Bloom DE, Cadarette D. Infectious disease threats in the twenty-first century: strengthening the global response. Front Immunol. 2019;10:549.
Article
PubMed
PubMed Central
Google Scholar
Toner E, Adlja A, Gronvall GK, Cicero A, Inglesby TV. Antimicrobial resistance is a global health emergency. Health Secur. 2015;13:153–5.
Article
PubMed
PubMed Central
Google Scholar
Afonso AC, Oliveira D, Saavedra MJ, Borges A, Simões M. Biofilms in diabetic foot ulcers: impact, risk factors and control strategies. Int J Mol Sci. 2021;22:8278.
Article
CAS
PubMed
PubMed Central
Google Scholar
Kohanski MA, Dwyer DJ, Collins JJ. How antibiotics kill bacteria: from targets to networks. Nat Rev Microbiol. 2010;8:423–35.
Article
CAS
PubMed
PubMed Central
Google Scholar
Fischbach MA, Walsh CT. Antibiotics for emerging pathogens. Science. 2009;325:1089–93.
Article
CAS
PubMed
PubMed Central
Google Scholar
Tyers M, Wright GD. Drug combinations: a strategy to extend the life of antibiotics in the 21st century. Nat Rev Microbiol. 2019;17:141–55.
Article
CAS
PubMed
Google Scholar
Crofts TS, Gasparrini AJ, Dantas G. Next-generation approaches to understand and combat the antibiotic resistome. Nat Rev Microbiol. 2017;15:422–34.
Article
CAS
PubMed
PubMed Central
Google Scholar
de Kraker MEA, Stewardson AJ, Harbarth S. Will 10 million people die a year due to antimicrobial resistance by 2050? PLoS Med. 2016;13:e1002184.
Article
PubMed
PubMed Central
Google Scholar
Blair JMA, Webber MA, Baylay AJ, Ogbolu DO, Piddock LJV. Molecular mechanisms of antibiotic resistance. Nat Rev Microbiol. 2015;13:42–51.
Article
CAS
PubMed
Google Scholar
Anand A, Unnikrishnan B, Wei SC, Chou CP, Zhang LZ, Huang CC. Graphene oxide and carbon dots as broad-spectrum antimicrobial agents-a minireview. Nanoscale Horiz. 2019;4:117–37.
Article
CAS
PubMed
Google Scholar
Gupta A, Mumtaz S, Li C-H, Hussain I, Rotello VM. Combatting antibiotic-resistant bacteria using nanomaterials. Chem Soc Rev. 2019;48:415–27.
Article
PubMed
PubMed Central
Google Scholar
Wang L, Hu C, Shao L. The antimicrobial activity of nanoparticles: present situation and prospects for the future. Int J Nanomed. 2017;12:1227.
Article
CAS
Google Scholar
Zheng K, **e J. Cluster materials as traceable antibacterial agents. Acc Mater Res. 2021;2:1104–16.
Article
CAS
Google Scholar
Nain A, Tseng YT, Wei SC, Periasamy AP, Huang CC, Tseng FG, et al. Cap** 1,3-propanedithiol to boost the antibacterial activity of protein-templated copper nanoclusters. Nanoscale. 2020;389: 121821.
CAS
Google Scholar
Vincent M, Duval RE, Hartemann P, Engels-Deutsch M. Contact killing and antimicrobial properties of copper. J Appl Microbiol. 2018;124:1032–46.
Article
CAS
PubMed
Google Scholar
Wang Y, Yang Y, Shi Y, Song H, Yu C. Antibiotic-free antibacterial strategies enabled by nanomaterials: progress and perspectives. Adv Mater. 2020;32:1904106.
Article
CAS
Google Scholar
Shaikh S, Nazam N, Rizvi SMD, Ahmad K, Baig MH, Lee EJ, et al. Mechanistic insights into the antimicrobial actions of metallic nanoparticles and their implications for multidrug resistance. Int J Mol Sci. 2019;20:2468.
Article
PubMed Central
CAS
Google Scholar
Bondarenko O, Juganson K. Toxicity of Ag, CuO and ZnO nanoparticles to selected environmentally relevant test organisms and mammalian cells in vitro: a critical review. Arch Toxicol. 2013;87:1181–200.
Article
CAS
PubMed
PubMed Central
Google Scholar
Le Ouay B, Stellacci F. Antibacterial activity of silver nanoparticles: a surface science insight. Nano Today. 2015;10:339–54.
Article
CAS
Google Scholar
Dwivedi N, Dhand C, Kumar P, Srivastava AK. Emergent 2D materials for combating infectious diseases: the potential of MXenes and MXene–graphene composites to fight against pandemics. Mater Adv. 2021;2:2892–905.
Article
CAS
Google Scholar
Sun W, Wu F. Two-dimensional materials for antimicrobial applications: graphene materials and beyond. Chem Asian J. 2018;13:3378–410.
Article
CAS
PubMed
Google Scholar
Begum S, Pramanik A, Davis D, Patibandla S, Gates K, Gao Y, et al. 2D and heterostructure nanomaterial based strategies for combating drug-resistant bacteria. ACS Omega. 2020;5:3116–30.
Article
CAS
PubMed
PubMed Central
Google Scholar
Nanobiotechnol J, Zhao B, Wang H, Dong W, Cheng S, Li H, et al. A multifunctional platform with single-NIR-laser-triggered photothermal and NO release for synergistic therapy against multidrug-resistant Gram-negative bacteria and their biofilms. J Nanobiotechnol. 2020;18:1–25.
CAS
Google Scholar
Ding H, Han D, Han Y, Liang Y, Liu X, Li Z. Visible light responsive CuS/protonated g-C3N4 heterostructure for rapid sterilization. J Hazard Mater. 2020;393: 122423.
Article
CAS
PubMed
Google Scholar
Naguib M, Barsoum MW, Gogotsi Y. Ten years of progress in the synthesis and development of MXenes. Adv Mater. 2021;33:2103393.
Article
CAS
Google Scholar
Meng W, Liu X, Song H, **e Y, Shi X, Dargusch M, et al. Advances and challenges in 2D MXenes: from structures to energy storage and conversions. Nano Today. 2021;40: 101273.
Article
CAS
Google Scholar
Wei Y, Zhang P, Soomro RA, Zhu Q, Xu B. Advances in the synthesis of 2D Mxenes. Adv Mater. 2021;33:2103148.
Article
CAS
Google Scholar
Lin H, Chen Y, Shi J. Insights into 2D MXenes for versatile biomedical applications: current advances and challenges ahead. Adv Sci. 2018;5:1800518.
Article
CAS
Google Scholar
Huang K, Li Z, Lin J, Han G, Huang P. Two-dimensional transition metal carbides and nitrides (MXenes) for biomedical applications. Chem Soc Rev. 2018;47:5109–24.
Article
CAS
PubMed
Google Scholar
Rasool K, Mahmoud KA, Johnson DJ, Helal M, Berdiyorov GR, Gogotsi Y. Efficient antibacterial membrane based on two-dimensional Ti3C2Tx (MXene) nanosheets. Sci Rep. 2017;7:1–11.
Article
CAS
Google Scholar
Arabi Shamsabadi A, Sharifian GhM, Anasori B, Soroush M. Antimicrobial mode-of-action of colloidal Ti3C2Tx MXene nanosheets. ACS Sustain Chem Eng. 2018;6:16586–96.
Article
CAS
Google Scholar
Li J, Li Z, Liu X, Li C, Zheng Y, Yeung KWK, et al. Interfacial engineering of Bi2S3/Ti3C2Tx MXene based on work function for rapid photo-excited bacteria-killing. Nat Commun. 2021;12:1–10.
CAS
Google Scholar
Zheng K, Li S, **g L, Chen P, **e J. Synergistic antimicrobial titanium carbide (MXene) conjugated with gold nanoclusters. Adv Healthc Mater. 2020;9:2001007.
Article
CAS
Google Scholar
Wu C-W, Unnikrishnan B, Chen I-WP, Harroun SG, Chang H-T, Huang C-C. Excellent oxidation resistive MXene aqueous ink for micro-supercapacitor application. Energy Storage Mater. 2020;25:563–71.
Article
Google Scholar
Hou T, Wang B, Ma M, Feng A, Huang Z, Zhang Y, et al. Preparation of two-dimensional titanium carbide (Ti3C2Tx) and NiCo2O4 composites to achieve excellent microwave absorption properties. Compos Part B Eng. 2020;180: 107577.
Article
CAS
Google Scholar
Wu X, Wang Z, Yu M, ** hierarchical nanohybrids with efficient lithium storage and hydrogen evolution capability. Adv Mater. 2017;29:1607017.
Article
CAS
Google Scholar
Zhang M, Chen X, Sui J, Abraha BS, Li Y, Peng W, et al. Improving the performance of a titanium carbide MXene in supercapacitors by partial oxidation treatment. Inorg Chem Front. 2020;7:1205–11.
Article
CAS
Google Scholar
Wang Z, Xu Z, Huang H, Chu X, **e Y, **ong D, et al. Unraveling and regulating self-discharge behavior of Ti3C2Tx MXene-based supercapacitors. ACS Nano. 2020;14:4916–24.
Article
CAS
PubMed
Google Scholar
She H, Zhou H, Li L, Zhao Z, Jiang M, Huang J, et al. Construction of a two-dimensional composite derived from TiO2 and SnS2 for enhanced photocatalytic reduction of CO2 into CH4. ACS Sustain Chem Eng. 2018;7:650–9.
Article
CAS
Google Scholar
Zhang CJ, Pinilla S, McEvoy N, Cullen CP, Anasori B, Long E, et al. Oxidation stability of colloidal two-dimensional titanium carbides (MXenes). Chem Mater. 2017;29:4848–56.
Article
CAS
Google Scholar
Guo Z, Gao L, Xu Z, Teo S, Zhang C, Kamata Y, et al. High electrical conductivity 2D MXene serves as additive of perovskite for efficient solar cells. Small. 2018;14:1802738.
Article
CAS
Google Scholar
Xu H, Ren A, Wu J, Wang Z. Recent advances in 2D MXenes for photodetection. Adv Funct Mater. 2020;30:2000907.
Article
CAS
Google Scholar
Chen G, Wang H, Wei X, Wu Y, Gu W, Hu L, et al. Efficient Z-Scheme heterostructure based on TiO2/Ti3C2Tx/Cu2O to boost photoelectrochemical response for ultrasensitive biosensing. Sensors Actuators B Chem. 2020;312: 127951.
Article
CAS
Google Scholar
Cai T, Wang L, Liu Y, Zhang S, Dong W, Chen H, et al. Ag3PO4/Ti3C2 MXene interface materials as a Schottky catalyst with enhanced photocatalytic activities and anti-photocorrosion performance. Appl Catal B Environ. 2018;239:545–54.
Article
CAS
Google Scholar
Nain A, Tseng YT, Gupta A, Lin YF, Sangili A, Huang YF, et al. Anti-microbial/oxidative/inflammatory nanogels accelerate chronic wound healing. Smart Mater Med. 2022. https://doi.org/10.1016/j.smaim.2021.12.006.
Article
Google Scholar
Mishin V, Gray JP, Heck DE, Laskin DL, Laskin JD. Application of the Amplex red/horseradish peroxidase assay to measure hydrogen peroxide generation by recombinant microsomal enzymes. Free Radic Biol Med. 2010;48:1485–91.
Article
CAS
PubMed
PubMed Central
Google Scholar
Zhang S, Cao C, Lv X, Dai H, Zhong Z, Liang C, et al. A H2O2 self-sufficient nanoplatform with domino effects for thermal-responsive enhanced chemodynamic therapy. Chem Sci. 2020;11:1926–34.
Article
CAS
PubMed
PubMed Central
Google Scholar
Dvoranová D, Barbieriková Z, Brezová V. Radical intermediates in photoinduced reactions on TiO2 (an EPR spin trap** study). Molecules. 2014;19:17279–304.
Article
PubMed
PubMed Central
CAS
Google Scholar
Deng L, Sheng D, Liu M, Yang L, Ran H, Li P, et al. A near-infrared laser and H2O2 activated bio-nanoreactor for enhanced photodynamic therapy of hypoxic tumors. Biomater Sci. 2020;8:858–70.
Article
CAS
PubMed
Google Scholar
Wang H, Cheng H, Wang F, Wei D, Wang X. An improved 3-(4, 5-dimethylthiazol-2-yl)-2, 5-diphenyl tetrazolium bromide (MTT) reduction assay for evaluating the viability of Escherichia coli cells. J Microbiol Methods. 2010;82:330–3.
Article
CAS
PubMed
Google Scholar
Zhao Y, Zhang S, Shi R, Waterhouse GIN, Tang J, Zhang T. Two-dimensional photocatalyst design: a critical review of recent experimental and computational advances. Mater Today. 2020;34:78–91.
Article
CAS
Google Scholar
Zhang Y, **a W, Wu Y, Zhang P. Prediction of MXene based 2D tunable band gap semiconductors: GW quasiparticle calculations. Nanoscale. 2019;11:3993–4000.
Article
CAS
PubMed
Google Scholar
Akhtar N, Rani M, Mahmood A, Saba H, Khan S, Murtaza G, et al. Synthesis and characterization of MXene/BiCr2O4 nanocomposite with excellent electrochemical properties. J Mater Res Technol. 2021;15:2007–15.
Article
CAS
Google Scholar
Liu T, **ao B, **ang F, Tan J, Chen Z, Zhang X, et al. Ultrasmall copper-based nanoparticles for reactive oxygen species scavenging and alleviation of inflammation related diseases. Nat Commun. 2020;11:1–16.
CAS
Google Scholar
Wang W, Feng H, Liu J, Zhang M, Liu S, Feng C, et al. A photo catalyst of cuprous oxide anchored MXene nanosheet for dramatic enhancement of synergistic antibacterial ability. Chem Eng J. 2020;386: 124116.
Article
CAS
Google Scholar
Xu D, Li Z, Li L, Wang J. Insights into the photothermal conversion of 2D MXene nanomaterials: synthesis, mechanism, and applications. Adv Funct Mater. 2020;30:2000712.
Article
CAS
Google Scholar
Hu W, Miao X, Tao H, Baev A, Ren C, Fan Q, et al. Manipulating nonradiative decay channel by intermolecular charge transfer for exceptionally improved photothermal conversion. ACS Nano. 2019;13:12006–14.
Article
CAS
PubMed
Google Scholar
Han X, Huang J, Lin H, Wang Z, Li P, Chen Y. 2D ultrathin MXene-based drug-delivery nanoplatform for synergistic photothermal ablation and chemotherapy of cancer. Adv Healthc Mater. 2018. https://doi.org/10.1002/adhm.201701394.
Article
PubMed
PubMed Central
Google Scholar
Li R, Zhang L, Shi L, Wang P. MXene Ti3C2: an effective 2D light-to-heat conversion material. ACS Nano. 2017;11:3752–9.
Article
CAS
PubMed
Google Scholar
Boerigter C, Campana R, Morabito M, Linic S. Evidence and implications of direct charge excitation as the dominant mechanism in plasmon-mediated photocatalysis. Nat Commun. 2016;7:1–9.
Article
CAS
Google Scholar
Shi Y, Cui D, Zhang Z. Quantitative study of the nonlinearly enhanced photoacoustic/ photothermal effect by strong LSPR-coupled nanoassemblies. Nanomaterials. 2020;10:1942.
Article
CAS
PubMed Central
Google Scholar
Liu Y, Tian Y, Han Q, Yin J, Zhang J, Yu Y, et al. Synergism of 2D/1D MXene/cobalt nanowire heterojunctions for boosted photo-activated antibacterial application. Chem Eng J. 2021;410: 128209.
Article
CAS
Google Scholar
Wang D, Fang Y, Yu W, Wang L, **e H, Yue Y. Significant solar energy absorption of MXene Ti3C2Tx nanofluids via localized surface plasmon resonance. Sol Energy Mater Sol Cells. 2021;220: 110850.
Article
CAS
Google Scholar
Wiegand I, Hilpert K, Hancock REW. Agar and broth dilution methods to determine the minimal inhibitory concentration (MIC) of antimicrobial substances. Nat Protoc. 2008;3:163–75.
Article
CAS
PubMed
Google Scholar
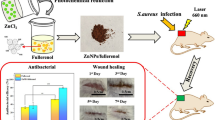
Nain A, Wei SC, Lin YF, Tseng YT, Mandal RP, Huang YF, et al. Copper sulfide nanoassemblies for catalytic and photoresponsive eradication of bacteria from infected wounds. ACS Appl Mater Interfaces. 2021;13:7865–78.
Article
CAS
PubMed
Google Scholar
Hudson MA, Siegele DA, Lockless SW. Use of a fluorescence-based assay to measure Escherichia coli membrane potential changes in high throughput. Antimicrob Agents Chemother. 2020;64:e00910-e920.
Article
CAS
PubMed
PubMed Central
Google Scholar
Parastan R, Kargar M, Solhjoo K, Kafilzadeh F. Staphylococcus aureus biofilms: structures, antibiotic resistance, inhibition, and vaccines. Gene Reports. 2020;20: 100739.
Article
Google Scholar
Ishida Y, Kuninaka Y, Nosaka M, Furuta M, Kimura A, Taruya A, et al. CCL2-mediated reversal of impaired skin wound healing in diabetic mice by normalization of neovascularization and collagen accumulation. J Invest Dermatol. 2019;139:2517–27.
Article
CAS
PubMed
Google Scholar
Banerjee K, Madhyastha R, Nakajima Y, Maruyama M, Madhyastha H. Nanoceutical adjuvants as wound healing material: precepts and prospects. Int J Mol Sci. 2021;22:4748.
Article
CAS
PubMed
PubMed Central
Google Scholar
Landén NX, Li D, Ståhle M. Transition from inflammation to proliferation: a critical step during wound healing. Cell Mol Life Sci. 2016;73:3861–85.
Article
PubMed
PubMed Central
CAS
Google Scholar
Nain A, Huang HH, Chevrier DM, Tseng YT, Sangili A, Lin YF, et al. Catalytic and photoresponsive bismuth-doped copper sulfide nanocomposites with multiple heterojunctions and surface vacancies for the treatment of multidrug-resistant clinical biofilm-associated infections. Nanoscale. 2021;13:18632–46.
Article
CAS
PubMed
Google Scholar