Abstract
Background
Laennec’s capsule has been found for about 200 years. However, laparoscopic anatomical right and left hemihepatectomy (LARH and LALH) using Laennec’s approach are rarely reported.
Methods
We retrospectively analyzed the technical details and the surgical outcomes of 15 patients who underwent LAH via Laennec’s approach between May 2017 and July 2020. The operation time, intraoperative blood loss, postoperative complications, and hospital stay were recorded and analyzed.
Results
Four of 15 patients were diagnosed with hepatic hemangioma, 2 had hepatolithiasis, and 9 patients had primary liver cancer. During the surgery, Laennec’s approach was used for LAH without conversion to open surgery. Four patients were treated with LARH, and 11 patients were cured with LALH. The mean age of the patients was 62.1 ± 6.5 years, and four were male. The mean operative time, blood loss, and length of the postoperative hospital stay were 193 ± 49 min, 247 ± 120 mL, and 8.7 ± 2.0 days, respectively. There was no incidence of postoperative bile leakage and bleeding. No mortality occurred. We also demonstrated that Laennec’s capsule does exist around the peripheral hepatic veins with histological confirmation.
Conclusions
Laennec’s approach is safe and feasible for LAH. Precise isolation of Laennec’s approach based on Laennec’s capsule helps to standardize the surgical techniques for laparoscopic anatomical hepatectomy.
Similar content being viewed by others
Introduction
Laparoscopic liver surgery, a widely accepted standard surgical practice for the management of liver neoplasm, has evolved over the past two decades, and the procedure has expanded from initial local hepatectomy to anatomical hepatectomy. Laparoscopic hepatic resection has attained an equivalent status of safety and efficacy as conventional open surgeries, but the expansion of the procedure depends on the experienced surgical team in hepatobiliary surgery, laparoscopic skills, and specialized centers with advanced laparoscopic surgery. Nevertheless, laparoscopic anatomical hemihepatectomies (LAH) are very challenging and technically demanding procedures. Notably, for deep-seated or invisible lesions, the development of LAH is greatly limited because of their deep anatomical position, surgical complication during exposure of the resection plane, and complexity in identifying the boundary of hemihepatectomy, and difficult hemorrhage control [1, 2]. In LAH, identification and anatomical separation of the Glissonean pedicle (GP) at the hepatic hilum and exposure of the landmark hepatic vein represents the critical steps in deciding the transection plane. However, there is a lack of consensus on the standardized approach to LAH [3].
Laennec’s capsule, the liver’s intrinsic membrane, represents an essential structure for the comprehensive understanding of the surgical anatomy of the liver and standardization of the surgical approach to LAH [4, 5]. Some studies have suggested that there is a gap between the extrahepatic GP and Laennec’s capsule that could be used as an anatomical gap to isolate GP and hepatic vein [6,7,8]. However, LAH based on Laennec’s capsule is rarely reported. Here we described the relevant application of Laennec’s approach for LAH based on Laennec’s capsule and highlighted the surgical anatomical description of the liver and related clinical experience. After that, we retrospectively analyzed the technical details and the surgical outcomes of our standardized approach performed on 15 patients who underwent LAH in our hospital between May 2017 and July 2020. We also investigated the safety and efficacy of this approach to expand our understanding of the membranous anatomy of the liver.
Materials and methods
General information
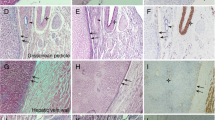
This study comprised 15 patients with benign or malignant neoplasms or hepatolithiasis who underwent LAH between May 2017 and July 2020. Of the 15 patients, 4 patients were diagnosed with hepatic hemangioma, 2 patients had hepatolithiasis, and 9 patients had primary liver cancer. The mean patient age was 62.1 ± 6.5 years, and four were male. The preoperative liver function of patients was Child-Pugh class A, and the indocyanine green retention rate at 15 min (ICG R15) was less than 10%. There was no apparent surgical contraindication before the surgery. None of the lesions affected the anatomy of the first or the second porta hepatis. Laennec’s approach for LAH was performed during the hemihepatectomy by isolating the GP and hepatic vein. The liver tissue specimens adjacent to the GP, hepatic veins, and inferior vena cava (IVC) were collected for hematoxylin and eosin (H&E) and Mallory’s phosphotungstic acid hematoxylin-eosin staining. The study protocol was approved by the Research Ethics Committee of the First Affiliated Hospital of Kangda College of Nan**g Medical University (Approval number: KY20170513001). This study was performed in accordance with the Declaration of Helsinki, and written informed consent was obtained from each patient before surgery.
Surgical methods
All procedures were performed under general anesthesia. Patients were placed in the supine position for resection. The 5-port technique was performed. The pneumoperitoneum pressure was maintained at 14 mmHg. The central venous pressure was maintained between 0 and 3 cm H2O during surgery in all cases. The hepatoduodenal ligament was encircled with extraperitoneal blocking tape through Winslow’s foramen by the Pringle maneuver. For right hemihepatectomy, the following procedures were performed: (1) Laennec’s approach for dissection of GP: the hepatic hilar plate was lowered after cholecystectomy. The peritoneum between segment 4 and the surface of GP was incised through Laennec’s capsule. After sufficient dissection, the right GP was ligated using a Goldfinger dissector for traction and transected with a laparoscopic vascular stapler (if the right GP was difficult to dissect, the liver parenchyma dissecting-first method through the hepatic Cantlie line was applied to reveal the root of the right GP [5, 10, 12]. However, we confirmed through H&E and Mallory staining that Laennec’s capsule also covers the branches of the peripheral hepatic vein of the segments II–VIII, and there is a gap between Laennec’s capsule and the veins. In precision liver excision, dissecting Laennec’s capsule gap along the liver venous trunk and its branches can effectively achieve segmental anatomic liver excision.
This study highlights that Laennec’s approach provides a new perspective for laparoscopic anatomical hepatectomy. It is beneficial to the procedure and standardization of laparoscopic anatomical hepatectomy. Laennec’s capsule can be used as an anatomical marker for anatomical hepatectomy, expecting to promote liver surgeons’ understanding of liver membrane anatomy and the development of LAH.
Conclusions
Laennec’s approach is safe and feasible for LAH. Precise isolation of Laennec’s approach based on Laennec’s capsule helps to standardize the surgical techniques for laparoscopic anatomical hepatectomy.
Availability of data and materials
Please contact the corresponding author with request for data.
Abbreviations
- LARH:
-
Laparoscopic anatomical right hemihepatectomy
- LALH:
-
Laparoscopic anatomical left hemihepatectomy
- LAH:
-
Laparoscopic anatomical hemihepatectomy
- GP:
-
Glissonean pedicle
- IVC:
-
Inferior vena cava
- ICGR15:
-
Indocyanine green retention rate at 15 min
References
Kim JH, Choi JW. Intrahepatic Glissonian approach to the ventral aspect of the Arantius ligament in laparoscopic left hemihepatectomy. World J Surg. 2019;43:1303–7.
Kim JH, Kim H. Laparoscopic right hemihepatectomy using the Glissonean approach: detachment of the hilar plate (with video). Ann Surg Oncol. 2021;28:459–64.
Wakabayashi G, Cherqui D, Geller DA, Buell JF, Kaneko H, Han HS, et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg. 2015;261:619–29.
Hayashi S, Murakami G, Ohtsuka A, Itoh M, Nakano T, Fukuzawa Y. Connective tissue configuration in the human liver hilar region with special reference to the liver capsule and vascular sheath. J Hepatobiliary Pancreat Surg. 2008;15:640–7.
Sugioka A, Kato Y, Tanahashi Y. Systematic extrahepatic Glissonean pedicle isolation for anatomical liver resection based on Laennec’s capsule: proposal of a novel comprehensive surgical anatomy of the liver. J Hepatobiliary Pancreat Sci. 2017;24:17–23.
Kiguchi G, Sugioka A, Kato Y, Uyama I. Laparoscopic S7 Segmentectomy using the inter-Laennec approach for hepatocellular carcinoma near the right hepatic vein. Surg Oncol. 2019;31:132–4.
Monden K, Sadamori H, Hioki M, Sugioka A. Laparoscopic anatomic segmentectomy 8 using the outer-Laennec approach. Surg Oncol. 2020;35:299–300.
Hu Y, Shi J, Wang S, Zhang W, Sun X, Sun B, et al. Laennec’s approach for laparoscopic anatomic hepatectomy based on Laennec’s capsule. BMC Gastroenterol. 2019;19:194.
**ao L, Wang Z, Zhou L. “Liver parenchyma dissecting-first” method facilitates the Glissonean pedicle approach in anatomical laparoscopic hepatolobectomy. Ann Transl Med. 2020;8:940.
Shirata C, Hasegawa K, Halkic N, Kokudo N. Laennec’s capsule does not exist around the peripheral hepatic veins. J Hepatobiliary Pancreat Sci. 2019;26:E13.
Sugioka A. Re: Laennec’s capsule does not exist around the peripheral hepatic veins. J Hepatobiliary Pancreat Sci. 2019;26:E14.
Shirata C, Kokudo T, Gillet M, Uldry E, Demartines N, Kokudo N, et al. Reappraisal of Laennec’s capsule. Surg Oncol. 2020;33:222–3.
Ferrero A, Lo TR, Giovanardi F, Langella S, Forchino F, Russolillo N. Laparoscopic right posterior anatomic liver resections with Glissonean pedicle-first and venous craniocaudal approach. Surg Endosc. 2021;35:449–55.
Lee JH, Han DH, Jang DS, Choi GH, Choi JS. Robotic extrahepatic Glissonean pedicle approach for anatomic liver resection in the right liver: techniques and perioperative outcomes. Surg Endosc. 2016;30:3882–8.
Yamamoto M, Ariizumi SI. Glissonean pedicle approach in liver surgery. Ann Gastroenterol Surg. 2018;2:124–8.
Acknowledgements
Not applicable.
Funding
This research was supported by the National Natural Science Foundation of China (81900772), the Foundation of Health and Family planning Commission of Lianyungang (201802 and 201906), and the Startup Fund for Doctoral Research (BS202003).
Author information
Authors and Affiliations
Contributions
WH and XS conceived the new approach used in this study. WH and GZ performed the histological examination of the liver. WH, XS, and KL performed the surgery. WH, CZ, MC, and ML wrote the manuscript. KL and ZW performed data analysis and revised the manuscript. The authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Research Ethics Committee of the First Affiliated Hospital of Kangda College of Nan**g Medical University (Approval number: KY20170513001). This study was performed in accordance with the Declaration of Helsinki, and written informed consent was obtained from each patient before surgery.
Consent for publication
Written informed consent for publication was obtained from all patients enrolled in the study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hu, W., Zhang, G., Chen, M. et al. Laennec’s approach for laparoscopic anatomical hemihepatectomy. World J Surg Onc 19, 295 (2021). https://doi.org/10.1186/s12957-021-02404-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-021-02404-1