Abstract
Delirium, a form of acute cerebral dysfunction, is a common complication of postoperative cardiac surgery in children. It is strongly associated with adverse outcomes, including prolonged hospitalization, increased mortality, and cognitive dysfunction. This study aimed to identify risk factors and incidence of delirium after cardiac surgery in children to facilitate early identification of delirium risk and provide a reference for the implementation of effective prevention and management. A systematic literature search was conducted in PubMed, Web of Science, Embase, Cochrane Library, Scopus, CNKI, Sinomed, and Wanfang for studies published in English or Chinese from the inception of each database to November 2023. The PRISMA guidelines were followed in all phases of this systematic review. The Risk of Bias Assessment for Nonrandomized Studies tool was used to assess methodological quality. A total of twelve studies were included in the analysis, with four studies classified as overall low risk of bias, seven studies as moderate risk of bias, and one study as high risk of bias. The studies reported 39 possible predictors of delirium, categorized into four broad groups: intrinsic and parent-related factors, disease-related factors, surgery and treatment-related factors, and clinical scores and laboratory parameters. By conducting qualitative synthesis and quantitative meta-analysis, we identified two definite factors, four possible factors, and 32 unclear factors related to delirium. Definite risk factors included age and mechanical ventilation duration. Possible factors included developmental delay, cyanotic heart disease, cardiopulmonary bypass time, and pain score. With only a few high-quality studies currently available, well-designed and more extensive prospective studies are still needed to investigate the risk factors affecting delirium and explore delirium prevention strategies in high-risk children.
Similar content being viewed by others
Introduction
Congenital heart disease (CHD) is the commonest birth defect worldwide, affecting millions of newborns annually [1,2,3]. The actual prevalence is difficult to determine because not all patients with CHD are diagnosed early. A recent systematic review integrating 260 studies showed that the birth prevalence of CHD globally continued to rise between 1970 and 2017, increasing by 10% every 5 years [4]. With the improvement of medical technology, anesthesia, and extracorporeal circulation, the diagnosis and treatment of CHD have become increasingly sophisticated, and the types of diseases treated have gradually become more complex. Surgery is still the most important and effective treatment for children with CHD, which improves the survival rate of children but may also bring a series of postoperative complications [5]. Delirium is one of the common postoperative complications, with an incidence rate of 9.8%-68% in children undergoing cardiac surgery [6,9]. Despite its typically transient nature, delirium is strongly associated with adverse outcomes, including prolonged hospitalization, increasing potential mortality, impact on prognosis, causing long-term cognitive dysfunction, and differentially affecting the quality of life of the child after discharge from the hospital [10,11,12,13]. From an economic perspective, the diagnosis of delirium in children increases medical and healthcare costs [14]. Therefore, prevention has emerged as a pivotal focus of current clinical research.
Identifying risk factors for delirium is crucial for its early identification and prevention, which can effectively decrease its incidence in children. However, there is limited research on delirium after cardiac surgery in children, and the independent risk factors for delirium varied in previous studies. The risk factors and prevalence of delirium have yet to be well established. Therefore, this study aimed to determine the potential risk factors and prevalence of delirium after cardiac surgery in children, to provide a reference for the early clinical identification of high-risk groups, and the implementation of effective prevention and management.
Methods
The review followed the PRISMA reporting guidelines, a 27-item list designed to improve the reporting of systematic evaluations [15], and was registered with PROSPERO (registration number: CRD42023475618). All relevant analyses were based on previously published studies and did not require ethical approval or patient consent.
Search strategy
A systematic literature search was conducted in PubMed, Web of Science, Embase, Cochrane Library, Scopus, China National Knowledge Infrastructure (CNKI), Sinomed, and Wanfang for studies that were published in English or Chinese from the inception of each database to November 2023 using keywords, Medical Subject Headings (MeSH), and other index terms, as well as combinations of these terms and appropriate synonyms. The search terms focused on “cardiac surgical procedures,” “thoracic surgical procedures,” “heart surgery,” “cardiac surgery,” “delirium,” “agitation,” “emergence delirium,” “postoperative delirium,” “child,” “pediatrics,” “children,” “neonate,” and their synonyms (see the Supplementary Material for the complete search strategy). Additionally, we manually searched the reference lists of all selected studies for any further relevant studies meeting our inclusion criteria.
Inclusion criteria
-
• Pediatric cardiac surgery patients younger than 18 were the primary study population.
-
• Postoperative delirium is the primary outcome indicator, and risk factors for delirium are the primary research objective.
-
• Reported at least one statistically significant risk factor for postoperative delirium.
-
• Published in English or Chinese.
Exclusion criteria
-
• Repeatedly published studies.
-
• Abstracts, clinical trial registries, and medical record reports.
-
• Conference proceedings, review articles, letters, and editorials.
-
• Animal or in vitro studies.
-
• Incomplete data or inability to extract relevant data.
-
• The original article could not be found by any means.
Data extraction
Two reviewers extracted the data using a pre-designed Microsoft Excel 2019 spreadsheet. The extraction procedure was conducted independently, and disputes were mediated by a third senior reviewer when necessary. Data were collected on the following characteristics for each included study.
-
(1)
Basic information: first author, country, year of publication, study duration, and study design.
-
(2)
Demographic characteristics: study population, sample size, number and rate of delirium.
-
(3)
Delirium-related features: measurement method and frequency.
-
(4)
Potential risk factors for delirium: for each risk factor, adjusted or unadjusted odds ratios (OR) or relative risks (RR) were recorded when available. If not explicitly reported, OR and 95% confidence interval (CI) were calculated with a 2 × 2 table using the number of patients with and without a given risk factor.
Quality assessment
Two reviewers independently assessed the study’s methodological quality, and disagreements were settled by consensus through a panel discussion. The risk of bias for each included study was assessed using the Risk of Bias Assessment for Nonrandomized Studies tool [16]. This tool was selected because of the nonrandomized nature of all included studies as well as its ability to evaluate six domains of risk of bias, including 1) selection of participants, 2) confounding variables, 3) measurement of exposure, 4) blinding of outcome assessments, 5) incomplete outcome data, and 6) selective outcome reporting. If the study received low risk ratings for each of the six evaluated domains, the risk of bias would be low. If at least one domain were rated to have an unclear risk (but no domains were rated to have a high risk), the study would be at moderate risk of bias, and if at least one domain were rated as having a high risk, the study would be at high risk of bias.
A third reviewer extracted data from five randomly selected studies and examined for methodological quality and bias risk to ensure the correctness of the assessment.
Qualitative synthesis and quantitative meta-analysis
Each reported risk factor was synthesized qualitatively. The total number of low and moderate risk of bias studies and the percentage of studies showing positive correlation were used to mark them as definite, likely, unclear, or not a risk factor (Table 1). For risk factors with sufficiently homogeneous definitions and reference ranges, a quantitative meta-analysis of low and moderate risk of bias studies was implemented to estimate a combined OR.
Data analysis was performed using Revman5.4 software provided by the Cochrane Collaboration Network. The generic inverse variance method was used for the meta-analysis of both risk factors and the incidence of delirium after cardiac surgery in children [17]. This method requires only effect estimates and their Standard Errors (SEs). The SEs were estimated by back transforming the 95% confidence limits using the standard normal distribution. The included studies were tested for heterogeneity (I2 test), if P ≥ 0.05 and I2 < 50%, this indicated less heterogeneity among studies and a fixed-effects model was selected for statistical analysis of the data, while conversely P < 0.05 or I2 ≥ 50% indicated greater heterogeneity among studies and a random-effects model was used.
Results
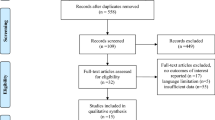
A total of 5141 articles were identified through a literature search of the databases, of which 1623 duplicates were removed. After screening the remaining 3518 articles for title and abstract, 46 were selected for full-text retrieval. Following the eligibility assessment, 11 articles were found to meet the inclusion criteria. The references of the selected articles were also checked, and a full-text search was performed on nine articles, including one article that met the eligibility criteria. Ultimately, 12 articles were identified for article inclusion in this review, with 11 studies contributing to qualitative synthesis and quantitative meta-analysis. Study identification is summarized in Fig. 1.
Of these studies, nine were prospective studies [6,7,8, 10, 18,19,20,21,22], and the remaining three studies were retrospective [23,24,25], with one being a multicenter studies [8] and 11 being single-center studies. The sample size ranged from 18 to 470, with the two largest studies including 470 children [20] and 327 children [7], respectively. One of these studies constructed clinical prediction models [20]. The basic characteristics of the included literature are given in Table 1.
Incidence of delirium and measurement method
The combined incidence of delirium was 39.0% (95% CI: 28.6–50.2%). The heterogeneity was high (I2 = 95%). The combined incidence of delirium was 40.8% (95% CI: 27.0–56.9%; I2 = 92%) in female children and 45.1% (95% CI: 29.6–61.2%; I2 = 94%) in male children. (Fig. S1-3 in the Supplementary material).
Two studies used the Pediatric Anesthesia Emergence Delirium (PAED) scale [26] to assess delirium in children. The scale was developed by Sikich et al. in 2004 includes five items: (1) The child makes eye contact with the caregiver, (2) the child’s actions are purposeful, (3) the child is aware of his/her surroundings, (4) the child is restless, and (5) the child is inconsolable. Items 1, 2, and 3 are reverse-scored as follows: 4, not at all; 3, just a little; 2, quite a bit; and 1, very much; 0, extremely. Items 4 and 5 are scored as follows: 0, not at all; 1, just a little; 2 quite a bit; 3, very much; and 4, extremely. A total PAED scale score was calculated by summing the scores of each item, with higher scores indicating more severe delirium. Children with a PAED score ≥ 10 were considered to have emergence delirium.
Ten studies assessed delirium in children using the Cornell Assessment of Pediatric Delirium (CAPD) scale, an instrument developed by Silver et al. for assessing delirium in patients aged 0–21 years [27]. The CAPD scale has eight items: (1) eye contact with the caregiver, (2) purposeful actions, (3) awareness of surroundings, (4) ability to communicate needs and wants, (5) restlessness, (6) difficulty calming, (7) underactive, and (8) long time to respond to interactions. Each item is scored on a scale of 0 to 4, with the fewer symptoms and behaviors from items 1–4, the higher the score. The more symptoms and behaviors from items 5–8, the higher the score. A child with a total score of ≥ 9 points is diagnosed with delirium.
Quality of included studies
The included studies differed in their methodological quality (Fig. 2, and Fig. S4 in the Supplementary material). Four studies were classified as low risk in all six domains and were considered to be at an overall low risk of bias. One study was considered to be at overall high risk of bias, associated with confounding variables. The remaining seven studies had at least one unclear risk in six domains and were categorized as having a moderate risk of bias.
Risk factors of delirium in included studies
The 12 included studies describe 39 statistically significant risk factors for delirium. These variables were divided into four major categories: intrinsic and parent-related factors (12.8%, 5/39); disease-related factors (18.0%, 7/39); surgery and treatment-related factors (48.7, 19/39) and clinical scores and laboratory parameters (20.5%, 8/39). Details of the risk factors identified in each study are presented in Table 2.
Two variables were found to be definite risk factors for delirium, based on either all low and moderate risk of bias studies showing a positive association (if at least three studies) or the majority of low and moderate risk of bias studies showing a positive association (if at least five studies). Definite risk factors included age and mechanical ventilation duration. Four variables were considered likely associated with delirium, and these included being of developmental delay, cyanotic heart disease, cardiopulmonary bypass (CPB) time, and pain score. 32 variables that showed conflicting results in studies with low and moderate risk of bias, or were positive in only one study, that were considered to have an unclear association with delirium (see Table 2 for specific variables). In addition, sufentanil was considered a non-risk factor.
Meta-analysis was performed for risk factors with at least two low or moderate risk of bias studies demonstrating homogeneous risk factor definitions and reference ranges (Figs. 3, 4, 5 and 6).
Meta-analysis of intrinsic factors. Forest plots of odds ratios (ORs) that were included in the quantitative meta-analysis and the associated overall ORs. For each OR, the size of the red square region is proportional to the corresponding study weight. Diamond shapes intervals represent the overall ORs. I2 represents the fraction of variability among the individual ORs that cannot be explained by sampling variability
Discussion
Our study was the first systematic review of risk factors for delirium after cardiac surgery in children. Based on the inclusion of 12 studies in the current meta-analysis, involving a total of 1976 patients, the pooled prevalence of delirium is 39.0%. By conducting a qualitative synthesis of 39 predictors and a quantitative meta-analysis of 13 factors, we identified two definite factors, four possible factors, and 32 unclear factors related to delirium. The definite factors included age and mechanical ventilation duration, while the possible factors included developmental delay, cyanotic heart disease, CPB time, and pain score. The results of our systematic review present an up-to-date comprehensive summary of the latest evidence, which can provide information for early identification of high-risk delirium after pediatric cardiac surgery and the development of interventions to reduce and prevent delirium.
The pathophysiology of delirium is not fully understood, but several theories have been put forth to explain the neuropsychiatric disturbances. Possible etiologic factors include brain changes revealed by neuroimaging, sepsis-related inflammation, genetics, biomarkers, and neurotransmitters [28,29,30]. The incidence of delirium in children after cardiac surgery is generally higher than in the group of nonsurgical children in the intensive care unit, which may be attributed to the correlation between the severity of the disease and delirium in children [31]. In comparison to nonsurgical critically ill children, children who undergo cardiac surgery exhibit more pronounced characteristics of critical illness, including specific risks such as preoperative hypoxemia, neurodevelopmental abnormalities, fluid overload, electrolyte disorders, and hypothermia [32]. Additionally, the extracorporeal circulation techniques commonly employed in pediatric cardiac surgery may induce extensive endothelial cell activation, systemic inflammatory response, and thromboembolic events [33], which in turn lead to brain damage and inflammation, hence the higher incidence of delirium in children after cardiac surgery [10, 22, 34]. Delirium can lead to prolongation of hospitalization, increased healthcare costs, impaired cognitive function, and higher mortality, causing immediate and long-term harm to patients. Hence, early identification of delirium helps healthcare professionals to take preventive and therapeutic measures as early as possible to reduce the adverse effects of delirium.
Our findings align with previous research indicating that age is the most critical risk factor affecting delirium [6, 22]. Furthermore, due to the challenge faced by evaluators in determining whether the level of consciousness and cognition of children with developmental delays is altered compared to their baseline conditions, more precise tools are needed to assess the interaction between developmental delay and delirium. Lyu et al. [19]. demonstrated that the risk of delirium in male children was 2.127 times higher than in female children. Similarly, a study by Alvarez et al. [10] indicated a higher probability of delirium in male children. However, other studies have not found a significant association between gender and the occurrence of delirium [6, 8, 18, 22, 24]. Moreover, the European Society of Anesthesiology evidence-based and consensus guidelines on postoperative delirium do not recommend gender as a risk factor for delirium [36]. Therefore, further research is warranted to expand the scope of studies and explore the relationship between gender and delirium.
Diseases and adverse conditions are not only the major cause of prolonged hospitalization and even death in children but may also be important risk factors for delirium. The increased risk of delirium in children with cyanotic heart disease may be due to the effects of prolonged chronic hypoxia, oxidative stress, blood transfusions, and poor nutritional status, all of which may independently act as predisposing factors for delirium [37, 38]. The majority of patients admitted to the pediatric cardiac intensive care unit (PCICU) after cardiac surgery are under 3 years of age [39], an age when neurocognitive development is rapid and healthy sleep is critical. Sleep disturbances are recognized as a potential risk factor for the development of delirium, and children with delirium frequently exhibit disrupted sleep patterns. Data from a study by Gregory et al. suggested that the majority of children in the PCICU had severe sleep disturbances [18]. It is necessary to further explore the importance of improving postoperative sleep status in children undergoing cardiac surgery, as well as the feasibility of continuous dynamic monitoring of sleep in the ICU environment. In addition, one study showed that preoperative lung infections and postoperative complications were risk factors for delirium [20].
The strengths of this systematic review include the systematic approach to identifying all publications containing risk factors for delirium after pediatric cardiac surgery and the division of risk factors into four major categories to provide a logical progression of possible factors of delirium. Nevertheless, the results of this systematic review and meta-analysis must take into account several limitations. First, the vast majority of studies were single-center studies, and most were conducted in the United States and China, which may limit their generalizability. Second, there is a lack of standardization in screening for delirium, and the CAPD is usually done by day shift nurses. Consequently, children with nighttime-only delirium may go undetected, which may lead to an underestimate of the true incidence and duration of delirium. Furthermore, despite the comprehensive and rigorous search strategy employed, it is possible that some studies may have been inadvertently overlooked. Lastly, and most importantly, our pooled analyses describe associations between specific factors and the odds of develo** delirium, but these observations do not establish causality.
Conclusions
In summary, we identified several of the most critical factors affecting delirium in our published studies, including age, mechanical ventilation duration, developmental delay, cyanotic heart disease, CPB time, and pain score. However, none of the included studies considered the impact of sociodemographic factors (e.g., family income), skill level of the intensive care unit team, and level of environmental management (e.g., light and sound exposure) on delirium. Therefore, future research should focus on well-designed and extensive prospective studies to investigate the risk factors associated with delirium and explore prevention strategies for high-risk children.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CHD:
-
Congenital heart disease
- CNKI:
-
China National Knowledge Infrastructure
- OR:
-
Odds ratios
- RR:
-
Relative risks
- CI:
-
Confidence interval
- SEs:
-
Standard Errors
- I2 :
-
Heterogeneity
- PAED:
-
Pediatric Anesthesia Emergence Delirium
- CAPD:
-
Cornell Assessment of Pediatric Delirium
- CPB:
-
Cardiopulmonary bypass
- CNS:
-
Central nervous system
- PCICU:
-
Pediatric cardiac intensive care unit
- Dex:
-
Dexmedetomidine
- RACHS-1 score:
-
Risk Adjustment in Congenital Heart Surgery-1 score
- STS-EACTS:
-
Society of Thoracic Surgeons and the European Association for Cardiothoracic Surgery Congenital Heart Surgery Mortality Score
- (PRISM) III:
-
Pediatric Risk of Mortality III
- PAH:
-
Pulmonary arterial hypertension
- rScO2:
-
Regional cerebral oxygen saturation
- NSE:
-
Neuron-specific enolase
- SBS:
-
State Behavioral Scale scores
- EMCO:
-
Extracorporeal membrane oxygenation
- VSD:
-
Ventricular septal defect
References
Zeng X, An J, Lin R, Dong C, Zheng A, Li J, et al. Prediction of complications after paediatric cardiac surgery. Eur J Cardiothorac Surg. 2020;57(2):350–8. https://doi.org/10.1093/ejcts/ezz198.
Pierpont ME, Brueckner M, Chung WK, Garg V, Lacro RV, McGuire AL, et al. Genetic basis for congenital heart disease: revisited: a scientific statement from the American Heart Association. Circulation. 2018;138(21):e653–711. https://doi.org/10.1161/cir.0000000000000606.
Rossano JW. Congenital heart disease: a global public health concern. Lancet Child Adolesc Health. 2020;4(3):168–9. https://doi.org/10.1016/s2352-4642(19)30429-8.
Liu Y, Chen S, Zühlke L, Black GC, Choy MK, Li N, et al. Global birth prevalence of congenital heart defects 1970–2017: updated systematic review and meta-analysis of 260 studies. Int J Epidemiol. 2019;48(2):455–63. https://doi.org/10.1093/ije/dyz009.
Ma XJ, Huang GY. Current status of screening, diagnosis, and treatment of neonatal congenital heart disease in China. World J Pediatr. 2018;14(4):313–4. https://doi.org/10.1007/s12519-018-0174-2.
Köditz H, Drouche A, Dennhardt N, Schmidt M, Schultz M, Schultz B. Depth of anesthesia, temperature, and postoperative delirium in children and adolescents undergoing cardiac surgery. BMC Anesthesiol. 2023;23(1):148. https://doi.org/10.1186/s12871-023-02102-3.
Yang J, Wang J, Zhao L, **ao J. Current status and influencing factors of delirium after extracorporeal circulation in children with congenital heart disease. China Health Statistics. 2021;38(06):923–5 (in Chinese).
Staveski SL, Pickler RH, Khoury PR, Ollberding NJ, Donnellan AL, Mauney JA, et al. Prevalence of ICU Delirium in Postoperative Pediatric Cardiac Surgery Patients. Pediatr Crit Care Med. 2021;22(1):68–78. https://doi.org/10.1097/pcc.0000000000002591.
Battle DE. Diagnostic and Statistical Manual of Mental Disorders (DSM). Codas. 2013;25(2):191–2. https://doi.org/10.1590/s2317-17822013000200017.
Alvarez RV, Palmer C, Czaja AS, Peyton C, Silver G, Traube C, et al. Delirium is a common and early finding in patients in the pediatric cardiac intensive care unit. J Pediatr. 2018;195:206–12. https://doi.org/10.1016/j.jpeds.2017.11.064.
Dervan LA, Di Gennaro JL, Farris RWD, Watson RS. Delirium in a tertiary PICU: risk factors and outcomes. Pediatr Crit Care Med. 2020;21(1):21–32. https://doi.org/10.1097/pcc.0000000000002126.
Trogrlić Z, van der Jagt M, Lingsma H, Gommers D, Ponssen HH, Schoonderbeek JFJ, et al. Improved guideline adherence and reduced brain dysfunction after a multicenter multifaceted implementation of ICU delirium guidelines in 3,930 patients. Crit Care Med. 2019;47(3):419–27. https://doi.org/10.1097/ccm.0000000000003596.
Dechnik A, Traube C. Delirium in hospitalised children. Lancet Child Adolesc Health. 2020;4(4):312–21. https://doi.org/10.1016/s2352-4642(19)30377-3.
Koch S, Stegherr AM, Rupp L, Kruppa J, Prager C, Kramer S, et al. Emergence delirium in children is not related to intraoperative burst suppression - prospective, observational electrography study. BMC Anesthesiol. 2019;19(1):146. https://doi.org/10.1186/s12871-019-0819-2.
Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162(11):777–84. https://doi.org/10.7326/m14-2385.
Kim SY, Park JE, Lee YJ, Seo HJ, Sheen SS, Hahn S, et al. Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. J Clin Epidemiol. 2013;66(4):408–14. https://doi.org/10.1016/j.jclinepi.2012.09.016.
Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1(2):97–111. https://doi.org/10.1002/jrsm.12.
Gregory JL, Brown AT, Kudchadkar SR. characterizing sleep disruption and delirium in children after cardiac surgery: a feasibility study. Pediatr Crit Care Med. 2021;22(11):988–92. https://doi.org/10.1097/pcc.0000000000002777.
Lyu J, Jia Y, Yan M, Zhao Y, Liu Y, et al. Risk factors for postoperative delirium in children with congenital heart disease: a prospective nested case-control study. Chin J Contemp Pediatr. 2022;24(03):232–9 ((in Chinese)).
Mao D, Fu L, Zhang W. Risk factors and nomogram model of postoperative delirium in children with congenital heart disease: a single-center prospective study. Pediatr Cardiol. 2023. https://doi.org/10.1007/s00246-023-03297-5.
Matsuishi Y, Hoshino H, Enomoto Y, Shimojo N, Matsubara M, Kato H, et al. Pediatric delirium is associated with increased brain injury marker levels in cardiac surgery patients. Sci Rep. 2022;12(1):18681. https://doi.org/10.1038/s41598-022-22702-2.
Patel AK, Biagas KV, Clarke EC, Gerber LM, Mauer E, Silver G, et al. Delirium in children after cardiac bypass surgery. Pediatr Crit Care Med. 2017;18(2):165–71. https://doi.org/10.1097/pcc.0000000000001032.
Jiang L, Ding S, Yan H, Li Y, Zhang L, Chen X, et al. A retrospective comparison of dexmedetomidine versus midazolam for pediatric patients with congenital heart disease requiring postoperative sedation. Pediatr Cardiol. 2015;36(5):993–9. https://doi.org/10.1007/s00246-015-1110-z.
Liu JF, Zhou SJ, Chen XH, Cao H, Chen Q. Effect of optimizing regional cerebral oxygen saturation during infant cardiac surgery on the incidence of postoperative delirium: a retrospective study. Ann Thorac Cardiovasc Surg. 2023. https://doi.org/10.5761/atcs.oa.23-00057.
Xu N, Chen Q, Huang ST, Sun KP, Cao H. Sufentanil reduces emergence delirium in children undergoing transthoracic device closure of VSD After sevoflurane-based cardiac anesthesia. Braz J Cardiovasc Surg. 2020;35(5):660–5. https://doi.org/10.21470/1678-9741-2019-0334.
Sikich N, Lerman J. Development and psychometric evaluation of the pediatric anesthesia emergence delirium scale. Anesthesiology. 2004;100(5):1138–45. https://doi.org/10.1097/00000542-200405000-00015.
Silver G, Traube C, Kearney J, Kelly D, Yoon MJ, Nash Moyal W, et al. Detecting pediatric delirium: development of a rapid observational assessment tool. Intensive Care Med. 2012;38(6):1025–31. https://doi.org/10.1007/s00134-012-2518-z.
Slooter AJ, Van De Leur RR, Zaal IJ. Delirium in critically ill patients. Handb Clin Neurol. 2017;141:449–66. https://doi.org/10.1016/b978-0-444-63599-0.00025-9.
Meagher DJ, Trzepacz PT. Motoric subtypes of delirium. Semin Clin Neuropsychiatry. 2000;5(2):75–85. https://doi.org/10.153/SCNP00500075.
Bryant KJ. Pediatric Delirium in the Cardiac Intensive Care Unit: Identification and Intervention. Crit Care Nurse. 2018;38(4):e1–7. https://doi.org/10.4037/ccn2018947.
Schieveld JN, Lousberg R, Berghmans E, Smeets I, Leroy PL, Vos GD, et al. Pediatric illness severity measures predict delirium in a pediatric intensive care unit. Crit Care Med. 2008;36(6):1933–6. https://doi.org/10.1097/CCM.0b013e31817cee5d.
Leroy PL, Schieveld JN. Mind the heart: delirium in children following cardiac surgery for congenital heart disease. Pediatr Crit Care Med. 2017;18(2):196–8. https://doi.org/10.1097/pcc.0000000000001038.
Whiting D, Yuki K, DiNardo JA. Cardiopulmonary bypass in the pediatric population. Best Pract Res Clin Anaesthesiol. 2015;29(2):241–56. https://doi.org/10.1016/j.bpa.2015.03.006.
Meyburg J, Dill ML, Traube C, Silver G, von Haken R. Patterns of postoperative delirium in children. Pediatr Crit Care Med. 2017;18(2):128–33. https://doi.org/10.1097/pcc.0000000000000993.
Maldonado JR. Neuropathogenesis of delirium: review of current etiologic theories and common pathways. Am J Geriatr Psychiatry. 2013;21(12):1190–222. https://doi.org/10.1016/j.jagp.2013.09.005.
Aldecoa C, Bettelli G, Bilotta F, Sanders RD, Audisio R, Borozdina A, et al. European Society of Anaesthesiology evidence-based and consensus-based guideline on postoperative delirium. Eur J Anaesthesiol. 2017;34(4):192–214. https://doi.org/10.1097/eja.0000000000000594.
Siegel EJ, Traube C. Pediatric delirium: epidemiology and outcomes. Curr Opin Pediatr. 2020;32(6):743–9. https://doi.org/10.1097/mop.0000000000000960.
Patel AK, Bell MJ, Traube C. Delirium in pediatric critical care. Pediatr Clin North Am. 2017;64(5):1117–32. https://doi.org/10.1016/j.pcl.2017.06.009.
Kudchadkar SR, Nelliot A, Awojoodu R, Vaidya D, Traube C, Walker T, et al. Physical rehabilitation in critically ill children: a multicenter point prevalence study in the United States. Crit Care Med. 2020;48(5):634–44. https://doi.org/10.1097/ccm.0000000000004291.
Rudolph JL, Inouye SK, Jones RN, Yang FM, Fong TG, Levkoff SE, et al. Delirium: an independent predictor of functional decline after cardiac surgery. J Am Geriatr Soc. 2010;58(4):643–9. https://doi.org/10.1111/j.1532-5415.2010.02762.x.
Horvath R, Shore S, Schultz SE, Rosenkranz ER, Cousins M, Ricci M. Cerebral and somatic oxygen saturation decrease after delayed sternal closure in children after cardiac surgery. J Thorac Cardiovasc Surg. 2010;139(4):894–900. https://doi.org/10.1016/j.jtcvs.2009.06.013.
Mao D, Fu L, Zhang W. Construction and validation of an early prediction model of delirium in children after congenital heart surgery. Transl Pediatr. 2022;11(6):954–64. https://doi.org/10.21037/tp-22-187.
Koster S, Hensens AG, van der Palen J. The long-term cognitive and functional outcomes of postoperative delirium after cardiac surgery. Ann Thorac Surg. 2009;87(5):1469–74. https://doi.org/10.1016/j.athoracsur.2009.02.080.
Pan W, Wang Y, Lin L, Zhou G, Hua X, Mo L. Outcomes of dexmedetomidine treatment in pediatric patients undergoing congenital heart disease surgery: a meta-analysis. Paediatr Anaesth. 2016;26(3):239–48. https://doi.org/10.1111/pan.12820.
Riker RR, Shehabi Y, Bokesch PM, Ceraso D, Wisemandle W, Koura F, et al. Dexmedetomidine vs midazolam for sedation of critically ill patients: a randomized trial. JAMA. 2009;301(5):489–99. https://doi.org/10.1001/jama.2009.56.
Smith HAB, Besunder JB, Betters KA, Johnson PN, Srinivasan V, Stormorken A, et al. 2022 Society of critical care medicine clinical practice guidelines on prevention and management of pain, agitation, neuromuscular blockade, and delirium in critically ill pediatric patients with consideration of the ICU environment and early mobility. Pediatr Crit Care Med. 2022;23(2):e74–110. https://doi.org/10.1097/pcc.0000000000002873.
Motta E, Luglio M, Delgado AF, Carvalho WB. Importance of the use of protocols for the management of analgesia and sedation in pediatric intensive care unit. Rev Assoc Med Bras (1992). 2016;62(6):602–9. https://doi.org/10.1590/1806-9282.62.06.602.
Kang X, Tang X, Yu Y, Bao F, Gan S, Zheng W, et al. Intraoperative dexmedetomidine infusion is associated with reduced emergence agitation and improved recovery profiles after lung surgery: a retrospective cohort study. Drug Des Devel Ther. 2019;13:871–9. https://doi.org/10.2147/dddt.S195221.
Simonini A, Brogi E, Conti G, Vittori A, Cascella M, Calevo MG. Dexmedetomidine reduced the severity of emergence delirium and respiratory complications, but increased intraoperative hypotension in children underwent tonsillectomy. A retrospective analysis. Minerva Pediatr (Torino). 2021. https://doi.org/10.23736/s2724-5276.21.06330-8.
Mantz J, Josserand J, Hamada S. Dexmedetomidine: new insights. Eur J Anaesthesiol. 2011;28(1):3–6. https://doi.org/10.1097/EJA.0b013e32833e266d.
Dahmani S, Delivet H, Hilly J. Emergence delirium in children: an update. Curr Opin Anaesthesiol. 2014;27(3):309–15. https://doi.org/10.1097/aco.0000000000000076.
Matute Crespo M, Montero MA. Pharmacological advances in the multimodal management of perioperative analgesia. Rev Esp Anestesiol Reanim. 2017;64(8):467–71. https://doi.org/10.1016/j.redar.2017.03.006.
Maclullich AM, Ferguson KJ, Miller T, de Rooij SE, Cunningham C. Unravelling the pathophysiology of delirium: a focus on the role of aberrant stress responses. J Psychosom Res. 2008;65(3):229–38. https://doi.org/10.1016/j.jpsychores.2008.05.019.
Cano Londoño EM, Mejía Gil IC, Uribe Hernández K, Alexandra Ricardo Ramírez C, Álvarez Gómez ML, Consuegra Peña RA, et al. Delirium during the first evaluation of children aged five to 14 years admitted to a paediatric critical care unit. Intensive Crit Care Nurs. 2018;45:37–43. https://doi.org/10.1016/j.iccn.2017.12.010.
Paterson RS, Kenardy JA, De Young AC, Dow BL, Long DA. Delirium in the critically ill child: assessment and sequelae. Dev Neuropsychol. 2017;42(6):387–403. https://doi.org/10.1080/87565641.2017.1374961.
Ista E, van Beusekom B, van Rosmalen J, Kneyber MCJ, Lemson J, Brouwers A, et al. Validation of the SOS-PD scale for assessment of pediatric delirium: a multicenter study. Crit Care. 2018;22(1):309. https://doi.org/10.1186/s13054-018-2238-z.
Acknowledgements
Not applicable.
Funding
This study was supported by the Fundamental Research Funds for the Central Universities (grant number:YCJJ20230244) and Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology Research Fund (grant number:2022C09).
Author information
Authors and Affiliations
Contributions
GY and YL framed the review questions on the basis of input from MF and XX. YY and MF conducted the literature search. MF, WS, and QY screened and evaluated the identified papers. GY and YY performed data extraction. MF, QY and WS prepared the initial manuscript with revisions and comments from GY, YL, and XX. All authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fu, M., Yuan, Q., Yang, Q. et al. Risk factors and incidence of postoperative delirium after cardiac surgery in children: a systematic review and meta-analysis. Ital J Pediatr 50, 24 (2024). https://doi.org/10.1186/s13052-024-01603-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13052-024-01603-2