Abstract
Background
While patients with multiple comorbidities may have frequent contact with medical providers, it is unclear whether their healthcare visits translate into earlier detection of cancers, specifically breast and colon cancers.
Methods
Patients diagnosed with stage I-IV breast ductal carcinoma and colon adenocarcinoma were identified from the National Cancer Database and stratified by comorbidity burden, dichotomized as a Charlson Comorbidity Index (CCI) Score of <2 or ≥2. Characteristics associated with comorbidities were analyzed by univariate and multivariate logistic regression. Propensity-score matching was performed to determine the impact of CCI on stage at cancer diagnosis, dichotomized as early (I-II) or late (III-IV).
Results
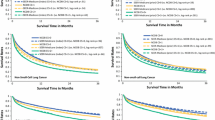
A total of 672,032 patients with colon adenocarcinoma and 2,132,889 with breast ductal carcinoma were included. Patients with colon adenocarcinoma who had a CCI ≥ 2 (11%, n = 72,620) were more likely to be diagnosed with early-stage disease (53% vs. 47%; odds ratio [OR] 1.02, p = 0.017), and this finding persisted after propensity matching (CCI ≥ 2 55% vs. CCI < 2 53%, p < 0.001). Patients with breast ductal carcinoma who had a CCI ≥ 2 (4%, n = 85,069) were more likely to be diagnosed with late-stage disease (15% vs. 12%; OR 1.35, p < 0.001). This finding also persisted after propensity matching (CCI ≥ 2 14% vs. CCI < 2 10%, p < 0.001).
Conclusions
Patients with more comorbidities are more likely to present with early-stage colon cancers but late-stage breast cancers. This finding may reflect differences in practice patterns for routine screening in these patients. Providers should continue guideline directed screenings to detect cancers at an earlier stage and optimize outcomes.



Similar content being viewed by others
References
Hamilton W, Walter FM, Rubin G, Neal RD. Improving early diagnosis of symptomatic cancer. Nat Rev Clin Oncol. 2016;13(12):740–9. https://doi.org/10.1038/nrclinonc.2016.109.
Crosby D, Bhatia S, Brindle KM, et al. Early detection of cancer. Science. 2022. https://doi.org/10.1126/science.aay9040.
Swann R, McPhail S, Witt J, et al. Diagnosing cancer in primary care: results from the national cancer diagnosis audit. Br J Gen Pract. 2018;68(666):e63-72. https://doi.org/10.3399/bjgp17X694169.
Søgaard M, Thomsen RW, Bossen KS, Sørensen HT, Nørgaard M. The impact of comorbidity on cancer survival: a review. Clin Epidemiol. 2013;5(Suppl 1):3–29. https://doi.org/10.2147/CLEP.S47150.
Sarfati D, Koczwara B, Jackson C. The impact of comorbidity on cancer and its treatment. CA Cancer J Clin. 2016;66(4):337–50. https://doi.org/10.3322/caac.21342.
Morishima T, Matsumoto Y, Koeda N, et al. Impact of comorbidities on survival in gastric, colorectal, and lung cancer patients. J Epidemiol. 2019;29(3):110–5. https://doi.org/10.2188/jea.JE20170241.
Zulman DM, Asch SM, Martins SB, Kerr EA, Hoffman BB, Goldstein MK. Quality of care for patients with multiple chronic conditions: the role of comorbidity interrelatedness. J Gen Intern Med. 2014;29(3):529–37. https://doi.org/10.1007/s11606-013-2616-9.
Schneider KM, O’Donnell BE, Dean D. Prevalence of multiple chronic conditions in the United States’ Medicare population. Health Qual Life Outcomes. 2009;7:82. https://doi.org/10.1186/1477-7525-7-82.
Wolff JL, Starfield B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch Intern Med. 2002;162(20):2269–76. https://doi.org/10.1001/archinte.162.20.2269.
Lehnert T, Heider D, Leicht H, et al. Review: health care utilization and costs of elderly persons with multiple chronic conditions. Med Care Res Rev. 2011;68(4):387–420. https://doi.org/10.1177/1077558711399580.
Gurney J, Sarfati D, Stanley J. The impact of patient comorbidity on cancer stage at diagnosis. Br J Cancer. 2015;113(9):1375–80. https://doi.org/10.1038/bjc.2015.355.
Fleming ST, Pursley HG, Newman B, Pavlov D, Chen K. Comorbidity as a predictor of stage of illness for patients with breast cancer. Med Care. 2005;43(2):132–40. https://doi.org/10.1097/00005650-200502000-00006.
American Cancer Society Guideline for Colorectal Cancer Screening. Accessed 7 Dec 2022. https://www.cancer.org/cancer/colon-rectal-cancer/detection-diagnosis-staging/acs-recommendations.html
Tsai MH, **rasagar S, Li YJ, de Groen PC. Colonoscopy screening among US adults aged 40 or older with a family history of colorectal cancer. Prev Chronic Dis. 2015;12:E80. https://doi.org/10.5888/pcd12.140533.
American Cancer Society Recommendations for the Early Detection of Breast Cancer. 2022.
Renzi C, Lyratzopoulos G, Hamilton W, Maringe C, Rachet B. Contrasting effects of comorbidities on emergency colon cancer diagnosis: a longitudinal data-linkage study in England. BMC Health Serv Res. 2019;19(1):311. https://doi.org/10.1186/s12913-019-4075-4.
Zafar SY, Abernethy AP, Abbott DH, et al. Comorbidity, age, race and stage at diagnosis in colorectal cancer: a retrospective, parallel analysis of two health systems. BMC Cancer. 2008;8:345. https://doi.org/10.1186/1471-2407-8-345.
Arneja J, Brooks JD. The impact of chronic comorbidities at the time of breast cancer diagnosis on quality of life, and emotional health following treatment in Canada. PLoS One. 2021;16(8):e0256536. https://doi.org/10.1371/journal.pone.0256536.
Zhang D, Advani S, Zhu Z, Dang L, Walter LC, Braithwaite D. Mammography use in relation to comorbidities and functional limitations among older breast cancer survivors. J Cancer Surviv. 2021;15(1):119–26. https://doi.org/10.1007/s11764-020-00917-4.
Fu MR, Axelrod D, Guth AA, et al. Comorbidities and quality of life among breast cancer survivors: a prospective study. J Pers Med. 2015;5(3):229–42. https://doi.org/10.3390/jpm5030229.
Ng HS, Vitry A, Koczwara B, Roder D, McBride ML. Patterns of comorbidities in women with breast cancer: a Canadian population-based study. Cancer Causes Control. 2019;30(9):931–41. https://doi.org/10.1007/s10552-019-01203-0.
Bilimoria KY, Stewart AK, Winchester DP, Ko CY. The National Cancer data base: a powerful initiative to improve cancer care in the United States. Ann Surg Oncol. 2008;15(3):683–90. https://doi.org/10.1245/s10434-007-9747-3.
Oeffinger KC, Fontham ET, Etzioni R, et al. Breast cancer screening for women at average risk: 2015 Guideline update from the American cancer society. JAMA. 2015;314(15):1599–614. https://doi.org/10.1001/jama.2015.12783.
Shaukat A, Kahi CJ, Burke CA, Rabeneck L, Sauer BG, Rex DK. ACG clinical guidelines: colorectal cancer screening 2021. Am J Gastroenterol. 2021;116(3):458–79. https://doi.org/10.14309/ajg.0000000000001122.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83. https://doi.org/10.1016/0021-9681(87)90171-8.
Quan H, Li B, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173(6):676–82. https://doi.org/10.1093/aje/kwq433.
de Groot V, Beckerman H, Lankhorst GJ, Bouter LM. How to measure comorbidity a critical review of available methods. J Clin Epidemiol. 2003;56(3):221–9. https://doi.org/10.1016/s0895-4356(02)00585-1.
Austin SR, Wong YN, Uzzo RG, Beck JR, Egleston BL. Why summary comorbidity measures such as the charlson comorbidity index and Elixhauser score work. Med Care. 2015;53(9):e65-72. https://doi.org/10.1097/MLR.0b013e318297429c.
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46(3):399–424. https://doi.org/10.1080/00273171.2011.568786.
Wolf AMD, Fontham ETH, Church TR, et al. Colorectal cancer screening for average-risk adults: 2018 guideline update from the American Cancer Society. CA Cancer J Clin. 2018;68(4):250–81. https://doi.org/10.3322/caac.21457.
Väyrynen JP, Tuomisto A, Väyrynen SA, et al. Preoperative anemia in colorectal cancer: relationships with tumor characteristics, systemic inflammation, and survival. Sci Rep. 2018;8(1):1126. https://doi.org/10.1038/s41598-018-19572-y.
Astin M, Griffin T, Neal RD, Rose P, Hamilton W. The diagnostic value of symptoms for colorectal cancer in primary care: a systematic review. Br J Gen Pract. 2011;61(586):e231–43. https://doi.org/10.3399/bjgp11X572427.
Ewing M, Naredi P, Zhang C, Månsson J. Identification of patients with non-metastatic colorectal cancer in primary care: a case-control study. Br J Gen Pract. 2016;66(653):e880–6. https://doi.org/10.3399/bjgp16X687985.
Virdee PS, Marian IR, Mansouri A, et al. The full blood count blood test for colorectal cancer detection: a systematic review, meta-analysis, and critical appraisal. Cancers (Basel). 2020. https://doi.org/10.3390/cancers12092348.
Shi C, **e M, Li L, Li K, Hu BL. The association and diagnostic value of red blood cell distribution width in colorectal cancer. Medicine (Baltimore). 2019;98(19):e15560. https://doi.org/10.1097/MD.0000000000015560.
Hornbrook MC, Goshen R, Choman E, et al. Early colorectal cancer detected by machine learning model using gender, age, and complete blood count data. Dig Dis Sci. 2017;62(10):2719–27. https://doi.org/10.1007/s10620-017-4722-8.
Lykkeboe S, Andersen SL, Nielsen CG, Vestergaard P, Christensen PA. Blood sampling frequency as a proxy for comorbidity indices when identifying patient samples for review of reference intervals. Clin Chem Lab Med. 2022;60(2):252–60. https://doi.org/10.1515/cclm-2021-0987.
Kaunitz JD, Ganz T. AGA clinical practice guidelines on the gastrointestinal evaluation of iron deficiency anemia. Gastroenterology. 2021;161(1):362–5. https://doi.org/10.1053/j.gastro.2021.03.001.
Diaz A, Kang J, Moore SP, et al. Association between comorbidity and participation in breast and cervical cancer screening: a systematic review and meta-analysis. Cancer Epidemiol. 2017;47:7–19. https://doi.org/10.1016/j.canep.2016.12.010.
Jiménez-Garcia R, Hernandez-Barrera V, Carrasco-Garrido P, Gil A. Prevalence and predictors of breast and cervical cancer screening among Spanish women with diabetes. Diabetes Care. 2009;32(8):1470–2. https://doi.org/10.2337/dc09-0479.
Lipscombe LL, Fischer HD, Austin PC, et al. The association between diabetes and breast cancer stage at diagnosis: a population-based study. Breast Cancer Res Treat. 2015;150(3):613–20. https://doi.org/10.1007/s10549-015-3323-5.
Schrager S, Ovsepyan V, Burnside E. Breast cancer screening in older women: the importance of shared decision making. J Am Board Fam Med. 2020;33(3):473–80. https://doi.org/10.3122/jabfm.2020.03.190380.
Walter LC, Schonberg MA. Screening mammography in older women: a review. JAMA. 2014;311(13):1336–47. https://doi.org/10.1001/jama.2014.2834.
Qaseem A, Lin JS, Mustafa RA, et al. Screening for breast cancer in average-risk women: a guidance statement from the American college of physicians. Ann Intern Med. 2019;170(8):547–60. https://doi.org/10.7326/M18-2147.
Siu AL, Force USPST. Screening for Breast Cancer U.S. preventive services task force recommendation statement. Ann Intern Med. 2016;164:279–96. https://doi.org/10.7326/M15-2886.
Land LH, Dalton SO, Jørgensen TL, Ewertz M. Comorbidity and survival after early breast cancer. A review Crit Rev Oncol Hematol. 2012;81(2):196–205. https://doi.org/10.1016/j.critrevonc.2011.03.001.
Li YR, Ro V, Tchou JC. Obesity, metabolic syndrome, and breast cancer: from prevention to intervention. Curr Surg Rep. 2018. https://doi.org/10.1007/s40137-018-0204-y.
Michalopoulou E, Matthes KL, Karavasiloglou N, et al. Impact of comorbidities at diagnosis on the 10-year colorectal cancer net survival: a population-based study. Cancer Epidemiol. 2021;73:101962. https://doi.org/10.1016/j.canep.2021.101962.
Boakye D, Rillmann B, Walter V, Jansen L, Hoffmeister M, Brenner H. Impact of comorbidity and frailty on prognosis in colorectal cancer patients: a systematic review and meta-analysis. Cancer Treat Rev. 2018;64:30–9. https://doi.org/10.1016/j.ctrv.2018.02.003.
Munro AJ, Bentley AH. Deprivation, comorbidity and survival in a cohort of patients with colorectal cancer. Eur J Cancer Care (Engl). 2004;13(3):254–62. https://doi.org/10.1111/j.1365-2354.2004.00480.x.
Tong L, Ahn C, Symanski E, Lai D, Du XL. Effects of newly developed chemotherapy regimens, comorbidities, chemotherapy-related toxicities on the changing patterns of the leading causes of death in elderly patients with colorectal cancer. Ann Oncol. 2014;25(6):1234–42. https://doi.org/10.1093/annonc/mdu131.
Sarfati D, Hill S, Blakely T, et al. The effect of comorbidity on the use of adjuvant chemotherapy and survival from colon cancer: a retrospective cohort study. BMC Cancer. 2009;9:116. https://doi.org/10.1186/1471-2407-9-116.
Funding
Dr. Fayanju is supported by the National Institutes of Health (NIH) under Award Number 7K08CA241390 (PI: Fayanju). The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
CS had full access to the data and takes responsibility for the integrity of the data and the accuracy of the analyses Study conception or design: Sharon, Wang, Tortorello, Perry, Ma, Miura, Karakousis Data acquisition, analysis, or interpretation: Sharon, Wang, Tortorello, Perry, Ma, Miura, Karakousis Drafting or critically revising the work: Sharon, Wang, Tortorello, Perry, Ma, Tchou, Fayanju, Mahmoud, Miura, Karakousis
Corresponding author
Ethics declarations
Disclosure
None
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sharon, C.E., Wang, M., Tortorello, G.N. et al. Impact of Patient Comorbidities on Presentation Stage of Breast and Colon Cancers. Ann Surg Oncol 30, 4617–4626 (2023). https://doi.org/10.1245/s10434-023-13596-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-023-13596-z