Abstract
Background: The burden of disease of obstructive sleep apnea (OSA) is highly underestimated by policy-makers. Therefore, diagnosis and treatment of OSA are often not prioritized in healthcare budget decision-making.
Objective: Analysis on the effect of OSA as a risk factor for other comorbidities on the (economic) burden of the disease, compared to OSA as a “stand-alone” medical condition.
Methods: Literature evaluation on the burden of disease of OSA.
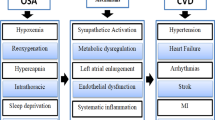
Results: OSA is a risk factor for comorbidities such as ischemic heart disease, stroke, and diabetes mellitus which are listed in the top three World Health Organization (WHO) global causes of disability-adjusted life years (DALYs). With a broader society perspective, cost of illness studies of OSA conclude that the disease produces a substantial economic burden, with indirect costs due to morbidity as one of the main cost drivers. Instead of focusing on direct treatment costs of OSA, publications emphasizing the potential economic benefit from a payer perspective are increasing and with positive results. Cost-effectiveness analysis defining OSA as a risk factor for comorbidities concludes positively; society benefits from treating OSA.
Conclusion: The disease burden of OSA as a risk factor for comorbidities is higher than OSA as a “stand-alone” medical condition. Additionally, the treatment of OSA is economically beneficial. This evaluation serves as a call for action to prioritize the treatment and diagnosis of OSA in healthcare budget decision-making by policy-makers.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Wickwire E. Value-based sleep and breathing: health economic aspects of obstructive sleep apnea. Faculty Rev. 2021;10(40) https://doi.org/10.12703/r/10-40.
Blissett D, Blissett R. Synchronized hypoglossal nerve stimulation with inspire for untreated severe obstructive sleep apnoea/hypopnoea syndrome: a simulated cost-utility analysis from a National Health Service Perspective. Pharmacoecon Open. 2021;5(3):475–89.
NCCID. Understanding summary measures used to estimate the burden of disease: all about HALY’s, DALYS and QALYS; 2015.
Wickwire E, Towe M. The impact of treatments for OSA on monetized health economic outcomes: a systematic review. Chest. 2019;155(5):947–61.
WHO Disease Burden 2000–2019. https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates/global-health-estimates-leading-causes-of-dalys
Himanshu W. What is the mortality rate for sleep apnea (OSA)? 2020. https://www.medscape.com/answers/295807-53497/what-is-the-mortality-rate-for-sleep-apnea-osa
Jose M, Alvar G. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365(9464):1046–53.
Young T, Stubbs R. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep. 2008;31(8):1071–8.
Pietzsch J, Geisler BP. Clinical and economic benefits of upper airway stimulation for obstructive sleep apnea in a European setting. Respiration. 2019;98(1):38–47.
Pevernagie D, Grote L. On the rise and fall of the apnea−hypopnea index: a historical review and critical appraisal. J Sleep Res. 2020;00:e13066. https://doi.org/10.1111/jsr.13066.
AlGhanim N, Ajas N. The economic impact of obstructive sleep. Apnea. 2007;186:7–12.
Guest JF. Clinical outcomes and cost-effectiveness of continuous positive airway pressure to manage obstructive sleep apnea in patients with type 2 diabetes in the U.K. Diabetes Care. 2014;37(5):1263–71.
Frost and Sullivan. American Academy of Sleep Medicine: Hidden health crisis costing America billions: Underdiagnosing and undertreating obstructive sleep apnea draining healthcare system; 2016. https://aasm.org/resources/pdf/sleep-apnea-economic-crisis.pdf
Grunstein R, Sjostrom L. Impact of self-reported sleep-breathing disturbances on psychosocialperformance in the Swedish obese subjects (SOS) study. Sleep. 1995;18:635–43.
Jennum P, Kjellberg J. Health, social and economical consequences of sleep- disordered breathing: a controlled national study. Thorax. 2011;66:560–6.
Jennum P, Kjellberg J. Social consequences of sleep disordered breathing on patients and their partners. A controlled national study. Eur Respir J. 2013;43(1):134–44.
Young T. Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep. 1997;20(9):705–6.
Bahammam A, Kryger M. Health care utilization in males with obstructive sleep apnea syndrome two years after diagnosis and treatment. Sleep. 1999;22(6):740–7.
Taraskiuka A, Reuvenib H. The economic impact of obstructive sleep apnea. Curr Opin Pulm Med. 2013;19(6):639–44.
Gami A, Somers V. Association of atrial fibrillation and obstructive sleep apnea. Circulation. 2004;110:364–7.
Harris M, Grunstein R. Obstructive sleep apnea and depression. Sleep Med Rev. 2009;13:437–44.
FIRS. The global burden of sleep apnoea; 2019. doi: https://doi.org/10.1016/S2213-2600(19)30226-7.
Benjafield A, Eastwood P. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med. 2019;7:687–98.
Lyons M, Magalang U. Global burden of sleep-disordered breathing and its implications. Respirology. 2020;25(7):690–702.
Afshin A, Murray C. Health effects of overweight and obesity in 195 countries. N Engl J Med. 2017;377:1496–7.
Romero-Corral A, Somers V. Interactions between obesity and obstructive sleep apnea: implications for treatment. Chest. 2010;137:711–9.
Peppard P, Hla K. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177:1006–14.
Schwartz A, Smith PL. Obesity and obstructive sleep apnea: pathogenic mechanisms and therapeutic approaches. Proc Am Thorac Soc. 2008;5:185–92.
Kim J, Park C (2004) Prevalence of sleep-disordered breathing in middle-aged Korean men and women. Am J Respir Crit Care Med170: 1108–1113.
Linz B, Hohl M. Repeated exposure to transient obstructive sleep apnea–related conditions causes an atrial fibrillation substrate in a chronic rat model. Heart Rythm. 2021;18(3):455–64.
Wickwire E. Value-based sleep and breathing: health economic aspects of obstructive sleep apnea. Fac Rev. 2021;10:40.
Wickwire E, Scharf S. The impact on monetized health economic outcomes of treatments for OSAA systematic review. Chest. 2019;155(5):947–61.
Potts KJ, Sims P. Cost savings associated with an education campaign on the diagnosis and management of sleep-disordered breathing: a retrospective, claims-based US study. Popul Health Manag. 2013;16:7–1.
Brouwer W. When is it too expensive? Cost-effectiveness thresholds and health care decision-making. Eur J Health Econ. 2019;20(2):175–80.
Edney LC. Estimating the reference incremental cost-effectiveness ratio for the Australian health system. PharmacoEcon. 2018;36(2):239–52.
Billings M, Kapur V. Medicare long-term CPAP coverage policy: a cost-utility analysis. J Clin Sleep Med. 2013;9(10):1023–9.
Catala R, Merino M. Cost-effectiveness of continuous positive airway pressure treatment in moderate-severe obstructive sleep apnea syndrome, Arch Bronconeumol. 2016;52(9):461–9.
Guest J, Stradling J. Cost-effectiveness of using continuous positive airway pressure in the treatment of severe obstructive sleep apnoea/hypopnoea syndrome in the UK. Thorax. 2008;63(10):860–5.
McDaid C, Weatherly H. Continuous positive airway pressure devices for the treatment of obstructive sleep apnoea-hypopnoea syndrome: a systematic review and economic analysis. Health Technol Assess. 2009;13(4).:iii–iv, xi–xiv, 1–119, 143–274.
Poullie A, Gauthier A. Cost-effectiveness of treatments for mild- to-moderate obstructive sleep apnea in France. Int J Technol Assess Health Care. 2016;32(1–2):37–45.
Weatherly HL, Mc Daid C. An economic analysis of continuous positive airway pressure for the treatment of obstructive sleep apnea-hypopnea syndrome. Int J Technol Assess Health Care. 2009;25(1):26–34.
Sleep Health Foundation & Deloitte Access Economics. Asleep on the job: costs of inadequate sleep in Australia; 2017. https://www.sleephealthfoundation.org.au/files/Asleep_on_the_job/Asleep_on_the_Job_SHF_report-WEB_small.pdf
Streatfeild J, Pezullo L. Cost-effectiveness of continuous positive airway pressure therapy for obstructive sleep apnea: health care system and societal perspectives. Sleep. 2019;42:zsz181–12.
Armeni P, Gupta A. Cost-of-illness study of obstructive sleep apnea syndrome (OSAS) in Italy. SDA Bocconi School of Management; 2019.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Carrasco-Llatas, M., Wollny, M., Bos, N. (2023). Burden of Disease. In: Baptista, P.M., Lugo Saldaña, R., Amado, S. (eds) Obstructive Sleep Apnea. Springer, Cham. https://doi.org/10.1007/978-3-031-35225-6_32
Download citation
DOI: https://doi.org/10.1007/978-3-031-35225-6_32
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-35224-9
Online ISBN: 978-3-031-35225-6
eBook Packages: MedicineMedicine (R0)