Abstract
Background
Venous thromboembolism (VTE) prophylaxis is effective in reducing VTE events, however, its impact on mortality is unclear. We examined the association between omission of VTE prophylaxis within the first 24 h after intensive care unit (ICU) admission and hospital mortality.
Methods
Retrospective analysis of prospectively collected data from the Australian New Zealand Intensive Care Society Adult Patient Database. Data were obtained for adult admissions between 2009 and 2020. Mixed effects logistic regression models were used to evaluate the association between omission of early VTE prophylaxis and hospital mortality.
Results
Of the 1,465,020 ICU admissions, 107,486 (7.3%) did not receive any form of VTE prophylaxis within the first 24 h after ICU admission without documented contraindication. Omission of early VTE prophylaxis was independently associated with 35% increased odds of in-hospital mortality (odds ratios (OR): 1.35; 95% CI: 1.31–1.41). The associations between omission of early VTE prophylaxis and mortality varied by admission diagnosis. In patients diagnosed with stroke (OR: 1.26, 95% CI: 1.05–1.52), cardiac arrest (OR: 1.85, 95% CI: 1.65–2.07) or intracerebral haemorrhage (OR: 1.48, 95% CI: 1.19–1.84), omission of VTE prophylaxis was associated with increased risk of mortality, but not in patients diagnosed with subarachnoid haemorrhage or head injury.
Conclusions
Omission of VTE prophylaxis within the first 24 h after ICU admission was independently associated with increased risk of mortality that varied by admission diagnosis. Consideration of early thromboprophylaxis may be required for patients with stroke, cardiac arrest and intracerebral haemorrhage but not in those with subarachnoid haemorrhage or head injury. The findings highlight the importance of individualised diagnosis-related thromboprophylaxis benefit-harm assessments.
Similar content being viewed by others
Background
Venous thromboembolism (VTE) is the leading cause of preventable death in hospitals, a leading contributor to increased length of stay, and is the number one patient safety priority [1, 2]. Globally, there are about 10 million cases of VTE every year, and around 30% of patients with VTE experience recurrence within 10 years [3]. The long-term mortality rate in untreated VTE patients ranges from 12 to 50% [4]. In addition to the impact of VTE on morbidity and mortality, VTE imposes a significant economic burden on patients, their families and the healthcare system [5]. In Australia, more than 17,000 people develop VTE each year, which costs patients and the health system $1.72 billion annually [6]. Although VTE is common in hospital patients, it is more prevalent in critically ill patients due to specific ICU risk factors of VTE, including sedation, immobilization, vasopressors or central venous catheterisation [7].
The use of appropriate VTE prophylaxis reduces the risk of VTE by 50–80% but may increase the risk of bleeding [1, 5, 8]. Current guidelines recommend that all hospital patients should be assessed for VTE risk and most patients should receive appropriate VTE prophylaxis within the first 24 h after admission [6, 9]. However, a significant proportion of patients at risk of having VTE do not receive VTE prophylaxis as recommended in guidelines [5, 10]. There is also considerable variation in VTE prophylaxis use and incident VTE between hospitals in Australia [11, 12] and globally [10], independent of differences in the proportion of patients at risk for VTE. The variation and underuse of VTE prophylaxis have been mainly attributed to uncertainty among clinicians as to how the benefits and risks of anticoagulants weigh up in patients with different risk profiles [13].
The association between delay or omission of VTE prophylaxis and increased risk of VTE is well established [14, 15]. However, current evidence on the association between delay or omission of VTE prophylaxis and mortality is not clear. Some studies [14, 16] have found an association between delay or omission of VTE prophylaxis and increased risk of mortality, whereas other studies reported that there is no association between delay or mission of early VTE prophylaxis and mortality [15, 17, 18]. In a multi-centre registry study of 175,665 critically ill adults, omission of VTE prophylaxis in the first 24 h after ICU admission was associated with 1.22-fold increase in hospital mortality, ranging from 1.07 to 1.88 fold depending on admission diagnosis and pre-existing chronic conditions [16]. However, meta-analyses studies [15, 18] and a large registry study [14] found no statistically significant difference in mortality between early versus late VTE prophylaxis. The extent of mortality attributable to omission of early thromboprophylaxis, and whether adverse outcomes attributable to omission of early thromboprophylaxis differ according to patients’ risk profiles remains unclear. Overall, current guidelines do not provide admission diagnosis specific recommendations for VTE prophylaxis use. The lack of standardised approaches to assess bleeding risk, including in cardiac arrest, intracerebral hemorrhage and stroke patients could influence the decision whether or not to prescribe pharmacological prophylaxis.
The lack of clear evidence between omission of early VTE prophylaxis and mortality has, in part, contributed to weak guideline recommendations and heterogeneity of practice. Larger sampled studies of contemporaneous patients are needed for identifying VTE prophylaxis strategies associated with lower risk of death among critically ill and clinically diverse patient groups. In this study, we investigated the association between omission of VTE prophylaxis and in-hospital mortality in a very large cohort of patients admitted to Intensive Care Units in Australia and New Zealand.
Methods
Data sources and participants
This is a retrospective analysis of data from the Australian and New Zealand Intensive Care Society (ANZICS) Adult Patient Database (APD) run by the ANZICS Centre for Outcome and Resource Evaluation (CORE). The ANZICS APD contains over 3 million patient episodes collected from 221 ICUs, representing about 90% of Australia and New Zealand ICU admissions. Additional details regarding the design and methods of the ANZICS APD study are described elsewhere [19].
The outcome of this study was hospital mortality, which was reported by the contributing ICUs. ICUs reported administration of VTE prophylaxis status within the first 24 h of ICU admission using a standard precoded response: “Yes,” “No,” “Contraindicated,” or “Not indicated.” Early VTE prophylaxis was defined as receiving one or more of the following methods of VTE prophylaxis, including unfractionated heparin, low molecular-weight heparin, pneumatic compression devices, compression stockings, or inferior vena cava filter, within the first 24 h after ICU admission [16, 20]. Omission of early VTE prophylaxis was defined as not receiving any method of VTE prophylaxis within the first 24 h after ICU admission without obvious reasons or contraindications to pharmacologic or mechanical VTE prophylaxis. Patients were considered as “not indicated” for early VTE prophylaxis if they did not receive any form of VTE prophylaxis within the first 24 h after ICU admission because they were assessed to have a very low risk of VTE events by their attending clinicians. VTE prophylaxis was considered contraindicated if patient was at risk of bleeding and had physical injuries to their lower extremities, unless an inferior vena cava filter was inserted within the first 24 h after ICU admission [16].
The analyses were adjusted for risk of hospital mortality estimated using the Australian and New Zealand Risk of Death (ANZROD) model. The ANZROD model has excellent discrimination and good calibration and provides better adjustment for case mix variation [21]. ANZROD is derived from patient and clinical characteristics, including the Acute Physiology and Chronic Health Evaluation (APACHE) III, ICU admission source, admission diagnoses, Acute Physiology score (APS), APACHE III chronic health score, treatment limitation, and ventilation [22].
Data analysis
Demographic and clinical characteristics are presented as means (with SDs) for continuous variables and percentages for categorical variables. We used mixed effects logistic regression modeling (accounting for the random effects of the contributing ICUs) to identify the association between omission of early VTE prophylaxis and hospital mortality overall and stratified according to admission diagnosis and pre-existing chronic conditions. Temporal changes in the association between omission of early VTE prophylaxis and mortality were assessed by including an interaction term between calendar year and VTE prophylaxis in the fully adjusted mixed effects logistic regression. P < 0.05 was considered significant in 2-sided tests. The proportion of missing data was negligible, and therefore, imputation methods were not necessary. Analyses were carried out using Stata version 16 (StataCorp, College Station, TX, USA).
The study was approved by the Alfred Health Human Research Ethics Committee (Project No: 276/21). The ANZICS CORE participating ICUs contribute de-identified data. Contributing ICUs allow subsequent data use as appropriate, understanding procedures and in compliance with the ANZICS CORE terms of reference and with a waiver of the need for informed consent.
Results
Study subjects
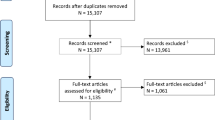
A total of 1,465,020 index admissions of patients aged 18 years or older (median age 65.3 ± 17.5 y, 43.3% females) admitted to 203 ICUs in Australia and New Zealand met the inclusion criteria for the analysis (Fig. 1). Patients with missing data on early thromboprophylaxis (n = 232,595) or hospital mortality (n = 4, 648), and admitted for palliative care or potential organ donation (n = 7,194) were excluded. Patient characteristics by early thromboprophylaxis status are shown in Table 1.
Early VTE prophylaxis and mortality
In total, 1,260,785 (86.1%) of ICU patients received VTE prophylaxis within the first 24 h after ICU admission. Omission of VTE prophylaxis without documented contraindication occurred in 107,486 (7.3%) ICU patients. VTE prophylaxis was contraindicated in 55,025 (3.8%) patients, and not indicated in 41,724 patients (2.9%). The hospital mortality rate in patients with omission of early thromboprophylaxis was higher compared to patients who received early VTE prophylaxis (10.5% vs. 7.1%) despite the former patients had longer hospital lengths of stay and severity of illness scores (Table 1).
Association of omission of early VTE prophylaxis with mortality
In the analysis adjusted for ANZROD, omission of early VTE prophylaxis (odds ratios (OR): 1.35; 95% CI: 1.31–1.40), or contraindications (OR: 1.35; 95% CI: 1.31–1.40) but not no indication (1.22; 95% CI: 0.94–1.14) to VTE prophylaxis was associated with significantly increased odds of hospital death. The increased mortality risk of mortality associated to omission of early VTE prophylaxis was consistent when stratified according to pre-existing chronic conditions (Table 2). After adjusting for ANZROD, the risk of mortality attributable to omission of early VTE prophylaxis varied according to admission diagnosis. In the analyses stratified by admission diagnosis, omission of VTE prophylaxis was associated with 23–85% statistically significant increased odds of mortality, except in patients diagnosed with head trauma (with or without multi trauma) (OR: 1.23; 95% CI: 0.97–1.56) or subarachnoid haemorrhage (OR: 1.09; 95% CI: 0.79–1.50) (Table 3). There was no statistically significant interaction (P-for interaction effect > 0.05) between ICU admission year and VTE prophylaxis on hospital mortality.
Discussion
In this multi-centre registry of more than 1.4 million critically ill patients, omission of early VTE phylaxis without obvious reasons or contraindications to VTE prophylaxis was independently associated with increased risk of mortality. The association between omission of early VTE prophylaxis varied substantially by admission diagnosis. In stroke, cardiac arrest, and intracerebral haemorrhage, omission of early thromboprophylaxis was associated with increased risk of mortality but not in those with subarachnoid haemorrhage or head injury.
There could be several possible reasons for the higher risk of mortality in patients who do not receive early VTE prophylaxis. First, the higher risk of death associated with omission of early VTE prophylaxis could be attributed to the high incidence of VTE and complications in patients at risk of VTE who did not receive VTE prophylaxis [4, 14]. Without appropriate VTE prophylaxis, the overall VTE incidence in medical and general surgery hospitalized patients ranges from 10 to 40%, while it ranges up to 40–60% in major orthopaedic surgery [23], and one in 10 patients who developed hospital-acquired VTE die in hospital [12]. Second, VTE prophylaxis is a key indicator of quality of care for hospitalized patients, and omission of early VTE prophylaxis without obvious reasons or contraindications to pharmacologic or mechanical thromboprophylaxis may reflect gaps in the overall quality of care, including physician awareness, compliance with guidelines for VTE prophylaxis [24, 25]. Previous research has suggested that improvement in prescription of risk appropriate VTE prophylaxis, reduces symptomatic VTE and preventable harm from VTE without increasing major bleeding [26].
The inconsistencies between studies in the association between VTE prophylaxis and mortality could be, in part, attributed to case mix variation, including comorbidities and admission diagnosis which affect the risk of mortality and the decision whether and the type of VTE prophylaxis prescribed [14, 17, 27]. First, the effectiveness of individual VTE prophylaxis in reducing VTE events is established, however, the balance of effectiveness and safety depends on the patient’s risk profiles [28]. Patients have different risk profiles, such as VTE risk factors, risk of bleeding, admission diagnosis, and some groups of patients may not benefit from VTE prophylaxis if their baseline risk of VTE is low or the associated risk of major bleeding is high [13, 29]. Second, differences in the association between omission of VTE prophylaxis and mortality between studies could be due to difference in prophylactic agent selection, dose, duration and timing of initiation of VTE prophylaxis [13, 14]. Third, omission of VTE prophylaxis could be due to other reasons, including patient preference, prescribing omission, medication errors or perceived unnecessary which could lead to a varying impact of omission of VTE on mortality [30]. For example, in cardiac arrest, intracerebral hemorrhage and stroke patients, there are no standardised ways to assess bleeding risk, which in turn plays a key role on determining whether pharmacological prophylaxis is given. Our analyses were adjusted for several risk factors that might influence use of VTE prophylaxis, including severity of illness, chronic health conditions, and admission diagnosis.
There is limited evidence regarding the mortality benefit of VTE prophylaxis in patients diagnosed with neurological conditions [17] and traumatic brain injury (TBI) [31], which could be among the reasons why omission of VTE prophylaxis was not associated with mortality in patients admitted due to subarachnoid haemorrhage or head trauma. A recent meta-analysis of patients undergoing neurosurgical interventions did not find evidence of the association between pharmacologic VTE prophylaxis and mortality [17]. Analysis of Victorian State Trauma Registry from July 2017 to June 2018, showed that in older patients with major trauma anticoagulant use was associated with higher odds of in-hospital mortality [32]. Exiting evidence suggest that patients diagnosed with intracerebral haemorrhage with indication for thromboprophylaxis benefit from pharmacological prophylaxis without significantly increasing bleeding complications [33, 34], whereas in initiation of mechanical prophylaxis is recommended in Subarachnoid haemorrhage patients [34]. The difference in VTE prophylaxis related mortality between intracerebral and subarachnoid haemorrhage patients could be because of variations in the location or cause of haemorrhage which influence disease management and outcomes. These could be among the reasons why the risk of mortality was not significantly higher in patients diagnosed with head injury or subarachnoid haemorrhage who missed out VTE prophylaxis. However, it is not clear from this study why there appear to be differences between the brain injury diagnoses groups.
Our findings have implications for improving VTE prevention and care, since they demonstrate the importance of individualising VTE prophylaxis decision making. Evidence-based guidelines acknowledge that VTE prophylaxis methods differ in their balance of benefits and harms depending on the patient’s risk profile and recommends balancing VTE risk and bleeding risk [6]. However, there are no tools for objective assessment of the benefit-harm balance of VTE prophylaxis, and VTE prophylaxis decisions are made based on clinician’s own judgment, often guided by anecdote or experience [27]. The lack of understanding how to individualize VTE prophylaxis decision making has been identified as a critical gap in VTE prevention practices [28].
Our study has some limitations. The variables which are potentially important for understanding VTE prophylaxis use, including VTE and bleeding risk assessment, reasons for not receiving VTE prophylaxis and type, dose and duration of VTE prophylaxis were not collected, therefore were not taken into account in the analyses. Contextual factors that influence VTE prophylaxis decision making such as patient preference, awareness of VTE prophylaxis, and local VTE prophylaxis guidelines were not collected. Furthermore, sometimes clinicians or data collectors may not differentiate between ‘contraindicated’ and ‘not indicated’, which is another potential limitation. Finally, data on treatments given in the ICU, and how many patients were already on anticoagulants when they come to ICU were not collected, therefore were not taken into account in the analyses.
Conclusions
In this multi-centre registry study including more than 1.4 million ICU admissions, omission of VTE prophylaxis within the first 24 h after ICU admission without obvious reasons or contraindications to VTE prophylaxis was independently associated with increased risk of in-hospital mortality. The risk of in-hospital mortality attributable to omission of VTE prophylaxis varied substantially by admission diagnosis. In stroke, cardiac arrest, intracerebral haemorrhage, thromboprophylaxis might be indicated but not in those with subarachnoid haemorrhage or head injury. The findings highlight the importance of individualised diagnosis-related thromboprophylaxis practices.
Data Availability
The datasets used in the current study are not publicly available, but are available from the corresponding author on reasonable request.
Abbreviations
- ANZICS:
-
Australian and New Zealand Intensive Care Society
- ANZROD:
-
Australian and New Zealand Risk of Death
- APACHE:
-
Acute Physiology and Chronic Health Evaluation
- APD:
-
Adult Patient Database
- CORE:
-
Centre for Outcome and Resource Evaluation
- ICU:
-
intensive care unit; VTE:Venous thromboembolism
- OR:
-
Odds Ratio
References
Nicholson M, Chan N, Bhagirath V, Ginsberg J. Prevention of venous thromboembolism in 2020 and Beyond. J Clin Med. 2020;9(8):2467. https://doi.org/10.3390/jcm9082467.
Lyman GH, Culakova E, Poniewierski MS, Kuderer NM. Morbidity, mortality and costs associated with venous thromboembolism in hospitalized patients with cancer. Thromb Res. 2018;164(Suppl 1):112–s8. https://doi.org/10.1016/j.thromres.2018.01.028.
Heit JA. Epidemiology of venous thromboembolism. Nat Rev Cardiol. 2015;12(8):464–74. https://doi.org/10.1038/nrcardio.2015.83.
Søgaard KK, Schmidt M, Pedersen L, Horváth–Puhó E, Sørensen HT. 30-Year mortality after venous thromboembolism. Circulation. 2014;130(10):829–36. https://doi.org/10.1161/CIRCULATIONAHA.114.009107.
Henke PK, Kahn SR, Pannucci CJ, et al. Call to action to prevent venous thromboembolism in hospitalized patients: a Policy Statement from the American Heart Association. Circulation. 2020;141(24):e914–e31. https://doi.org/10.1161/cir.0000000000000769.
Tran HA, Gibbs H, Merriman E, et al. New guidelines from the thrombosis and Haemostasis Society of Australia and New Zealand for the diagnosis and management of venous thromboembolism. Med J Aust. 2019;210(5):227–35. https://doi.org/10.5694/mja2.50004.
Minet C, Potton L, Bonadona A, et al. Venous thromboembolism in the ICU: main characteristics, diagnosis and thromboprophylaxis. Crit Care. 2015;19(1):287. https://doi.org/10.1186/s13054-015-1003-9.
Fernando SM, Tran A, Cheng W et al. VTE Prophylaxis in Critically Ill Adults: A Systematic Review and Network Meta-analysis. Chest. doi:https://doi.org/10.1016/j.chest.2021.08.050.
Kahn SR, Lim W, Dunn AS, et al. Prevention of VTE in nonsurgical patients: antithrombotic therapy and Prevention of thrombosis, 9th ed: american college of chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141(2 Suppl):e195S–e226S. https://doi.org/10.1378/chest.11-2296.
Cohen AT, Tapson VF, Bergmann J-F, et al. Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross-sectional study. The Lancet. 2008;371(9610):387–94. https://doi.org/10.1016/S0140-6736(08)60202-0.
Tracy LM, Cameron PA, Singer Y, et al. Venous thromboembolism prophylaxis practice and its association with outcomes in Australia and New Zealand burns patients. Burns Trauma. 2021;9:tkaa044. https://doi.org/10.1093/burnst/tkaa044.
Assareh H, Chen J, Ou L, Hillman K, Flabouris A. Incidences and variations of hospital acquired venous thromboembolism in australian hospitals: a population-based study. BMC Health Serv Res. 2016;16(1):511. https://doi.org/10.1186/s12913-016-1766-y.
Skeik N, Westergard E. Recommendations for VTE Prophylaxis in medically ill patients. Ann Vasc Dis. 2020;13(1):38–44. https://doi.org/10.3400/avd.ra.19-00115.
Hecht JP, Han EJ, Cain-Nielsen AH, Scott JW, Hemmila MR, Wahl WL. Association of timing of initiation of pharmacologic venous thromboembolism prophylaxis with outcomes in trauma patients. J Trauma Acute Care Surg. 2021;90(1):54–63. https://doi.org/10.1097/ta.0000000000002912.
Lamb T, Lenet T, Zahrai A, et al. Timing of pharmacologic venous thromboembolism prophylaxis initiation for trauma patients with nonoperatively managed blunt abdominal solid organ injury: a systematic review and meta-analysis. World J Emerg Surg. 2022;17(1):19. https://doi.org/10.1186/s13017-022-00423-1.
Ho KM, Chavan S, Pilcher D. Omission of early thromboprophylaxis and mortality in critically ill patients: a multicenter registry study. Chest. 2011;140(6):1436–46. https://doi.org/10.1378/chest.11-1444.
Yepes-Nuñez JJ, Rajasekhar A, Rahman M, et al. Pharmacologic thromboprophylaxis in adult patients undergoing neurosurgical interventions for preventing venous thromboembolism. Blood Adv. 2020;4(12):2798–809. https://doi.org/10.1182/bloodadvances.2020002195.
Lu VM, Alvi MA, Rovin RA, Kasper EM. Clinical outcomes following early versus late pharmacologic thromboprophylaxis in patients with traumatic intracranial hemorrhage: a systematic review and meta-analysis. Neurosurg Rev. 2020;43(3):861–72. https://doi.org/10.1007/s10143-018-1045-y.
Stow PJ, Hart GK, Higlett T, et al. Development and implementation of a high-quality clinical database: the australian and New Zealand Intensive Care Society Adult Patient Database. J Crit Care. 2006;21(2):133–41. https://doi.org/10.1016/j.jcrc.2005.11.010.
Sahle BW, Pilcher D, Peter K, McFadyen JD, Bucknall T. Trends and risk factors for omission of early thromboprophylaxis in australian and New Zealand ICUs between 2009 and 2020. Intensive Care Med. 2022;48(5):590–8. https://doi.org/10.1007/s00134-022-06672-7.
Paul E, Bailey M, Kasza J, Pilcher D. The ANZROD model: better benchmarking of ICU outcomes and detection of outliers. Crit Care Resusc. 2016;18(1):25–36.
Paul E, Bailey M, Pilcher D. Risk prediction of hospital mortality for adult patients admitted to australian and New Zealand intensive care units: development and validation of the australian and New Zealand risk of death model. J Crit Care. 2013;28(6):935–41. https://doi.org/10.1016/j.jcrc.2013.07.058.
Flevas DA, Megaloikonomos PD, Dimopoulos L, Mitsiokapa E, Koulouvaris P, Mavrogenis AF. Thromboembolism prophylaxis in orthopaedics: an update. EFORT Open Rev. 2018;3(4):136–48. https://doi.org/10.1302/2058-5241.3.170018.
Streiff MB, Lau BD, Hobson DB, et al. The Johns Hopkins venous thromboembolism collaborative: multidisciplinary team approach to achieve perfect prophylaxis. J Hosp Med. 2016;11(S2):8–S14. https://doi.org/10.1002/jhm.2657.
Lauzier F, Muscedere J, Deland É, et al. Thromboprophylaxis patterns and determinants in critically ill patients: a multicenter audit. Crit Care. 2014;18(2):R82. https://doi.org/10.1186/cc13844.
Zeidan AM, Streiff MB, Lau BD, et al. Impact of a venous thromboembolism prophylaxis “smart order set”: improved compliance, fewer events. Am J Hematol. 2013;88(7):545–9. https://doi.org/10.1002/ajh.23450.
Angchaisuksiri P, Goto S, Farjat AE, et al. Venous thromboembolism in Asia and worldwide: emerging insights from GARFIELD-VTE. Thromb Res. 2021;201:63–72. https://doi.org/10.1016/j.thromres.2021.02.024.
Australian Commission on Safety and Quality in Health Care. Venous Thromboembolism Prevention Clinical Care Standard. Sydney: ACSQHC. ; 2020. Available: https://www.safetyandquality.gov.au/sites/default/files/2020-01/venous_thromboembolism_prevention_clinical_care_standard_-_jan_2020_2.pdf. Accessed 27 August 2020.
Lyman GH, Carrier M, Ay C, et al. American Society of Hematology 2021 guidelines for management of venous thromboembolism: prevention and treatment in patients with cancer. Blood Adv. 2021;5(4):927–74. https://doi.org/10.1182/bloodadvances.2020003442.
Lauzier F, Muscedere J, Deland E, et al. Thromboprophylaxis patterns and determinants in critically ill patients: a multicenter audit. Crit Care. 2014;18(2):R82. https://doi.org/10.1186/cc13844.
Hecht JP, LaDuke ZJ, Cain-Nielsen AH, Hemmila MR, Wahl WL. Effect of Preinjury oral anticoagulants on outcomes following traumatic Brain Injury from Falls in older adults. Pharmacotherapy. 2020;40(7):604–13. https://doi.org/10.1002/phar.2435.
Sato N, Cameron P, Mclellan S, Beck B, Gabbe B. Association between anticoagulants and mortality and functional outcomes in older patients with major trauma. Emerg Med J. 2021;emermed–2019. https://doi.org/10.1136/emermed-2019-209368.
Kuramatsu JB, Huttner HB. Management of oral anticoagulation after intracerebral hemorrhage. Int J Stroke. 2019;14(3):238–46. https://doi.org/10.1177/1747493019828555.
Nyquist P, Jichici D, Bautista C et al. Prophylaxis of Venous Thrombosis in Neurocritical Care Patients: An Executive Summary of Evidence-Based Guidelines: A Statement for Healthcare Professionals From the Neurocritical Care Society and Society of Critical Care Medicine. Crit Care Med. 2017;45(3).
Acknowledgements
The authors and the ANZICS CORE management committee would like to thank clinicians, data collectors and researchers at the contributing sites (Supplementary Table 1).
Funding
The authors declare that no funding was received for the present study. Berhe W. Sahle is supported by an Alfred Deakin Postdoctoral Research Fellowship. James D. McFadyen is supported by an NHMRC Early Career Fellowship.
Author information
Authors and Affiliations
Contributions
BWS: conceived the study, analysed data, wrote the initial drafts of the manuscript, created tables and figures, and finalized the manuscript. DP and EL: contributed to the concept and design, statistical analysis and interpretation of data. All authors contributed to the interpretation of results, review and editing of the manuscript. All authors critically reviewed the manuscript and approved the final version before submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Alfred Health Human Research Ethics Committee (Project No: 276/21). ANZICS Centre for Outcome and Resource Evaluation Management Committee granted access to the ANZICS-APD in accordance with standing protocols. All methods were carried out in accordance with the relevant guidelines and regulations of the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
All authors declare no financial or non-financial competing interests with regards to the submitted work.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sahle, B.W., Pilcher, D., Peter, K. et al. Mortality data from omission of early thromboprophylaxis in critically ill patients highlights the importance of an individualised diagnosis-related approach. Thrombosis J 21, 59 (2023). https://doi.org/10.1186/s12959-023-00499-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12959-023-00499-y