Abstract
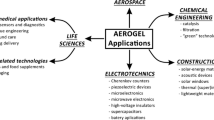
This section highlights the biocompatibility of aerogels and some of the biomedical applications associated with aerogels. Research has shown that certain aerogel formulations are compatible with the cardiovascular system, so these formulations and possibly others can be potentially used for cardiovascular implantable devices. Aerogels can also be used as bone grafts and dental implants. Multiple studies have provided proof that drugs/proteins can be loaded or embedded within aerogels and that they can maintain their functionality and be released in a controllable manner; therefore aerogels can be used in drug delivery systems. Many have also suggested that aerogels can be used in tissue engineering as scaffolding materials, as aerogels can be made biocompatible, biodegradable, and have high porosity, large surface area, and proper surface chemistry to support cell attachment and proliferation. Furthermore, as a strong and highly porous material, aerogels can have proper acoustic and ultrasonic properties to be used for ultrasound imaging. With the improvements in aerogel processing along with a better understanding of biomaterials, the biomedical applications of aerogels are expanding. Aerogels will play a significant role in the biomaterials field in the future.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Lysaght, M.J., O’Loughlin, J.A.: Demographic scope and economic magnitude of contemporary organ replacement therapies. ASAIO J. 46, 515–521 (2000)
Implantable Medical Devices Market: Global Industry Analysis, Size, Share, Growth, Trends, and Forecast 2016–2024. (2016). http://www.prnewswire.com/news-releases/implantable-medical-devices-market-global-industry-analysis-size-share-growth-trends-and-forecast-2016%2D%2D-2024-300348850.html. Accessed 31 May 2017
Pierre, A.C., Pajonk, G.M.: Chemistry of aerogels and their applications. Chem. Rev. 102, 4243–4265 (2002)
Maleki, H., Durães, L., García-González, C.A., del Gaudio, P., Portugal, A., Mahmoudi, M.: Synthesis and biomedical applications of aerogels: possibilities and challenges. Adv. Colloid Interf. Sci. 236, 1–27 (2016). https://doi.org/10.1016/j.cis.2016.05.011
Arboleda, J.C., Hughes, M., Lucia, L.A., Laine, J., Ekman, K., Rojas, O.J.: Soy protein-nanocellulose composite aerogels. Cellulose. 20, 2417–2426 (2013)
Betz, M., Garcia-Gonzalez, C.A., Subrahmanyam, R.P., Smirnova, I., Kulozik, U.: Preparation of novel whey protein-based aerogels as drug carriers for life science applications. J. Supercrit. Fluid. 72, 111–119 (2012)
Mallepally, R.R., Marin, M.A., Surampudi, V., Subia, B., Rao, R.R., Kundu, S.C., McHugh, M.A.: Silk fibroin aerogels: potential scaffolds for tissue engineering applications. Biomed. Mater. 10, 035002 (2015). https://doi.org/10.1088/1748-6041/10/3/035002
Andrade, J.D., Hlady, V.: Protein adsorption and materials biocompatibility – a tutorial review and suggested hypotheses. Adv. Polym. Sci. 79, 1–63 (1986)
Jones, M.I., McColl, I.R., Grant, D.M., Parker, K.G., Parker, T.L.: Protein adsorption and platelet attachment and activation, on TiN, TiC, and DLC coatings on titanium for cardiovascular applications. J. Biomed. Mater. Res. 52, 413–421 (2000). https://doi.org/10.1002/1097-4636(200011)52:2<413::AID-JBM23>3.0.CO;2-U
Wu, Y., Meyerhoff, M.E.: Nitric oxide-releasing/generating polymers for the development of implantable chemical sensors with enhanced biocompatibility. Talanta. 75, 642–650 (2008). https://doi.org/10.1016/j.talanta.2007.06.022
Burd, J., Noetzel, V., Tamerius, J.: Rapid testing of biomaterials for complement activation using in vitro complement immunoassays. In: Paper Presented at the 19th Annual Meeting of the Society of Biomaterials, Birmingham, Alabama (1993)
Friedewald, V.E., Bonow, R.O., Borer, J.S., Carabello, B.A., Kleine, P.P., Akins, C.W., Roberts, W.C.: The editor’s roundtable: cardiac valve surgery. Am. J. Cardiol. 99, 1269–1278 (2007). https://doi.org/10.1016/j.amjcard.2007.02.040
Yacoub, M.H., Takkenberg, J.J.: Will heart valve tissue engineering change the world? Nat. Clin. Pract. Cardiovasc. Med. 2, 60–61 (2005). https://doi.org/10.1038/ncpcardio0112
Bezuidenhout, D., Williams, D.F., Zilla, P.: Polymeric heart valves for surgical implantation, catheter-based technologies and heart assist devices. Biomaterials. 36, 6–25 (2015). https://doi.org/10.1016/j.biomaterials.2014.09.013
Maines, B.H., Brennen, C.E.: Lumped parameter model for computing the minimum pressure during mechanical heart valve closure. J. Biomech. Eng. 127, 648–655 (2005)
Bang, A., Sadekar, A.G., Buback, C., Curtin, B., Acar, S., Kolasinac, D., Yin, W., Rubenstein, D.A., Lu, H.B., Leventis, N., Sotiriou-Leventis, C.: Evaluation of Dysprosia aerogels as drug delivery systems: a comparative study with random and ordered mesoporous silicas. ACS Appl. Mater. Interfaces. 6, 4891–4902 (2014)
Rubenstein, D.A., Lu, H.B., Mahadik, S.S., Leventis, N., Yin, W.: Characterization of the physical properties and biocompatibility of polybenzoxazine-based aerogels for use as a novel hard-tissue scaffold. J. Biomater. Sci. Polym. Ed. 23, 1171–1184 (2012)
Yin, W., Lu, H.B., Leventis, N., Rubenstein, D.A.: Characterization of the biocompatibility and mechanical properties of polyurea organic aerogels with the vascular system: potential as a blood implantable material. Int. J. Polym. Mater. 62, 109–118 (2013)
Yin, W., Venkitachalam, S.M., Jarrett, E., Staggs, S., Leventis, N., Lu, H.B., Rubenstein, D.A.: Biocompatibility of surfactant-templated polyurea-nanoencapsulated macroporous silica aerogels with plasma platelets and endothelial cells. J. Biomed. Mater. Res. A. 92a, 1431–1439 (2010)
Leventis, N., Mulik, S., Wang, X.J., Dass, A., Patil, V.U., Sotiriou-Leventis, C., Lu, H.B., Chum, G., Capecelatro, A.: Polymer nano-encapsulation of templated mesoporous silica monoliths with improved mechanical properties. J. Non-Cryst. Solids. 354, 632–644 (2008)
Ayers, M.R., Hunt, A.J.: Synthesis and properties of chitosan–silica hybrid aerogels. J. Non-Cryst. Solids. 285, 123–127 (2001). https://doi.org/10.1016/S0022-3093(01)00442-2
Taghvaee, T., Donthula, S., Rewatkar, P.M., Majedi Far, H., Sotiriou-Leventis, C., Leventis, N.: K-index: a descriptor, predictor, and correlator of complex nanomorphology to other material properties. ACS Nano. 13, 3677–3690 (2019). https://doi.org/10.1021/acsnano.9b00396
Mellado, C., Figueroa, T., Báez, R., Castillo, R., Melendrez, M., Schulz, B., Fernández, K.: Development of graphene oxide composite aerogel with proanthocyanidins with hemostatic properties as a delivery system. ACS Appl. Mater. Interfaces. 10, 7717–7729 (2018). https://doi.org/10.1021/acsami.7b16084
Gavillon, R., Budtova, T.: Aerocellulose: new highly porous cellulose prepared from cellulose-NaOH aqueous solutions. Biomacromolecules. 9, 269–277 (2008)
Govindarajan, D., Duraipandy, N., Srivatsan, K.V., Lakra, R., Korapatti, P.S., Jayavel, R., Kiran, M.S.: Fabrication of hybrid collagen aerogels reinforced with wheat grass bioactives as instructive scaffolds for collagen turnover and angiogenesis for wound healing applications. ACS Appl. Mater. Interfaces. 9, 16939–16950 (2017). https://doi.org/10.1021/acsami.7b05842
Quraishi, S., Martins, M., Barros, A.A., Gurikov, P., Raman, S.P., Smirnova, I., Duarte, A.R.C., Reis, R.L.: Novel non-cytotoxic alginate–lignin hybrid aerogels as scaffolds for tissue engineering. J. Supercrit. Fluids. 105, 1–8 (2015). https://doi.org/10.1016/j.supflu.2014.12.026
Ge, J.H., Li, M.S., Zhang, Q.G., Yang, C.Z., Wooley, P.H., Chen, X.F., Yang, S.Y.: Silica aerogel improves the biocompatibility in a poly-epsilon-caprolactone composite used as a tissue engineering scaffold. Int. J. Polym. Sci. 2013, Artn 402859 (2013). https://doi.org/10.1155/2013/402859
Pircher, N., Fischhuber, D., Carbajal, L., Strauß, C., Nedelec, J.-M., Kasper, C., Rosenau, T., Liebner, F.: Preparation and reinforcement of dual-porous biocompatible cellulose scaffolds for tissue engineering. Macromol. Mater. Eng. 300, 911–924 (2015). https://doi.org/10.1002/mame.201500048
Toledo-Fernandez, J.A., Mendoza-Serna, R., Morales, V., de la Rosa-Fox, N., Pinero, M., Santos, A., Esquivias, L.: Bioactivity of wollastonite/aerogels composites obtained from a TEOS-MTES matrix. J. Mater. Sci. Mater. Med. 19, 2207–2213 (2008)
Horvat, G., Xhanari, K., Finšgar, M., Gradišnik, L., Maver, U., Knez, Ž., Novak, Z.: Novel ethanol-induced pectin–xanthan aerogel coatings for orthopedic applications. Carbohydr. Polym. 166, 365–376 (2017). https://doi.org/10.1016/j.carbpol.2017.03.008
Weng, L., Boda, S.K., Wang, H., Teusink, M.J., Shuler, F.D., **e, J.: Novel 3D hybrid nanofiber aerogels coupled with BMP-2 peptides for cranial bone regeneration. Adv. Healthc. Mater. (2018). https://doi.org/10.1002/adhm.201701415
Parandoush, P., Fan, H.X., Song, X.L., Lin, D.: Laser surface engineering of hierarchy hydroxyapatite aerogel for bone tissue engineering. J. Micro Nano-Manuf. 6, Artn 011007 (2018). https://doi.org/10.1115/1.4038669
Goimil, L., Braga, M.E.M., Dias, A.M.A., Gomez-Amoza, J.L., Concheiro, A., Alvarez-Lorenzo, C., de Sousa, H.C., Garcia-Gonzalez, C.A.: Supercritical processing of starch aerogels and aerogel-loaded poly (epsilon-caprolactone) scaffolds for sustained release of ketoprofen for bone regeneration. J. Co2 Util. 18, 237–249 (2017). https://doi.org/10.1016/j.jcou.2017.01.028
Kuttor, A., Szaloki, M., Rente, T., Kerenyi, F., Bako, J., Fabian, I., Lazar, I., Jenei, A., Hegedus, C.: Preparation and application of highly porous aerogel-based bioactive materials in dentistry. Front. Mater. Sci. 8, 46–52 (2014). https://doi.org/10.1007/s11706-014-0231-2
Veronovski, A., Novak, Z., Knez, Z.: Synthesis and use of organic biodegradable aerogels as drug carriers. J. Biomater. Sci. Polym. Ed. 23, 873–886 (2012). https://doi.org/10.1163/092050611x566126
Gaudio, P.D., Auriemma, G., Mencherini, T., Porta, G.D., Reverchon, E., Aquino, R.P.: Design of alginate-based aerogel for nonsteroidal anti-inflammatory drugs controlled delivery systems using prilling and supercritical-assisted drying. J. Pharm. Sci. 102, 185–194 (2013). https://doi.org/10.1002/jps.23361
Giray, S., Bal, T., Kartal, A.M., Kizilel, S., Erkey, C.: Controlled drug delivery through a novel PEG hydrogel encapsulated silica aerogel system. J. Biomed. Mater. Res. A. 100, 1307–1315 (2012). https://doi.org/10.1002/jbm.a.34056
Smirnova, I., Suttiruengwong, S., Seiler, M., Arlt, W.: Dissolution rate enhancement by adsorption of poorly soluble drugs on hydrophilic silica aerogels. Pharm. Dev. Technol. 9, 443–452 (2004)
Garcia-Gonzalez, C.A., **, M., Gerth, J., Alvarez-Lorenzo, C., Smirnova, I.: Polysaccharide-based aerogel microspheres for oral drug delivery. Carbohydr. Polym. 117, 797–806 (2015). https://doi.org/10.1016/j.carbpol.2014.10.045
Veres, P., Lopez-Periago, A.M., Lazar, I., Saurina, J., Domingo, C.: Hybrid aerogel preparations as drug delivery matrices for low water-solubility drugs. Int. J. Pharm. 496, 360–370 (2015). https://doi.org/10.1016/j.ijpharm.2015.10.045
Li, C.C., Chen, Y.T., Lin, Y.T., Sie, S.F., Chen-Yang, Y.W.: Mesoporous silica aerogel as a drug carrier for the enhancement of the sunscreen ability of benzophenone-3. Colloids Surf. B Biointerfaces. 115, 191–196 (2014). https://doi.org/10.1016/j.colsurfb.2013.11.011
Li, Y.K., Chou, M.J., Wu, T.Y., **n, T.R., Chen-Yang, Y.W.: A novel method for preparing a protein-encapsulated bioaerogel: using a red fluorescent protein as a model. Acta Biomater. 4, 725–732 (2008)
Gao, S.L., Wang, Y.J., Wang, T., Luo, G.S., Dai, Y.Y.: Immobilization of lipase on methyl-modified silica aerogels by physical adsorption. Bioresour. Technol. 100, 996–999 (2009)
Rossi, B., Campia, P., Merlini, L., Brasca, M., Pastori, N., Farris, S., Melone, L., Punta, C., Galante, Y.M.: An aerogel obtained from chemo-enzymatically oxidized fenugreek galactomannans as a versatile delivery system. Carbohydr. Polym. 144, 353–361 (2016). https://doi.org/10.1016/j.carbpol.2016.02.007
Arruebo, M.: Drug delivery from structured porous inorganic materials. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 4, 16–30 (2012)
Sher, P., Ingavle, G., Ponrathnam, S., Pawar, A.P.: Low density porous carrier – drug adsorption and release study by response surface methodology using different solvents. Int. J. Pharm. 331, 72–83 (2007)
Ulker, Z., Erkey, C.: An emerging platform for drug delivery: aerogel based systems. J. Control. Release. 177, 51–63 (2014). https://doi.org/10.1016/j.jconrel.2013.12.033
Veres, P., Sebok, D., Dekany, I., Gurikov, P., Smirnova, I., Fabian, I., Kalmar, J.: A redox strategy to tailor the release properties of Fe(III)-alginate aerogels for oral drug delivery. Carbohydr. Polym. 188, 159–167 (2018). https://doi.org/10.1016/j.carbpol.2018.01.098
Gonçalves, V.S.S., Matias, A.A., Poejo, J., Serra, A.T., Duarte, C.M.M.: Application of RPMI 2650 as a cell model to evaluate solid formulations for intranasal delivery of drugs. Int. J. Pharm. 515, 1–10 (2016). https://doi.org/10.1016/j.ijpharm.2016.09.086
Obaidat, R.M., Tashtoush, B.M., Bayan, M.F., Al Bustami, R.T., Alnaief, M.: Drying using supercritical fluid technology as a potential method for preparation of chitosan aerogel microparticles. AAPS PharmSciTech. 16, 1235–1244 (2015). https://doi.org/10.1208/s12249-015-0312-2
Alnaief, M., Obaidat, R., Mashaqbeh, H.: Effect of processing parameters on preparation of carrageenan aerogel microparticles. Carbohydr. Polym. 180, 264–275 (2018). https://doi.org/10.1016/j.carbpol.2017.10.038
Salmaso, S., Caliceti, P.: Stealth properties to improve therapeutic efficacy of drug nanocarriers. J. Drug Deliv. 2013, 19 (2013). https://doi.org/10.1155/2013/374252
Chen, R., Pearce, D.J.G., Fortuna, S., Cheung, D.L., Bon, S.A.F.: Polymer vesicles with a colloidal armor of nanoparticles. J. Am. Chem. Soc. 133, 2151–2153 (2011)
Sundararaj, S.C., Thomas, M.V., Peyyala, R., Dziubla, T.D., Puleo, D.A.: Design of a multiple drug delivery system directed at periodontitis. Biomaterials. 34, 8835–8842 (2013)
T. A. Technologies Bilipidex. http://www.bilipidex-aerogel.com/bilipidex/. Accessed 8 May 2018
Attia, Y.A.: Polymeric aerogel fibers and fiber webs. US Patent (2015)
Sabri, F., Sebelik, M.E., Meacham, R., Boughter Jr., J.D., Challis, M.J., Leventis, N.: In vivo ultrasonic detection of polyurea crosslinked silica aerogel implants. PLoS One. 8, e66348 (2013). https://doi.org/10.1371/journal.pone.0066348
Li, V.C.F., Dunn, C.K., Zhang, Z., Deng, Y., Qi, H.J.: Direct Ink Write (DIW) 3D printed cellulose nanocrystal aerogel structures. Sci Rep. 7 (2017). https://doi.org/10.1038/s41598-017-07771-y
Li, V.C.F., Mulyadi, A., Dunn, C.K., Deng, Y., Qi, H.J.: Direct ink write 3D printed cellulose nanofiber aerogel structures with highly deformable, shape recoverable, and functionalizable properties. ACS Sustain. Chem. Eng. 6, 2011–2022 (2018). https://doi.org/10.1021/acssuschemeng.7b03439
Foraida, Z.I., Kamaldinov, T., Nelson, D.A., Larsen, M., Castracane, J.: Elastin-PLGA hybrid electrospun nanofiber scaffolds for salivary epithelial cell self-organization and polarization. Acta Biomater. 62, 116–127 (2017). https://doi.org/10.1016/j.actbio.2017.08.009
Rubenstein, D.A., Venkitachalam, S.M., Zamfir, D., Wang, F., Lu, H., Frame, M.D., Yin, W.: In vitro biocompatibility of sheath-core cellulose-acetate-based electrospun scaffolds towards endothelial cells and platelets. J. Biomater. Sci. Polym. Ed. 21, 1713–1736 (2010). https://doi.org/10.1163/092050609x12559317149363
Markert, C.D., Guo, X., Skardal, A., Wang, Z., Bharadwaj, S., Zhang, Y., Bonin, K., Guthold, M.: Characterizing the micro-scale elastic modulus of hydrogels for use in regenerative medicine. J. Mech. Behav. Biomed. Mater. 27, 115–127 (2013). https://doi.org/10.1016/j.jmbbm.2013.07.008
Author information
Authors and Affiliations
Corresponding authors
Editor information
Editors and Affiliations
Glossary
- Anaphylatoxins
-
A toxic substance formed in the blood that is associated with bacterial polysaccharides
- Bolus Release
-
Administration of a drug over a relatively quick amount of time (less than 5 min) in comparison to a sustained delivery which can last over hours
- Cytotoxicity
-
A quantification of the products that may have a toxic effect on cells
- Hemolysis
-
The breakdown of red blood cells with the release of hemoglobin
- Live/Dead Cell Cytotoxicity Assay
-
A measurement technique to quantify cell viability through the number of live and dead cells within the culture. Only live cells uptake calcein which is hydrolyzed by intracellular esterases to fluoresce green. Only cells with a compromised cell membrane (dead or dying cells) can uptake ethidium which binds to DNA to fluoresce red
- Scaffold
-
A three-dimensional structure that can be used to direct cell growth or serve as a location for cell growth
Rights and permissions
Copyright information
© 2023 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Yin, W., Rubenstein, D.A. (2023). Biomedical Applications of Aerogels. In: Aegerter, M.A., Leventis, N., Koebel, M., Steiner III, S.A. (eds) Springer Handbook of Aerogels. Springer Handbooks. Springer, Cham. https://doi.org/10.1007/978-3-030-27322-4_57
Download citation
DOI: https://doi.org/10.1007/978-3-030-27322-4_57
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-27321-7
Online ISBN: 978-3-030-27322-4
eBook Packages: Chemistry and Materials ScienceChemistry and Material Science (R0)