Abstract
Background
Dementia [i.e., Alzheimer disease (AD)], the most common neurodegenerative disease, causes profound negative impacts on executive function and quality of life. Available pharmacological treatments often fail to achieve satisfactory outcomes. Noninvasive brain stimulation (NIBS) techniques, which focally modify cortical function and enhance synaptic long-term potentiation, are potentially beneficial for the cognition in patients with AD. The aim of the current network meta-analysis (NMA) was to evaluate the efficacy and safety of different NIBS interventions in patients with AD through NMA.
Methods
Only randomized controlled trials (RCTs) examining NIBS interventions in patients with AD had been included. All NMA procedures were performed under the frequentist model. The primary and secondary outcomes were changes in cognitive function and quality of life, respectively.
Results
Nineteen RCTs (639 participants) were included. The mean treatment and follow-up durations were 5.7 and 10.5 weeks, respectively. The combination of cathodal tDCS of the left dorsolateral prefrontal cortex and anodal tDCS over the right supraorbital region (c-tDCS-F3 + a-tDCS-Fp2) was associated with a significant beneficial effect on cognition compared with sham controls (standardized mean difference=2.43, 95% confidence interval=0.61–4.26, n=12 and 11). It was also associated with the greatest beneficial effect on cognition among all the investigated NIBS approaches. All the methods were well tolerated with regard to the safety profile, as reflected in the rates of adverse events or local discomfort, as well as acceptability, as indicated by dropout rate.
Conclusions
The present findings provide evidence of the benefits of NIBS, especially tDCS, for beneficial effect on cognition in patients with AD. However, because of few studies included, this effect was not replicated yet in the other studies. Therefore, future larger-scale and longer follow-up duration RCTs should be warranted.
Trial registration
PROSPERO CRD42020209516. The current study had been approved by the Institutional Review Board of the Tri-Service General Hospital, National Defense Medical Center (TSGHIRB No. B-109-29).
Similar content being viewed by others
Introduction
Affecting 46.8 million people globally, the dementia [i.e., Alzheimer disease (AD)] is the most common neurodegenerative disease characterized by progressive cognitive decline [1, 2]. In individuals aged between 65 and 95 years, its incidence doubles approximately every 5 years [3]. AD causes profound negative impacts on executive function and quality of life. Patients also experience memory impairment, behavioral disturbance, and insomnia [4]. Therefore, the amelioration of cognitive decline in the early stages of the disease is regarded as essential in AD management. The efficacy of AD medications, most of which are oral, do not provide satisfactory results [5, 6].
The unsatisfactory efficacy of AD leaves room for alternative treatments. Noninvasive brain stimulation (NIBS) interventions, which are based on the theory of alterations in synaptic function and neuroplasticity [7, 8] and target specific brain regions, have attracted increasing scholarly attention. NIBS techniques include repetitive transcranial magnetic stimulation (rTMS) [9] and transcranial electrical stimulation such as transcranial direct current stimulation (tDCS) [10]. According to the frequency applied, rTMS can induce different changes in brain activity. For example, high-frequency rTMS (HF-rTMS) induces higher brain activity, whereas low-frequency rTMS (LF-rTMS) suppresses cerebral cortex activity [11]. Studies have indicated that anodal [12, 13] and cathodal [10] tDCS exert stimulate and suppress activity in the targeted cortices, respectively. However, whether suppression or enhancement associated with the polarity of tDCS remains under debate [14, 15]. In AD management, rTMS or tDCS of specific cortical regions constitute promising NIBS techniques with regard to their enhancing [10] and neuroplasticity-related effects [16], as well as their effects on neurotransmitter modulation [17, 18].
Conventional pairwise meta-analyses have indicated the substantial efficacy of tDCS [19] and rTMS [20, 21] compared with that of sham treatment in improving cognitive function in patients with AD. In 2020, a recent network meta-analysis (NMA) comparing the efficacy of different NIBS techniques in improving cognitive function in patients with mild cognitive impairment (MCI) or AD suggested that rTMS was superior to tDCS and that patients with AD responded better to rTMS and tDCS than those with MCI did [22]. We identified 3 major limitations from this study. First, it did not address the regions that were stimulated in the interventions; for instance, rTMS over the left dorsolateral prefrontal cortex (DLPFC) and over multiple brain regions were considered to be the same technique. Second, heterogeneity risk was increased because patients with MCI were included along with patients with AD. Third, the potentially synergistic effects or priming effect [23] of stimulations over different cortex within the same session were not addressed. Similar limitations are observable in a past pairwise meta-analyses [24]. Specifically, methodological limitations meant that different NIBS interventions were not effectively compared. Conventional pairwise meta-analyses cannot provide information regarding the relative efficacy of interventions that have not been directly compared in head-to-head RCTs, which constitutes an essential indicator of interventions’ therapeutic value. The risk was heterogeneity among studies which was also increased in other meta-analyses that included RCTs of not only patients with AD but also those with MCI [19, 20, 25].
Given this background, an NMA including only patients with AD that addresses variations in the targeted brain regions in NIBS interventions enables the estimation of comparative efficacy or risk and the understanding of the relative merits of different interventions. To the best of our knowledge, no NMAs on this subject have been performed. Therefore, we conducted a systematic review and NMA to compare the efficacy and safety of various central NIBS interventions in cognitive function in patients with AD.
Methods
General aspects
The NMA was performed according to the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement 2020 guideline (eTable 1) [26] and AMSTAR2 (a measurement tool to assess systematic reviews) guideline [27]. The current study had been approval by the Institutional Review Board of the Tri-Service General Hospital, National Defense Medical Center (TSGHIRB No. B-109-29).
Search strategy and selection criteria
The systematic review involved searching the PubMed, Embase, ClinicalKey, Cochrane CENTRAL, ProQuest, ScienceDirect, Web of Science, and ClinicalTrials.gov databases from their inception to September 15, 2020, and final update at November 26, 2020 (the keyword used in each database had been listed in eTable 2). No language restrictions were applied. The reference lists of review articles and pairwise meta-analyses [19,20,21, 24, 25, 28,29,30,31,32,33,34,39]. (3) The initial MMSE scores were significant for determining the time to clinically meaningful decline during longitudinal follow-up [40]. Similarly, the MMSE total score can serve as an index of disease progression and cognitive decline in patients with AD [41]. (4) The MMSE is suitable for evaluating patients with varying severities of AD; by contrast, the ADAS-Cog is recommended only for patients with MMSE scores of ≥14 [42]. Whenever MMSE scores were not available, we have chosen ADAS-Cog scores. Notably, previous RCTs have found that patients with AD receiving sham controls exhibited improvement in cognitive function but returned to baseline in a longer follow-up (2–6 mo) [10, 43]. Therefore, to reduce the risk of these potential time effects, we extracted the data from the “final follow-up assessment.”
Secondary outcome, safety profile, and intervention acceptability
The secondary outcome was the changes in quality of life. The safety profile was calculated using the rate of any adverse event and the rate of any local discomfort, including headache, itching, swelling, or local erythematous changes. Intervention acceptability was calculated using the dropout rate, which was defined as the percentage of patients withdrawing their participation before the end of study period for any reason.
Node definition
Because the central NIBS methods varied widely among the studies, we categorized them into 2 major subgroups: (1) rTMS modalities, namely HF-rTMS (≥5 Hz) and LF-rTMS (<5 Hz), and (2) tDCS modalities, which were particularly categorized according to the anodal or cathodal placement position (e.g., a-tDCS over F3 or c-tDCS over F3). We further categorized the treatment arms on the basis of the stimulation position according to the electroencephalogram brain map. The nomenclature of the node definition was defined according to our previous four NMAs of NIBS studies in other different neuropsychiatric diseases [23, 44,45,46].
Cochrane risk-of-bias tool
Two independent authors (YW Chen and BS Zeng) evaluated the risk of bias (interrater reliability =.85) for each domain using the Cochrane risk-of-bias tool [47]. The studies were further categorized according to overall risk of bias.
Statistical analysis
The NMA was performed using STATA (version 16.0; StataCorp Statistics/Data Analysis, StataCorp LLC, College Station, TX, USA). We estimated the standardized mean difference (SMD) with a 95% confidence intervals (95%CIs) for the continuous variable (i.e., the primary outcome of changes in cognitive function). In the subgroup analysis based on specific cognitive rating scales (i.e., the MMSE and ADAS-Cog), we estimated the mean differences (MDs) with 95%CIs to provide additional clinical information. For the categorical variables (i.e., the safety profile and acceptability), we estimated efficacy using odds ratios and 95%CIs and applied a 0.5 zero-cell correction during the meta-analysis procedure. However, if both the intervention and control arms of a study contained zeroes, we did not apply this correction procedure because of the risk of increasing the bias but rather excluded such studies from the analysis [48, 49]. We used the frequentist model of NMAs to compare the effect sizes of studies with similar interventions. All comparisons were performed using 2-tailed t tests, and differences were considered significant at P < .05. Between-study heterogeneity was evaluated using the tau value, the estimated standard deviation of the effect across the studies.
The meta-analysis procedure was mixed comparisons with direct and indirect comparisons made using generalized linear mixed models [50]. Specifically, indirect comparisons were conducted using transitivity, in which the differences between treatments A and B could be calculated from their comparisons with a third treatment C. To compare multiple treatment arms, we combined the direct and indirect evidence from the included studies [51]. The mvmeta command in STATA software [52] was used in the NMA. The restricted maximum likelihood method was used to evaluate the between-study variance [53].
To provide additional information for clinical application, we calculated the relative ranking probabilities of the treatment effects of all treatments for the target outcomes. In brief, we used the surface under the cumulative ranking curve (SUCRA), which indicates the percentage of the mean rank of each treatment relative to an imaginary intervention that is without uncertainty the optimal one [54].
We evaluated the potential within-network inconsistencies between the direct and indirect evidence by using the loop-specific approach, identifying local inconsistencies through the node-splitting method. The design-by-treatment model was used to evaluate global inconsistencies in the NMA [55]. We evaluated the quality of evidence with the Grading of Recommendations Assessment, Development and Evaluation (GRADE) rating tools described previously [56, 57]. Finally, according to the rationale of a previous NMA study [58], we assessed the effectiveness of the sham interventions to justify our assumption of transitivity. Specifically, we determined cognitive changes following sham tDCS and rTMS using Comprehensive Meta-Analysis software (version 3; Biostat, Englewood, NJ, USA).
Results
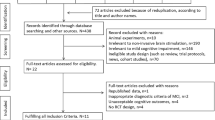
After the initial screening procedure, 88 articles were considered for full-text review (Fig. 1). After 69 were excluded for various reasons (eTable 3), 19 remained for analysis (eTable 4) [2, 9, 10, 43, 59,60,61,62,63,64,65,66,67,68,69,70,71,72,73]. Figure 2 presents the overall geometric distribution of the treatment arms.
Network structure of the changes of cognitive function. Overall structure of the network meta-analysis. The lines between nodes represent direct comparisons in various trials, and the size of each circle is proportional to the number of participants in each specific treatment. The thickness of the lines is proportional to the number of trials connected to the network
Characteristics of the included studies
The mean age of the 639 participants was 72.5 years (range = 65.7–80.5 y; interquartile range [IQR] = 69.0–73.6 y), and women constituted 54.7% (range =10.0–83.3%; IQR = 44.1–65.4%). The mean duration of central NIBS treatment was 5.7 weeks (range = 2–32 wk; IQR = 2–6 wk). The corresponding mean follow-up duration was 10.5 weeks (range = 2–32 wk; IQR = 3.8–13.3 wk). The mean baseline MMSE was 19.1 (range = 14.8–22.5; IQR = 15.9–21.5). The most included RCTs allowed participants to use concomitant medication during the interventions [9, 43, 59,60,61,62,63,64, 67, 68, 70,71,72]. The investigated NIBS approaches were tDCS [10, 43, 60, 63, 67, 69, 72] and rTMS [2, 9, 59, 61, 62, 64,65,66, 68, 70, 71, 73]. All the tDCS treatments applied were 2mA in intensity. Although we planned to consider other NIBS techniques (i.e., TBS), no relevant RCTs on patients with AD receiving such therapies were retrieved.
Primary outcome: changes in cognitive function (based on either MMSE or ADAS-Cog measurement)
The NMA revealed that only the cathodal tDCS of the left DLPFC (F3) and anodal tDCS over the right supraorbital region montage (Fp2; c-tDCS-F3 + a-tDCS-Fp2; SMD = 2.43 [95%CIs = 0.61-4.26]) were associated with significant beneficial effect on cognition compared with sham controls (Table 1, Figs. 2A and 3A). The associations between the NIBS methods and the beneficial effect on cognition were ranked according to the SUCRA. In brief, c-tDCS-F3 + a-tDCS-Fp2 was associated with the greatest benefit, followed by high-frequency rTMS over the bilateral DLPFC (HF-rTMS-F3F4; SMD = 1.12 [95%CIs = −0.24 to 2.49]) and anodal tDCS of the left DLPFC and cathodal tDCS over the right supraorbital region (a-tDCS-F3 + c-tDCS-Fp2; SMD = 1.14 [95%CIs = −0.17 to 2.45]; eTable 6A).
Notably, the sham therapy effect did not significantly differ between the sham rTMS and tDCS therapies (P = .061). However, a significant placebo effect was observed in the sham rTMS group (SMD = 0.171 [95%CIs = 0.009–0.333], P = .038) but not in the sham tDCS group (SMD= −0.124 [95%CIs = −0.386 to 0.138], P = .355; eFigure 1).
Subgroup of primary outcome: changes in cognitive function as measured by the MMSE
Only the HF-rTMS-F3F4 (MD = 6.11 [95%CIs = 2.38–9.83]), c-tDCS-F3 + a-tDCS-Fp2 (MD = 5.55 [95%CIs = 3.72–7.38]), a-tDCS-F3 + c-tDCS-Fp2 (MD = 4.61 [95%CIs = 2.75–6.47]), and anodal tDCS of the left frontotemporal lobe and cathodal tDCS over the right Fp2 region (a-tDCS-F7 + c-tDCS-Fp2; MD = 2.38 [95%CIs = 0.45–4.32]) were associated with significant beneficial effect on cognition (measured by MMSE) compared with sham controls (Table 2, Figs. 2B and 3B). The associations between an NIBS method and the changes of cognitive function (measured by MMSE) were ranked according to the SUCRA. In brief, HF-rTMS-F3F4 was associated with the greatest benefit, followed by c-tDCS-F3 + a-tDCS-Fp2 and a-tDCS-F3 + c-tDCS-Fp2 (eTable 6B).
Subgroup of primary outcome: changes in cognitive function as measured by the ADAS-Cog
The NMA revealed that only the high-frequency rTMS over the left DLPFC (HF-rTMS-F3; MD = −3.40 [95%CIs = −6.57 to −0.23]) and high-frequency rTMS multifocal stimulation (HF-rTMS-Mx; MD = −3.06 [95%CIs = −4.55 to −1.57]) were associated with significant beneficial effect on cognition (measured by ADAS-Cog) compared with sham controls (Table 3, Figs. 2C and 3C). The associations between NIBS interventions and benefit of cognitive decline (measured by ADAS-Cog) were ranked according to the SUCRA. In brief, HF-rTMS-F3F4 was associated with the greatest benefit (MD = −4.00 [95%CIs = −8.73 to 0.73]) compared with sham controls, followed by HF-rTMS-F3 and HF-rTMS-Mx (eTable 6C).
Secondary outcome: changes in quality of life
None of the NIBS methods were associated with differences in changes of quality of life compared with sham controls (eTable 5A, eTable 6D, eFigure 2A, and eFigure 3A).
Safety profile: any adverse event rate
The NMA revealed that none of the NIBS methods were associated with different rates of any adverse events compared with sham controls (eTable 5B, eTable 6E, eFigure 2B, and eFigure 3B).
Safety profile: any local discomfort rate
No differences between the NIBS interventions and sham controls with regard to local discomfort rate were observed (eTable 5C, eTable 6F, eFigure 2C, and eFigure 3C).
Intervention acceptability: dropout rate
No differences in dropout rate between the NIBS interventions and sham controls were noted (eTable 5D, eTable 6G, eFigure 2D, and eFigure 3D).
Risk of bias, publication bias, inconsistency, and GRADE ratings
Overall, 74.4% (99/133 items), 24.1% (32/133 items), and 1.5% (2/133 items) of the included studies had a low, unclear, and high risk of bias, respectively, to which unclear reporting of the allocation procedure was the major contributor of unclear risk of bias (eFigure 4A-B). Funnel plots of publication bias revealed general symmetry and Egger’s test results indicated no significant publication bias among the included articles (eFigure 5A-N). Overall, no inconsistencies in the NMA were demonstrated in either local inconsistencies, as assessed using the loop-specific approach and node-splitting method, or global inconsistencies, as determined using the design-by-treatment method, with the exception of significant inconsistency in the primary outcome (design-by-treatment method: P = .0125) (eTable 7-8). However, this inconsistency disappeared in the subgroup of the primary outcome: changes of cognitive function measured by MMSE or ADAS-Cog (design-by-treatment method: P = .7001 and .9044, respectively). The results of GRADE evaluation are listed in eTable 9. In brief, the overall quality of evidence of the overall NMA, direct evidence, and indirect evidence were low to medium.
Discussion
To the best of our knowledge, this is the first comprehensive NMA investigating the efficacy and safety of NIBS interventions in patients with AD. As mentioned, c-tDCS-F3 + a-tDCS-Fp2 was associated with significant beneficial effect on cognition compared with sham controls. When focusing on specific cognition-rating scales, HF-rTMS-F3F4, c-tDCS-F3 + a-tDCS-Fp2, and a-tDCS-F3 + c-tDCS-Fp2 were determined to be associated with significant beneficial effect on cognition (measured by MMSE) compared with sham controls. Only HF-rTMS-F3 and HF-rTMS-Mx were associated with significant beneficial effect on cognition (measured by ADAS-Cog) compared with sham controls. Notably, a study reported significant placebo effects in sham rTMS therapy [74]. In addition, all the NIBS methods were well tolerated with regard to safety profile, as reflected in the rates of adverse events or local discomfort, as well as acceptability, as indicated by dropout rate.
The first main finding of this study was that the c-tDCS-F3 + a-tDCS-Fp2 was associated with a significant beneficial effect on cognition compared with sham controls and was also associated with the greatest beneficial effect on cognition among all the NIBS methods. The role of tDCS in changes of cognitive function in patients with AD is believed to be associated with the cognitive-enhancing effect of tDCS targeting the DLPFC, an area widely connected to cortical/subcortical regions and associated with executive control and memory [75]. However, the effect of the direction of tDCS currents on the specific cortical region is under debate. Although cathodal tDCS is generally believed to be associated with inhibitory effects on the targeted cortex, tDCS administered at higher intensity (i.e., 2mA) appears to result in reversal to excitatory effects [15]. Studies have indicated that these cortical effects outlast the original stimulation due to synaptic long-term potentiation [10, 76]. Another hypothetical mechanism regarding the cognitive benefits of tDCS involves the concerns about the activation of the cognitive reserve pool through acetylcholine and dopamine modulation [17, 18]. In addition, the beneficial effect of tDCS on cognitive function might be derived not only from cortical targeting but also from the effect of currents spreading to nearby cortical regions [77]. Taken together, the potential beneficial effect of c-tDCS-F3 + a-tDCS-Fp2 on the beneficial effect on cognition, if any, may involve different effects on multiple cortical regions. Notably, the finding of a beneficial cognitive effect of c-tDCS-F3 + a-tDCS-Fp2 was mainly drawn from a single study using small sample sizes (n = 12 and 11) [10]. In addition, its confidence interval was relatively wide (i.e., 95%CIs = 0.61–4.26). Therefore, it should be interpreted with caution, and future large-scale RCTs are warranted to provide more evidence.
Significant inconsistency in the primary outcome was noted overall (design-by-treatment method: P = .0125). However, this inconsistency disappeared in the subgroup of the primary outcome: changes of cognitive function measured by MMSE or ADAS-Cog (design-by-treatment method: P = .7001 and .9044, respectively). When we reexamined the evidence of the individual treatment arm, we found that the potential beneficial effect of a-tDCS-F3 + c-tDCS-Fp2 was also demonstrated in the subgroup analysis of changes of cognitive decline as measured by MMSE. In the overall NMA results, a-tDCS-F3 + c-tDCS-Fp2 did not achieve significant outcomes, in contrast to the fact that anodal tDCS targeted to the left DLPFC and left temporal cortex, among other cortices, has been reported to enhance executive function and the memory process [12, 13]. The nonsignificant result may be ascribable to the relatively shorter follow-up duration in one RCT, in which the a-tDCS-F3 + c-tDCS-Fp2 and sham control groups did not differ significantly in cognitive changes at a 3-week follow-up [72]. RCTs have shown that patients with AD receiving sham tDCS exhibited improvement in cognitive function but returned to baseline in a longer follow-up (i.e., 2-6 mo) [10, 43]. In the present study, we tried to reduce the potential impacts of time by extracting data at the final follow-up. Nevertheless, the relatively short follow-up duration (mean follow-up duration was 10.5 wks) may have confounded with time. Therefore, future RCTs are encouraged to use longer follow-up duration (i.e., at least 2–6 mo).
In the present NMA, the tDCS studies had relatively consistent findings. By contrast, those of the rTMS studies were inconsistent. This may be partially attributed to bias in the rTMS studies, such as the significant placebo effect observed in sham rTMS (SMD = 0.171, 95%CIs = 0.009-0.333, P = .038, eFigure 1). The placebo effect of NIBS interventions on cognitive outcomes may be associated with several mechanisms. First, because mimicking active rTMS is challenging, several modifications have been developed for rTMS, such as the application of peripheral auditory clicking sounds for intersensory facilitation [78]. The potential placebo effect may also result from the introduction of the intervention itself, the expectation of outcomes, optimism, and emotional goal-seeking [79]. Therefore, as suggested in one study, the alleviation of negative emotion (i.e., depressive mood) in older adults and the presence or company of study staff members may contribute to cognitive improvement [70]. To reduce the potential bias from the placebo effect, the development of adequate rTMS sham control interventions should be urgent. Finally, the electromagnetic field of standard coils decays rapidly, and they can only penetrate to a depth of 2–3 cm [80], which may be insufficient to reach the outer brain layers of older adults and patients with brain atrophy, both characteristics of patients with AD. Therefore, the potential of alternative rTMS techniques that can reach deeper structures (e.g., deep TMS) should be explored.
Limitations
This study has several limitations. First, this NMA may have been underpowered because of the heterogeneity of the participants (e.g., with regard to comorbidities, effects of concomitant medications on cognition, baseline AD severity, differences in AD onset age, different methods to define the stimulation target, different NIBS stimulation protocols, and follow-up duration). Second, although all the RCTs included a sham control in their study design, they may not have been adequately blinded because of differences in the interventions used. The placebo effect by the sham control, especially that of sham rTMS (SMD = 0.171, 95%CIs = 0.009–0.333, P = .038, eFigure 1), may also have imposed bias with regard to patients with AD [70]. Third, given the relatively small number of RCTs (and by extension patients) included, the main present findings should perhaps be conservatively applied in clinical practice. Specifically, the evidence of potentially beneficial effect of c-tDCS-F3 + a-tDCS-Fp2 on cognition in patients with AD was mainly derived from one RCT [10], which evaluated patients with mild-to-moderate AD (MMSE score between 11 and 23) with a 10-week follow-up. Therefore, the corresponding finding in the present study should be limited to patients with the same severity of AD that were followed up for at least 10 weeks. Fourth, whether tDCS can target specific cortices remains under debate [77]. Therefore, whether the potential beneficial effect of tDCS resulted from enhancement on the specific cortex remains unclear. Fifth, although most of the included RCTs provided comparisons between NIBS and sham control interventions, few provided comparisons between different NIBS interventions [2, 10, 66]. Therefore, the geometric structure of the current NMA was relatively weak (Fig. 2A–C). Sixth, although we intended to also include RCTs of deep TMS and TBS by adding these modalities in our search keywords, there was a lack of such RCTs available at present time. Finally, significant inconsistency was detected in the primary outcome overall. Although this inconsistency disappeared after subgroup analysis, clinicians should remain cautious in practical applications of those findings.
Conclusion
In summary, c-tDCS-F3 + a-tDCS-Fp2 was associated with significant beneficial effect on cognition compared with sham control. Moreover, it was associated with the greatest benefit of cognitive decline among all the NIBS interventions. In addition, all of the methods were suggested to be well tolerated with regard to safety profile, as reflected in the rates of adverse events or local discomfort, as well as acceptability, as indicated by dropout rate. The significant placebo effect in sham rTMS indicates that adequate sham control interventions in rTMS therapy should be urgently developed. However, because the treatment duration of the included studies was relatively short (mean=5.7 weeks, IQR = 2–6 weeks), future RCTs of tDCS are encouraged to use longer treatment duration to obtain more evidence of the beneficial effect by long-term NIBS interventions.
Availability of data and materials
All the data and materials of the current study were available upon reasonable request.
Abbreviations
- AD:
-
Alzheimer’s disease
- ADAS-Cog:
-
Alzheimer’s disease assessment scale-cognitive subscale
- a-tDCS-F3 + c-tDCS-F4:
-
Anodal tDCS of the left DLPFC and cathodal over the right DLPFC
- a-tDCS-F3 + c-tDCS-Fp2:
-
Anodal tDCS of the left DLPFC and cathodal over the right supraorbital region
- a-tDCS-F3 + c-tDCS-RtLb:
-
Anodal tDCS of the left DLPFC and cathodal over the right deltoid muscle
- a-tDCS-F7 + c-tDCS-Fp2:
-
Anodal tDCS of the left frontotemporal lobe and cathodal over the right frontal lobe
- a-tDCS-T3 + c-tDCS-Fp2:
-
Anodal tDCS of the left lateral temporal lobe and cathodal over the right frontal lobe
- a-tDCS-T3 + c-tDCS-RtLb:
-
Anodal tDCS of the left lateral temporal lobe and cathodal over the right upper limb
- a-tDCS-T3P3/T4P4 + c-tDCS-LtLb:
-
Anodal tDCS 2mA alternatively over the bilateral temporo-parietal lobe (T3-P3 or T4-P4) and cathodal over left arm deltoid muscle
- CDR:
-
Clinical Dementia Rating
- CI:
-
Confidence interval
- c-tDCS-F3 + a-tDCS-Fp2:
-
Cathodal tDCS of the left DLPFC and anodal over the right supraorbital region
- DLPFC:
-
Dorsolateral prefrontal cortex
- dTMS:
-
Deep TMS
- HF-rTMS:
-
High-frequency rTMS
- HF-rTMS-F3:
-
High-frequency rTMS over left DLPFC
- HF-rTMS-F3F4:
-
High-frequency rTMS over bilateral DLPFC
- HF-rTMS-F3T3:
-
High-frequency rTMS over left DLPFC and left lateral temporal lobe
- HF-rTMS-F4:
-
High-frequency rTMS over right DLPFC
- HF-rTMS-Mx:
-
High-frequency rTMS multifocal stimulation
- IQR:
-
Interquartile range
- LF-rTMS:
-
Low-frequency rTMS
- LF-rTMS-F3F4:
-
Low-frequency rTMS over bilateral DLPFC
- MD:
-
Mean difference
- MMSE:
-
Mini-Mental State Examination
- NIBS:
-
Noninvasive brain stimulation
- NMA:
-
Network meta-analysis
- OR:
-
Odds ratio
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RCT:
-
Randomized controlled trial
- rTMS:
-
Repetitive transcranial magnetic stimulation
- Sham:
-
Sham control
- SMD:
-
Standardized mean difference
- SUCRA:
-
Surface under the cumulative ranking curve
- TBS:
-
Theta-burst stimulation
- tDCS:
-
Transcranial direct current stimulation
References
Sosa-Ortiz AL, Acosta-Castillo I, Prince MJ. Epidemiology of dementias and Alzheimer’s disease. Arch Med Res. 2012;43(8):600–8.
Alcala-Lozano R, Morelos-Santana E, Cortes-Sotres JF, Garza-Villarreal EA, Sosa-Ortiz AL, Gonzalez-Olvera JJ. Similar clinical improvement and maintenance after rTMS at 5 Hz using a simple vs. complex protocol in Alzheimer's disease. Brain Stimul. 2018;11(3):625–7.
Qiu C, Kivipelto M, von Strauss E. Epidemiology of Alzheimer’s disease: occurrence, determinants, and strategies toward intervention. Dialogues Clin Neurosci. 2009;11(2):111–28.
Scheltens P, Blennow K, Breteler MM, de Strooper B, Frisoni GB, Salloway S, et al. Alzheimer’s disease. Lancet. 2016;388(10043):505–17.
Briggs R, Kennelly SP, O'Neill D. Drug treatments in Alzheimer’s disease. Clin Med (Lond). 2016;16(3):247–53.
Ballard C, Gauthier S, Corbett A, Brayne C, Aarsland D, Jones E. Alzheimer’s disease. Lancet. 2011;377(9770):1019–31.
Rossini PM, Burke D, Chen R, Cohen LG, Daskalakis Z, Di Iorio R, et al. Non-invasive electrical and magnetic stimulation of the brain, spinal cord, roots and peripheral nerves: basic principles and procedures for routine clinical and research application. An updated report from an I.F.C.N. Committee. Clin Neurophysiol. 2015;126(6):1071–107.
Koch G, Di Lorenzo F, Bonni S, Ponzo V, Caltagirone C, Martorana A. Impaired LTP- but not LTD-like cortical plasticity in Alzheimer’s disease patients. J Alzheimers Dis. 2012;31(3):593–9.
Cotelli M, Calabria M, Manenti R, Rosini S, Zanetti O, Cappa SF, et al. Improved language performance in Alzheimer disease following brain stimulation. J Neurol Neurosurg Psychiatry. 2011;82(7):794–7.
Khedr EM, Gamal NF, El-Fetoh NA, Khalifa H, Ahmed EM, Ali AM, et al. A double-blind randomized clinical trial on the efficacy of cortical direct current stimulation for the treatment of Alzheimer’s disease. Front Aging Neurosci. 2014;6:275.
Milev RV, Giacobbe P, Kennedy SH, Blumberger DM, Daskalakis ZJ, Downar J, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 Clinical Guidelines for the Management of Adults with Major Depressive Disorder: Section 4. Neurostimulation Treatments. Can J Psychiatry Revue canadienne de psychiatrie. 2016;61(9):561–75.
Boggio PS, Khoury LP, Martins DC, Martins OE, de Macedo EC, Fregni F. Temporal cortex direct current stimulation enhances performance on a visual recognition memory task in Alzheimer disease. J Neurol Neurosurg Psychiatry. 2009;80(4):444–7.
Ferrucci R, Mameli F, Guidi I, Mrakic-Sposta S, Vergari M, Marceglia S, et al. Transcranial direct current stimulation improves recognition memory in Alzheimer disease. Neurology. 2008;71(7):493–8.
Horvath JC, Carter O, Forte JD. Transcranial direct current stimulation: five important issues we aren’t discussing (but probably should be). Front Syst Neurosci. 2014;8:2.
Batsikadze G, Moliadze V, Paulus W, Kuo MF, Nitsche MA. Partially non-linear stimulation intensity-dependent effects of direct current stimulation on motor cortex excitability in humans. J Physiol. 2013;591(7):1987–2000.
Cooke SF, Bliss TV. Plasticity in the human central nervous system. Brain. 2006;129(Pt 7):1659–73.
Kuo MF, Grosch J, Fregni F, Paulus W, Nitsche MA. Focusing effect of acetylcholine on neuroplasticity in the human motor cortex. J Neurosci. 2007;27(52):14442–7.
Monte-Silva K, Kuo MF, Thirugnanasambandam N, Liebetanz D, Paulus W, Nitsche MA. Dose-dependent inverted U-shaped effect of dopamine (D2-like) receptor activation on focal and nonfocal plasticity in humans. J Neurosci. 2009;29(19):6124–31.
Cruz Gonzalez P, Fong KNK, Chung RCK, Ting KH, Law LLF, Brown T. Can transcranial direct-current stimulation alone or combined with cognitive training be used as a clinical intervention to improve cognitive functioning in persons with mild cognitive impairment and dementia? A systematic review and meta-analysis. Front Hum Neurosci. 2018;12:416.
Chou YH, Ton That V, Sundman M. A systematic review and meta-analysis of rTMS effects on cognitive enhancement in mild cognitive impairment and Alzheimer’s disease. Neurobiol Aging. 2020;86:1–10.
Liao X, Li G, Wang A, Liu T, Feng S, Guo Z, et al. Repetitive transcranial magnetic stimulation as an alternative therapy for cognitive impairment in Alzheimer’s disease: a meta-analysis. J Alzheimers Dis. 2015;48(2):463–72.
Chu CS, Li CT, Brunoni AR, Yang FC, Tseng PT, Tu YK, et al. Cognitive effects and acceptability of non-invasive brain stimulation on Alzheimer's disease and mild cognitive impairment: a component network meta-analysis. J Neurol Neurosurg Psychiatry. 2021;92(2):195–203.
Chen JJ, Zeng BS, Wu CN, Stubbs B, Carvalho AF, Brunoni AR, et al. Association of central noninvasive brain stimulation interventions with efficacy and safety in tinnitus management: a meta-analysis. JAMA Otolaryngol Head Neck Surg. 2020;146(9):801–9.
Vacas SM, Stella F, Loureiro JC. Simoes do Couto F, Oliveira-Maia AJ, Forlenza OV: Noninvasive brain stimulation for behavioural and psychological symptoms of dementia: a systematic review and meta-analysis. Int J Geriatr Psychiatry. 2019;34(9):1336–45.
Xu Y, Qiu Z, Zhu J, Liu J, Wu J, Tao J, et al. The modulation effect of non-invasive brain stimulation on cognitive function in patients with mild cognitive impairment: a systematic review and meta-analysis of randomized controlled trials. BMC Neurosci. 2019;20(1):2.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
Wang X, Mao Z, Yu X. The role of noninvasive brain stimulation for behavioral and psychological symptoms of dementia: a systematic review and meta-analysis. Neurol Sci. 2020;41(5):1063–74.
Wang X, Mao Z, Ling Z, Yu X. Repetitive transcranial magnetic stimulation for cognitive impairment in Alzheimer’s disease: a meta-analysis of randomized controlled trials. J Neurol. 2020;267(3):791–801.
Lin Y, Jiang WJ, Shan PY, Lu M, Wang T, Li RH, et al. The role of repetitive transcranial magnetic stimulation (rTMS) in the treatment of cognitive impairment in patients with Alzheimer's disease: a systematic review and meta-analysis. J Neurol Sci. 2019;398:184–91.
Dong X, Yan L, Huang L, Guan X, Dong C, Tao H, et al. Repetitive transcranial magnetic stimulation for the treatment of Alzheimer’s disease: a systematic review and meta-analysis of randomized controlled trials. PloS One. 2018;13(10):e0205704.
May BH, Feng M, Hyde AJ, Hugel H, Chang SY, Dong L, et al. Comparisons between traditional medicines and pharmacotherapies for Alzheimer disease: a systematic review and meta-analysis of cognitive outcomes. Int J Geriatr Psychiatry. 2018;33(3):449–58.
Holczer A, Nemeth VL, Vekony T, Vecsei L, Klivenyi P, Must A. Non-invasive brain stimulation in Alzheimer’s disease and mild cognitive impairment-a state-of-the-art review on methodological characteristics and stimulation parameters. Front Hum Neurosci. 2020;14:179.
Rajji TK. Transcranial magnetic and electrical stimulation in Alzheimer’s disease and mild cognitive impairment: A review of randomized controlled trials. Clin Pharmacol Ther. 2019;106(4):776–80.
Cai M, Guo Z, **ng G, Peng H, Zhou L, Chen H, et al. Transcranial direct current stimulation improves cognitive function in mild to moderate Alzheimer disease: a meta-analysis. Alzheimer Dis Associated Disord. 2019;33(2):170–8.
Iimori T, Nakajima S, Miyazaki T, Tarumi R, Ogyu K, Wada M, et al. Effectiveness of the prefrontal repetitive transcranial magnetic stimulation on cognitive profiles in depression, schizophrenia, and Alzheimer’s disease: a systematic review. Progress Neuro-Psychopharmacol Biol Psychiatry. 2019;88:31–40.
Gonsalvez I, Baror R, Fried P, Santarnecchi E, Pascual-Leone A. Therapeutic noninvasive brain stimulation in Alzheimer’s disease. Curr Alzheimer Res. 2017;14(4):362–76.
Wlodarczyk JH, Brodaty H, Hawthorne G. The relationship between quality of life, Mini-Mental State Examination, and the Instrumental Activities of Daily Living in patients with Alzheimer’s disease. Arch Gerontol Geriatr. 2004;39(1):25–33.
Perneczky R, Wagenpfeil S, Komossa K, Grimmer T, Diehl J, Kurz A. Map** scores onto stages: mini-mental state examination and clinical dementia rating. Am J Geriatr Psychiatry. 2006;14(2):139–44.
Doody RS, Massman P, Dunn JK. A method for estimating progression rates in Alzheimer disease. Arch Neurol. 2001;58(3):449–54.
Henneges C, Reed C, Chen YF, Dell'Agnello G, Lebrec J. Describing the sequence of cognitive decline in Alzheimer’s disease patients: results from an observational study. J Alzheimers Dis. 2016;52(3):1065–80.
Mohs RC, Knopman D, Petersen RC, Ferris SH, Ernesto C, Grundman M, et al. Development of cognitive instruments for use in clinical trials of antidementia drugs: additions to the Alzheimer’s Disease Assessment Scale that broaden its scope. The Alzheimer's Disease Cooperative Study. Alzheimer Dis Associated Disord. 1997;11(Suppl 2):S13–21.
Cotelli M, Manenti R, Brambilla M, Petesi M, Rosini S, Ferrari C, et al. Anodal tDCS during face-name associations memory training in Alzheimer’s patients. Front Aging Neurosci. 2014;6:38.
Cheng YC, Zeng BY, Hung CM, Su KP, Wu YC, Tu YK, et al. Effectiveness and acceptability of noninvasive brain and nerve stimulation techniques for migraine prophylaxis: a network meta-analysis of randomized controlled trials. J Headache Pain. 2022;23(1):28.
Tseng PT, Jeng JS, Zeng BS, Stubbs B, Carvalho AF, Brunoni AR, et al. Efficacy of non-invasive brain stimulation interventions in reducing smoking frequency in patients with nicotine dependence: a systematic review and network meta-analysis of randomized controlled trials. Addiction. 2022;117(7):1830-42.
Zeng BY, Zeng BS, Chen YW, Hung CM, Sun CK, Cheng YS, et al. Efficacy and acceptability of noninvasive brain stimulation interventions for weight reduction in obesity: a pilot network meta-analysis. Int J Obes (Lond). 2021;45(8):1705-16.
Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2: The Cochrane Collaboration; 2009.
Brockhaus AC, Bender R, Skipka G. The Peto odds ratio viewed as a new effect measure. Stat Med. 2014;33(28):4861–74.
Cheng J, Pullenayegum E, Marshall JK, Iorio A, Thabane L. Impact of including or excluding both-armed zero-event studies on using standard meta-analysis methods for rare event outcome: a simulation study. BMJ Open. 2016;6(8):e010983.
Tu YK. Use of generalized linear mixed models for network meta-analysis. Med Decis Mak. 2014;34(7):911–8.
Lu G, Ades AE. Combination of direct and indirect evidence in mixed treatment comparisons. Stat Med. 2004;23(20):3105–24.
White IR. Network meta-analysis. Stata J. 2015;15:951–85.
Kontopantelis E, Springate DA, Reeves D. A re-analysis of the Cochrane Library data: the dangers of unobserved heterogeneity in meta-analyses. PloS One. 2013;8(7):e69930.
Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. 2011;64(2):163–71.
Higgins JP, Del Giovane C, Chaimani A, Caldwell DM, Salanti G. Evaluating the quality of evidence from a network meta-analysis. Value Health. 2014;17(7):A324.
Cipriani A, Furukawa TA, Salanti G, Chaimani A, Atkinson LZ, Ogawa Y, et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. Lancet. 2018;391(10128):1357–66.
Puhan MA, Schunemann HJ, Murad MH, Li T, Brignardello-Petersen R, Singh JA, et al. A GRADE Working Group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ. 2014;349:g5630.
Mutz J, Vipulananthan V, Carter B, Hurlemann R, Fu CHY, Young AH. Comparative efficacy and acceptability of non-surgical brain stimulation for the acute treatment of major depressive episodes in adults: systematic review and network meta-analysis. BMJ. 2019;364:l1079.
Brem AK, Di Iorio R, Fried PJ, Oliveira-Maia AJ, Marra C, Profice P, et al. Corticomotor plasticity predicts clinical efficacy of combined neuromodulation and cognitive training in Alzheimer’s disease. Front Aging Neurosci. 2020;12:200.
Gangemi A, Colombo B, Fabio RA. Effects of short- and long-term neurostimulation (tDCS) on Alzheimer’s disease patients: two randomized studies. Aging Clin Exp Res. 2021;33(2):383-90.
Sabbagh M, Sadowsky C, Tousi B, Agronin ME, Alva G, Armon C, et al. Effects of a combined transcranial magnetic stimulation (TMS) and cognitive training intervention in patients with Alzheimer’s disease. Alzheimers Dement. 2020;16(4):641–50.
Zhang F, Qin Y, **e L, Zheng C, Huang X, Zhang M. High-frequency repetitive transcranial magnetic stimulation combined with cognitive training improves cognitive function and cortical metabolic ratios in Alzheimer’s disease. J Neural Transm. 2019;126(8):1081–94.
Im JJ, Jeong H, Bikson M, Woods AJ, Unal G, Oh JK, et al. Effects of 6-month at-home transcranial direct current stimulation on cognition and cerebral glucose metabolism in Alzheimer’s disease. Brain Stimul. 2019;12(5):1222–8.
Wu Y, Xu W, Liu X, Xu Q, Tang L, Wu S. Adjunctive treatment with high frequency repetitive transcranial magnetic stimulation for the behavioral and psychological symptoms of patients with Alzheimer’s disease: a randomized, double-blind, sham-controlled study. Shanghai Arch Psychiatry. 2015;27(5):280–8.
Rabey JM, Dobronevsky E, Aichenbaum S, Gonen O, Marton RG, Khaigrekht M. Repetitive transcranial magnetic stimulation combined with cognitive training is a safe and effective modality for the treatment of Alzheimer’s disease: a randomized, double-blind study. J Neural Transm. 2013;120(5):813–9.
Ahmed MA, Darwish ES, Khedr EM, El Serogy YM, Ali AM. Effects of low versus high frequencies of repetitive transcranial magnetic stimulation on cognitive function and cortical excitability in Alzheimer’s dementia. J Neurol. 2012;259(1):83–92.
Khedr EM, Salama RH, Abdel Hameed M, Abo Elfetoh N, Seif P. Therapeutic role of transcranial direct current stimulation in Alzheimer disease patients: double-blind, placebo-controlled clinical trial. Neurorehabil Neural Repair. 2019;33(5):384–94.
Zhao J, Li Z, Cong Y, Zhang J, Tan M, Zhang H, et al. Repetitive transcranial magnetic stimulation improves cognitive function of Alzheimer's disease patients. Oncotarget. 2017;8(20):33864–71.
Bystad M, Gronli O, Rasmussen ID, Gundersen N, Nordvang L, Wang-Iversen H, et al. Transcranial direct current stimulation as a memory enhancer in patients with Alzheimer's disease: a randomized, placebo-controlled trial. Alzheimers Res Ther. 2016;8(1):13.
Lee J, Choi BH, Oh E, Sohn EH, Lee AY. Treatment of Alzheimer’s disease with repetitive transcranial magnetic stimulation combined with cognitive training: a prospective, randomized, double-blind, placebo-controlled study. J Clin Neurol. 2016;12(1):57–64.
Rutherford G, Lithgow B, Moussavi Z. Short and long-term effects of rTMS treatment on Alzheimer’s disease at different stages: a pilot study. J Exp Neurosci. 2015;9:43–51.
Suemoto CK, Apolinario D, Nakamura-Palacios EM, Lopes L, Leite RE, Sales MC, et al. Effects of a non-focal plasticity protocol on apathy in moderate Alzheimer's disease: a randomized, double-blind, sham-controlled trial. Brain Stimul. 2014;7(2):308–13.
Padala PR, Boozer EM, Lensing SY, Parkes CM, Hunter CR, Dennis RA, et al. Neuromodulation for apathy in Alzheimer’s disease: a double-blind, randomized, sham-controlled pilot study. J Alzheimers Dis. 2020;77(4):1483-93.
Borrione L, Bellini H, Razza LB, Avila AG, Baeken C, Brem AK, et al. Precision non-implantable neuromodulation therapies: a perspective for the depressed brain. Braz J Psychiatry. 2020;42(4):403–19.
Frith C, Dolan R. The role of the prefrontal cortex in higher cognitive functions. Brain Res Cogn Brain Res. 1996;5(1-2):175–81.
Karim AA, Kammer T, Lotze M, Nitsche MA, Godde B, Hinterberger T, et al. Effects of TMS and tDCS on the physiological Regulation of cortical excitability in a Brain-Computer Interface. Biomed Eng. 2004;49:55–7.
Yun K, Song IU, Chung YA. Changes in cerebral glucose metabolism after 3 weeks of noninvasive electrical stimulation of mild cognitive impairment patients. Alzheimers Res Ther. 2016;8(1):49.
Terao Y, Ugawa Y, Suzuki M, Sakai K, Hanajima R, Gemba-Shimizu K, et al. Shortening of simple reaction time by peripheral electrical and submotor-threshold magnetic cortical stimulation. Exp Brain Res. 1997;115(3):541–5.
Horing B, Weimer K, Muth ER, Enck P. Prediction of placebo responses: a systematic review of the literature. Front Psychol. 2014;5:1079.
Brunoni AR, Sampaio-Junior B, Moffa AH, Aparicio LV, Gordon P, Klein I, et al. Noninvasive brain stimulation in psychiatric disorders: a primer. Braz J Psychiatry. 2019;41(1):70–81.
Acknowledgements
**-Tao Tseng and Yen-Wen Chen both had full access to all the data in the study, conducted the data analysis, and took responsibility for the integrity of the data, data analysis, and the accuracy of the data analysis. This manuscript was edited by Wallace Academic Editing.
Funding
There was no any funding to the current work. This paper presents independent research. The views expressed in this publication are those of the authors and not necessarily those of the acknowledged institutions. The authors of this work were supported by the following grants: Brendon Stubbs is supported by a Clinical Lectureship (ICA-CL-2017-03-001) jointly funded by Health Education England (HEE) and the National Institute for Health Research (NIHR). Brendon Stubbs is partly funded by the NIHR Biomedical Research Centre at South London and Maudsley NHS Foundation Trust. Brendon Stubbs is also supported by the Maudsley Charity, King’s College London, and the NIHR South London Collaboration for Leadership in Applied Health Research and Care (CLAHRC) funding. This paper presents independent research. The views expressed in this publication are those of the authors and not necessarily those of the acknowledged institutions. The work of Kuan-Pin Su is supported by the following grants: MOST 106-2314-B-039-027-MY3, 108-2320-B-039-048, 108-2813-C-039-133-B, and 108-2314-B-039-016 from the Ministry of Science and Technology, Taiwan; NHRI-EX108-10528NI from the National Health Research Institutes, Taiwan; MYRG2018-00242-ICMS from University of Macau, China; CMRC-CMA-3 from Higher Education Sprout Project by the Ministry of Education (MOE), Taiwan; CMU108-SR-106 from the China Medical University, Taichung, Taiwan; and CMU104-S-16-01, CMU103-BC-4-1, CRS-108-048, DMR-108-216, DMR-109-102, DMR-109-244, DMR-HHC-109-11, and DMR-HCC-109-12 from the China Medical University Hospital, Taichung, Taiwan. The work by Pao-Yen Lin is supported by the following grants: MOST 106-2314-B-182A-085-MY2 from the Ministry of Science and Technology, Taiwan, and CMRPG8F1371, CMRPG8E1061F from Kaohsiung Chang Gung Memorial Hospital, Taiwan. The work of Cheng-Ta Li was supported by the following grants: the Ministry of Science and Technology (MOST 108-2321-B-075-004-MY2; 111-2314-B-075-085 -MY3), and the Brain Research Center (108BRC-B502) of National Yang-Ming Chiao-Tung University from The Featured Areas Research Center Program within the framework of the Higher Education Sprout Project by the Ministry of Education (MOE) in Taiwan. The work of Yu-Kang Tu was supported by a grant from the Ministry of Science and Technology, Taiwan (grant no: 106-2314-B-002 -098 -MY3). None of the above funders play any role in the current work.
Author information
Authors and Affiliations
Contributions
P-TT, Y-WC, B-YZ, B-SZ, and C-MH, who contributed equally as first authors, took the whole responsibility of literature search, data extraction, data analysis, and manuscript drafting. C-KS, Y-SC, BS, AFC, ARB, K-PS, Y-KT, Y-CW, T-YC, P-YL, C-SL, C-WH, C-SC, and M-WS all major contributed to the study design, concept formation, and manuscript revision. C-TL, who contributed as corresponding author, took the whole responsibility of manuscript revision, collection of all data from the authors, and manuscript submission.
The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Institutional Review Board of the Tri-Service General Hospital has confirmed that no ethical approval is required (TSGHIRB: B-109-29). The current study did not directly involve individual participant so that we did not have the chance to approach individual participant or explore individual participant’s information. Therefore, it would be impossible to obtain consent to participate in the current study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: eTable 1.
PRISMA 2020 checklist of the current network meta-analysis. eTable 2. Keyword used in each database and search results. eTable 3. Excluded studies and reason. eTable 4. Characteristics of the included studies. eTable 5. A League table of the changes of quality of life. B: League table of the rate of any adverse event. C: League table of the rate of local discomfort. D:League table of the drop-out rate. eTable 6. A SUCRA of the changes of cognition function-overall. B: SUCRA of the changes of cognition function: measured with MMSE. C: SUCRA of the changes of cognition function: measured with ADAS-Cog. D: SUCRA of the changes of quality of life. E: SUCRA of the rate of any adverse event. F: SUCRA of the rate of local discomfort. G: SUCRA of the drop-out rate. eTable 7. Inconsistency of different intervention. eTable 8. Estimated between-studies standard deviation of different outcome. eTable 9. GRADE evaluation quality of evidence for primary outcome. eFigure1. Test for transitivity assumption of primary outcome: changes of cognition function-overall. eFigure2. A network structure of NMA of changes of quality of life. B network structure of NMA of safety profile in aspect of rate of any adverse event. C network structure of NMA of safety profile in aspect of rate of any local discomfort. D network structure of NMA of acceptability in aspect of drop-out rate. eFigure3. A forest plot of NMA of change of quality of life. B forest plot of NMA of safety profile in aspect of rate of any adverse event. C forest plot of NMA of safety profile in aspect of rate of any local discomfort. D forest plot of NMA of acceptability in aspect of drop-out rate. eFigure4. A overview of risk of bias. B detailed risk of bias in each study. eFigure5. A Funnel plot of changes of cognition function: overall. B Egger’s regression of changes of cognition function: overall. C Funnel plot of changes of cognition function: MMSE measurement. D Egger’s regression of changes of cognition function: MMSE measurement. E Funnel plot of changes of cognition function: ADAS-Cog measurement. F Egger’s regression of changes of cognition function: ADAS-Cog measurement. G Funnel plot of changes of quality of life. H Egger’s regression of changes of quality of life. I Funnel plot of safety profile in aspect of rate of any adverse event. J Egger’s regression of safety profile in aspect of rate of any adverse event. K Funnel plot of safety profile in aspect of rate of any local discomfort. L Egger’s regression of safety profile in aspect of rate of any local discomfort. M Funnel plot of acceptability in aspect of drop-out rate. N Egger’s regression of acceptability in aspect of drop-out rate.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tseng, PT., Chen, YW., Zeng, BY. et al. The beneficial effect on cognition of noninvasive brain stimulation intervention in patients with dementia: a network meta-analysis of randomized controlled trials. Alz Res Therapy 15, 20 (2023). https://doi.org/10.1186/s13195-023-01164-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13195-023-01164-2