Abstract
Background
The lack of approved treatments for the majority of rare diseases is reflective of the unique challenges of orphan drug development. Novel methodologies, including new functionally relevant endpoints, are needed to render the development process more feasible and appropriate for these rare populations and thereby expedite the approval of promising treatments to address patients’ high unmet medical need. Here, we describe the development of an innovative master protocol and primary outcome assessment to investigate the modified amino acid N-acetyl-l-leucine (Sponsor Code: IB1001) in three separate, multinational, phase II trials for three ultra-rare, autosomal-recessive, neurodegenerative disorders: Niemann-Pick disease type C (NPC), GM2 gangliosidoses (Tay-Sachs and Sandhoff disease; “GM2”), and ataxia telangiectasia (A-T).
Methods/design
The innovative IB1001 master protocol and novel CI-CS primary endpoints were developed through a close collaboration between the Industry Sponsor, Key Opinion Leaders, representatives of the Patient Communities, and National Regulatory Authorities. As a result, the open-label, rater-blinded study design is considerate of the practical limitations of recruitment and retention of subjects in these ultra-orphan populations. The novel primary endpoint, the Clinical Impression of Change in Severity© (CI-CS), accommodates the heterogenous clinical presentation of NPC, GM2, and A-T: at screening, the principal investigator appoints for each patient a primary anchor test (either the 8-m walk test (8MWT) or 9-hole peg test of the dominant hand (9HPT-D)) based on his/her unique clinical symptoms. The anchor tests are videoed in a standardized manner at each visit to capture all aspects related to the patient’s functional performance. The CI-CS assessment is ultimately performed by independent, blinded raters who compare videos of the primary anchor test from three periods: baseline, the end of treatment, and the end of a post-treatment washout. Blinded to the time point of each video, the raters make an objective comparison scored on a 7-point Likert scale of the change in the severity of the patient’s neurological signs and symptoms from video A to video B. To investigate both the symptomatic and disease-modifying effects of treatment, N-acetyl-l-leucine is assessed during two treatment sequences: a 6-week parent study and 1-year extension phase.
Discussion
The novel CI-CS assessment, developed through a collaboration of all stakeholders, is advantageous in that it better ensures the primary endpoint is functionally relevant for each patient, is able to capture small but meaningful clinical changes critical to the patients’ quality of life (fine-motor skills; gait), and blinds the primary outcome assessment. The results of these three trials will inform whether N-acetyl-l-leucine is an effective treatment for NPC, GM2, and A-T and can also serve as a new therapeutic paradigm for the development of future treatments for other orphan diseases.
Trial registration
The three trials (IB1001-201 for Niemann-Pick disease type C (NPC), IB1001-202 for GM2 gangliosidoses (Tay-Sachs and Sandhoff), IB1001-203 for ataxia telangiectasia (A-T)) have been registered at www.clinicaltrials.gov (NCT03759639; NCT03759665; NCT03759678), www.clinicaltrialsregister.eu (EudraCT: 2018-004331-71; 2018-004406-25; 2018-004407-39), and https://www.germanctr.de (DR KS-ID: DRKS00016567; DRKS00017539; DRKS00020511).
Similar content being viewed by others
Background
The Orphan Drug Act of 1983 [1] defines rare (“orphan”) diseases as those which affect 200,000 or fewer individuals in the USA. Recently, advances in diagnostic techniques, particularly next-generation sequencing of DNA, have led to the rapid expansion in the number of recognized “ultra-rare diseases,” proposed to describe disorders with a prevalence of less than 1:100,000 individuals [2]. It is now estimated there are over 10,000 rare and ultra-rare diseases which, although individually rare in prevalence, are collectively estimated to affect some 30 million Americans [3]. For over 95% of these disorders there are no US Food and Drug Administration (FDA)-approved treatments [4].
The lack of approved orphan drugs reflects the unique challenges of orphan drug development. The conventional pathway to drug approval is often unsuitable for rare diseases and raises hurdles that cannot be easily overcome, if at all [5, 6]. Novel drug-development strategies are needed to render the regulatory and development processes more feasible and cost-effective and more quickly address the extremely high unmet medical need of orphan diseases [7].
One response to expedite the development of novel treatments for rare diseases is to utilize a master protocol, where a single drug can be investigated for multiple indications. These may take three forms:
-
(i)
Umbrella trials, which study multiple targeted therapies in a single disease;
-
(ii)
Platform trials, in which multiple targeted therapies are studied in a single disease on an ongoing basis. Therapies are added or subtracted to the platform on the basis of previously agreed algorithms, with therapies allowed to enter or leave the platform on the basis of a decision algorithm;
-
(iii)
Basket studies, in which a single targeted therapy is studied in multiple diseases, or disease subtypes [8].
Here, we describe the development of a master protocol comprising three separate basket studies to investigate a novel agent, N-acetyl-l-leucine (Sponsor Code: IB1001), as a therapy for three different ultra-rare neurodegenerative diseases: Niemann-Pick disease type C (NPC), GM2 gangliosidoses (Tay-Sachs and Sandhoff diseases; “GM2”), and ataxia telangiectasia (A-T), which share cerebellar ataxia as a common central manifestation.
Protocol references
IB1001-201 investigates N-acetyl-l-leucine for the treatment of Niemann-Pick disease type C (NPC). NPC is an ultra-rare (1:120,000), prematurely fatal, autosomal recessive, neurovisceral lysosomal storage disease that predominantly affects children. However, adolescent and adult onset cases are being increasingly recognized [9, 10]. Treatment of NPC is so far limited to reducing the rate of disease progression with the substrate reduction therapy drug miglustat (Zavesca™ [11]), approved in the European Union and several other countries, but not in the USA.
IB1001-202 investigates N-acetyl-l-leucine for the treatment of the GM2 gangliosidoses (Tay-Sachs and Sandhoff diseases; “GM2”). GM2 is an ultra-rare (0.28:100,000), prematurely fatal, autosomal recessive, neurovisceral lysosomal storage disorder that predominantly and most severely affect pediatric patients [12]. There is currently no approved treatment in any jurisdiction for GM2.
IB1001-203 investigates N-acetyl-l-leucine for the treatment of ataxia telangiectasia (A-T). A-T is an ultra-rare (1:40,000–100,000), autosomal recessive, cerebellar ataxia that predominantly affects pediatric patients [13]. There is currently no approved treatment in any jurisdiction for A-T.
Despite their different etiologies, NPC, GM2, and A-T are all characterized by progressive neurodegeneration of the cerebellum and cerebrum, resulting in physical and cognitive decline, and premature death. Each disorder manifests systemic, neurological, and neuropsychological findings. The three disorders share a number of hallmark symptoms, in particular, cerebellar ataxia, dysarthria, and dysphagia. Owing to their common neurological manifestations, and the mechanism of action of the investigational product N-acetyl-l-leucine, a single master protocol has been developed for the three disorders.
N-acetyl-l-leucine
N-acetyl-l-leucine is the L-enantiomer of N-acetyl-leucine, a modified amino acid that has been available in France since 1957 as a racemate (equal amounts of both D- and L-enantiomers) under the trade name Tanganil® (Pierre Fabre Laboratories) as a treatment for acute vertigo. N-acetyl-l-leucine is not approved for any indication in any jurisdiction.
The mechanisms of action of N-acetyl-dl-leucine for vertigo are not fully understood. It may act directly on neurons; in the vestibular nuclei, N-acetyl-dl-leucine has been shown to restore membrane potential in hyperpolarized/depolarized vestibular neurons following unilateral labyrinthectomy in guinea pigs [14]. This effect may be mediated by N-acetyl-dl-leucine’s direct interactions with membrane phospholipids such as phosphatidylinositol 4,5-bisphosphate, which influence ion channel activity [15]. Thus, N- acetyl-DL-leucine can normalize neuronal function. In patients with a unilateral neurotomy and labyrinthectomy, the agent was described to normalize the vestibular asymmetry, showing an effect only in the subgroup of individuals with residual vestibular function [16].
Subsequent studies in models of vertigo on the individual enantiomers have revealed that the therapeutic effects of N-acetyl-dl-leucine are due to the L-enantiomer. Studies of a rat model of unilateral labyrinthectomy revealed that N-acetyl-l-leucine, but not N-acetyl-d-leucine, is the pharmacologically active substance that improves central vestibular compensation [17]. Furthermore, a study in a unilateral vestibular neurectomy cat model suggested that N-acetyl-l-leucine is the enantiomer that leads to a significant acceleration of the vestibular compensation process, most likely acting on vestibular nuclei neurons [18].
Given the phylogenetic and electrophysiological similarities and close interactions between vestibular and deep cerebellar neurons, it was hypothesized both N-acetyl-dl-leucine and therefore also N-acetyl-l-leucine may have clinical utility in the treatment of cerebellar symptoms that occur in diseases such as NPC through a similar mechanism as that observed in models of vertigo, acting on neurons. However, in vitro experiments using non-neuronal, Npc1-deficient Chinese hamster ovary cells or fibroblasts derived from patients with NPC demonstrated N-acetyl-l-leucine and N-acetyl-dl-leucine also reverse disease-related cellular phenotypes in non-neuronal cells, including expanded lysosomal volume, with superior efficacy resulting from the L-enantiomer [19]. The mechanisms leading to effects on lysosomal storage in non-neuronal cells are currently under investigation.
N-acetyl-l-leucine has also been demonstrated to reduce neuroinflammation in the cerebellum. Activated microglia are associated with the neurodegenerative and neuroinflammatory components of cerebellar disorders, as engulfment of neuronal processes by microglia precede Purkinje cell death (an important type of nerve cell involved in movement control). In vivo studies in a mouse model for traumatic brain injury demonstrate treatment with N-acetyl-l-leucine improves lysosome-related autophagy flux and thereby restores its neuroprotective function in the cortices after traumatic brain injury [20]. This is expected to lead to the attenuation and restrict neuronal cell death, hence improving neurological function [20]. As acute and prolonged neuroinflammation contribute to neuronal death, these results suggest that N-acetyl-l-leucine may protect cells from neurodegeneration arising from genetic or acquired neurological disorders.
Trial rationale
The development of N-acetyl-leucine for NPC, GM2, and A-T began with the investigation of the commercially available racemic mixture, N-acetyl-dl-leucine (Tanganil®). In a case series of 12 patients with NPC, it was shown that N-acetyl-dl-leucine (3 g/day for 1 week followed by 5 g/day for 3 weeks) significantly improved the symptoms of NPC after 4 weeks of treatment, measured by the Scale for the Assessment and Rating of Ataxia (SARA), the Spinocerebellar Ataxia Functional Index (SCAFI), and EuroQol-5D-5L. N-acetyl-dl-leucine was well tolerated, and no side effects except for intermittent dizziness were reported [21]. An additional case series describes the disease-modifying effect of long-term treatment with N-acetyl-dl-leucine in 10 patients with NPC treated for a median length of 7.7 months (maximum 21.2, minimum 2.7 months) [22].
The clinical utility of N-acetyl-dl-leucine for the treatment of Tay-Sachs, Sandhoff, and A-T has also been investigated in a compassionate-use case-series, as well as a variety of inherited cerebellar ataxias [23,24,25]. In all studies, the compound was well-tolerated with no discernible serious side effects.
These preliminary clinical findings have been supported by in vitro studies in NPC and GM2 gangliosidoses patient cell lines, and in vivo studies in the NPC (Npc1−/−) and Sandhoff (Hexb−/−) mouse models, which corroborate the pharmacological properties of N-acetyl-l-leucine and N-acetyl-dl-leucine in relation to the observed therapeutic effects (Ecem Kaya and Frances Platt, personal communication) [19]. These non-clinical studies have demonstrated the L-enantiomer, i.e., acetyl-l-Leucine, is believed to have potential clinical benefits compared to the racemic mixture [14,15,16]. Further, pharmacokinetic studies suggest that the D-enantiomer could accumulate relative to the L-enantiomer during chronic administration of the racemate, which has the potential for long term negative effects [26].
The development of N-acetyl-L-leucine has therefore been initially prioritized for the treatment of NPC, GM2, and A-T based on the existing pre-clinical and clinical data in these three disorders demonstrating safety and significant efficacy and the high unmet medical need of each indication. Following the IB1001 clinical trials, it is planned to investigate N-acetyl-l-leucine for the treatment of additional rare disorders, including common ataxias, as well as rare and common neurological disorders.
Rare disease trial design
NPC, GM2, and A-T are progressive, life-threatening conditions with limited or no approved drugs, mandating greater urgency for trials to be conducted as efficiently as possible to maximize the chance they can be made available before the window of therapeutic opportunity is lost. However, like many clinical trials for rare and ultra-rare diseases, there are a number of critical protocol considerations which must be considered to do so:
-
1.
For each disorder, the potential pool of participants is small, and within that circumscribed group, not all individuals are willing to participate or suitable candidates for clinical trials.
-
2.
Parents and caregivers in these communities have legitimate ethical concerns about placebo-controlled trials. This may complicate and delays the recruitment and completion of studies and, subsequently, approval and availability of the treatment for patients. The risk is even greater for trials like IB1001 which involves a modified version of a compound (Tanganil®) that is approved in France (as well as Lebanon, Vietnam, and Tunisia) for use in another clinical setting (acute vertigo) and which is known to be widely used in an unlicensed setting within these patient communities.
-
3.
Each of these indications is characterized by broad variability in the symptoms and signs of rare diseases they exhibit, in the age at which they first present, and the rate at which they progress. The high inter-individual variability in the clinical course of the disease renders an assembly of well-matched cohorts of patients for controlled trials impossible.
-
4.
Given the heterogeneity of the diseases, there are significant limitations in selecting and prioritizing a single outcome measure that can be considered clinically meaningful for the entire patient population.
Together, these factors significantly diminish a study’s ability to detect a therapeutic effect. Thus, detecting a statistically significant difference between intervention and control groups is hard to achieve.
Collaboration
As a consequence of these challenges, many promising treatments for orphan diseases will never surpass the development hurdles and become approved for patients. In too many instances, when a rare disease trial fails, it is not clear if this is a consequence of the compound’s lack of a biological effect or an inadequate study design that was not compatible with what can be reasonably achieved within the rare disease patient population. To avoid this pitfall in the IB1001 studies, an innovative master protocol and novel primary outcome measure were developed through a close collaboration between Regulatory Agencies, Key Opinion Leaders—including clinicians and patient communities—and the industry sponsors. Such cooperation was essential to create a trial design founded on a strong scientific rationale, but also taking into account the demographics of these heterogenous, rare populations. It is our hope that the collaboration between these stakeholders and resulting development program for IB1001 represent a model to expedite the development of novel treatments for rare diseases.
Methods/design
Trial centers
The IB1001-201 (NPC), IB1001-202 (GM2), and IB1001-203 (A-T) clinical trials are separate multinational, multicenter, open-label, rater-blinded phase II studies. Each trial will enroll approximately 30 patients. Subjects are currently screened at 13 centers across Germany, Spain, Slovakia, the UK, and the USA, including Ludwig Maximilians University, Munich (201, 202, 203); University of Giessen (201, 202, 203); Bellvitge University Hospital (201, 202); Hospital University La Paz (203); Comenius University in Bratislava (201); Great Ormond Street Hospital (201); Royal Free Hospital (201); Royal Manchester Children’s Hospital (201, 202); Salford Royal NHS Foundation Trust (201, 202); Royal Papworth Hospital (203); The Mayo Clinic, Rochester MN (201, 202); New York University Langone (202), and University of California Los Angeles (202, 203).
Study oversight
The IB1001 trials are conducted in accordance with the International Conference for Harmonisation (of Technical Requirements for Pharmaceuticals for Human Use) - Good Clinical Practice Guideline, the General Data Protection Regulator, and the Declaration of Helsinki. The studies have been approved by the ethics committees of each participating center and the regulatory authorities in each respective country. The safety, integrity, and feasibility of the trial is monitored by an independent data safety monitoring board (DSMB) consisting of three independent, non-participating members (including two clinicians and a statistician). The function of the DSMB is to monitor the course of the studies and, as applicable, give a recommendation to the Sponsor of the trial for discontinuation, modification or continuation of the study.
Patient population and eligibility criteria
Patients are screened for eligibility according to the inclusion and exclusion criteria. To be eligible for the respective study, patients with a confirmed diagnosis of NPC, GM2, or A-T (aged ≥ 6 years in Europe and ≥ 18 years in the USA) must present with clinical symptoms, provide appropriate informed consent, and undertake a washout of any prohibited medications (if applicable). These include any variant of N-acetyl-dl-leucine (e.g., Tanganil®). For a detailed description of the inclusion and exclusion criteria, see Table 1.
Recruitment and patient involvement
Patients are recruited via personal correspondence, routine care appointments, and referrals. In addition, there is tremendous collaboration and support from multinational patient organizations representing these rare disease communities.
The principal investigator at each trial site is responsible for obtaining informed consent for each patient. All eligible patients who agree to participate in the study are provided with a full verbal explanation of the trial and the patient information sheet. This includes detailed information about the rationale, design, and personal implications of the study.
Study design and procedures
The IB1001 clinical trials are open-label, rater-blinded studies. During the development of the IB1001 master protocol, the appropriateness of initiating a randomized, double-blind, controlled studies for these ultra-orphans was strongly questioned by clinical experts and representatives of the patient communities, given the diseases’ relentless and often rapid progression, prematurely fatal outcome, and lack of alternative treatment options. A formal feasibility study was initiated by the Sponsor that demonstrated that a long-term, randomized, double-blind, placebo-controlled, crossover study would be difficult to recruit and carry out without changes to the study design. This was largely attributed to the known, widespread, off-label/unlicensed use of N-acetyl-dl-leucine (Tanganil®). Patients and families expressed reluctance to participate in a placebo-controlled study where they would be required to washout from this off-label/unlicensed medication and receive an inactive treatment for even 50% of the time.
In order to assure the feasibility of recruitment, an open-label study schema is used. Based on observational and pre-clinical studies that demonstrate the potential of symptomatic benefit of treatment in as little as 4 weeks [21, 23], in the first treatment sequence (“parent study”), patients are assessed during three study phases: a baseline period (with or without a study run-in), a treatment period of 6 weeks (42–49 days), and a washout period of 6 weeks (42–49 days). Patients will be assessed twice during each period to allow an assessment of intra-patient variability.
At the initial screening visit, patients will be classified as either “naïve” or “non-naïve” depending on their use of prohibited medications within the past 6 weeks (42 days). The schedule of events during the initial screening visit and throughout the baseline period (through visit 1) will vary depending on the patient’s classification as either “naïve” or “non-naïve.”
Given the known unlicensed use of the racemate (Tanganil®), for all patients, a urine sample will be taken at visit 1 to detect N-acetyl-d-leucine using a validated liquid chromatography mass spectrometry/mass spectrometry method. Provided the level of N-acetyl-d-leucine tests below the permitted threshold, the initial screening visit will be confirmed as visit 1 (baseline 1). If a patient classified as “Naïve” unexpectedly tests positive for levels of N-acetyl-d-leucine above the permitted threshold, at the direction of their principal investigator, a run-in wash-out period of 6 weeks (42 days) is requested before they are eligible to return for a repeat visit 1. Patients who fail two urine N-acetyl-d-leucine tests (e.g., visit 1 and repeat visit 1) are ineligible for the study.
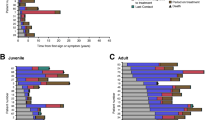
Figure 1 displays the naïve and non-naïve study schemes for the parent study. Suppl. Table 1 lists the schedule of enrolment and assessments together with pre-planned time points for clinic visits during.
Parent study schema. During the treatment period, all patients will receive N-acetyl-l-leucine for 42 days (+ 7 days). Visit 3 (treatment 1) will occur at day 28 (+ 7 days) of the treatment period and visit 4 (treatment 2) will occur after the full 42 days (+ 7 days) of treatment. A 42-day (+ 7 days) washout period will be performed following treatment with N-acetyl-l-leucine. Visit 5 (washout 1) will occur on day 28 (+ 7 days) of the washout period and visit 6 (washout 2) will occur after the full 42 days (+ 7 days) of washout. a Naïve patients screening pathway: patients who have not used any prohibited medications within 42 days of screening are “naïve.” Their initial screening visit is treated as visit 1 (baseline 1). b Non-naïve patient screening pathway: patients who have used or are unable to confirm or deny if they have used any prohibited medication within the past 42 days are “non-naïve.” Patient will be given the opportunity to undergo a minimum of 42 days washout before returning for a repeat visit 1 (baseline 1)
Patients who have completed visit 6 of the parent study have the opportunity to continue treatment with N-acetyl-l-leucine (IB1001) in an extension phase if the principal investigator determines it is in their best interest. The extension phase consists of a 1-year (351–379 days) treatment period followed by a 6 weeks (42–56 days) washout period. Table 2 lists the inclusion criteria for the extension phase. Figure 2 displays the extension phase study schema. Suppl. Table 2 lists the schedule of enrolment and assessments together with pre-planned time points for clinic visits in the extension phase.
Study drug
In the parent study, the dosage formulation of N-acetyl-l-leucine is 1000 mg powder for oral suspension (manufacture: Patheon UK Limited, Oxfordshire, UK) which is suspended in 40 mL Ora-Blend®.
In the extension phase, the dosage form of N-acetyl-l-leucine is 1000 mg granules for oral suspension in a sachet (manufacture: Patheon UK Limited, Oxfordshire, UK, and Patheon France S.A.S., Bourgoin, France) which is suspended in 40 mL water.
Administration and study drug dosage
During the treatment periods for both treatment sequences, the dosing of the study drug is as follows: Patients aged ≥ 13 years or aged 6–12 years weighing ≥ 35 kg will take 4 g/day (2 g in the morning, 1 g in the afternoon, and 1 g in the evening). Patients aged 6–12 years weighing 25 to < 35 kg will take 3 g/day (1 g in the morning, 1 g in the afternoon, and 1 g in the evening). Patients aged 6–12 years weighing 15 to < 25 kg will take 2 g/day (1 g in the morning and 1 g in the evening). Medication should be taken at least 30 min before or at least 2 h after a meal.
If adverse events are noted, patients are permitted to down-titrate to one-half their daily dose, at the direction of the investigator. Compliance will be assessed upon a review of the inventory of IB1001 bottles/sachets returned by patients.
Study objectives
The two treatment sequences in the parent study and extension phase enable the investigation of both the symptomatic (6 week) and long-term (1 year) safety and efficacy of treatment with N-acetyl-l-leucine.
The primary objective of both treatment sequences is to evaluate the efficacy of N-acetyl-l-leucine based on blinded raters’ Clinical Impression of Change in Severity© (CI-CS) in the treatment of NPC, GM2, or A-T.
The secondary objectives are:
-
To assess the clinical efficacy (symptomatic and long-term) of N-acetyl-l-Leucine on symptoms of ataxia, functioning, and quality of life for patients with NPC, GM2, or A-T;
-
To evaluate the safety and tolerability of N-acetyl-l-leucine at 4 g/day in patients with NPC, GM2, or A-T, including patients aged ≥ 18 years in the USA and patients aged ≥ 13 years in Europe, and weight-tiered doses in patients 6 to 12 years of age in Europe.
In the extension phase, an additional secondary objective is to characterize the pharmacokinetics of N-acetyl-l-leucine in patients with NPC, GM2, or A-T.
Safety and efficacy parameters
Primary efficacy endpoint
In light of the defined challenges to conducting an open-label clinical trial in these ultra-orphan diseases, a novel primary endpoint, the Clinical Impression of Change in Severity© (CI-CS) was developed.
The administration and assessment of the CI-CS involves three tasks. Table 3 provides an overview of each task, the responsible party and the time point at which it is performed.
-
(1)
Determine CI-CS primary anchor test (8MWT or 9HPT-D)
Given the heterogeneity of symptoms, the appointment of a single symptom scale, such as either the 8-m walk test (8MWT) or the 9-hole peg test of the dominant hand (9HPT-D), as the primary outcome measure is not appropriate for patient populations. To better ensure the primary outcome measure is clinically meaningful for each individual patient, at visit 1, the principal investigator selects either the 8MWT or 9HPT-D to be the patient’s “primary anchor test.” The selection is guided by pre-defined criteria based on patient’s performance on ataxia rating scales (Spinocerebellar Ataxia Functional Index (SCAFI) and Scale for the Assessment and Rating of Ataxia (SARA)), as well as interactions with the patient, their family, and/or caregivers. A cognitive assessment is also performed at visit 1 according to the standard procedures of the clinical site to select an anchoring functional test which is appropriate for each patient from both a cognitive and a motor perspective. The primary anchor test remains fixed for each patient for the duration of the study.
-
(2)
Video recordings: primary and non-primary anchor tests
At each study visit (except visit 0), the 8MWT and 9HPT-D are videoed in a standardized manner by qualified members of the study team. Video consultation has been validated in other diseases and can minimize variability in the data [27,28,29]. Out of necessity, the trials are conducted at multiple study sites in different geographical locations, with inherent potential for considerable inter-rater variability in assessment scores [27]. Video recordings allow for centralized review and repeated viewing without the necessity for repetition and patient fatigue [30].
Each clinical site must qualify two videographers before any patients are screened. All patient videos should be performed by the same videographer, in the same environment, to ensure consistency and reduce the potential for variability. Videos will be collected by the clinical sites and submitted to Medpace Core Laboratories via the web based ClinTrak Imaging Windows Client Application for collection, quality control, central review, and storage. A more detailed description on the acquisition, submission, and video review process is provided in Suppl. Material I.
-
(3)
CI-CS assessment of primary anchor test
The primary CI-CS assessment is performed by two, independent raters based on the videos of each patient’s primary anchor test acquired throughout the respective treatment sequence (visits 1–6; visits 7–10). Prior to their review of patient videos, the raters are trained on existing videos to ensure standardization of the assessments.
Raters are asked to assess three video pairs:
-
Pair A: (i) Baseline and (ii) end of treatment
-
Pair B: (ii) End of treatment and (iii) end of washout
-
Pair C: (iii) End of washout and (i) baseline
Pairs A, B, and C are reviewed by the raters in random order. The internal pairing of videos (i) baseline, (ii) end of treatment, and (iii) end of washout will also be arranged randomly. The raters will be blinded in this way to reduce detection and performance biases.
For each pair, raters are asked to assess: “Compared to the first video, how has the severity of the patient’s performance on the 8MWT or 9HPT-D changed (improved or worsened) as observed in the second video?” The CI-CS assessment is based on a 7-point Likert scale ranging from + 3 (significantly improved) to − 3 (significantly worse). If there is a difference of one (1) point in the two primary blinded raters’ CI-CS scores for a specific video pairing, the two scores will be averaged. If there is a difference greater than one (1) point between the two primary blinded reviewers’ CI-CS scores for a specific video pairing, an adjudication rating will be triggered. In such cases, a third blinded rater will review the scores given from each of the two primary independent raters and determine which score is more accurate, that of rater A or rater B (adjudication by consensus). The adjudicator’s decision will provide the final score for that video assessment.
Primary endpoint definition
The primary endpoint is defined as:
Assessment A: the CI-CS comparing videos of the patient’s performance on the pre-defined anchor test at (i) the end of treatment versus (ii) baseline; minus
Assessment B: the CI-CS comparing videos of the patient’s performance on the pre-defined anchor test at (i) the end of washout versus (ii) end of treatment.
The CI-CS achieves the following: first, detection and performance bias for the primary endpoint is reduced by the blinded, independent review. Second, each patient’s washout period (assessment B) serves as a control arm to their treatment period (assessment A). Third, videos increase reliability and minimize the burden on patients. Finally, the CI-CS is a platform to capture and assess small but clinically meaningful changes in patient’s performance, which relate to their level of functioning and quality of life, but which cannot be obtained from the quantitative timed 8MWT or 9HPT-D assessments. This is critical: although functioning typically improves with symptom reduction, these concepts are not always concordant [31]. For example, a change in gait velocity does not necessarily account for the way gait patterns deviate from normal (i.e., balance, variability, asymmetry, rhythm, posture, or, notably, the ability to walk unaided [23, 30]) and, therefore, a meaningful improvement in ambulation. Similarly, a faster 9HPT score does not necessarily capture a change in fine-motor skills, grip, or tremor wherein individuals may perform the test more carefully or precisely which results, paradoxically, in an increase in 9HPT time. Therefore, the CI-CS is a metric of clinical importance that cannot be obtained from traditional assessment measures.
In the extension phase, the primary endpoint is defined as success on the Clinical Impression of Change in Severity© (CI-CS) comparing videos of the primary anchor test at (i) the end of the extension phase treatment with N-acetyl-l-leucine (visit 9) versus (ii) the extension phase baseline (visit 7). Clinical benefit is defined as a CI-CS value of 0 (no change) or better (≥ 1, at least some improvement).
Secondary efficacy endpoints to supplement the analysis of the primary endpoint
Supportive secondary endpoints will be evaluated that directly supplement the analysis of the primary endpoint, including the independent raters’ Clinical Impression of Severity (CI-S). The raters will be given videos of the patient’s performance on the primary and non-primary anchor test acquired at each visit of the respective treatment sequence (visits 1 to 6; visits 7 to 10). This will enable the evaluation of both of the possible anchor tests and assess the appropriateness of the chosen primary anchor test with regard to its ability to function as a clinically meaningful outcome measure for the patient. Again, videos will be presented to the raters in a randomized, blinded manner.
For each video, the raters are asked to assess: “Considering your total clinical experience with this particular population, how ill is the patient at this time?” The CI-S is rated on a 7-point Likert scale ranging from + 3 (normal, not at all ill) to − 3 (among the most extremely ill patients). For the CI-S, if there is any difference in the two blinded reviewers’ scores, the two scores will be averaged.
Secondary endpoints
Additional secondary endpoints will measure other symptoms and evaluate quality of life. Descriptive statistics will be provided for these measures at each visit and, also, changes from [parent study/extension phase] baseline (visit 2/visit 7) to the end of treatment with N-acetyl-l-leucine (visit 4/visit 9), as well as end of treatment with N-acetyl-l-leucine (visit 4/visit 9) to the end of the post-treatment washout (visit 6/visit 10) for the following measures:
-
Spinocerebellar Ataxia Functional Index (SCAFI) [32].
-
Scale for Assessment and Rating of Ataxia (SARA) score [32, 33].
-
Quality of Life EQ-5D-5L for patients aged ≥ 18; EQ-5D-Y for patients aged < 18 years [34].
-
Modified Disability Rating Scale (mDRS) (201 and 202 study only) [35, 36].
-
Clinical Global Impression Scales [37]:
-
Investigator, caregiver, and patient (if able) clinical global impression of severity at every visit
-
Investigator, caregiver, and patient (if able) clinical global impression of improvement comparing end of treatment (visit 4/visit 9) to baseline (visit 2/visit 7) and end of washout (visit 6/visit 10) to end of treatment (visit 4/visit 9)
-
-
Columbia Suicide Severity Rating Scale (203 study only) [38].
In the extension phase of the IB1001-201 study only, the Niemann-Pick disease type C Clinical Severity Scale (NPC-CSS) will be introduced as a secondary endpoint, where the graduation of changes is expected to detect clinically relevant changes in functioning/benefit after 1 year of treatment [39].
In addition, the Annual Severity Increment Score [22] will be assessed in the extension phase.
Safety parameters
Adverse events (serious and non-serious), concomitant drug and non-drug therapies, safety laboratory blood samples (hemoglobin, erythrocytes, hematocrit, thrombocytes, leukocytes, sodium, lactate dehydrogenase, potassium, creatinine, serum bilirubin level, aspartate aminotransferase, alanine aminotransferase, urea, alkaline phosphatase, follicle-stimulating hormone for postmenopausal women only), and urine samples (leukocytes, nitrite, urobilinogen, protein, pH, occult blood (erythrocytes, leucocytes), specific gravity, ketones, bilirubin, glucose) will be collected routinely throughout the study. Sparse pharmacokinetic blood sampling will be conducted at every visit (visit 1–visit 10). Blood samples for the quantification of N-acetyl-l-leucine in plasma will be obtained at visit 7 and visit 9. Urine samples will also be collected for concentrations of N-acetyl-d-leucine at the time points designated on the schedule of events (Suppl. Table 1, 2). At visit 1, this urine sample serves as a key enrollment criterion testing for the use of the prohibited medication N-acetyl-dl-leucine. Vital signs, physical exams, height/weight, and electrocardiograms will also be collected at the time points designated on the schedule of events (Suppl. Table 1, 2). A detailed description of the safety parameters is provided in Suppl. Material II.
Statistical planning and analyses
The statistical analysis plan details the statistical methods for analysis for each of the three clinical trials. Data from the three clinical trials will be analyzed separately.
The primary analysis population is the modified intention to treat (mITT) analysis set defined as all patients who receive at least one dose of study drug (N-acetyl-l-leucine) and with one video recording at either visit 1 or visit 2 (or both) and visit 3 or visit 4 (or both). Analyses will also be conducted on the per protocol analysis set which will consist of all patients with video recordings at baseline (visit 1 and/or visit 2), end of treatment (visit 3 and/or visit 4), and end of washout (visit 5 and/or visit 6) and without any major protocol deviations that can influence the validity of the data for the primary efficacy variable.
The primary endpoint will utilize assessments based on single video recordings at the end baseline period (visit 2), end of the treatment period (visit 4), and end of the washout period (visit 6). If the visit 2 video is missing, the visit 1 video will be used in its place. Similarly, if the visit 4 and visit 6 videos are missing, visit 3 and visit 5 videos will respectively be used in their place. Analyses based on the mITT analysis set will utilize a last observation carried forward approach for missing videos 5 and 6. For the primary endpoint CI-CS, this implies that the CI-CS value for visit 4 to visit 6 will be assigned the value 0 if both videos 5 and 6 are not available.
The analysis of the primary endpoint will be based on a single sample one-sided t test comparing the mean of the CI-CS differences with zero. The null hypothesis is that the mean is ≤ 0, with the alternative hypothesis that this mean is > 0, and the test will be conducted at the one-sided 5% significance level. The secondary endpoint that is based on a 3-point categorization of the CI-CS will be evaluated based on the Wilcoxon-signed-rank test. The analysis of the secondary endpoint, Clinical Impression of Severity (CI-S), will be analyzed for the primary endpoint. All other endpoints will be evaluated descriptively. There will be no formal control of multiplicity across these endpoints.
For each of the primary and secondary endpoints, there will be evaluation within key subgroups; naïve versus non-naïve, age (pediatric versus adult), gender (male versus female), region (USA versus Europe), primary anchor test (9HPT-D or 8MWT), patients on miglustat vs patients not on miglustat (201 study only); Tay-Sachs versus Sandhoff patients (202 study only), individual components of SARA scale at baseline: Gait Subtest, composite of SARA Subtests 1–4 (Gait, Stance, Sitting, Speech), intra-patient variability between SARA score at visit 1 (baseline 1) versus visit 2 (baseline 2) (below/above median) and intra-patient variability between CI-S score visit 1 (baseline 1) versus visit 2 (baseline 2) (below/above median). These evaluations will be based on plotting treatment differences together with 90% confidence intervals within each subgroup.
It is postulated that N-acetyl-l-leucine will show effectiveness in 30% of patients and this success rate is viewed as being clinically important. It is assumed that this group of patients will have scores that are distributed across the values 1 and 2 for the primary endpoint with 10% scoring 1 and 20% scoring 2 and further that the remaining 70% of patients will have scores that are evenly distributed between the values − 1, 0, and 1. The resulting mean score is 0.5 and the standard deviation for the primary endpoint under these assumptions is then 1.075. With 30 patients reporting on the primary endpoint, the study will have 80% power to detect a treatment benefit in a 5% one-sided one-sample t test. Assuming alternatively that the 30% of patients improving will have scores that are evenly distributed across the values 1 and 2, then the mean score for the primary endpoint will be 0.45 with an SD of 1.02. Under these assumptions, the study will have power of 76%.
In observational case-series, N-acetyl-leucine has demonstrated potential as a broad treatment for the general symptoms of other progressive, inherited ataxias [23, 24]. Meta-analyses will therefore be conducted across the three separate studies for NPC, GM2, and A-T to assess more general question regarding the effectiveness of N-acetyl-l-leucine for symptoms of ataxia. A description of Data Collection is provided in Suppl. Material III.
Discussion
Given the lack of global symptomatic or disease-modifying therapies for NPC, GM2, or A-T, there is an urgent need for effective and well-tolerated drug treatments. The open-label, rater-blinded IB1001 master protocol was designed through a collaboration between National Regulatory Agencies, leading Clinical Experts, Patient Organizations, and the industry Sponsor, to address of the unique ethical and practical challenges to conducting clinical trials for these orphan, heterogenous patient populations, and be better able to capture N-acetyl-l-leucine’s therapeutic effect and, therefore, best positioned to expedite the development and availability of this promising drug candidate [7].
In Sponsor meetings with National Regulatory Authorities, methodological and statistical concerns were raised and discussed, with an emphasis on selecting a specific primary outcome measure that focuses on the aspects of the diseases that are relevant and meaningful to patients. Subsequent interviews with representatives of the patient communities and leading clinicians, regarding the core signs/symptoms that are most meaningful for patients and clinically relevant to physicians, elucidated the key symptoms that affect patient’s quality of life. These symptoms, namely gait and fine motor skills, were established as the anchor tests.
In the absence of a placebo, to minimize detection bias in the primary endpoint, the CI-CS assessment was performed by blinded, independent raters. To prevent potential expectation or performance bias, all aspects of the administration and video recording of the CI-CS anchor tests were standardized to ensure the quality of videos assessed by the blinded raters. Prior to any patient visit, all sites were trained on these detailed protocols, including precise verbal instructions, encouragement, break times between test trials, and instructions on which trial to video. Given the majority of NPC patients enrolled in the IB1001-201 clinical trial featured severe physical impairments with regard to both their fine motor skills as well as balance and gait, and mild to significant levels of cognitive impairment, the potential for a placebo-effect which significantly altered neurological signs and symptoms—the basis of the CI-CS assessment—was therefore considered minimal, ensuring the interpretability of the blinded raters’ CI-CS assessments.
Ultimately, the issues raised during regulatory review and the feasibility process were instructive to develo** the innovative trial design and adaptive primary outcome assessment for the IB1001 studies (tailored to the capabilities of individual patients to maximize inclusion, and better detect a clinically meaningful treatment effect). The pathway to the studies approval was facilitated by frequent communication between all parties, and the collaborative adaptation of study methodology and statistical approaches ensured the IB1001 trials were feasible to recruit, tailored to the capabilities of the NPC, GM2, and A-T patents and, importantly, best positioned to detect a meaningful clinical change in patients’ quality of life.
Trial status
At the time of manuscript submission, the protocol for IB1001-201 (ES: V4.0, 28 August 2019; DE/UK/SL: V5.0, 14 November 2020; US: V5.1, 14 December 2019), IB1001-202 (V5.0, 14 November 2019), and IB1001-203 (V5.0, 30 December 2019) have been accepted/approved in each country where they are respectively planned to be conducted, including the US Food and Drug Administrations (201, 202, 203); UK Medicines and Healthcare products Regulatory Authority (201, 202, 203); German Federal Institute for Drugs and Medical Devices (201, 202, 203), Spanish Agency of Medicines and Medical Products (201, 202), and Slovakia Štátny ústav pre kontrolu liečiv (201), as well as respective research ethics committees (REC)/institutional review boards (IRB) (active approved protocol version varies based on status of enrollment per site/per study). The first study participants were enrolled on 7 June 2019 for IB1001-202 (GM2), 4 September 2019 for IB1001-201 (NPC), and 09 January 2019 for IB1001-203 (A-T). Recruitment for the IB1001-201 study completed 31 January 2020, and the parent study completed September 2020 (extension phase ongoing). Recruitment for the IB1001-202 study was scheduled to be completed 31 March 2020, and June 2020 for the IB1001-203 study. However, due to the global outbreak of COVID-19, further enrollment in these studies has been delayed and is expected to be completed in Spring 2021.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current studies (study protocols).
Abbreviations
- 8MWT:
-
8-m walk test
- 9HPT-D:
-
9-hole peg test of the dominant hand
- A-T:
-
Ataxia telangiectasia
- CI-CS:
-
Clinical impression of change in severity
- CI-S:
-
Clinical impression of severity
- DSMB:
-
Data safety monitoring board
- EQ-QoL:
-
Euro Quality of Life
- EP:
-
Extension phase
- FDA:
-
Food and Drug Administration
- GM2:
-
GM2 gangliosidoses
- mITT:
-
Modified intention to treat
- mDRS:
-
Modified Disability Rating Scale
- NPC:
-
Niemann-Pick type C
- NPC-CSS:
-
NPC clinical severity scale
- PI:
-
Principal investigator
- SARA:
-
Scale for the Assessment and Rating of Ataxia
- SCAFI:
-
Spinocerebellar Ataxia Functional Index
References
Public Law. Orphan Drug Act of 1983. Pub L. No. 97–414, 96 Stat. 2049. Available from: https://www.fda.gov/media/99546/download. [cited 2020 Feb 25].
Richter T, Janoudi G, Amegatse W, Nester-Parr S. Characteristics of drugs for ultra-rare diseases versus drugs for other rare diseases in HTA submissions made to the CADTH CDR. Orphanet J Rare Dis. 2018;13:15.
Haendel M, Vasilevsky N, Unni D, Bologa C, Harris N, Rehm H, et al. How many rare diseases are there? Nat Rev Drug Discov. Nat Publ Group; 2020;19:77–78.
RARE Facts [Internet]. Glob. Genes. [cited 2020 Feb 25]. Available from: https://globalgenes.org/rare-facts/.
Picavet E, Cassiman D, Hollak CE, Maertens JA, Simoens S. Clinical evidence for orphan medicinal products-a cause for concern? Orphanet J Rare Dis. 2013;8:164.
Wilcken B. Rare diseases and the assessment of intervention: what sorts of clinical trials can we use? J Inherit Metab Dis. 2001;24:291–8.
Kempf L, Goldsmith JC, Temple R. Challenges of develo** and conducting clinical trials in rare disorders. Am J Med Genet A. 2018;176:773–83.
Woodcock J, LaVange LM. Master protocols to study multiple therapies, multiple diseases, or both. N Engl J Med. 2017;377:62–70.
Patterson MC, Mengel E, Wijburg FA, Muller A, Schwierin B, Drevon H, et al. Disease and patient characteristics in NP-C patients: findings from an international disease registry. Orphanet J Rare Dis. 2013;8:12.
Vanier MT, Millat G. Niemann-Pick disease type C. Clin Genet. 2003;64:269–81.
Pineda M, Walterfang M, Patterson MC. Miglustat in Niemann-Pick disease type C patients: a review. Orphanet J Rare Dis. 2018;13:140.
Orphanet. Prevalence and incidence of rare diseases. [Internet]. Orphanet Rep. Ser. 2017 [cited 2020 Feb 15]. Available from: https://www.orpha.net/orphacom/cahiers/docs/GB/Prevalence_of_rare_diseases_by_alphabetical_list.pdf.
Reference GH. Ataxia-telangiectasia [Internet]. Genet. Home Ref. [cited 2020 Feb 25]. Available from: https://ghr.nlm.nih.gov/condition/ataxia-telangiectasia.
Vibert N, Vidal PP. In vitro effects of acetyl-DL-leucine (tanganil) on central vestibular neurons and vestibulo-ocular networks of the guinea-pig. Eur J Neurosci. 2001;13:735–48.
Suh B-C, Hille B. PIP2 is a necessary cofactor for ion channel function: how and why? Annu Rev Biophys. 2008;37:175–95.
Ferber-Viart C, Dubreuil C, Vidal PP. Effects of acetyl-DL-leucine in vestibular patients: a clinical study following neurotomy and labyrinthectomy. Audiol Neurootol. 2009;14:17–25.
Günther L, Beck R, **ong G, Potschka H, Jahn K, Bartenstein P, et al. N-acetyl-L-leucine accelerates vestibular compensation after unilateral labyrinthectomy by action in the cerebellum and thalamus. PLoS One. 2015;10:e0120891.
Tighilet B, Leonard J, Bernard-Demanze L, Lacour M. Comparative analysis of pharmacological treatments with N-acetyl-DL-leucine (Tanganil) and its two isomers (N-acetyl-L-leucine and N-acetyl-D-leucine) on vestibular compensation: behavioral investigation in the cat. Eur J Pharmacol. 2015;769:342–9.
te Vruchte D, Galione A, Strupp M, Mann M. Effects of N-Acetyl-Leucine and its enantiomers in Niemann-Pick disease type C cells. bioRxiv. 2019;826222.
Sarkar C, Hegdekar N, Lipinski MM. N-acetyl-L-leucine treatment attenuates neuronal cell death and suppresses neuroinflammation after traumatic brain injury in mice. bioRxiv. 2019:759894.
Bremova T, Malinová V, Amraoui Y, Mengel E, Reinke J, Kolníková M, et al. Acetyl-dl-leucine in Niemann-Pick type C: a case series. Neurology. 2015;85:1368–75.
Cortina-Borja M, Te Vruchte D, Mengel E, Amraoui Y, Imrie J, Jones SA, et al. Annual severity increment score as a tool for stratifying patients with Niemann-pick disease type C and for recruitment to clinical trials. Orphanet J Rare Dis. 2018;13:143.
Schniepp R, Strupp M, Wuehr M, Jahn K, Dieterich M, Brandt T, et al. Acetyl-DL-leucine improves gait variability in patients with cerebellar ataxia-a case series. Cerebellum Ataxias. 2016;3:8.
Strupp M, Teufel J, Habs M, Feuerecker R, Muth C, van de Warrenburg BP, et al. Effects of acetyl-dl-leucine in patients with cerebellar ataxia: a case series. J Neurol. 2013;260:2556–61.
Laumen A, Schneider S, Bremova-Ertl T, Kraus L, Feil K, Strupp M. Rates of responsiveness of acetyl-DL-leucine treatment for ataxia symptoms. Eur J Neurol. 2019;26.
Churchill GC, Strupp M, Galione A, Platt FM. Unexpected differences in the pharmacokinetics of N-acetyl-DL-leucine enantiomers after oral dosing and their clinical relevance. PLUS ONE. 2020;15(2).
Carswell C, Rañopa M, Pal S, MacFarlane R, Siddique D, Thomas D, et al. Video rating in neurodegenerative disease clinical trials: the experience of PRION-1. Dement Geriatr Cogn Disord Extra. 2012;2:286–97.
Handforth A, Ondo WG, Tatter S, Mathern GW, Simpson RK, Walker F, et al. Vagus nerve stimulation for essential tremor: a pilot efficacy and safety trial. Neurology. 2003;61:1401–5.
Quinn J, Moore M, Benson DF, Clark CM, Doody R, Jagust W, et al. A videotaped CIBIC for dementia patients: validity and reliability in a simulated clinical trial. Neurology. 2002;58:433–7.
Lord SE, Halligan PW, Wade DT. Visual gait analysis: the development of a clinical assessment and scale. Clin Rehabil. 1998;12:107–19.
Dunlop BW, Gray J, Rapaport MH. Transdiagnostic clinical global impression scoring for routine clinical settings. Behav Sci [Internet]. 2017 [cited 2020 Feb 15];7. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5618048/.
Schmitz-Hübsch T, Giunti P, Stephenson DA, Globas C, Baliko L, Saccà F, et al. SCA Functional Index: a useful compound performance measure for spinocerebellar ataxia. Neurology. 2008;71:486–92.
Subramony SH. SARA--a new clinical scale for the assessment and rating of ataxia. Nat Clin Pract Neurol. 2007;3:136–7.
EuroQol Group. EQ-5D Instruments | About EQ-5D. 2017. [Internet]. 2017 [cited 2020 Feb 15]. Available from: https://euroqol.org/eq-5d-instruments/eq-5d-5l-about.
Iturriaga C, Pineda M, Fernández-Valero EM, Vanier MT, Coll MJ. Niemann-Pick C disease in Spain: clinical spectrum and development of a disability scale. J Neurol Sci. 2006;249:1–6.
Pineda M, Perez-Poyato MS, O’Callaghan M, Vilaseca MA, Pocovi M, Domingo R, et al. Clinical experience with miglustat therapy in pediatric patients with Niemann-Pick disease type C: a case series. Mol Genet Metab. 2010;99:358–66.
Quinn TJ, Dawson J, Walters MR, Lees KR. Variability in modified Rankin scoring across a large cohort of international observers. Stroke. 2008;39:2975–9.
Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, et al. The Columbia–Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. 2011;168:1266–77.
Yanjanin NM, Vélez JI, Gropman A, King K, Bianconi SE, Conley SK, et al. Linear clinical progression, independent of age of onset, in Niemann-Pick disease, type C. Am J Med Genet Part B Neuropsychiatr Genet. 2010;153B:132–40.
Acknowledgements
We thank each of the study sites and principal investigators participating in the IB1001 clinical trials for their participation outstanding conduct of the studies. We thank the multinational Patient Organizations representing the NPC, GM2, A-T, and related rare-disease communities, for their essential involvement, including the following: NPC Organizations: Australian Niemann-Pick Type C Foundation, Fundación Niemann-Pick de España (Spain), International Niemann-Pick disease Alliance (Worldwide), National Niemann-Pick Disease Foundation (USA), Niemann-Pick Association of Fuenlabrada (Spain), Niemann-Pick Selbsthilfegruppe (Germany), and Niemann-Pick Suisse (Switzerland), Niemann-Pick UK (UK). GM2 Organizations: Acción y Cura para Tay-Sachs (Spain), Associação Nacional D O C E T (Portugal), Cure and Action for Tay-Sachs Foundation (UK), Cure Tay-Sachs Foundation (USA), Hand in Hand gegen Tay-Sachs und Sandhoff (Germany), National Tay-Sachs and Allied Disease Association (USA), and Vaincre les Maladies Lysosomales (France). Ataxia Organizations: Asociación Española Familia Ataxia-Telangiectasia (Spain) Associazione Nazionale A-T (Italy), A-T Children's Project (USA), Ataxia-Telangiectasia Society (UK), Ataxia UK (UK), ATEurope (EU), and National Ataxia Foundation (USA). We thank the National Regulatory Agencies, including the Dutch Medicines Evaluation Board, German Federal Institute for Drugs and Medical Devices, Spanish Agency of Medicines and Medical Products, Slovak Human and Veterinary Medicines Agencies, US Food and Drug Administration, and UK Medicines and Healthcare products Regulatory Agency for their critical collaboration. Without their considerable effort to understand the unique challenges of drug development for NPC, GM2, and A-T patients and actively help define a development program which expedites the availability of promising treatments for these patients, the IB1001 development program would not be feasible. Finally, we are very grateful to all the patients and their families who participated in these studies.
Declarations
N/A
Funding
This study was financially supported by IntraBio (https://intrabio.com). The authors (TF, IB, MF) are officers in IntraBio, and the authors (MP, GB, GCC, SF, MS, AG, UG, R. Kay, TMeyer, FMP, LT, and CV) were paid for consultancy work for IntraBio. Authors, acting in their capacity as consultants for IntraBio, played roles in study design, decision to publish, or preparation of the manuscript. IntraBio is not involved in the data collection and analysis.
Author information
Authors and Affiliations
Contributions
MS conceived the initial studies. MS and TB initiated the initial case series, and FP, AG, GC, and MS initiated the non-clinical studies, together establishing the current study concept and rational. All authors made contributions to the conception and/or the trial design. TF and RKay conceptualized the novel primary outcome assessment, and MP, MS, IB, WD, WE, JG, DP, RK, DL, TM, and MF made substantial contributions to the design of the CI-CS. TF and MS wrote and revised the study protocol. MP, TB, IB, UG, RK, TMeyer, and LT made contributions to the study protocol and revised the final protocol for content. RKay has the main responsibility for statistical analyses and made substantial contributions to the study protocol. GB had the main responsibility for medical monitoring and pharmacovigilance oversight and made substantial contributions to the study protocol. CV and SF had the main responsibility for study conduct and made substantial contributions to the study protocol. TF, MF, UG, TMeyer, CV, and SF contributed decisively to ethics approval to ethics and regulatory authorities. MF is the sponsor’s delegated person. MS is the sponsor’s delegated clinician. TF, SF, and CV are responsible for the implementation of the study. TF and MS wrote and revised the manuscript. RKay developed the statistical concept and performed the sample size calculation. MP, GB, IB, FP, and WE revised the final manuscript for content. All authors read and approved the final manuscript.
Authors’ information
M. Strupp is Joint Chief Editor of the Journal of Neurology, Editor in Chief of Frontiers of Neuro-otology and Section Editor of F1000.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The studies have been approved by the responsible central research ethics committees/institutional review boards, including the Ethics Committee of Ludwig Maximilian University of Munich (19-135; 19-119; 20-079), National Institute of Child Diseases Bratislava Ethics Committee (EudraCT 2018-004431-71), Bellvitge Hospital University Clinical Research Ethics Committee (AC001/19; AC004/19), Hospital University La Paz (5621); East Midlands – Derby Research Ethics Committee (259038), North West- Greater Manchester South Research Ethics Committee (260774), Office for Research Ethics Committees Northern Ireland (260363), Mayo Clinic Institutional Review Board (18-011974; 19-000373), Office of Science and Research Institutional Review Board, New York University School of Medicine (i17-01666), and University of California Los Angeles Institutional Review Board (19-000348; 19-000442).
Informed consent will be obtained for all study participants.
Consent for publication
Not applicable.
Competing interests
MF is a co-founder, shareholder, and Chairman of IntraBio. TF and IB are officers and shareholders of IntraBio. FP is a cofounder, shareholder, and consultant to IntraBio and consultant to Actelion and Orphazyme. MS is a shareholder to IntraBio, and consultant for Abbott, Actelion, AurisMedical, Heel, IntraBio and Sensorion; he has received speaker’s honoraria from Abbott, Actelion, Auris Medical, Biogen, Eisai, Grünenthal, GSK, Henning Pharma, Interacoustics, Johnson & Johnson, MSD, Otometrics, Pierre-Fabre, TEVA, UCB. He is the distributor of M-glasses and positional vertigo App. AG and GC are cofounders, shareholders, and consultants to IntraBio. MP is a shareholder of IntraBio and has received consulting fees, honoraria, and research grants from Actelion Pharmaceuticals Ltd. and Biomarin. CV and SF are consultants and shareholders of IntraBio. UG, TM, GB, and RKay are consultants to IntraBio. TBE received honoraria for lecturing from Actelion and Sanofi Genzyme.
IntraBio owns patents EP3359146 and EP3416631 (related to treatment of lysosomal storage disorders and neurodegenerative diseases with acetyl-leucine and its analogues).
IntraBio has pending patent applications EP19174007.5, EP3482754, PCT/US2018/056420, PCT/US2018/018420, PCT/IB2018/054676, PCT/IB2019/051214, PCT/IB2017/054928, PCT/GB2017/051090, PCT/IB2017/054929, USPTO 62/812,987, USPTO 62/842,296, USPTO 62/888,894, USPTO 62/895,144, USPTO 62/868,383, USPTO 62/931,003, USPTO 62/960,637, and PCT/IB2019/060525 relating to treatment of lysosomal storage disorders, neurodegenerative diseases, and neurodegeneration with acetyl-leucine and its analogues.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Material I.
Video Acquisition, Submission, and Review. Supplementary Material II. Safety Parameters. Supplementary Material III. Data Collection.
Additional file 2: Supplementary Table 1.
Parent Study schedule of enrolment, interventions, and assessments. Supplementary Table 2. Extension Phase schedule of enrolment, interventions, and assessments.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fields, T., Patterson, M., Bremova-Ertl, T. et al. A master protocol to investigate a novel therapy acetyl-l-leucine for three ultra-rare neurodegenerative diseases: Niemann-Pick type C, the GM2 gangliosidoses, and ataxia telangiectasia. Trials 22, 84 (2021). https://doi.org/10.1186/s13063-020-05009-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13063-020-05009-3