Abstract
Traditionally, other than its role in lymphadenectomy for neoplastic disease, the mesentery has not been the target of surgery in gastrointestinal diseases. However, increasingly the mesentery has been implicated in the pathophysiology of Crohn’s disease and possibly ulcerative colitis. In this chapter, we review the role of the mesentery in inflammation as well as the traditional surgical approaches to both malignant and benign diseases including colorectal cancer and inflammatory bowel disease. We will then review the progressive surgical approaches targeting the mesentery as a source of inflammation, including peri-pouch fat, extended mesenteric excision, and the Kono-S anastomosis. Surgical targeting of the mesentery in colorectal cancer is the current standard of care globally. However, for ulcerative colitis, additional studies are needed to assess whether mesenteric excision in the setting of ileoanal pouch construction is beneficial. Given the low rate of surgical recurrence of diverticular disease, such studies are unlikely to be undertaken. In Crohn’s disease, forthcoming studies will reveal whether novel techniques and procedures lead to reductions in postoperative disease recurrence.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Coffey JC, O’Leary DP. The mesentery: structure, function, and role in disease. Lancet Gastroenterol Hepatol. 2016;1(3):238–47.
Li Y, Zhu W, Zuo L, et al. The role of the mesentery in Crohn’s disease: the contributions of nerves, vessels, lymphatics, and fat to the pathogenesis and disease course. Inflamm Bowel Dis. 2016;22(6):1483–95.
Drouet M, Dubuquoy L, Desreumaux P, et al. Visceral fat and gut inflammation. Nutrition. 2012;28(2):113–7.
Deitch EA, Xu D, Franko L, et al. Evidence favoring the role of the gut as a cytokine-generating organ in rats subjected to hemorrhagic shock. Shock. 1994;1(2):141–5.
Suliburk J, Helmer K, Moore F, et al. The gut in systemic inflammatory response syndrome and sepsis. Enzyme systems fighting multiple organ failure. Eur Surg Res. 2008;40(2):184–9.
Weidinger C, Ziegler JF, Letizia M, et al. Adipokines and their role in intestinal inflammation. Front Immunol. 2018;9:1974.
Kredel L, Batra A, Siegmund B. Role of fat and adipokines in intestinal inflammation. Curr Opin Gastroenterol. 2014;30(6):559–65.
Rivera ED, Coffey JC, Walsh D, et al. The mesentery, systemic inflammation, and Crohn’s disease. Inflamm Bowel Dis. 2019;25(2):226–34.
Delibegovic S. Introduction to total mesorectal excision. Med Arch. 2017;71(6):434–8.
Heald RJ, Husband EM, Ryall RD. The mesorectum in rectal cancer surgery—the clue to pelvic recurrence? Br J Surg. 1982;69(10):613–6.
Quirke P, Durdey P, Dixon MF, et al. Local recurrence of rectal adenocarcinoma due to inadequate surgical resection. Histopathological study of lateral tumour spread and surgical excision. Lancet. 1986;2(8514):996–9.
Wibe A, Moller B, Norstein J, et al. A national strategic change in treatment policy for rectal cancer—implementation of total mesorectal excision as routine treatment in Norway. A national audit. Dis Colon Rectum. 2002;45(7):857–66.
MacFarlane JK, Ryall RD, Heald RJ. Mesorectal excision for rectal cancer. Lancet. 1993;341(8843):457–60.
McAnena OJ, Heald RJ, Lockhart-Mummery HE. Operative and functional results of total mesorectal excision with ultra-low anterior resection in the management of carcinoma of the lower one-third of the rectum. Surg Gynecol Obstet. 1990;170(6):517–21.
Bolognese A, Cardi M, Muttillo IA, et al. Total mesorectal excision for surgical treatment of rectal cancer. J Surg Oncol. 2000;74(1):21–3.
Martling A, Holm T, Rutqvist LE, et al. Impact of a surgical training programme on rectal cancer outcomes in Stockholm. Br J Surg. 2005;92(2):225–9.
Kapiteijn E, Putter H, van de Velde CJ, et al. Impact of the introduction and training of total mesorectal excision on recurrence and survival in rectal cancer in the Netherlands. Br J Surg. 2002;89(9):1142–9.
Adam IJ, Mohamdee MO, Martin IG, et al. Role of circumferential margin involvement in the local recurrence of rectal cancer. Lancet. 1994;344(8924):707–11.
Wibe A, Rendedal PR, Svensson E, et al. Prognostic significance of the circumferential resection margin following total mesorectal excision for rectal cancer. Br J Surg. 2002;89(3):327–34.
Quirke P, Steele R, Monson J, et al. Effect of the plane of surgery achieved on local recurrence in patients with operable rectal cancer: a prospective study using data from the MRC CR07 and NCIC-CTG CO16 randomised clinical trial. Lancet. 2009;373(9666):821–8.
van Gijn W, Marijnen CA, Nagtegaal ID, et al. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer: 12-year follow-up of the multicentre, randomised controlled TME trial. Lancet Oncol. 2011;12(6):575–82.
Hohenberger W, Weber K, Matzel K, et al. Standardized surgery for colonic cancer: complete mesocolic excision and central ligation—technical notes and outcome. Colorectal Dis. 2009;11(4):354–64; discussion 364-355.
Bertelsen CA, Neuenschwander AU, Jansen JE, et al. Disease-free survival after complete mesocolic excision compared with conventional colon cancer surgery: a retrospective, population-based study. Lancet Oncol. 2015;16(2):161–8.
De Simoni O, Barina A, Sommariva A, et al. Complete mesocolic excision versus conventional hemicolectomy in patients with right colon cancer: a systematic review and meta-analysis. Int J Colorectal Dis. 2021;36(5):881–92.
Ow ZGW, Sim W, Nistala KRY, et al. Comparing complete mesocolic excision versus conventional colectomy for colon cancer: a systematic review and meta-analysis. Eur J Surg Oncol. 2021;47(4):732–7.
Du L, Ha C. Epidemiology and pathogenesis of ulcerative colitis. Gastroenterol Clin North Am. 2020;49(4):643–54.
Dalal RS, Osterman MT, Buchner AM, et al. A user-friendly prediction tool to identify colectomy risk in patients with ulcerative colitis. Inflamm Bowel Dis. 2019;25(9):1550–8.
Kuehn F, Hodin RA. Impact of modern drug therapy on surgery: ulcerative colitis. Visc Med. 2018;34(6):426–31.
Jenkinson PW, Plevris N, Lyons M, et al. Analysis of colectomy rates for ulcerative colitis in pre-and postbiological eras in Lothian, Scotland. Colorectal Dis. 2021;23(5):1175–83.
Parragi L, Fournier N, Zeitz J, et al. Colectomy rates in ulcerative colitis are low and decreasing: 10-year follow-up data from the Swiss IBD cohort study. J Crohns Colitis. 2018;12(7):811–8.
Barnes EL, Jiang Y, Kappelman MD, et al. Decreasing colectomy rate for ulcerative colitis in the United States between 2007 and 2016: a time trend analysis. Inflamm Bowel Dis. 2020;26(8):1225–31.
Ghoz H, Kesler A, Hoogenboom SA, et al. Decreasing colectomy rates in ulcerative colitis in the past decade: improved disease control? J Gastrointest Surg. 2020;24(2):270–7.
Akiyama S, Rai V, Rubin DT. Pouchitis in inflammatory bowel disease: a review of diagnosis, prognosis, and treatment. Intest Res. 2021;19(1):1–11.
Plietz MC, Kayal M, Rizvi A, et al. Slow and steady wins the race: a solid case for a 3-stage approach in ulcerative colitis. Dis Colon Rectum. 2021;64(12):1511–20.
Spinelli A, Bonovas S, Burisch J, et al. ECCO guidelines on therapeutics in ulcerative colitis: surgical treatment. J Crohns Colitis. 2021;16(2):179–89.
Kayal M, Ungaro RC, Riggs A, et al. Ileal pouch anal anastomosis for the management of ulcerative colitis is associated with significant disability. Clin Gastroenterol Hepatol. 2021;20(4):e761–9.
Leeds IL, Sundel MH, Gabre-Kidan A, et al. Outcomes for ulcerative colitis with delayed emergency colectomy are worse when controlling for preoperative risk factors. Dis Colon Rectum. 2019;62(5):600–7.
Lightner AL, Grass F, McKenna NP, et al. Short-term postoperative outcomes following robotic versus laparoscopic ileal pouch-anal anastomosis are equivalent. Tech Coloproctol. 2019;23(3):259–66.
Chu BK, Scott FI, Bewtra M. Optimal placement of colectomy in the treatment of ulcerative colitis: a Markov model analysis. J Gastrointest Surg. 2021;25(12):3208–17.
Gu J, Stocchi L, Ashburn J, et al. Total abdominal colectomy vs. restorative total proctocolectomy as the initial approach to medically refractory ulcerative colitis. Int J Colorectal Dis. 2017;32(8):1215–22.
Lashner BA, Silverstein MD, Hanauer SB. Hazard rates for dysplasia and cancer in ulcerative colitis. Results from a surveillance program. Dig Dis Sci. 1989;34(10):1536–41.
Eaden JA, Abrams KR, Mayberry JF. The risk of colorectal cancer in ulcerative colitis: a meta-analysis. Gut. 2001;48(4):526–35.
Lennardjones JE, Melville DM, Morson BC, et al. Precancer and cancer in extensive ulcerative-colitis—findings among 401 patients over 22 years. Gut. 1990;31(7):800–6.
Rutter MD, Saunders BP, Wilkinson KH, et al. Thirty-year analysis of a colonoscopic surveillance program for neoplasia in ulcerative colitis. Gastroenterology. 2006;130(4):1030–8.
Bernstein CN, Shanahan F, Weinstein WM. Are we telling patients the truth about surveillance colonoscopy in ulcerative-colitis. Lancet. 1994;343(8889):71–4.
von Herbay A, Herfarth C, Otto HF. Cancer and dysplasia in ulcerative colitis: a histologic study of 301 surgical specimen. Z Gastroenterol. 1994;32(7):382–8.
Gorfine SR, Bauer JJ, Harris MT, et al. Dysplasia complicating chronic ulcerative colitis: is immediate colectomy warranted? Dis Colon Rectum. 2000;43(11):1575–81.
Greenstein AJ, Slater G, Heimann TM, et al. A comparison of multiple synchronous colorectal cancer in ulcerative colitis, familial polyposis coli, and de novo cancer. Ann Surg. 1986;203(2):123–8.
Kiran RP, Khoury W, Church JM, et al. Colorectal cancer complicating inflammatory bowel disease: similarities and differences between Crohn’s and ulcerative colitis based on three decades of experience. Ann Surg. 2010;252(2):330–5.
Gearhart SL, Nathan H, Pawlik TM, et al. Outcomes from IBD-associated and non-IBD-associated colorectal cancer: a surveillance epidemiology and end results Medicare study. Dis Colon Rectum. 2012;55(3):270–7.
Blackstone MO, Riddell RH, Rogers BHG, et al. Dysplasia-associated lesion or mass (Dalm) detected by colonoscopy in long-standing ulcerative-colitis—an indication for colectomy. Gastroenterology. 1981;80(2):366–74.
Kariv R, Remzi FH, Lian L, et al. Preoperative colorectal neoplasia increases risk for pouch neoplasia in patients with restorative proctocolectomy. Gastroenterology. 2010;139(3):806–12. 812 e801-802
Ziv Y, Fazio VW, Strong SA, et al. Ulcerative colitis and coexisting colorectal cancer: recurrence rate after restorative proctocolectomy. Ann Surg Oncol. 1994;1(6):512–5.
Abdalla M, Landerholm K, Andersson P, et al. Risk of rectal cancer after colectomy for patients with ulcerative colitis: a National Cohort study. Clin Gastroenterol Hepatol. 2017;15(7):1055–1060 e1052.
Derikx L, Nissen LHC, Smits LJT, et al. Risk of neoplasia after colectomy in patients with inflammatory bowel disease: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2016;14(6):798–806 e720.
Mark-Christensen A, Erichsen R, Brandsborg S, et al. Long-term risk of cancer following Ileal pouch-anal anastomosis for ulcerative colitis. J Crohns Colitis. 2018;12(1):57–62.
Lo B, Vester-Andersen MK, Vind I, et al. Changes in disease behaviour and location in patients with Crohn’s disease after seven years of follow-up: a Danish population-based inception cohort. J Crohns Colitis. 2018;12(3):265–72.
Ng SC, Shi HY, Hamidi N, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2017;390(10114):2769–78.
Torres J, Mehandru S, Colombel JF, et al. Crohn’s disease. Lancet. 2017;389(10080):1741–55.
GBDIBD. The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet Gastroenterol Hepatol. 2020;5(1):17–30.
Connelly TM, Tinsley A, Koltun WA. Inflammatory bowel disease: general conditions, approaches to medical management, and the future of surgery. In: Sea A, editor. ACS surgery principles and practice textbook. New York: Scientific American; 2014.
Park SH, Hwang SW, Ye BD, et al. Concordance regarding disease type and phenotypic characteristics among patients with familial inflammatory bowel disease. J Gastroenterol Hepatol. 2020;35(6):988–93.
Cabre E, Manosa M, Garcia-Sanchez V, et al. Phenotypic concordance in familial inflammatory bowel disease (IBD). Results of a nationwide IBD Spanish database. J Crohns Colitis. 2014;8(7):654–61.
Goligher JC. The long-term results of excisional surgery for primary and recurrent Crohn’s disease of the large intestine. Dis Colon Rectum. 1985;28(1):51–5.
Loftus EV Jr, Schoenfeld P, Sandborn WJ. The epidemiology and natural history of Crohn’s disease in population-based patient cohorts from North America: a systematic review. Aliment Pharmacol Ther. 2002;16(1):51–60.
Trnka YM, Glotzer DJ, Kasdon EJ, et al. The long-term outcome of restorative operation in Crohn’s disease: influence of location, prognostic factors and surgical guidelines. Ann Surg. 1982;196(3):345–55.
Greenstein AJ, Lachman P, Sachar DB, et al. Perforating and non-perforating indications for repeated operations in Crohn’s disease: evidence for two clinical forms. Gut. 1988;29(5):588–92.
Fichera A, Lovadina S, Rubin M, et al. Patterns and operative treatment of recurrent Crohn’s disease: a prospective longitudinal study. Surgery. 2006;140(4):649–54.
Maconi G, Colombo E, Sampietro GM, et al. CARD15 gene variants and risk of reoperation in Crohn’s disease patients. Am J Gastroenterol. 2009;104(10):2483–91.
Dittrich AE, Sutton RT, Haynes K, et al. Incidence rates for surgery in Crohn’s disease have decreased: a population-based time-trend analysis. Inflamm Bowel Dis. 2020;26(12):1909–16.
Kirsner JB. Historical origins of medical and surgical therapy of inflammatory bowel disease. Lancet. 1998;352(9136):1303–5.
Wirts CW Jr, BBV L. The incidence of regional ileitis. Am J Dig Dis. 1941;8:246–8.
Hughes CW, Baugh JH, Mologne LA, et al. A review of the late general Eisenhower’s operations: epilog to a footnote to history. Ann Surg. 1971;173(5):793–9.
Lee EC, Papaioannou N. Minimal surgery for chronic obstruction in patients with extensive or universal Crohn’s disease. Ann R Coll Surg Engl. 1982;64(4):229–33.
Sehgal RCT, Mohan H, Byrnes G, Peirce C, Coffey JC. The importance of the mesentery in emergency general surgery: ignore the mesentery at your peril. Mesentery Perit. 2018;2(4):1.
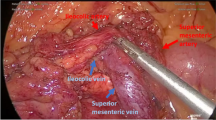
Coffey JC, Kiernan MG, Sahebally SM, et al. Inclusion of the mesentery in ileocolic resection for Crohn’s disease is associated with reduced surgical recurrence. J Crohns Colitis. 2018;12(10):1139–50.
Yamamoto T. Factors affecting recurrence after surgery for Crohn’s disease. World J Gastroenterol. 2005;11(26):3971–9.
Cristaldi M, Sampietro GM, Danelli PG, et al. Long-term results and multivariate analysis of prognostic factors in 138 consecutive patients operated on for Crohn’s disease using “bowel-sparing” techniques. Am J Surg. 2000;179(4):266–70.
Kulaylat AN, Hollenbeak CS, Sangster W, et al. Impact of smoking on the surgical outcome of Crohn’s disease: a propensity-score matched National Surgical quality improvement program analysis. Colorectal Dis. 2015;17(10):891–902.
De Dombal FT, Burton I, Goligher JC. Recurrence of Crohn’s disease after primary excisional surgery. Gut. 1971;12(7):519–27.
Goyer P, Alves A, Bretagnol F, et al. Impact of complex Crohn’s disease on the outcome of laparoscopic ileocecal resection: a comparative clinical study in 124 patients. Dis Colon Rectum. 2009;52(2):205–10.
Tan JJ, Tjandra JJ. Laparoscopic surgery for Crohn’s disease: a meta-analysis. Dis Colon Rectum. 2007;50(5):576–85.
Milsom JW, Hammerhofer KA, Bohm B, et al. Prospective, randomized trial comparing laparoscopic vs. conventional surgery for refractory ileocolic Crohn’s disease. Dis Colon Rectum. 2001;44(1):1–8; discussion 8-9.
McLeod RS, Wolff BG, Ross S, et al. Recurrence of Crohn’s disease after ileocolic resection is not affected by anastomotic type: results of a multicenter, randomized, controlled trial. Dis Colon Rectum. 2009;52(5):919–27.
Connelly TM, Messaris E. Predictors of recurrence of Crohn’s disease after ileocolectomy: a review. World J Gastroenterol. 2014;20(39):14393–406.
Stappenbeck TS, Rioux JD, Mizoguchi A, et al. Crohn disease: a current perspective on genetics, autophagy and immunity. Autophagy. 2011;7(4):355–74.
Campbell L, Ambe R, Weaver J, et al. Comparison of conventional and nonconventional strictureplasties in Crohn’s disease: a systematic review and meta-analysis. Dis Colon Rectum. 2012;55(6):714–26.
Fazio VW, Tjandra JJ. Strictureplasty for Crohn’s disease with multiple long strictures. Dis Colon Rectum. 1993;36(1):71–2.
Michelassi F, Taschieri A, Tonelli F, et al. An international, multicenter, prospective, observational study of the side-to-side isoperistaltic strictureplasty in Crohn’s disease. Dis Colon Rectum. 2007;50(3):277–84.
Seifarth C, Kreis ME, Grone J. Indications and specific surgical techniques in Crohn’s disease. Viszeralmedizin. 2015;31(4):273–9.
Michelassi F, Balestracci T, Chappell R, et al. Primary and recurrent Crohn’s disease. Experience with 1379 patients. Ann Surg. 1991;214(3):230–8. discussion 238-240
de Buck van Overstraeten A, Vermeire S, Vanbeckevoort D, et al. Modified side-to-side isoperistaltic strictureplasty over the ileocaecal valve: an alternative to ileocaecal resection in extensive terminal ileal Crohn’s disease. J Crohns Colitis. 2016;10(4):437–42.
Sasaki I, Funayama Y, Naito H, et al. Extended strictureplasty for multiple short skipped strictures of Crohn’s disease. Dis Colon Rectum. 1996;39(3):342–4.
Sampietro GM, Cristaldi M, Maconi G, et al. A prospective, longitudinal study of nonconventional strictureplasty in Crohn’s disease. J Am Coll Surg. 2004;199(1):8–20; discussion 20-22.
Gaetini A, De Simone M, Resegotti A. Our experience with strictureplasty in the surgical treatment of Crohn’s disease. Hepatogastroenterology. 1989;36(6):511–5.
Yamamoto T, Fazio VW, Tekkis PP. Safety and efficacy of strictureplasty for Crohn’s disease: a systematic review and meta-analysis. Dis Colon Rectum. 2007;50(11):1968–86.
Sehgal R, Coffey JC. Historical development of mesenteric anatomy provides a universally applicable anatomic paradigm for complete/total mesocolic excision. Gastroenterol Rep (Oxf). 2014;2(4):245–50.
Dinnick T. The origins and evolution of colostomy. Br J Surg. 1934;22:142–54.
Treves F. Lectures on the anatomy of the intestinal canal and peritoneum in man. Br Med J. 1885;1(1264):580–3.
Coffey JC. Surgical anatomy and anatomic surgery—clinical and scientific mutualism. Surgeon. 2013;11(4):177–82.
Coffey JC, Sehgal R, Walsh D. Mesenteric principles of gastrointestinal surgery: basic and applied science. 1st ed. Boca Raton: CRC; 2017. https://doi.org/10.1201/9781315381565.
Gray’s anatomy. The anatomical basis of clinical practice. 41st ed. London: Elsevier
Tursi A, Papa A, Danese S. Review article: the pathophysiology and medical management of diverticulosis and diverticular disease of the colon. Aliment Pharmacol Ther. 2015;42(6):664–84.
Connelly TM, Berg AS, Hegarty JP, et al. The TNFSF15 gene single nucleotide polymorphism rs7848647 is associated with surgical diverticulitis. Ann Surg. 2014;259(6):1132–7.
Strate LL, Morris AM. Epidemiology, pathophysiology, and treatment of diverticulitis. Gastroenterology. 2019;156(5):1282–1298 e1281.
Jeong JH, Lee HL, Kim JO, et al. Correlation between complicated diverticulitis and visceral fat. J Korean Med Sci. 2011;26(10):1339–43.
Murray KA, Hoad CL, Garratt J, et al. A pilot study of visceral fat and its association with adipokines, stool calprotectin and symptoms in patients with diverticulosis. PLoS One. 2019;14(5):e0216528.
Meyer J, Orci LA, Combescure C, et al. Risk of colorectal cancer in patients with acute diverticulitis: a systematic review and meta-analysis of observational studies. Clin Gastroenterol Hepatol. 2019;17(8):1448–1456e1417.
Phillips EH, Franklin M, Carroll BJ, et al. Laparoscopic colectomy. Ann Surg. 1992;216(6):703–7.
Bokey EL, Chapuis PH, Pheils MT. Elective resection for diverticular disease and carcinoma. Comparison of postoperative morbidity and mortality. Dis Colon Rectum. 1981;24(3):181–2.
Sher ME, Agachan F, Bortul M, et al. Laparoscopic surgery for diverticulitis. Surg Endosc. 1997;11(3):264–7.
Hall J, Hardiman K, Lee S, et al. The American Society of Colon and Rectal Surgeons clinical practice guidelines for the treatment of left-sided colonic diverticulitis. Dis Colon Rectum. 2020;63(6):728–47.
Vargas HD, Ramirez RT, Hoffman GC, et al. Defining the role of laparoscopic-assisted sigmoid colectomy for diverticulitis. Dis Colon Rectum. 2000;43(12):1726–31.
Longchamp G, Abbassi Z, Meyer J, et al. Surgical resection does not avoid the risk of diverticulitis recurrence—a systematic review of risk factors. Int J Colorectal Dis. 2021;36(2):227–37.
Haak BW, Bodewitz ST, Kuijper CF, et al. Intestinal malrotation and volvulus in adult life. Int J Surg Case Rep. 2014;5(5):259–61.
Akinkuotu A, Samuel JC, Msiska N, et al. The role of the anatomy of the sigmoid colon in develo** sigmoid volvulus: a case-control study. Clin Anat. 2011;24(5):634–7.
Cirocchi R, Farinella E, La Mura F, et al. The sigmoid volvulus: surgical timing and mortality for different clinical types. World J Emerg Surg. 2010;5:1.
Arung W, Meurisse M, Detry O. Pathophysiology and prevention of postoperative peritoneal adhesions. World J Gastroenterol. 2011;17(41):4545–53.
Shen B. Problems after restorative proctocolectomy: assessment and therapy. Curr Opin Gastroenterol. 2016;32(1):49–54.
Shen B, Achkar JP, Connor JT, et al. Modified pouchitis disease activity index: a simplified approach to the diagnosis of pouchitis. Dis Colon Rectum. 2003;46(6):748–53.
Gao XH, Li JQ, Khan F, et al. Difference in the frequency of pouchitis between ulcerative colitis and familial adenomatous polyposis: is the explanation in peripouch fat? Colorectal Dis. 2019;21(9):1032–44.
Rabbenou W, Chang S. Medical treatment of pouchitis: a guide for the clinician. Therap Adv Gastroenterol. 2021;14:17562848211023376.
Brown JJ, Balfe DM, Heiken JP, et al. Ileal J pouch: radiologic evaluation in patients with and without postoperative infectious complications. Radiology. 1990;174(1):115–20.
Harper JW, Zisman TL. Interaction of obesity and inflammatory bowel disease. World J Gastroenterol. 2016;22(35):7868–81.
Wu XR, Zhu H, Kiran RP, et al. Excessive weight gain is associated with an increased risk for pouch failure in patients with restorative proctocolectomy. Inflamm Bowel Dis. 2013;19(10):2173–81.
Gao XH, Chouhan H, Liu GL, et al. Peripouch fat area measured on MRI image and its association with adverse pouch outcomes. Inflamm Bowel Dis. 2018;24(4):806–17.
Karrasch T, Schaeffler A. Adipokines and the role of visceral adipose tissue in inflammatory bowel disease. Ann Gastroenterol. 2016;29(4):424–38.
Gore RM, Marn CS, Kirby DF, et al. CT findings in ulcerative, granulomatous, and indeterminate colitis. AJR Am J Roentgenol. 1984;143(2):279–84.
Gao XH, Yu GY, Khan F, et al. Greater peripouch fat area on CT image is associated with chronic pouchitis and pouch failure in inflammatory bowel diseases patients. Dig Dis Sci. 2020;65(12):3660–71.
Nally DM, Kavanagh DO, Winter DC. Close rectal dissection in benign diseases of the rectum: a review. Surgeon. 2019;17(2):119–26.
Rink AD, Radinski I, Vestweber KH. Does mesorectal preservation protect the ileoanal anastomosis after restorative proctocolectomy? J Gastrointest Surg. 2009;13(1):120–8.
Hicks CW, Hodin RA, Savitt L, et al. Does intramesorectal proctectomy with rectal eversion affect postoperative complications compared to standard total mesorectal excision in patients with ulcerative colitis? J Gastrointest Surg. 2014;18(2):385–90.
Hicks CW, Hodin RA, Savitt L, et al. Does intramesorectal excision for ulcerative colitis impact bowel and sexual function when compared with total mesorectal excision? Am J Surg. 2014;208(4):499–504 e494.
de Groof EJ, van der Meer JHM, Tanis PJ, et al. Persistent mesorectal inflammatory activity is associated with complications after proctectomy in Crohn’s disease. J Crohns Colitis. 2019;13(3):285–93.
D'Hoore A. Persistent mesorectal inflammatory activity is associated with complications after proctectomy in Crohn’s disease: immediate surgical implications! J Crohns Colitis. 2019;13(3):271–2.
Byrnes KG, Walsh D, Lewton-Brain P, et al. Anatomy of the mesentery: historical development and recent advances. Semin Cell Dev Biol. 2019;92:4–11.
Byrnes KG, Walsh D, Dockery P, et al. Anatomy of the mesentery: current understanding and mechanisms of attachment. Semin Cell Dev Biol. 2019;92:12–7.
Coffey JC, O'Leary DP. Defining the mesentery as an organ and what this means for understanding its roles in digestive disorders. Expert Rev Gastroenterol Hepatol. 2017;11(8):703–5.
Coffey JC, Walsh D, Byrnes KG, et al. Mesentery—a ‘New’ organ. Emerg Top Life Sci. 2020;4(2):191–206.
Kiernan MG, Coffey JC, McDermott K, et al. The human mesenteric lymph node microbiome differentiates between Crohn’s disease and ulcerative colitis. J Crohns Colitis. 2019;13(1):58–66.
Mao R, Kurada S, Gordon IO, et al. The mesenteric fat and intestinal muscle Interface: cree** fat influencing stricture formation in Crohn’s disease. Inflamm Bowel Dis. 2019;25(3):421–6.
Coffey JC, O'Leary DP, Kiernan MG, et al. The mesentery in Crohn’s disease: friend or foe? Curr Opin Gastroenterol. 2016;32(4):267–73.
Keller DS, Joshi HM, Rodriguez-Justo M, et al. Using fluorescence lymphangiography to define the ileocolic mesentery: proof of concept for the watershed area using real-time imaging. Tech Coloproctol. 2017;21(9):757–60.
Li XH, Feng ST, Cao QH, et al. Degree of cree** fat assessed by computed tomography enterography is associated with intestinal fibrotic stricture in patients with Crohn’s disease: a potentially novel mesenteric cree** fat index. J Crohns Colitis. 2021;15(7):1161–73.
Mohan HM, Coffey JC. Surgical treatment of intestinal stricture in inflammatory bowel disease. J Dig Dis. 2020;21(6):355–9.
Li Y, Zhu W, Gong J, et al. Visceral fat area is associated with a high risk for early postoperative recurrence in Crohn’s disease. Colorectal Dis. 2015;17(3):225–34.
Heald RJ, Ryall RD. Recurrence and survival after total mesorectal excision for rectal cancer. Lancet. 1986;1(8496):1479–82.
Buskens CJ, Bemelman WA. Inclusion of the mesentery in ileocolic resection for Crohn’s disease is associated with reduced surgical recurrence: editorial by Coffey et al. J Crohns Colitis. 2018;12(10):1137–8.
Caprino P, Sacchett F, Sofo L. A warning about the role of extended mesenteric excision in Crohn’s disease recurrence. J Crohns Colitis. 2019;13(12):1583.
Fleming C, Mohan H, Coffey JC. Should we resect the mesentery in ileocolic Crohn’s disease? A response to ‘a warning about the role of extended mesenteric resection in Crohn’s disease recurrence’. J Crohns Colitis. 2019;13(12):1584.
Katsuno H, Maeda K, Hanai T, et al. Novel antimesenteric functional end-to-end handsewn (Kono-S) anastomoses for Crohn’s disease: a report of surgical procedure and short-term outcomes. Dig Surg. 2015;32(1):39–44.
Meima-van Praag EM, Buskens CJ, Hompes R, et al. Surgical management of Crohn’s disease: a state of the art review. Int J Colorectal Dis. 2021;36(6):1133–45.
Luglio G, Rispo A, Imperatore N, et al. Surgical prevention of anastomotic recurrence by excluding mesentery in Crohn’s disease: the SuPREMe-CD study—a randomized clinical trial. Ann Surg. 2020;272(2):210–7.
Fichera A, Zoccali M, Kono T. Antimesenteric functional end-to-end handsewn (Kono-S) anastomosis. J Gastrointest Surg. 2012;16(7):1412–6.
Kono T, Ashida T, Ebisawa Y, et al. A new antimesenteric functional end-to-end handsewn anastomosis: surgical prevention of anastomotic recurrence in Crohn’s disease. Dis Colon Rectum. 2011;54(5):586–92.
Maguire LH, Alavi K, Sudan R, et al. Surgical considerations in the treatment of small bowel Crohn’s disease. J Gastrointest Surg. 2017;21(2):398–411.
Alshantti A, Hind D, Hancock L, et al. The role of Kono-S anastomosis and mesenteric resection in reducing recurrence after surgery for Crohn’s disease: a systematic review. Colorectal Dis. 2021;23(1):7–17.
Click B, Merchea A, Colibaseanu DT, et al. Ileocolic resection for Crohn disease: the influence of different surgical techniques on perioperative outcomes, recurrence rates, and endoscopic surveillance. Inflamm Bowel Dis. 2021;28(2):289–98.
Kono T, Fichera A, Maeda K, et al. Kono-S anastomosis for surgical prophylaxis of anastomotic recurrence in Crohn’s disease: an international multicenter study. J Gastrointest Surg. 2016;20(4):783–90.
Fornaro R, Caristo G, Stratta E, et al. Crohn’s disease and postoperative recurrence. The role of anastomotic configurations and the kono-S anastomosis. Ann Ital Chir. 2019;90:111–20.
Kono T, Fichera A. Surgical treatment for Crohn’s disease: a role of Kono-S anastomosis in the west. Clin Colon Rectal Surg. 2020;33(6):335–43.
Kono T, Fichera A. Kono-S anastomosis for Crohn’s disease: narrative—a video vignette. Colorectal Dis. 2014;16(10):833.
Peltrini R, Greco PA, Manfreda A, et al. Kono-S anastomosis after intestinal resection for Crohn’s disease. Updates Surg. 2020;72(2):335–40.
Ng CH, Chin YH, Lin SY, et al. Kono-S anastomosis for Crohn’s disease: a systemic review, meta-analysis, and meta-regression. Surg Today. 2021;51(4):493–501.
Horisberger K, Birrer DL, Rickenbacher A, et al. Experiences with the Kono-S anastomosis in Crohn’s disease of the terminal ileum—a cohort study. Langenbecks Arch Surg. 2021;406(4):1173–80.
Luglio G, Tropeano FP, Amendola A, et al. Preventing recurrence in Crohn’s disease: the Kono-S anastomosis with two-layer technique. Tech Coloproctol. 2020;24(11):1213–4.
Cavallaro P, Goldstone R, Ricciardi R, et al. Robotic intracorporeal Kono-S anastomosis—a video vignette. Colorectal Dis. 2021;23(6):1597.
Holubar SD, Gunter RL, Click BH, et al. Mesenteric excision and exclusion for ileocolic Crohn’s disease: feasibility and safety of an innovative, combined surgical approach with extended mesenteric excision and Kono-S anastomosis. Dis Colon Rectum. 2022;65(1):e5–e13.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Ethics declarations
The authors declare no conflicts of interest.
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Choi, S., Prien, C., Connelly, T., Holubar, S.D. (2023). Targeting the Mesentery with Surgery. In: Coffey, J.C. (eds) The Mesentery and Inflammation . Progress in Inflammation Research, vol 90. Springer, Cham. https://doi.org/10.1007/978-3-031-17774-3_11
Download citation
DOI: https://doi.org/10.1007/978-3-031-17774-3_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-17773-6
Online ISBN: 978-3-031-17774-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)