Abstract
This book chapter is dedicated to map** and analyzing the digital mental health servicescape as an ecosystem generating transformative value and contributing to overall consumer wellbeing. The value propositions of multiple forms of digital mental health service offerings are discussed, and recommendations are provided to managers and retailers for optimizing consumer experience and value creation in the digital mental health services sector.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Introduction
In 2018, the European Commission announced the advent of the Digital Decade, emphasizing the digital transformation of businesses and public services (European Commission, 2018). Particular attention was paid to the digitalization of healthcare system, with billions in funding being directed to mobile health apps, making it one of the most promising fields in the digital health sector.
In recent years, digital mental health services have emerged as an alternative to in-person psychotherapy treatment, and their proliferation has been greatly intensified by the COVID-19 pandemic. The digital mental health market has experienced unprecedented growth over the past few years (Statista, 2022). More and more mental health professionals are offering their services online and exploring new formats, for example, online group psychotherapy, webinars, multi-day social media workshops, and pre-recorded mental health sessions. The online platforms serving as service provider aggregators are making mental health services available globally on a 24/7 basis, and the emergence of artificial intelligence-powered mental health apps, for example, Replika, has in some instances completely removed a human psychotherapist from the equation. Nevertheless, currently, scholars cannot come to an agreement regarding whether or not these services can lead to successful positive outcomes compared with traditional psychotherapy that involves the physical presence of therapists and consumers in a shared space.
But are we going in the right direction, in turning mental healthcare services into a market commodity, removing the intricate human therapeutic relationship from the equation and replacing it with an uberized customer experience? With the rapid onset of digitalization and the fourth industrial revolution, researchers have been raising concerns during recent years over the potential effects these processes can have on consumer wellbeing and value creation, especially in the domains of healthcare and personal relationships (Boninsegni et al., 2022).
While extant research on digital mental health services tends to focus on their clinical aspects, treating these services as a unified landscape, it is important to also acknowledge the unregulated proliferation of multiple value propositions in the non-clinical sector which is playing an increasingly important part in the daily lives of consumers. The purpose of the current chapter is to investigate the digital mental health servicescape as a service ecosystem composed of multiple clinical and non-clinical market actors. In doing so, we seek to answer the following research questions: (1) How is the digital mental health servicescape organized? and (2) What are the characteristics of multiple actors in digital mental health services ecosystems? Specifically, we provide an overview of the main market actors, as well as their specifics and value propositions, and we discuss the specific mechanisms of value co-creation and co-destruction in this setting. We share ethical reflections on whether the transformation of traditional psychotherapy into digital retail therapy can result in cheaper, faster and better treatment, or whether certain aspects of standards of practice, for example, a therapeutic relationship between a patient and his/her psychotherapist, could be compromised in digital mental health services settings. Finally, we provide recommendations for retail managers and digital mental health service providers as regards optimizing the transformative and therapeutic service experiences of consumers.
Value Creation and Consumer Wellbeing in Digital Mental Health Ecosystems
Many scholars in the field of marketing and service research have dedicated their time and effort to studying the concept of value. Despite an ever-growing number of contributions in the field, we are not getting any closer to providing a unified definition of value, while acknowledging its idiosyncratic and context-dependent nature. Current understanding indicates that successful value creation means that, after engaging with the service, a customer would feel better off after his/her interaction with the service (Gronroos, 2011). At the same time, it is not only true that value can be created, it can also be destroyed as multiple actors interact with each other during the service process.
If we regard digital mental health services as an ecosystem (Anderson & Ostrom, 2015; Vargo et al., 2017), we can observe the interactions between consumers and service providers, who function together in a shared context, co-creating value through processes of market exchange. The value derived from the interactions between the market actors in this ecosystem serves as a function of collective wellbeing. The creation, or co-creation, of value is not an automatic result of the exchange. The interrelationship between market actors can co-create value in cases where the expectations and perceptions of both the service providers and the customers are aligned (Rintamäki & Saarijärvi, 2021). However, the value can also be co-destroyed in cases where the notions of value in the marketplace come into conflict with each other (Minina et al., 2022), or in cases where the participants in the exchange process misuse the resources available to them (Plé & Cáceres, 2010). In the context of digital mental health, we can regard the value derived from this service experience as transformative value that creates an uplifting change and improves consumer wellbeing (Blocker & Barrios, 2015).
Before we proceed, it is important to specify the notion of consumer wellbeing, which is gaining the interest of researchers, but nevertheless remaining a notoriously “fluffy” concept that is hard to define or measure. According to Dodge et al. (2012), stable wellbeing can be observed when individuals have the resources (social, physical and psychological) to meet particular challenges during their everyday lives. In transformative service research (Anderson & Ostrom, 2015), the dimensions of wellbeing are defined as physical health, mental health, financial wellbeing, marginalization, discrimination, literacy, inclusion, access, capacity-building and decreased disparity. Digital mental health services are being marketed as a tool for improving consumer wellbeing, reducing the strain on mental health services, and increasing access by underrepresented groups. These advantages depend heavily on contextual as well as service-specific factors, for example, user characteristics, technology, implementation environment, accessibility, functionality, and performance (Funnell et al., 2022). At the same time, the concept of digital therapy raises certain ethical issues, for example, consumer privacy, the competence of therapists, or the ability of counterparts to build a therapeutic relationship.
Map** the Digital Mental Health Servicescape
In the marketing literature, the places and spaces where consumption experiences take place are commonly referred to as servicescapes (Figueiredo et al., 2021). They can also be referred to as cyberscapes (Williams & Dargel, 2004) if consumption encounters take place in the virtual environment, displaying characteristics of intangibility, perishability, the inseparability of production and consumption, and heterogeneity in delivery quality. In carefully configuring their servicescapes, businesses can use these to influence consumption experiences, to enhance brand image, to attract customers, or even to stimulate sustainable consumption by weaving ethical ideological messages into elements of the service environments (Pecoraro et al., 2021).
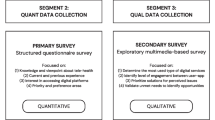
The current research project applies the theoretical value configuration space model (Blocker & Barrios, 2015), specifically its service design dimension, to the digital mental health servicescape with the purpose of systematizing, dimensionalizing and understanding the specifics of the value configuration of existing services and their value propositions. In selecting services for our investigation, we defined digital mental health as any technological application that involves mental health assessment, support, prevention, and treatment. Other inclusion criteria for these mental health apps involved the public availability of the service in question, as well as its searchability on Google Playstore. In our investigation of mental health influencers, we have searched Instagram and Facebook for public profiles, as well as online communities oriented toward general target audiences and addressing issues of mental health, mental wellbeing, or specific mental health conditions. Our exclusion criteria were as follows: that the service was not publicly available (i.e. by prescription only), not available on cellphones (i.e. web version only), private or restricted influencer profiles and online communities, a specific “niche” demographic orientation, or a primary focus on physical fitness and nutrition with no significant attention paid to psychological wellbeing.
Our interpretive analysis proceeded from descriptive coding during the first round of analysis to identifying the theoretically informed themes during the second, and theory extension during the third round. The analytical framework applied during the second round of coding and subsequently followed the value configuration space model, with a specific focus on examining: (1) the service design, or the user interface and value propositions of the selected mental health apps, (2) the human agents, or mental health influencers, and their communicative and discursive strategies, (3) the service practices, or the specific procedures, understandings and engagements needed on the part of consumers in order to interact with the service or specialist, and (4) the social structures, or the overarching value discourse surrounding the service experiences.
It’s a Wild Wild West: General Characteristics of the Digital Mental Health Servicescape
Building upon the conceptualization of service provision as “the ongoing combination of resources, through integration, and their application, driven by operant resources — the activities of actors” (Vargo & Lusch, 2011, p. 184), we can see how the elements of service design, guided by companies’ value propositions, provide resources that are further integrated (or not) by consumers during the value creation process. The first thing that strikes the unprepared consumer is the sheer number of offerings available out there. In a way, the landscape of digital mental health services resembles a metaphorical Wild Wild West movie, with multiple human, non-human and hybrid actors all competing for limited consumer attention in a crowded hypercompetitive market, where professional clinical psychologists and psychotherapists compete with energy healers and life coaches, and clinical grade psychotherapy platforms coexist alongside artificial intelligence chatbots. The global availability of digital mental health services turns the market into a deterritorialized entity, where local specifics get blurred, and where local rules and regulations do not always apply, often creating confusion when it comes to the rules governing successful resource integration by market actors.
While the clinical sector, partially represented by the local clinics providing online consultations, can partially be covered by the national insurance regulations of some countries, depending on local healthcare legislation, the non-clinical sector is largely unregulated. The multiple globally available service provider aggregator platforms, chatbot apps, and mental health influencers all enjoy quasi-complete freedom of action and access to consumers worldwide. The ease of access and the ability to change therapist in a couple of clicks replaces the traditional, prolonged, and close therapeutic relationship, built between therapist and client over time, with a more liquid consumption logic (Bardhi & Eckhardt, 2017), characterized by the flexibility, adaptability, fluidity, lightness, detachment, and speed of the uberized service experience. In the social media influence space, where the hybridization of the clinical and new age discourses can be observed in posts like “Things you’ll learn during a spiritual awakening”, it is becoming harder for a consumer to distinguish a reputable clinical practitioner from an astropsychologist, a self-taught psychotherapist, or an energy healer.
In our analysis, we have separated the digital mental health servicescape into four quadrants, based on actor involvement and intended service outcomes, the delineation of clinical service offerings, from those related to general consumer wellbeing, and we have also separated the services centering on human interaction from those powered by Artificial Intelligence. These four quadrants can best be understood as ideal types (Weber, 1949), or as analytic constructions accentuating certain aspects of the studied phenomenon, for explanatory purposes, rather than naturally given entities or a technically generated perceptual map. Figure 15.1 illustrates these four quadrants of the digital mental health servicescape using a few selected examples of the market actors involved.
The coming sections will discuss the specifics of each of these four quadrants, with the specific focus on the type of offering, the available value propositions, the monetization strategies of the service providers, and the type of engagement requested from consumers, followed by reflections on the balance between the potential advantages and potential risks, as well as ethical considerations. As this project is primarily concerned with understanding the service design elements of value-creating commercial actors in the digital mental health servicescape (Blocker & Barrios, 2015), our understanding of the value proposition leads us to focus on its proposing dimension (Rintamäki & Saarijärvi, 2021); that is, the value proposed by commercial market actors to their customers, rather than on customer perceptions of value. Specifically, we focus on the generation of the value-in-use during these service experiences, which emerges from the usage of the resources provided by the market, or even from the mental states arising during the process of consumption (Gronroos, 2011).
Self-Care Valley: AI Platforms for Consumer Wellbeing
The first quadrant of digital mental health is represented by a wide range of freemium and subscription-based wellbeing and meditation apps, and online platforms. We have also included in our analysis mainstream fitness apps with a strong mental health element (e.g. programs dedicated to mental wellbeing and guided meditations), as well as health applications integrated with wearable tech, for example, fitness watches, bracelets, and rings, with a strong focus on mental wellbeing. The peculiarity of the services provided in this quadrant is their lack of real-life human interactions with service providers—the meditation videos are pre-recorded and the recommendations are generated by a program algorithm. Some applications offer discussion boards and chats, where app users cannot interact with each other, but they do not provide direct real-time one-on-one interaction with a human mental health specialist. In this quadrant, market actors provide value-creating resources to consumers, but hold these independently responsible for successful resource integration (Vargo & Lusch, 2011) as the value-creation and wellbeing outcomes of service experiences rely on consistent, prolonged, and frequent use of these service offerings manifesting themselves as a regular and technology-facilitated meditation practice.
It is important to note that the offerings presented in this quadrant do not claim to manage clinical mental health conditions, rather they aim to generate transformative value (Blocker & Barrios, 2015) by generating an uplifting change that can improve the daily lives of their users. The value propositions of these service providers are centered around the themes of self-care, mental balance, performance optimization, and basic stress management. This gamified and self-guided user experience gives a certain flexibility to users, who can engage in liquid consumption (Bardhi & Eckhardt, 2017) by deciding where, when and how to use these apps.
The accessibility and convenience of these self-guided solutions is the obvious advantage at the forefront of the user experience. However, due to the lack of regulations regarding consumer privacy in some geographical regions, and on some platforms, the procedures for processing the demographic data of subscribed consumers remain blurry at best, and concealed at worst, raising concerns around resource misuse (Plé & Cáceres, 2010), specifically, when it comes to the use of consumer data and the potential of this being resold to third parties, for advertising purposes, especially in countries not protected by the GDPR regulation.
The Blue Pill: Clinical AI Solutions
The second quadrant, which we call the Blue Pill here, or the quick fix, is represented by a range of AI-powered clinical grade mental health applications, operating according to a freemium, subscription-based, or one-time payment model. Among these, we are able to observe the therapy chatbots, as well as the screening and diagnostic apps. The services provided in this quadrant offer relief from mild symptoms of panic, depression, and anxiety, as well as a range of mental health tests that allow consumers to self-diagnose without visiting a human mental health professional.
Unlike the everyday wellbeing solutions represented in the first quadrant, the offerings in this quadrant highlight the scientific and clinical expertise of app developers and rely on mainstream clinical methodologies, for example, variations of cognitive behavioral therapy, in their value propositions and algorithms. With this in mind, we can say that, unlike the generic wellbeing apps discussed in the previous quadrant, successful resource integration by consumers (Vargo & Lusch, 2011) is controlled to a greater degree here by commercial market actors. While these apps still operate using a self-guided user interface, they often provide AI-generated nudges and suggestions that guide the user experience, or gamify it in order to ensure the stickiness of the customer journey (Siebert et al., 2020).
An important feature present in certain chatbot apps is the ability to add an emergency contact, which can be a relative or a friend, as well as acquiring a referral to a human mental health provider. This way, while the main user experience as regards managing mild symptoms resulting from mental health conditions is AI-driven, for emergency cases and more serious symptoms, customers are redirected to clinical experts and human points of contact, represented in the fourth quadrant of the digital mental health servicescape.
The accessibility of these apps, as well as the clinical base underpinning the self-guided techniques offered in order to manage mild symptoms resulting from mental health conditions, can potentially reduce the strain on physical health services, providing customers with early-stage diagnostic and treatment solutions, and advising them when to take the next step of consulting a human expert. At the same time, just as in the first quadrant, the potential for resource misuse by market actors (Plé & Cáceres, 2010) is abundant as the rules and regulations governing consumer privacy remain unclear, and chatbots remain notoriously evasive when asked how data is being protected, referring to a corporate confidentiality policy on a developer’s website, which in turn makes reference to other guidelines or describes that confidentiality policy in very abstract terms that do not exclude reselling consumer data to third parties. In the absence of clear confirmation that consumer data is safe and protected, there is a danger of information being leaked, for example, conversation transcripts, descriptions of symptoms, demographic data and so on. The self-guided nature of these apps also opens doors to resource misuse by consumers through self-misdiagnosis, or the lack of treatment effectiveness without the guidance of human specialists.
The Happiness Market: Human Actors in Search of Wellbeing
The third quadrant—the Happiness Market—is represented by a wide array of mental health influencers, mental health experts with a social media presence, and online support communities and discussion boards. It is a notoriously deregulated space where PhDs in clinical psychology are positioned in the same marketspace as energy healers or self-taught psychology practitioners, competing for limited levels of consumer attention. In such marketspaces, successful resource integration (Vargo & Lusch, 2011), within the boundaries of a singular market system, becomes quite challenging as the happiness market provides consumers with an abundance of professional and non-professional resources that can freely be brought together in infinite combinations.
The value propositions in this space are abundant, and for the purposes of classification, we have positioned the non-clinical offerings in this segment, that is, it includes the empowerment, support, self-improvement and educational content, as well as daily guidance and advice. The monetization strategies of the mental health experts and gurus present online vary between the charging of fees for one-on-one consultations and the development of training programs, workshops and seminars, as well as the production of infotainment content, for example, writing self-help books and recording podcasts aimed at improving the daily lives of readers and listeners.
Consumer engagement in this quadrant is very active and involved, being facilitated by the interactive nature of social networks—consumers write comments, engage in discussions, and build online pool-, web- and hub-type communities (Fournier & Lee, 2009) based on shared interests, personal relationships, or on admiration for a certain influencer. The offerings present in this quadrant have a great potential for generating transformative value (Blocker & Barrios, 2015), and increasing consumer wellbeing, due to their accessibility, the ease of community building and the destigmatization of mental health issues by discussing them openly in the online space. However, the complete lack of entry barriers to market actors and the deregulated nature of the social media space raise serious ethical issues as regards controlling the qualifications and expertise of the service providers. While not necessarily leading to resource misuse (Plé & Cáceres, 2010), the hybridization of the clinical and New Age discourses in the social media space can also potentially damage the image of the psychological profession in the eyes of an unprepared consumer, a consumer who does not know, or see, the difference between online individuals claiming (whether supported by official credentials or not) to be psychologists, psychotherapists, psychiatrists, psycho-practitioners, and experts in mental health and self-improvement. The issue of limiting the harmful information and advice available online can also pose a serious challenge to legislators: This is because, in the global online space, it is often unclear where the legal jurisdiction of each country applies, and where it does not.
The Therapy Room: Online Clinical Human Interactions
The fourth quadrant of the digital mental health servicescape is represented by what we can most readily imagine as classic mental health services—online psychotherapy consultations with licensed mental health professionals, where the rules of engagement are clear and regulated, facilitating successful resource integration (Vargo & Lusch, 2011) by both consumer and service provider The range of offerings includes the online aggregator platforms, offering to connect consumers with a matching mental health specialist, telemedicine platforms, and a range of online licensed mental health practitioners, operating either independently or as part of a clinic or mental health organization.
The solutions present in this quadrant still follow the liquid consumption logic (Bardhi & Eckhardt, 2017), offering affordable and accessible therapy whenever and wherever a customer wants it, although to a lesser extent than with the completely deregulated happiness market logic of the previous quadrant. Indeed, the prices of online consultations are often much lower than those of physical consultations, opening up this type of therapy to wider populations. The one-on-one telemedicine consultations and online therapy groups accessible in this quadrant have an advantage over the consultations offered in the unregulated social media space, as the clinical expertise and competence of therapists is verified by the aggregator and telemedicine platforms, serving as market intermediaries. Some telemedicine platforms even collaborate locally with insurance providers, covering part of the consultation fees paid by consumers.
In more serious cases, this type of online therapy—the market of specialists—has a clear advantage over the other three types of solutions, as competent human therapists can deal individually with the queries of their clients. At the same time, the potential for resource misuse (Plé and Cáceres) is still present in the case of global platforms where legal responsibility and liability issues may still be unresolved, and the liquid and non-committed nature of these uberized therapeutic relationships, whereby a client can change his/her therapist in a couple of clicks, can potentially compromise the continuity of the therapy and the quality of the therapeutic relationship.
Discussion: Generating Transformative Value in Digital Mental Health
In our analysis of the four quadrants of the digital mental health servicescape, we have shown how the different value propositions and usage logics present in each quadrant play a part in the co-creation and co-destruction of transformative value in use (Blocker & Barrios, 2015; Gronroos, 2011), when the resources provided by market actors are either successfully integrated by consumers (Vargo & Lusch, 2011) or misused by either consumers or market actors, or by both (Plé & Cáceres, 2010). By viewing, in this chapter, the digital mental health servicescape as a heterogeneous service ecosystem, we go beyond viewing digital mental health services as either a combination of purely clinical offerings or a unified marketspace, showing how the variety and specifics of the digital mental health solutions available online call for a nuanced approach to service provision, rather than a unified one-size-fits-all solution. The service ecosystem of digital mental health services can be seen as an interactive online retail space, where a wide range of offerings can be matched to specific customers looking for specific types of solutions, and where digital service environments can be carefully configured to introduce consumers to certain ideological cues, thus encouraging desirable consumer behaviors (Pecoraro et al., 2021; Williams & Dargel, 2004).
So how can marketers and service providers ensure that the transformative value creation of these ecosystems is minimally inhibited by the potential risk of value destruction? Here, we conceptualize the value co-creation and co-destruction mechanisms of the digital mental health services space through the lens of resource integration and resource misuse, where the integration of resources facilitates exchanges between actors (Sklyar et al., 2019), and resource misuse leads to value co-destruction (Plé & Cáceres, 2010), and we provide the following recommendations for online digital health retailers and service experience designers willing to optimize the customer experience in the mental health services sector:
-
1.
Know your quadrant to optimize resource integration. Recognize the specifics of the service offerings provided and know which benefits should be brought to the forefront of the value proposition. The first element of resource integration (Vargo & Lusch, 2011), in this context, is the ability of service providers to highlight the advantages of the service experience, for example, the instantaneousness, accessibility and measurability of consumption outcomes. This can involve educating consumers on the specifics of engagement with a given service offering, as well as transparency regarding the credentials of app developers or human service providers. The second main element of resource integration is creating a human connection, either through direct interactions with mental health experts or through community-building strategies on AI-powered apps, for example, integrating discussion boards for consumers wishing to exchange and share their experiences with others.
-
2.
Define the rules of engagement to avoid resource misuse. The dangers of resource misuse (Plé & Cáceres, 2010) manifest themselves primarily in the dangers of unregulated servicescapes and issues related to consumer privacy. The dangers arising from the lack of regulation can potentially be mitigated by increased quality control and fine-tuning of the selection processes on service provider aggregator platforms, as well as by integrating verification mechanisms for the credentials of mental health experts offering advice in the social media space. To appease consumer concerns over the privacy of their data, service providers are advised to increase the transparency of their disclosure of the procedures related to the handling of consumer data. This can be achieved by means of reassuring consumers about the safety of their personal information in simple accessible statements and visible front and center on the app interface, instead of hiding these in the legalese jargon of corporate confidentiality policies.
-
3.
Avoid value conflict. The notion of value conflict refers to a situation when competing notions of value clash in the shared marketspace, due to multiple market actors having their own understanding of the potential value outcomes of the service experience (Minina et al., 2022), Aligning service outcomes with the dominant discourse in the respective consumption quadrant can help service providers avoid potential value conflict situations. This can take the form of delineating the discursive strategies between clinical and non-clinical offerings, as well as fine-tuning the value propositions to the specifics of the relevant consumption communities (i.e. yoga lovers, empowerment-seeking consumers, anxiety-affected individuals etc.).
By recognizing digital mental health services as an umbrella term, uniting multiple human and non-human actors with their own specifics, varying degrees of agency and different rules of engagement, online mental health service providers can fine-tune their value propositions to the specifics of their service offerings. By focusing on the respective needs of the consumers in each quadrant, and uncovering their service usage strategies, service providers will be able to design optimal customer journeys, defining specific rules of engagement with their customer counterparts. Future research is invited to focus on the in-depth investigation of the different relationship logics emerging between consumers and service providers in the digital mental health servicescape, as well as the particularities of the consumer practices that lead to transformative service outcomes. Finally, it is important to remember that, in today’s world, technology is advancing faster than regulatory space, causing important ethical and legal challenges for the policymakers and service providers who want to protect and enhance consumer wellbeing.
References
Anderson, L., & Ostrom, A. L. (2015). Transformative service research: Advancing our knowledge about service and well-being. Journal of Service Research, 18(3), 243–249.
Bardhi, F., & Eckhardt, G. M. (2017). Liquid Consumption. Journal of Consumer Research, 44(5), 599–623.
Blocker, C. P., & Barrios, A. (2015). The transformative value of a service experience. Journal of Service Research, 18(3), 265–283.
Boninsegni, M. F., Roy, A., Bakpayev, M., Kumar, S., Peronard, J.-P., & Reimer, T. (2022). Opportunities of and threats to consumer well-being in the age of fourth industrial revolution (IR 4.0) technologies. Digital Policy, Regulation and Governance, 24(1), 93–105.
Dodge, R., Daly, A. P., Huyton, J., & Sanders, L. D. (2012). The challenge of defining wellbeing. International Journal of Wellbeing, 2(3), 222–235.
European Commission. (2018). Europe’s Digital Decade: Digital targets for 2030. European Commission.
Figueiredo, B., Pico Larsen, H., & Bean, J. (2021). The cosmopolitan Servicescape. Journal of Retailing, 97(2), 267–287.
Fournier, S., & Lee, L. (2009). Getting brand communities right (pp. 105–112). Harvard Business Review.
Funnell, E. L., Spadaro, B., Martin-Key, N., Metcalfe, T., & Bahn, S. (2022). mHealth solutions for mental health screening and diagnosis: A review of app user perspectives using sentiment and thematic analysis. Frontiers in Psychiatry, 13, 857304.
Gronroos, C. (2011). Value co-creation in service logic: A critical analysis. Marketing Theory, 11(3), 279–301.
Minina, A., Masè, S., & Smith, J. (2022). Commodifying love: Value conflict in online dating. Journal of Marketing Management, 38(1–2), 98–126.
Pecoraro, M., Uusitalo, O., & Valtonen, A. (2021). Experiencing ethical retail ideology in the servicescape. Journal of Marketing Management, 37(5–6), 520–547.
Plé, L., & Cáceres, R. C. (2010). Not always co-creation: Introducing interactional co-destruction of value in service-dominant logic. Journal of Services Marketing, 24(6), 430–437.
Rintamäki, T., & Saarijärvi, H. (2021). An integrative framework for managing customer value propositions. Journal of Business Research, 134(September), 754–764.
Siebert, A., Gopaldas, A., Lindridge, A., & Simões, C. (2020). Customer experience journeys: Loyalty loops versus involvement spirals. Journal of Marketing, 84(4), 45–66.
Sklyar, A., Kowalkowski, C., Sörhammar, D., & Tronvoll, B. (2019). Resource integration through digitalisation: A service ecosystem perspective. Journal of Marketing Management, 35(11–12), 974–991.
Statista. (2022). Digital health study.
Vargo, S. L., Akaka, M. A., & Vaughan, C. M. (2017). Conceptualizing value: A service-ecosystem view. Journal of Creating Value, 3(2), 117–124.
Vargo, S. L., & Lusch, R. F. (2011). It’s all B2B…and beyond: Toward a systems perspective of the market. Industrial Marketing Management, 40(2), 181–187.
Weber, M. (1949). The methodology of the social sciences. The Free Press.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2024 The Author(s)
About this chapter
Cite this chapter
Jeunemaître, A.M. (2024). The Future of Wellbeing: Value Creation in Digital Mental Health Services. In: Bäckström, K., Egan-Wyer, C., Samsioe, E. (eds) The Future of Consumption. Palgrave Macmillan, Cham. https://doi.org/10.1007/978-3-031-33246-3_15
Download citation
DOI: https://doi.org/10.1007/978-3-031-33246-3_15
Published:
Publisher Name: Palgrave Macmillan, Cham
Print ISBN: 978-3-031-33245-6
Online ISBN: 978-3-031-33246-3
eBook Packages: Business and ManagementBusiness and Management (R0)