Abstract
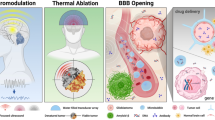
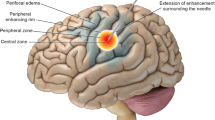
Neurosurgeons can use several high precision technologies to create lesions in the central nervous system for the treatment of functional disorders. These include radiofrequency ablation (RFA), laser interstitial thermal therapy (LITT), and high-intensity focused ultrasound (HIFU). While all of these methods use thermal energy to create permanent tissue damage, each has a unique profile of indications, risks, and advantages related to how the energy is deployed and how it interacts with biological structures. In this chapter, we discuss the historical development, mechanism of action, and current indications for each modality, including future directions for clinical and research development.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Kirschner M. Elektrocoagulation des ganglion gasseri. Zentralbl Chir. 1932;(47):2841–3.
Guridi J, Lozano AM. A brief history of pallidotomy. Neurosurgery. 1997;41(5):1169–80; discussion 80–3.
Spiegel EA, Wycis HT. Ansotomy in paralysis agitans. AMA Arch Neurol Psychiatry. 1954;71(5):598–614.
Narabayashi H, Nagao T, Saito Y, Yoshida M, Nagahata M. Stereotaxic amygdalotomy for behavior disorders. Arch Neurol. 1963;9:1–16.
Marossero F, Ravagnati L, Sironi VA, Miserocchi G, Franzini A, Ettorre G, et al. Late results of stereotactic radiofrequency lesions in epilepsy. Acta Neurochir Suppl. 1980;30:145–9.
Patil AA, Andrews R, Torkelson R. Stereotactic volumetric radiofrequency lesioning of intracranial structures for control of intractable seizures. Stereotact Funct Neurosurg. 1995;64(3):123–33.
Parrent AG, Blume WT. Stereotactic amygdalohippocampotomy for the treatment of medial temporal lobe epilepsy. Epilepsia. 1999;40(10):1408–16.
Lozano CS, Tam J, Lozano AM. The changing landscape of surgery for Parkinson’s disease. Mov Disord. 2018;33(1):36–47.
Laitinen LV, Bergenheim AT, Hariz MI. Leksell’s posteroventral pallidotomy in the treatment of Parkinson’s disease. J Neurosurg. 1992;76(1):53–61.
Webb H, Lubner MG, Hinshaw JL. Thermal ablation. Semin Roentgenol. 2011;46:133–41.
Liscak R, Malikova H, Kalina M, Vojtech Z, Prochazka T, Marusic P, et al. Stereotactic radiofrequency amygdalohippocampectomy in the treatment of mesial temporal lobe epilepsy. Acta Neurochir. 2010;152(8):1291–8.
Voges J, Buntjen L, Schmitt FC. Radiofrequency-thermoablation: general principle, historical overview and modern applications for epilepsy. Epilepsy Res. 2018;142:113–6.
Hirabayashi H, Hariz MI, Wardell K, Blomstedt P. Impact of parameters of radiofrequency coagulation on volume of stereotactic lesion in pallidotomy and thalamotomy. Stereotact Funct Neurosurg. 2012;90(5):307–15.
Catenoix H, Bourdillon P, Guenot M, Isnard J. The combination of stereo-EEG and radiofrequency ablation. Epilepsy Res. 2018;142:117–20.
Kramska L, Vojtech Z, Lukavsky J, Stara M, Malikova H. Five-year neuropsychological outcome after stereotactic radiofrequency amygdalohippocampectomy for mesial temporal lobe epilepsy: longitudinal study. Stereotact Funct Neurosurg. 2017;95(3):149–57.
Homma J, Kameyama S, Masuda H, Ueno T, Fujimoto A, Oishi M, et al. Stereotactic radiofrequency thermocoagulation for hypothalamic hamartoma with intractable gelastic seizures. Epilepsy Res. 2007;76(1):15–21.
Kameyama S, Shirozu H, Masuda H, Ito Y, Sonoda M, Akazawa K. MRI-guided stereotactic radiofrequency thermocoagulation for 100 hypothalamic hamartomas. J Neurosurg. 2016;124(5):1503–12.
Tandon V, Chandra PS, Doddamani RS, Subianto H, Bajaj J, Garg A, et al. Stereotactic radiofrequency thermocoagulation of hypothalamic hamartoma using robotic guidance (ROSA) coregistered with O-arm guidance-preliminary technical note. World Neurosurg. 2018;112:267–74.
Wei PH, An Y, Fan XT, Wang YH, Yang YF, Ren LK, et al. Stereoelectroencephalography-guided radiofrequency thermocoagulation for hypothalamic hamartomas: preliminary evidence. World Neurosurg. 2018;114:e1073–e8.
Perez-Suarez J, Torres Diaz CV, Lopez Manzanares L, Navas Garcia M, Pastor J, Barrio Fernandez P, et al. Radiofrequency lesions through deep brain stimulation electrodes in movement disorders: case report and review of the literature. Stereotact Funct Neurosurg. 2017;95(3):137–41.
Bown SG. Phototherapy in tumors. World J Surg. 1983;7(6):700–9.
Ascher PW, Justich E, Schrottner O. A new surgical but less invasive treatment of central brain tumours preliminary report. Acta Neurochir Suppl. 1991;52:78–80.
Stafford RJ, Fuentes D, Elliott AA, Weinberg JS, Ahrar K. Laser-induced thermal therapy for tumor ablation. Crit Rev Biomed Eng. 2010;38(1):79–100.
De Poorter J. Noninvasive MRI thermometry with the proton resonance frequency method: study of susceptibility effects. Magn Reson Med. 1995;34(3):359–67.
Kang JY, Sperling MR. Magnetic resonance imaging-guided laser interstitial thermal therapy for treatment of drug-resistant epilepsy. Neurotherapeutics. 2017;14(1):176–81.
Du VX, Gandhi SV, Rekate HL, Mehta AD. Laser interstitial thermal therapy: a first line treatment for seizures due to hypothalamic hamartoma? Epilepsia. 2017;58(Suppl 2):77–84.
Missios S, Bekelis K, Barnett GH. Renaissance of laser interstitial thermal ablation. Neurosurg Focus. 2015;38(3):E13.
Norred SE, Johnson JA. Magnetic resonance-guided laser induced thermal therapy for glioblastoma multiforme: a review. Biomed Res Int. 2014;2014:761312.
Carpentier A, McNichols RJ, Stafford RJ, Itzcovitz J, Guichard JP, Reizine D, et al. Real-time magnetic resonance-guided laser thermal therapy for focal metastatic brain tumors. Neurosurgery. 2008;63(1 Suppl 1):ONS21–8; discussion ONS8–9.
Schwarzmaier HJ, Eickmeyer F, von Tempelhoff W, Fiedler VU, Niehoff H, Ulrich SD, et al. MR-guided laser-induced interstitial thermotherapy of recurrent glioblastoma multiforme: preliminary results in 16 patients. Eur J Radiol. 2006;59(2):208–15.
Rahmathulla G, Recinos PF, Kamian K, Mohammadi AM, Ahluwalia MS, Barnett GH. MRI-guided laser interstitial thermal therapy in neuro-oncology: a review of its current clinical applications. Oncology. 2014;87(2):67–82.
Bezchlibnyk YB, Willie JT, Gross RE. A neurosurgeon’s view: laser interstitial thermal therapy of mesial temporal lobe structures. Epilepsy Res. 2018;142:135–9.
Southwell DG, Birk HS, Larson PS, Starr PA, Sugrue LP, Auguste KI. Laser ablative therapy of sessile hypothalamic hamartomas in children using interventional MRI: report of 5 cases. J Neurosurg Pediatr. 2018;21(5):460–5.
Wilfong AA, Curry DJ. Hypothalamic hamartomas: optimal approach to clinical evaluation and diagnosis. Epilepsia. 2013;54(Suppl 9):109–14.
Ho AL, Miller KJ, Cartmell S, Inoyama K, Fisher RS, Halpern CH. Stereotactic laser ablation of the splenium for intractable epilepsy. Epilepsy Behav Case Rep. 2016;5:23–6.
Drane DL, Loring DW, Voets NL, Price M, Ojemann JG, Willie JT, et al. Better object recognition and naming outcome with MRI-guided stereotactic laser amygdalohippocampotomy for temporal lobe epilepsy. Epilepsia. 2015;56(1):101–13.
Ellis JA, Mejia Munne JC, Wang SH, McBrian DK, Akman CI, Feldstein NA, et al. Staged laser interstitial thermal therapy and topectomy for complete obliteration of complex focal cortical dysplasias. J Clin Neurosci. 2016;31:224–8.
Curie PJ, Curie J. Crystal physics: development by pressure of polar electricity in hemihedral crystals with inclined faces. C R Hebd Seances Acad Sci. 1880;91(291).
Fry WJ, Fry FJ. Fundamental neurological research and human neurosurgery using intense ultrasound. IRE Trans Med Electron. 1960;Me-7:166–81.
Harary M, Segar DJ, Huang KT, Tafel IJ, Valdes PA, Cosgrove GR. Focused ultrasound in neurosurgery: a historical perspective. Neurosurg Focus. 2018;44(2):E2.
Hynynen K, Jolesz FA. Demonstration of potential noninvasive ultrasound brain therapy through an intact skull. Ultrasound Med Biol. 1998;24(2):275–83.
Damianou C, Hynynen K. The effect of various physical parameters on the size and shape of necrosed tissue volume during ultrasound surgery. J Acoust Soc Am. 1994;95(3):1641–9.
McDannold N, Clement GT, Black P, Jolesz F, Hynynen K. Transcranial magnetic resonance imaging- guided focused ultrasound surgery of brain tumors: initial findings in 3 patients. Neurosurgery. 2010;66(2):323–32; discussion 32.
Tempany CM, McDannold NJ, Hynynen K, Jolesz FA. Focused ultrasound surgery in oncology: overview and principles. Radiology. 2011;259(1):39–56.
Lynn JG, Zwemer RL, Chick AJ, Miller AE. A new method for the generation and use of focused ultrasound in experimental biology. J Gen Physiol. 1942;26(2):179–93.
Mohammed N, Patra D, Nanda A. A meta-analysis of outcomes and complications of magnetic resonance-guided focused ultrasound in the treatment of essential tremor. Neurosurg Focus. 2018;44(2):E4.
Chang WS, Jung HH, Zadicario E, Rachmilevitch I, Tlusty T, Vitek S, et al. Factors associated with successful magnetic resonance-guided focused ultrasound treatment: efficiency of acoustic energy delivery through the skull. J Neurosurg. 2016;124(2):411–6.
Wang TR, Bond AE, Dallapiazza RF, Blanke A, Tilden D, Huerta TE, et al. Transcranial magnetic resonance imaging-guided focused ultrasound thalamotomy for tremor: technical note. Neurosurg Focus. 2018;44(2):E3.
Zaaroor M, Sinai A, Goldsher D, Eran A, Nassar M, Schlesinger I. Magnetic resonance-guided focused ultrasound thalamotomy for tremor: a report of 30 Parkinson’s disease and essential tremor cases. J Neurosurg. 2018;128(1):202–10.
Iacopino DG, Gagliardo C, Giugno A, Giammalva GR, Napoli A, Maugeri R, et al. Preliminary experience with a transcranial magnetic resonance-guided focused ultrasound surgery system integrated with a 1.5-T MRI unit in a series of patients with essential tremor and Parkinson’s disease. Neurosurg Focus. 2018;44(2):E7.
Ram Z, Cohen ZR, Harnof S, Tal S, Faibel M, Nass D, et al. Magnetic resonance imaging-guided, high-intensity focused ultrasound for brain tumor therapy. Neurosurgery. 2006;59(5):949–55; discussion 55–6.
Hynynen K, McDannold N, Vykhodtseva N, Jolesz FA. Noninvasive MR imaging-guided focal opening of the blood-brain barrier in rabbits. Radiology. 2001;220(3):640–6.
Tsivgoulis G, Eggers J, Ribo M, Perren F, Saqqur M, Rubiera M, et al. Safety and efficacy of ultrasound-enhanced thrombolysis: a comprehensive review and meta-analysis of randomized and nonrandomized studies. Stroke. 2010;41(2):280–7.
Monteith SJ, Kassell NF, Goren O, Harnof S. Transcranial MR-guided focused ultrasound sonothrombolysis in the treatment of intracerebral hemorrhage. Neurosurg Focus. 2013;34(5):E14.
Foley JL, Eames M, Snell J, Hananel A, Kassell N, Aubry JF. Image-guided focused ultrasound: state of the technology and the challenges that lie ahead. Imaging Med. 2013;5(4):357–70.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Bhansali, A.P., Gwinn, R.P. (2020). Ablation: Radiofrequency, Laser, and HIFU. In: Pouratian, N., Sheth, S. (eds) Stereotactic and Functional Neurosurgery. Springer, Cham. https://doi.org/10.1007/978-3-030-34906-6_16
Download citation
DOI: https://doi.org/10.1007/978-3-030-34906-6_16
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-34905-9
Online ISBN: 978-3-030-34906-6
eBook Packages: MedicineMedicine (R0)