobayashi S, Sakae K, Nakata S, Chiba S, Ishihara Y, Isomura S (1991) Isolation of cytopathic small round viruses with BS-C-1 cells from patients with gastroenteritis. J Infect Dis 164:954–957
Yamashita T, Sakae K, Ishihara Y, Isomura S, Utagawa E (1993) Prevalence of newly isolated, cytopathic small round virus (aichi strain) in Japan. J Clin Microbiol 31:2938–2943
Yamashita T, Sakae K, Tsuzuki H, Suzuki Y, Ishikawa N, Takeda N, Miyamura T, Yamazaki S (1998) Complete nucleotide sequence and genetic organization of aichi virus, a distinct member of the Picornaviridae associated with acute gastroenteritis in humans. J Virol 72:8408–8412
Yamashita Y, Ootsuka Y, Kondo R, Oseto M, Doi M, Miyamoto T, Ueda T, Kondo H, Tanaka T, Wakita T, Katayama K, Takeda N, Oka T (2010) Molecular characterization of sapovirus detected in a gastroenteritis outbreak at a wedding hall. J Med Virol 82:720–726
Yazaki Y, Mizuo H, Takahashi M, Nishizawa T, Sasaki N, Gotanda Y, Okamoto H (2003) Sporadic acute or fulminant hepatitis E in Hokkaido, Japan, may be food-borne, as suggested by the presence of hepatitis E virus in pig liver as food. J Gen Virol 84:2351–2357
Yen C, Tate JE, Patel MM, Cortese MM, Lopman B, Fleming J, Lewis K, Jiang B, Gentsch J, Steele D, Parashar UD (2011) Rotavirus vaccines: update on global impact and future priorities. Hum Vaccin 7:1282–1290
Yoshida T, Kasuo S, Azegami Y, Uchiyama Y, Satsumabayashi K, Shiraishi T, Katayama K, Wakita T, Takeda N, Oka T (2009) Characterization of sapoviruses detected in gastroenteritis outbreaks and identification of asymptomatic adults with high viral load. J Clin Virol 45:67–71
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Greening, G.E., Cannon, J.L. (2016). Human and Animal Viruses in Food (Including Taxonomy of Enteric Viruses). In: Goyal, S., Cannon, J. (eds) Viruses in Foods. Food Microbiology and Food Safety(). Springer, Cham. https://doi.org/10.1007/978-3-319-30723-7_2
Download citation
DOI: https://doi.org/10.1007/978-3-319-30723-7_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-30721-3
Online ISBN: 978-3-319-30723-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)