Abstract
Objective
With the increase in the prevalence rate and improvements in the survival of breast cancer patients, there is a growing interest in understanding the level of psychosocial adjustment in these patients. The study aimed to describe the illness perception and psychosocial adjustment levels of both breast cancer patients and their spouses, to use the Actor-Partner Interdependence Model (APIM) to clarify the actor-partner relationships between spouses, and to explore the impact of illness perception on psychosocial adjustment to the disease within the joint actions of both spouses.
Methods
A total of 216 female patients with breast cancer and their spouses participated in the study. They were selected from two tertiary hospitals in Guangdong Province, China from October 2022 to May 2023 using a convenience sampling method. The participants were assessed using the Brief Illness Perception Questionnaire and the Psychosocial Adjustment to Illness Scale to examine the relationship between illness perception and psychosocial adjustment. AMOS24.0 was used to test and analyze the actor-partner interdependence model.
Results
The illness perception score (57.75 ± 10.91) was slightly higher than that of the spouse (57.10 ± 11.00), and the psychosocial adjustment score (64.67 ± 6.33) was slightly lower than that of the spouse (64.76 ± 7.49). The results of the actor-partner interdependence model indicated that there was a couple partner between breast cancer patients and their spouses: the spouse’s illness perception significantly affected the patient’s psychosocial adjustment (β = 0.095, p = 0.015); the patient’s illness perception also significantly affected the spouse’s psychosocial adjustment (β = 0.106, p = 0.033). Among them, the patient’s psychosocial adjustment was found to be related to the patient’s illness comprehensibility or coherence of illness (β = 0.433, p = 0.009), the spouse’s emotional illness representation (β = 0.218, p = 0.037), and the spouse’s illness comprehensibility or coherence of illness (β = 0.416, p = 0.007), while the spouse’s psychosocial adjustment was only related to the spouse’s illness comprehensibility or coherence of illness (β = 0.528, p = 0.007).
Conclusions
The psychosocial adjustment of breast cancer patients is affected by both their own and spouse’s illness perception. Therefore, in the future, the healthcare staff can implement early psychological interventions for patients diagnosed with breast cancer and their spouses as a unit to promote the psychosocial adjustment of them.
Similar content being viewed by others
Background
Breast cancer (BC) is the most common malignancy threatening women’s health worldwide. According to the Global Cancer Statistics Report [1], there are approximately 2.26 million new cases of BC each year, ranking first in the incidence of cancer. In China, there are approximately 368,000 new cases of BC annually, and the number is increasing yearly [2]. With advancements in medicine, the survival rate of patients with BC has gradually increased. In the United States, the five-year survival rate of patients with early-stage BC is 90% [3], and in China, the five-year survival rate of patients with middle- and advanced-stage BC has also increased from 20 to 60% [4]. With the prolongation of the survival cycle of BC patients, patients faced not only various problems arising from disease treatment and symptom management [5], but also complex physical and psychological changes that affect the quality of life [6, 7].
Psychosocial adjustment is an essential facet of enhancing the quality of life for patients [8]. It refers to the ability of patients with BC to adapt and coordinate in multiple aspects [9], such as family life, social life, and sex, when they endure various symptoms and pain caused by the diagnosis and treatment of BC. A study has shown that illness perception is a pivotal predictor of the physical and mental health of patients and can significantly affect their psychosocial adjustment level [10]. Several theories and models have highlighted the profound impact of patients’ beliefs and perceptions of their disease and symptoms on their psychological adjustment [11, 12]. In addition, Leventhal’s self-regulatory model suggests that when people are stimulated (disease diagnosis or symptom presentation), they form an illness perception [13]. Illness perception [14] (IP) refers to the process in which patients adjust, modify, and cope with disease cognition and emotional response based on previous disease experience when facing a disease or health threat, including the cognitive representation (problem-centred and different responses to the individual’s perception of the disease), emotional representation (pmotionally centered, tending to adopt a certain emotion to cope), and illness comprehensibility (degree of knowledge of the disease).
Cancer, as a kind of “we disease”, not only affects the physical and mental health of patients with BC but also introduces challenges and pressure to the entire family [15]. Particularly in intimate relationships, there exists a strong interaction between two individuals [16], and an individual’s emotion can be easily conveyed between the two [17]. During the diagnosis and treatment of patients with BC, the spouse, as their primary caregiver and source of emotional and financial support also suffers from different levels of stress, which are similar to or even stronger than that of the patient [18]. However, the majority of current studies only discuss the influence of patients’ illness perception on the psychosocial adjustment of illness, neglecting the influence of patients and their spouses on the psychosocial adjustment to illness (PAI).
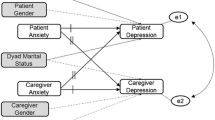
Therefore, this study aims to explore the impact of disease perception on disease psychosocial adjustment under the joint action of husband and wife by describing the illness perception and psychosocial adjustment level of BC patients and their spouses, and using APIM to clarify the actor-partner relationship between husband and wife. The hypothesis framework of this study is shown in Fig. 1.
The hypothesis framework of IP and PAI between patients and spouses. Note. S-IP represents Spouse-Illness Perception; P-IP stands for Patient-Illness Perception; P-PAI represents Patient-Psychosocial Adjustment to Illness; S-PAI refers to Spouse-Psychosocial Adjustmentto Illness. a1: S-IP → S-PAI; a2: P-IP → P-PAI; p1:P-IP → S-PAI; p2: S-IP → P-PAI; where k equals the ratio of patient to spouse (p/a)
Method
Design and participants
A cross-sectional design using a survey was employed in this study. Patients with BC and their spouses from two tertiary hospitals in Guangdong Province, China, were selected between October 2022 and May 2023 using a convenience sampling method. Inclusion criteria for patients were: (1) diagnosis of primary BC (without metastatic); (2) having normal cognitive and understanding abilities; (3) being aware of BC diagnosis and participating in this study voluntarily. Exclusion criteria for patients were: (1) previous diagnoses of other primary malignancies; (2) a state of illness that does not permit collaboration with the investigator. Inclusion criteria for spouses were: (1) being the legal spouse of patients with BC; (2) having normal cognitive and understanding abilities; (3) knowing the patient’s BC diagnosis and participated in this study voluntarily. Exclusion criteria for spouses were: (1) having a serious life-threatening disease.
Data collection
This study was conducted by uniformly trained investigators who undertook the investigation process. During the patient’s treatment, the investigator conducted surveys of the patient and their spouse. During the investigation, the investigator answered the respondents’ questions while filling in the questionnaire. The investigator collected and checked the questionnaire on the spot and promptly communicated with the patient to fill in the missing items.
A total of 227 pairs of patients (all female) and their spouses were recruited, and 11 pairs were excluded based on the exclusion criteria. Finally, 216 pairs of cancer patients and their spouses completed the survey. Two researchers input the data to ensure the accuracy of the data.
Measurements
Baseline variables
The researchers designed the general demographic characteristics questionnaire. Basic information included the age, occupation, the education level of the patient and her spouse. The patient case data included the course of the disease, the clinical stage of the tumor, and the surgical method.
Illness perception
The Brief Illness Perception Questionnaire (BIPQ), developed by Broadbent et al. [19] and adjusted by Meiyaqi et al. [20] has been widely used to measure the IP of Chinese patients. The questionnaire consisted of eight items, with each item divided into three dimensions: cognitive representation, emotional illness representation, and illness comprehensibility or coherence of illness. We used 0–10 points, with a total score of 0–80 points. The higher the score, the more patients’ cognition and negative emotions about the disease. The Cronbach’s α of the Chinese vision of this scale was 0.77.
Psychosocial adjustment to illness
Psychosocial adjustment was assessed using the Psychosocial Adjustment to Illness Scale (PAIS-SR) developed by Derogatis et al. [21] The Chinese version of PAIS-SR, translated by Yao et al. [22], has been widely used in China. The Chinese version of PAIS-SR contains 44 items and the following seven dimensions: health care orientation, vocational environment, domestic environment, sexual relationship, extended family relationship, social environment, and psychological distress. Each item is scored from 0 to 3 points, with total points from 0 to 132. A total of 0–34, 35–50, and 51–132 indicated mild, moderate, and severe, respectively. The higher the score, the greater the psychological and social adjustment problems. The Cronbach’s α of Chinese visions was 0.872.
Statistic analysis
SPSS24.0 and AMOS24.0 were used for data analysis. The mean and standard deviation were used to describe the measurement data, and the frequency and percentage were used to describe the count data. Chi-square test and paired sample t-test were used to compare patients’ and spouses’ general information, IP, and psychosocial adjustment to illness. The Pearson correlation coefficient was used to test the correlation between variables. When analyzing data between spouses, the two are interdependent, which violates the independence hypothesis of the materiality test [23]. Considering the non-independence of paired samples, Kenny et al. [23] put forward the actor–partner interdependence model (APIM), which has been used in the study of couple interaction. This model is a paired data analysis method mostly used in marriage and family fields and can simultaneously assess the influence between individual variables and between individual and spouse variables [24]. We used a structural equation model (SEM) with maximum likelihood estimation for APIM [25]. Set the calculation formula of k in the software k = p/a, and set clearly what a and p in the model represent respectively. The purpose of calculating the k value is to determine whether the relationship between the patient and the spouse is actor-only, contrast partner, parter-only, or couple partner by comparing the size and confidence interval of the k value between the patient and the spouse, and finally determine the optimal model. And we use the following recommended indicators to judge the fit of the model: χ2 /df < 3, GFI > 0.9, AGFI > 0.9, RMSEA < 0.08, SRMR < 0.05, AIC (the lower the AIC value, the better the model fits).
Results
Characteristics of the participants
The mean ages of patients and spouses were 52.77 ± 11.04 and 52.70 ± 10.74, respectively. About 53.70% of patients and 38.89% of spouses had an education level at or below junior high school. Most participants had a monthly income of less than 3,000 yuan. According to the clinical data of patients, for 44.44% of patients, the time since diagnosis was within three months. All patients with BC in this study were female. Other characteristics of the samples are shown in Table 1.
IP and PAI scores of patients with breast cancer and their spouses
The total scores of patients’ and spouses’ IP were 57.75 ± 10.91 and 57.10 ± 11.00, and the total scores of PAI were 64.67 ± 6.33 and 64.76 ± 7.49, respectively (Table 2). The total scores of IP and PAI of patients and spouses showed no statistically significant (p > 0.05), but the dimensions of emotional illness representation within IP and health care orientation and domestic environment within PAI showed statistically significant differences (p < 0.05) (Table 2).
Correlation between IP and PAI
Table 3 shows that the patient’s IP was positively correlated with their PAI and the IP and PAI of their spouses (p < 0.01). There was a positive correlation between spouses’ IP and patients’ PAI (p < 0.01), as well as between the spouses’ PAI and the patients’ PAI (p < 0.01) (Table 3).
Breast cancer - APIM fitting of IP and PAI in spouses
As patients and spouses can be distinguished by their roles, the standard model of APIM was first tested for distinguishable pairwise relationships (MODEL 1). The results of the actor effect showed that the wife’s IP significantly influenced her own PAI (β = 0.182, p = 0.001). However, the spouse’s IP did not significantly affect t his own PAI (β = 0.078, p = 0.113). Regarding the partner effect, the spouse’s IP significantly impacted the patient’s PAI (β = 0.095, p = 0.015), and the patient’s IP also significantly impacted the spouse’s PAI (β = 0.106, p = 0.033).
Before calculating the value of k (k = p/a), limiting the actor effect between couples to equal the partner effect did not worsen MODEL 2: χ2 = 3.390, p = 0.184. The p-value was less than the 0.20 as suggested by Kenny et al. [23], indicating that the model could not accept equal effects for patients and spouses. Therefore, the pairwise model analysis was still calculated as a distinguishable pairwise relationship.
According to the results of the saturation model, the normalized absolute values of the actor effect of the patient and spouse both exceeded 0.1, so the k-value can be estimated by estimating the APIM containing the ghost variable. The confidence interval was determined through 5,000 repeated Bootstrap samplings. After testing, the patient’s k-value (k2) was 0.522, and the 95% confidence interval ranged from 0.058 to 1.329; the confidence interval contained 1, indicating that the patient’s pairing pattern was couple pattern. The spouse’s k-value (k1) was 1.356, and the 95% confidence interval ranged from − 0.068 to 14.187, with 0 and 1 in the confidence interval, indicating that the spouse’s pair pattern was actor-only or couple pattern. To verify the pairing pattern of the spouse and patient, the restriction k was equal to a special value in the confidence interval (1) MODEL 3: k1 = 1, k2 = 1, that is, a1 = p1, a2 = p2; MODEL 4: k1 = 0, k2 = 1, that is, p1 = 0, a2 = p2. The results showed that Model 3 had the best fitting effect, and the patient and spouse were couple pattern (Fig. 2; Tables 4 and 5).
To further explore the relationship between the disease perception and psychosocial adjustment of breast cancer patients and their spouses, the disease perception of patients and spouses was divided into three dimensions: Cognitive Representation, Emotional Illness Representation, and Illness Comprehensibility or Coherence of illness for APIM analysis. The results show that the model fits well, χ2 /df = 1.931, GFI = 0.991, AGFI = 0.920, RMSEA = 0.066, SRMR = 0.034, The patient’s psychosocial adjustment to illness is related to the patient’s illness comprehensibility or coherence of illness, the spouse’s emotional illness representation, and the spouse’s illness comprehensibility or coherence of illness, while the spouse’s psychosocial adjustment to illness is only related to the spouse’s illness comprehensibility or coherence of illness. As shown in Fig. 3.
APIM paths of the patients and spouses 2. Note. P-PAI: Patient-Psychosocial Adjustment to Illness; S-PAI: Spouse-Psychosocial Adjustment to Illness; S-EIR: Spouse-Emotional illness representation; S-ICC: Spouse-Illness comprehensibility or coherence of illness; P-ICC: Patient-Illness comprehensibility or coherence of illness. ***p < 0.001, **p < 0.01, *p < 0.05
Discussion
This study investigated the status of illness perception and its association with psychosocial adjustment in patients with BC and their spouses. Additionally, this study explored the interactive impact of IP between patients with BC and their spouses on their psychosocial adjustment based on the APIM. This approach further strengthened the understanding of the mechanism of interaction between the two, providing a unique perspective for future experimental research.
The findings showed that the IP scores of patients with BC and their spouses were (57.75 ± 10.91) and (57.10 ± 11.00) points, respectively, which were similar to the results by Zhou Jie et al. [26], but higher than the results of Xu et al. [27] in patients with lung cancer. This difference may be related to gender [28] and disease characteristics. First, the somatic symptoms and psychological stress of patients participating in the study during the treatment of the disease may affect their perception of the disease [29, 30], resulting in a significantly higher score in the emotional dimension of the patients’ illness perception compared to their spouses. Second, studies have shown that women are more focused on health and emotional expression [31, 32], and women are the predominant group for breast cancer, which means that they may exhibit greater awareness of their feelings and may have a stronger perception of the disease due to the change in body image that comes with breast cancer [31, 33]. In addition, differences in educational attainment may also be a factor influencing their perception of the disease due to differences in the educational level of patients and spouses in this study [34, 35].
In this study, the PAI scores of the patients and their spouses were in the stage of severe maladjustment, which was higher than the results of Shen Aomei et al. [36] This may be because the patients and their spouses in this study are mostly farmers or self-employed individuals. When patients initially receive treatment for their illness, both the patients and their spouses have to temporarily leave their work to cope with the illness together, leading to a sudden decrease in family income. Additionally, due to the high cost of cancer treatment and other factors, both patients and spouses bear a significant psychological burden. In addition, we found that the family relationship dimension of the spouses’ PAI was significantly poorer than that of the patients (p < 0.05). This finding may be attributed to the spouse needs to assume multiple roles in the family to make up for the instability of the family structure caused by the illness, leading to potential difficulties in the adjustment process while taking on these responsibilities [5]. Therefore, during medical treatment and diagnosis of patients with BC, medical personnel should not only pay attention to the psychosocial status of patients but also extend their attention to the psychosocial status of spouses. Targeted psychological counseling should be provided to alleviate the psychological stress of both patients and spouses, enhance their ability to cope with and adjust to the disease, and ultimately improve the patients’ quality of life.
Similar to previous studies, we found that patients’ perception of illness was significantly correlated with the level of psychosocial adjustment to illness [37]. Positive perception of illness can improve patients’ self-efficacy and self-management ability, promote emotional and psychosocial adjustment, and improve their quality of life [38, 39]. This study also confirmed the positive relationship between the two: the lower the patient’s perception of illness, the better the psychosocial adjustment. Because the trajectories of couples are often closely related after BC diagnosis [40], they experience a series of BC-associated stresses, such as changes in sexual behavior, during which individual interactions may affect their adjustment to the disease [41]. Moreover, APIM analysis results confirmed that IP and PAI have actor–partner effects in patients with BC and their spouses and formed a couple pattern. Specifically, patients’ PAI was affected by themselves and their spouses, but spouses’ PAI was affected only by their patients. This can be easily comprehended because BC affects both spouses collectively, and a spouse’s BC may bring about changes in the relationship dynamics—either fostering greater closeness or creating distance—and affect the psychosocial status of both partners [15, 42]. However, the PAI of spouses is only influenced by the IP of patients, which further elucidates the specific pathway of the role of IP and PAI between spouses. This finding could be promising as it offers a new perspective and intervention pathway for enhancing PAI in BC patients. For example, IP-related interventions targeted at spouses can enhance the PAI of patients, while IP-related interventions targeted at patients can simultaneously improve the PAI of both spouses. Further research has revealed that the emotional illness manifestation of spouses and the comprehensibility or coherence of the illness can affect the patient’s level of psychosocial adaptation. This underscores the strong interaction between patients and spouses as an intimate unit, where enhancing the patient’s level of psychosocial adaptation can be achieved through intervening in the emotions of the spouse and their understanding of the illness.
Study limitations
There are some limitations in this study. First, the study only collected data on patients with BC and their spouses at two hospitals, so caution is needed when generalizing the results to other groups. Second, the study used a cross-sectional study design with limited explanations for causality. Therefore, longitudinal studies, including the period from cancer diagnosis to treatment and recovery, are needed along with consideration of the effects of confounding variables on psychosocial adjustment to the disease. Third, these instruments have been validated for use in breast cancer patients, but have not yet been validated in their partners. Fourth, while this study has revealed factors influencing PAI, addressing other factors affecting marital relationships (such as intimacy, dynamics of couples before and after cancer) is necessary.
Conclusion and clinical implications
In this study, the level of IP and PAI were investigated on 216 pairs of patients with BC and their spouses. The results showed that the PAI of patients with BC was affected by the actor’s IP and the partner’s IP. Therefore, in the future, after the diagnosis of BC disease, medical personnel can implement early psychological intervention by treating patients and their spouses as dual subjects using mindfulness-based stress reduction, cognitive behavioral therapy, and other measures to promote PAI.
Data availability
The data is not publicly available because further research is being conducted and more manuscripts are being prepared. Data for the present study will be made accessible upon reasonable request from the principal investigator or corresponding author.
References
Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49. https://doi.org/10.3322/caac.21660.
Feng RM, Zong YN, Cao SM, et al. Current cancer situation in China: good or bad news from the 2018 global cancer statistics? Cancer Commun (Lond). 2019;39:22. https://doi.org/10.1186/s40880-019-0368-6.
Siegel RL, Miller KD, Wagle NS, et al. Cancer statistics, 2023. CA Cancer J Clin. 2023;73:17–48. https://doi.org/10.3322/caac.21763.
Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115–32. https://doi.org/10.3322/caac.21338.
Zhang YX. The relationship between disease perception, mindfulness and fear of cancer recurrence among breast cancer patients and their spouses: the mediating role of family cancer avoidance communication. Shan Dong University (China); 2023.
Van Vulpen JK, Peeters PH, Velthuis MJ, et al. Effects of physical exercise during adjuvant breast cancer treatment on physical and psychosocial dimensions of cancer-related fatigue: a meta-analysis. Maturitas. 2016;85:104–11. https://doi.org/10.1016/j.maturitas.2015.12.007.
Pitman A, Suleman S, Hyde N. Depression and anxiety in patients with cancer. BMJ (Clin Res Ed). 2018;361:k1415. https://doi.org/10.1136/bmj.k1415.
Falagas ME, Zarkadoulia EA, Ioannidou EN. The effect of psychosocial factors on breast cancer outcome: a systematic review. Breast Cancer Res. 2007;9:R44. https://doi.org/10.1186/bcr1744.
Stanton AL, Bower JE. (2015) Psychological adjustment in breast cancer survivors. In: Improving Outcomes for Breast Cancer Survivors: Perspectives on Research Challenges and Opportunities 231–242.
Lu Q, Zeng L, Gong MF. Research progress of disease perception in chronic disease management. Nurs Res (China). 2016;30:1288–91.
Hagger MS, Koch S, Chatzisarantis NLD, et al. The common sense model of self-regulation: Meta-analysis and test of a process model. Psychol Bull. 2017;143(11):1117–54.
Jørgensen IL, Frederiksen K, Boesen E, et al. An exploratory study of associationsbetween illness perceptions and adjustment and changes after psychosocial rehabilitation in survivors of breast cancer. Acta Oncol. 2009;48(8):1119–27.
Leventhal H, Nerenz DR, Steele DJ. Illness representations and co** with Health threats. In: Baum A, Taylor SE, Singer JE, editors. Handbook of Psychology and Health. Volume IV: Social Psychological Aspects of Health, Erlbaum; 1984. pp. 219–52.
Leventhal H, Phillips LA, Burns E. The common-sense model of self-regulation (CSM): a dynamic framework for understanding illness self-management. J Behav Med. 2016;39:935–46. https://doi.org/10.1007/s10865-016-9782-2.
Traa MJ, De Vries J, Bodenmann G, et al. Dyadic co** and relationship functioning in couples co** with cancer: a systematic review. Br J Health Psychol. 2015;20:85–114. https://doi.org/10.1111/bjhp.12094.
Sun HY, Qin Y, Xu YR, et al. The subject-object interaction model of dualistic co** and mental resilience of cancer patients and their spouses. J Nurs(China). 2022;29:60–4. https://doi.org/10.16460/j.issn1008-9969.2022.06.060.
Zhao J, Zuo F. The development of interpersonal interdependence theory. J Shanghai Norm Univ. 2005;34:119–23.
Li JQ, Zhu BJ, Li MY, et al. The status quo and influencing factors of fear of disease progression in spouses of advanced cancer patients. J Nurs (China). 2019;26:5–9. https://doi.org/10.16460/j.issn1008-9969.2019.14.005.
Broadbent E, Petrie KJ, Main J, et al. The brief illness perception questionnaire. J Psychosom Res. 2006;60:631–7. https://doi.org/10.1016/j.jpsychores.2005.10.020.
Mei YQ, Li HP, Yang YJ, et al. Reliability and validity of simplified version of Chinese version of disease perception questionnaire in female breast cancer patients. J Nurs(China). 2015;22:11–4. https://doi.org/10.16460/j.issn1008-9969.2015.24.011.
Derogatis LR. The psychosocial adjustment to illness scale (PAIS). J Psychosom Res. 1986;30:77–91. https://doi.org/10.1016/0022-3999(86)90069-3.
Yao JJ. A cross-sectional investigation of adaptive level and its predictive factors in cancer patients. Second Military Medical University; 2013.
Kenny DA, Kashy DA, Cook WL. Dyadic Data Analysis. Guilford; 2020.
Marmarosh CL, Kivlighan DM, Bieri K, et al. The insecure psychotherapy base: using client and therapist attachment styles to understand the early alliance. Psychother (Chic). 2014;51:404–12. https://doi.org/10.1037/a0031989.
Chen SZ, Cui H, Zhou RL, et al. Revision and validation of the mindful attention awareness scale (MAAS). Chin J Clin Psychol (China). 2012;20:148–51. https://doi.org/10.16128/j.cnki.1005-3611.2012.02.024.
Zhou J. Study on the correlation between disease perception, health belief and health outcomes in patients with breast cancer after surgery. Yanbian University (China); 2021.
Tian X, Tang L, Yi LJ, et al. Mindfulness affects the level of psychological distress in patients with lung cancer via illness perception and perceived stress: a cross-sectional survey study. Front Psychol. 2022;13:857659. https://doi.org/10.3389/fpsyg.2022.857659.
Van der Ende-van Loon MCM, Nieuwkerk PT, van Stiphout SHC, et al. Barrett esophagus: quality of life and factors associated with illness perception. U Eur Gastroenterol J. 2022;10:721–9. https://doi.org/10.1002/ueg2.12266.
Shim EJ, Lee JW, Min YH. Does depression decrease the moderating effect of self-efficacy in the relationship between illness perception and fear of progression in breast cancer? Psycho-oncology. 2018;27:539–47. https://doi.org/10.1002/pon.4532.
Ugur O, Karadag E, Mert H, et al. Examining the relationship between symptoms watched in lung cancer patients and illness perception. JPMA J Pak Med Assoc. 2022;72:634–8. https://doi.org/10.47391/jpma.0179.
Zhang N, Fielding R, Soong I, et al. Illness perceptions among cancer survivors. Support Care Cancer. 2016;24:1295–304. https://doi.org/10.1007/s00520-015-2914-3.
Galdas PM, Cheater F, Marshall P. Men and health help-seeking behaviour: literature review. J Adv Nurs. 2005;49:616–23. https://doi.org/10.1111/j.1365-2648.2004.03331.x.
Chiu HC, Lin CY, Kuo YL, et al. Resilience among women with breast cancer surviving longer than five years: the relationship with illness perception and body image. Eur J Oncol Nurs. 2023;62:102254. https://doi.org/10.1016/j.ejon.2022.102254.
Karabulutlu EY, Avcı İA, Karayurt Ö, et al. Evaluation of illness perception of women with breast cancer in Turkey. Eur J Breast Health. 2019;15:98–104. https://doi.org/10.5152/ejbh.2019.4317.
Alaa H, Shah SA. Perception of Cancer Risk and its Associated Risk factors among young iraqis living in Baghdad. Asian Pac J Cancer Prev. 2019;20:2339–43. https://doi.org/10.31557/apjcp.2019.20.8.2339.
Shen AM, Qiang WM. Correlation between hope level and psychosocial adjustment of breast cancer patients during chemotherapy. Nurs Res (China). 2017;31:1056–60.
Hu N, Wang A, Chang T. Social support mediates the relationship between illness perception and psychosocial adaptation among young and middle-aged kidney transplant recipients in China. Front Psychol. 2023;14:1062337. https://doi.org/10.3389/fpsyg.2023.1062337.
Lotfi-Tokaldany M, Shahmansouri N, Karimi A. et a l(2019) Association between illness perception and health-related quality of life in patients with preexisting premature coronary artery disease. J Psychosom Res 120:118–123. https://doi.org/10.1016/j.jpsychores.2019.03.001.
Quiles Marcos Y, Terol Cantero MC, Romero Escobar C, et al. Illness perception in eating disorders and psychosocial adaptation. Eur Eat Disord Rev. 2007;15:373–84. https://doi.org/10.1002/erv.793.
Rottmann N, Hansen DG, Hagedoorn M, et al. Depressive symptom trajectories in women affected by breast cancer and their male partners: a nationwide prospective cohort study. J Cancer Surviv. 2016;10:915–26. https://doi.org/10.1007/s11764-016-0538-3.
Segrin C, Badger TA, Sikorskii A, et al. Longitudinal dyadic interdependence in psychological distress among latinas with breast cancer and their caregivers. Support Care Cancer. 2020;28:2735–43. https://doi.org/10.1007/s00520-019-05121-4.
Kayser K, Acquati C, Reese JB, et al. A systematic review of dyadic studies examining relationship quality in couples facing colorectal cancer together. Psycho-oncology. 2018;27:13–21. https://doi.org/10.1002/pon.4339.
Funding
No external funding.
Author information
Authors and Affiliations
Contributions
Yan-feng Wang: Conceptualisation and study design; Data analysis and interpretation; Manuscript writing (original draft). An-kang Liu: Conceptualisation and study design; Data collection; Manuscript editing. **-zhen Dai: Data collection; analysis; and interpretation; Manuscript editing. Ji-** Zhang: Conceptualisation; Data collection; processing; Manuscript editing. Hui-hua Chen: Data interpretation; Manuscript editing. **ao-hao Jiang: Conceptualisation and study design; Data collection; Manuscript editing. Lu Tang: Conceptualisation and study design; Manuscript editing. Yong-yue He: Conceptualisation and study design; Manuscript editing; Conceptualisation and study design. Qiao-hong Yang: Conceptualisation and study design; Data collection; Manuscript editing. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
All participants have signed informed consent in accordance with the ethical principles of the Declaration of Helsinki. The institutional Ethics Committee at the First Affiliated Hospital of **an University approved the study (Ethics number: KY-2023-169).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, Yf., Liu, Ak., Dai, Jz. et al. The effect of illness perception on psychosocial adjustment of patients with breast cancer and their spouses: actor–partner independence model. BMC Psychol 12, 310 (2024). https://doi.org/10.1186/s40359-024-01741-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40359-024-01741-6