Abstract
Background
Recommendations of non-HDL amplification varied from different guidelines. We aim to test the relationships between various lipid parameters and target organ damage (TOD) including aortic stiffness, peripheral arterial disease and chronic kidney disease in a community-based elderly cohort.
Methods
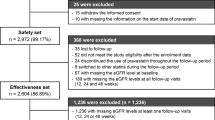
1599 (aged 71.4 ± 6.1 years) participants were recruited. Eight lipid parameters, including total cholesterol (TC), triglycerides (TG), LDL-C, HDL-C, non-HDL-C, TC/HDL ratio, TG/HDL ratio and LDL/HDL ratio, together with other plasma biomarkers like creatinine were measured. Pulse wave velocity (PWV) was measured by the SphygmoCor device, and ankle-brachial index (ABI) was assessed by Omron VP-1000 device.
Results
Four individual lipid parameters (TC, TG, LDL-C and HDL-C) significantly correlated with most, but not all, TOD indices. Meanwhile, 4 combined lipid parameters, namely non-HDL-C, TC/HDL, TG/HDL and LCL/HDL, significantly correlated with all TOD (P ≤ 0.033). In multiple linear regression analyses, 4 combined lipid parameters also significantly associated with TOD (P ≤ 0.027), while none of individual lipid parameters significantly associated with all TOD indices. In multiple logistic regression analyses, only non-HDLC and TC/HDL significantly associated with TOD (P ≤ 0.039), and other lipid parameters did not significantly associate with TOD.
Conclusion
In an elderly community sample, non-HDLC and TC/HDLC were better associated with TOD than other lipid parameters. This finding should be considered in future clinical lipid-lowing therapy.
Trial registration
This trial was retrospectively registered in ClinicalTrials.gov (No. NCT02368938, registered on 15 Feb 2015).
Similar content being viewed by others
Background
Classical lipid profiles, including total cholesterol (TC), triglycerides (TG), low-density lipoprotein (LDL) cholesterol (LDL-C) and high-density lipoprotein (HDL) cholesterol (HDL-C), were identified to play very important roles in cardiovascular diseases (CVD) over past decades. Of these lipid profiles, LDL-C is considered to be one of the strongest predictors of CVD, and lowering LDL-C is fundamental in current CVD prevention and treatment strategies [1,2,3,4]. The 2016 European Society of Cardiology guideline for the management of dyslipidemias stated that, LDL-C had to be used in primary lipid analysis and should be the primary target for treatment, while other lipid parameters could be considered in selected cases, for example, those at high risk [4]. However, this LDL-C-based cardiovascular risk assessment and lipid management did not pay much attention to the role of various lipid profiles apart from LDL-C. Numerous studies showed that other lipid profiles, for example HDL, independently associated with CVD [5]. Recent years, there were some attempts to investigate that if these individual lipid parameters could be combined to improve the risk assessment and prediction of cardiovascular events [6]. Non-HDL-C, which calculated as TC - (HDL-C), was found to be another strong independent risk factor of CVD [7]. Based on these findings, the International Atherosclerosis Society guideline recommended that non-HDL-C was as important as LDL-C and non-HDL-C should be the primary targets of therapy since it carried more information of lipids than LDL-C alone [2]. Besides, the recent American National Lipid Association guideline and British National Institute for Health and Care Excellence guideline recommended that non-HDL-C was a better risk indicator than LDL-C [1, 3]. Given the fact that different studies had various population and methodologies, the clinical significance of these combined lipid parameters was still in discussion.
Target organ damage (TOD) is the intermediate stage in the development of CVD, and is a determinant cardiovascular risk factor [8]. Because lipid profiles largely attributed to atherosclerosis, they may closely associate with vascular TOD. Thus, we investigated and compared the individual lipid parameters, which were represented by LDL-C, and the combined lipid parameters, which were represented by non-HDL-C, in association of vascular TOD, aiming to examine the clinical significance of these indices.
Methods
Study design and population
The present analysis was based on the “Northern Shanghai Study” (Registry Number: NCT02368938), whose study design and selection criteria has been published before [21]. Several studies tried to compare the effects of non-HDL-C and TC/HDL, but the difference was too little to distinguish these two lipid parameters [22, 23]. Given the fact that non-HDL-C and TC/HDL showed different aspects of the relationship of atherogenic and anti-atherogenic lipid profiles, namely the absolute difference and the ratio, the role of TC/HDL might be of great importance in risk stratification and treatment in the future.
There were some limitations in this study. As a cross-sectional study, we could not provide more information other than associations. However, the Northern Shanghai Study is an on-going study and we are doing the follow-up. Hopefully, we could have more interesting findings in the future. Second, we did not measure other lipid parameters such as apo B, which also showed its superiority over LDL-C in some studies [7]. Third, the present analysis did not include the analysis on intima-media thickness and carotid plaque, which had been regarded as an important marker of vascular TOD for several decades. However, emerging data showed that intima-media thickness might not be a good marker of TOD. Fourth, it should be pointed out that though the associations between TOD and lipid parameters were significant in our study, the correlation coefficients were not high, suggesting that TOD was a multi-factor-driven process.
Conclusion
The present analysis showed that, in this community-dwelling elderly cohort, non-HDLC and TC/HDLC were better associated with vascular TOD including arterial stiffening, PAD and CKD. This finding should be considered in future clinical practice and dyslipidemia management. Large clinical trials, especially RCTs directly comparing LDL-C and non-HDL-C as treatment target, are warranted in the future.
Abbreviations
- ABI:
-
Ankle-brachial index
- BMI:
-
Body mass index
- BP:
-
Blood pressure
- CVD:
-
Cardiovascular diseases
- eGFR:
-
Estimated glomerular filtration rate
- HDL:
-
High-density lipoprotein
- LDL:
-
Low-density lipoprotein
- PAD:
-
Peripheral arterial disease
- PWV:
-
Pulse wave velocity
- RCT:
-
Random controlled trials
- SD:
-
Standard deviation
- TC:
-
Total cholesterol
- TG:
-
Triglycerides
- TOD:
-
Target organ damage
- UACR:
-
Urine albumin-to-creatinine ratio
- VLDL:
-
Very low density lipoprotein
References
National Institute for Health and Care Excellence Lipid modification: cardiovascular risk assessment and the modification of blood lipids for the primary and secondary prevention of cardiovascular disease. NICE guidelines [CG181]. http://www.nice.org.uk/Guidance/CG181. Accessed 15 June 2017.
Grundy SM, Arai H, Barter PJ, Bersot TP, Betteridge DJ, Carmena R, et al. An international atherosclerosis society position paper: global recommendations for the management of dyslipidemia. J Clin Lipidol. 2013;7:29–60.
Jacobson TA, Ito MK, Maki KC, Orringer CE, Bays HE, Jones PH, et al. National Lipid Association Recommendations for patient-centered Management of Dyslipidemia: part 1—full report. J Clin Lipidol. 2015;9:129–69.
Catapano AL, Graham I, De Backer G, Wiklund O, Chapman MJ, Drexel H, et al. 2016 ESC/EAS Guidelines for the Management of Dyslipidaemias: The Task Force for the Management of Dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS) Developed with the special contribution of the European Assocciation for Cardiovascular Prevention & Rehabilitation (EACPR). Atherosclerosis. 2016;253:281–344.
Rader DJ, Hovingh GK. HDL and cardiovascular disease. Lancet. 2014;384:618–25.
Angelantonio ED, Gao P, Pennells L, Kaptoge S, Caslake MJ, Thompson A, et al. Lipid-related markers and cardiovascular disease prediction. JAMA. 2012;307:2499–506.
Boekholdt SM, Arsenault BJ, Mora S, Pedersen TR, LaRosa JC, Nestel PJ, et al. Association of LDL cholesterol, non-HDL cholesterol, and apolipoprotein B levels with risk of cardiovascular events among patients treated with statins: a meta-analysis. JAMA. 2012;307:1302–9.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension. Eur Heart J. 2013;34:2159–219.
Ji H, **ong J, Yu S, Chi C, Fan X, Bai B, et al. Northern shanghai study: cardiovascular risk and its associated factors in the Chinese elderly-a study protocol of a prospective study design. BMJ Open. 2017; https://doi.org/10.1136/bmjopen-2016-013880.
Van Bortel LM, Laurent S, Boutouyrie P, Chowienczyk P, Cruickshank K, De Backer T, et al. Expert consensus document on the measurement of aortic stiffness in daily practice using carotid-femoral pulse wave velocity. J Hypertens. 2012;30:445–8.
Warnick GR, Benderson J, Albers JJ. Dextran sulfate-Mg2+ precipitation procedure for quantitation of high-density-lipoprotein cholesterol. Clin Chem. 1982;28:1379–88.
Mcnamara JR, Schaefer EJ. Automated enzymatic standardized lipid analyses for plasma and lipoprotein fractions. Clin Chim Acta. 1987;166:1–8.
Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502.
Ma Y, Zuo L, Chen J, Luo Q, Yu X, Li Y, et al. Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. J Am Soc Nephrol. 2006;17:2937–44.
Havel RJ. Remnant lipoproteins as therapeutic targets. Curr Opin Lipidol. 2000;11:615–20.
Varbo A, Benn M, Tybjaerghansen A, Jorgensen A, Frikkeschmidt R, Nordestgaard BG. Remnant cholesterol as a causal risk factor for ischemic heart disease. J Am Coll Cardiol. 2013;61:427–36.
Farwell WR, Sesso HD, Buring JE, Gaziano JM. Non–high-density lipoprotein cholesterol versus low-density lipoprotein cholesterol as a risk factor for a first nonfatal myocardial infarction. Am J Cardiol. 2005;96:1129–34.
Liu J, Sempos CT, Donahue RP, Dorn J, Trevisan M, Grundy SM. Non-high-density lipoprotein and very-low-density lipoprotein cholesterol and their risk predictive values in coronary heart disease. Am J Cardiol. 2006;98:1363–8.
Veniant MM, Sullivan M, Kim SK, Ambroziak P, Chu A, Wilson MD, et al. Defining the atherogenicity of large and small lipoproteins containing apolipoprotein B100. J Clin Invest. 2000;106:1501–10.
Dzau VJ, Braunwald E. Resolved and unresolved issues in the prevention and treatment of coronary artery disease: a workshop consensus statement. Am Heart J. 1991;121:1244–63.
Castelli WP. Epidemiology of triglycerides: a view from Framingham. Am J Cardiol. 1992;70:292.
Jiang R, Schulze MB, Li T, Rifai N, Stampfer MJ, Rimm EB, Hu FB. Non-HDL cholesterol and apolipoprotein B predict cardiovascular disease events among men with type 2 diabetes. Diabetes Care. 2004;27:1991–7.
Sone H, Tanaka S, Tanaka S, Iimuro S, Ishibashi S, Oikawa S, et al. Comparison of various lipid variables as predictors of coronary heart disease in Japanese men and women with type 2 diabetes subanalysis of the Japan diabetes complications study. Diabetes Care. 2012;35:1150–7.
Acknowledgements
The authors would like to thank Prof. Jue Li from the Research Institute of Clinical Epidemiology, Tongji University School of Medicine, for his technical support.
Funding
This study is authorized and financially supported by the Shanghai municipal government (Grant ID. 2013ZYJB0902; 15GWZK1002) and the national key research and development program (2017YFC0111800). Dr. Yi Zhang is supported by the National Nature Science Foundation of China (Grant ID. 81670377). The funder did not participate in the design of the study, the collection, analysis, interpretation of the data, or the preparation of the manuscript.
Availability of data and materials
The datasets generated and analyzed during the current study are not publicly available because this study is still on-going and the follow-up is not finished, but are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
CC analyzed the patient data and was the major contributor in writing the manuscript. JT, YL and XF contributed to the preparation of blood/urine samples and lipid variables measurements. YS performed the PWV measurements, and YZ performed the ABI measurements. JX and WJ carried out the questionnaires. YZ and YX conceived and designed this study. All authors read and approved the final manuscript, and agreed to the submission of this research for publication.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study is approved by the Ethics Committee of Shanghai Tenth People’s Hospital. All participants or their legal caregivers voluntarily signed the individual informed consents.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Chi, C., Teliewubai, J., Lu, YY. et al. Comparison of various lipid parameters in association of target organ damage: a cohort study. Lipids Health Dis 17, 199 (2018). https://doi.org/10.1186/s12944-018-0800-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-018-0800-y