Abstract
Background
The swift transition to online teaching in medical education has presented the challenge of replicating in-class engagement and interaction essential for active learning. Despite online team-based learning (TBL) offering potential solutions through structured cooperative activities, its efficacy in virtual simulation experiment courses remains scantily researched. This study investigates the effectiveness of online TBL for teaching virtual patient experiments in a basic medical laboratory course and contrasts it with traditional offline teaching in terms of student performance and perceptions.
Methods
A comparative analysis involved 179 Year 3 medical students using online TBL, face-to-face TBL (FTF-TBL), and the flipped classroom (FC) approach. The learning outcomes were assessed based on experiment reports, IRAT scores, TRAT scores, and final exam performance. Students’ perceptions of both online and in-class TBL methodologies were also surveyed.
Results
Both online and in-class TBL groups demonstrated comparable academic outcomes and surpassed the FC group in academic performance. Students displayed a marked preference for the TBL format (whether online or in-class), valuing its enhancement of learning interest and practical knowledge application. Nevertheless, refinements in discussion efficiency, platform convenience, and student-instructor interaction were indicated as potential areas of improvement in the online setting.
Conclusions
Online TBL, along with its in-class counterpart, showed superior academic performance and a more positive learning experience compared to the FC group. These findings underscore the potential of online TBL in adapting to modern pedagogical challenges and enriching medical education through virtual simulation experiments.
Similar content being viewed by others

Introduction
Technological advancements are rapidly transforming medical and health education, providing rich learning environments, immersive learning experiences, and opportunities for self-paced or supplementary learning [1, 2]. The COVID-19 pandemic accelerated this transformation, triggering an urgent global shift from traditional face-to-face (FTF) teaching to virtual remote learning in academic institutions. This emergency transition has brought about unique challenges in course delivery, including adapting traditional teaching methods for effective online instruction, struggles to keep students engaged and motivated, and preserving sufficient social interaction among learners and instructors [3, 4].
To address these challenges, the fully online flipped classroom (FC) model has been touted as a promising strategy. Prior research has demonstrated that the conventional FC model—where students learn basic concepts online before class and engage in face-to-face activities during class—typically outperforms traditional teaching methods in enhancing student performance and engagement [5,6,7]. However, during the pandemic, several studies reported that students in online flipped classrooms did not achieve superior learning outcomes compared to those in traditional teaching settings, and some students expressed lower satisfaction with instructor motivation and feedback [8,9,10,Data collection and analysis Scores from IRAT, TRAT, experiment reports, and final exams across all groups were aggregated and analyzed using SPSS 26.0. Upon completing the VP experiment module, all students filled out a feedback questionnaire featuring five items on a five-point Likert scale (1 = strongly disagree; 5 = strongly agree), designed to evaluate their engagement, satisfaction, and perception of the learning experience in different teaching methods. The selection of these specific items aimed to capture students’ subjective experiences and perceptions, providing insights into the impact of TBL and FC approaches on student learning. Additional insights were gathered from the online TBL group about their virtual learning experiences. Data distribution normality was evaluated using the Kolmogorov-Smirnov test. The Kruskal-Wallis test was used to analyze the differences between groups for non-normally distributed data. Cronbach’s alpha assessed the tool’s reliability. A P-value below 0.05 denoted statistical significance. Thematic analysis of student questionnaire responses was conducted through an inductive approach. Initial themes were identified by the first author and refined in collaboration with the second author to ensure consistent interpretation. A coding framework, emergent from the data, was then applied across the dataset by the research team. This process enabled the authentic capture of student perspectives, with representative quotes selected for their relevance and clarity [36].
Results
Student performance
Figure 2 displays a comparison of the IRAT and TRAT scores between the FTF-TBL and online TBL groups. While the median TRAT scores outperformed the IRAT scores in both groups, the online TBL group’s median TRAT score was notably lower than that of the FTF-TBL group, despite similar IRAT scores. Upon assessing the academic performance of all participants in three groups, the FTF-TBL and online TBL groups demonstrated comparable scores in experiment reports and final exams, yet both outperformed the FC group, as illustrated in Fig. 3.
Student satisfaction
Of the 179 students across the three groups, 166 (representing a 92.7% response rate) completed the questionnaire on their experiences with FTF-TBL, online TBL, or FC. The results of each group were non-normally distributed according to the Kolmogorov-Smirnov test. The Cronbach’s α coefficient of the questionnaire is 0.84. As outlined in Table 1, students exposed to both FTF-TBL and online TBL methods reported these approaches as superior to FC in terms of stimulating their learning interest, enhancing learning efficiency, and improving their practical knowledge application. In general, students found FTF-TBL and online TBL more challenging than FC but were more satisfied with the TBL approaches. Comparing the two TBL groups, online TBL students felt their method was slightly less efficient and more challenging than what FTF-TBL students reported.
To better understand student views on virtual learning, we asked those in the online TBL group to compare their online experience with their prior offline TBL sessions from different modules within the same course. Of the 61 students, 51 responded: 49.0% (25/51) favored FTF-TBL, 23.5% (12/51) found online TBL superior, and 27.5% (14/51) regarded both formats as equally effective. For the open question “What areas do you believe need improvement in online TBL?”, four themes were generated from the codes: “efficiency of discussions”, “convenience of the online platform”, “student engagement”, and “interaction with the instructor”.
Efficiency of discussions
Almost a third of the respondents (33.3%, 17/51) felt that the cooperation efficiency of team discussion in online TBL could be enhanced.
It is not timely for team members to enter the breakout room, and the communication efficiency is not as good as face-to-face.
Compared with offline, team members need more time to fully understand each other’s ideas, affecting the efficiency of cooperation.
We sometimes waited for each other to speak first, and time quickly passed. This led to a decrease in the efficiency of the discussion.
Convenience of the online platform
Of the respondents, 17.6% (9/51) indicated that the software and platform usability could be improved.
Video conferencing is not easy to switch.
The window label of the video conference is not clear enough to identify the group members.
When making a mind map, only one student can operate it, and other team members cannot cooperate to edit it.
Student engagement and interaction with the instructor
Five students (9.8%, 5/51) reported insufficient engagement in group discussions. Some described that a few students did not speak, and some students found it awkward to speak in an online environment. Two students (3.9%, 2/51) expressed a desire for increased communication with the instructor. They found that they could not consult the instructor in time when they encountered problems in the experiment, and they also voiced a desire for the instructor to step in and provide guidance when team discussions were insufficient.
Discussion
Since the push for reform in medical education, accelerated by the pandemic crisis, online teaching and learning across all areas of medical and healthcare education has significantly increased [37, 38]. This shift has forced institutions to confront new challenges, such as recreating the in-class interactions and dynamics which are considered essential for engaging students in active learning instruction. With the help of the highly structured form of small group learning, online TBL provides students with opportunities to apply conceptual knowledge through active cooperative learning activities [21,22,23, 25]. However, there is limited research on the effectiveness of online implementation of such instructional strategy, particularly in the context of virtual simulation experiment courses. Therefore, in this study, we aimed to investigate the educational impact of online TBL in a Year 3 basic medical laboratory course focusing on virtual patient-based experiments. Our results show that students in the online TBL group performed as well as those in the in-class TBL group, and better than the FC group. Overall, students expressed greater satisfaction with the TBL method regardless of the environment (online or face-to-face), but they also suggested room for improvement in the online version.
Our previous research discovered that a blended learning model combining FC with TBL led to better academic outcomes and higher student satisfaction than flipped teaching alone in medical laboratory teaching [17]. Interestingly, in the present study, we further found that online TBL retained the effectiveness of its in-class counterpart in fully virtual experiments. These results align with earlier studies [23, 25], which suggest that students can successfully perform team-based activities in both online and in-class settings, with no significant difference in learning outcomes. An intriguing observation in our study was that while the IRAT scores were comparable between the online TBL and FTF-TBL groups, the TRAT scores were significantly lower in the online group. This hints at potential differences in readiness between the two settings. However, these disparities seemed to be resolved following the group application activities, including VP experiments and group discussions, as we observed no differences in the quality of experiment reports or final exam scores between the two groups.
Some studies have highlighted the role of technological proficiency for effective participation in online learning [26, 39]. While our students were comfortable with video conferencing platforms, largely due to the widespread use of online lectures, they were less familiar with online group discussion tools. This gap in familiarity could affect the quality and depth of discussions during the TRAT. Nevertheless, in the subsequent VP experiments that were focused on task-oriented learning and case study problem-solving, teachers noted more active and engaged discussions among students in the breakout rooms. This heightened level of engagement, therefore, could improve both the quality of student discussions and their sense of social interdependence [40].
In student surveys, both online and in-class TBL were perceived as more effective and satisfying than FC in stimulating learning interest, enhancing efficiency, and improving practical knowledge application. Several factors may contribute to the high levels of satisfaction observed with our online TBL approach. Firstly, it has been suggested that robust faculty development and support could offer benefits like adapting existing programs for online delivery, curating resources, and fostering faculty collaboration [41, 42]. To ensure effective practice, we consulted with experienced TBLC instructors and followed established guidelines for online flipped learning, such as develo** the orientation session pre-class, discussing each question one by one in the class, and using online tools to implement the 4 S principles [35, 43]. Secondly, most participants, including teachers and students, were relatively proficient in using different online platforms. This technological familiarity likely contributed to the smooth transition to online learning, though there’s room for further investigation to measure its specific impact on student satisfaction and learning outcomes. Thirdly, our task-oriented virtual patient experiments allowed students to tackle real-world problems and apply their theoretical knowledge in practical settings. This not only fostered positive interdependence by encouraging task-sharing among students but also helped to mitigate feelings of isolation that can sometimes accompany online learning [44].
While the online TBL approach was generally well-received by students, it is important to address the areas identified for improvement to optimize the overall learning experience. In the survey, some students pointed out specific aspects that could be enhanced, including the “efficiency of discussions”, “convenience of the online platform”, and “student engagement and interaction with the instructor”. It has been reported that students often need an adjustment period to engage effectively in online group discussions [45]. Given that our intervention spanned only a brief period of two weeks, students might not have had adequate time to acclimate to the online setting, thereby affecting the efficiency of discussions. Furthermore, effective time management and self-discipline are crucial for meaningful participation in virtual TBL [26]. Students should set objectives, manage tasks wisely, and allocate time efficiently to meet deadlines and contribute effectively to team progress. Incorporating relevant content into the pre-class orientation session could enhance the efficiency of online discussions and learning. To enhance the convenience of the online platform, introducing features like collaboratively editable documents could be beneficial. Additionally, a comprehensive platform that encompasses all facets of online TBL—including video conferencing, RAT, and group discussions—may be worth develo** in the future [22]. As for the issue of student engagement and interaction with the instructor, several strategies could be employed to enhance the digital learning environment. Strengthening the existing peer evaluation process can further minimize the “free rider” phenomenon among students, thereby fostering a heightened sense of responsibility and engagement. Instructors could also focus on creating a safe environment where students feel comfortable answering questions without fear of ridicule or blame. Additionally, instructors might increase their visits to the breakout discussion rooms to offer real-time assistance and feedback, thereby promoting more effective learning. Furthermore, future research could benefit from a deeper exploration of the facilitator’s role in online TBL settings. Effective facilitation, particularly in navigating online platforms and maintaining student participation, is crucial for TBL’s success. The facilitator’s ability to manage online discussions and provide timely feedback can significantly influence student engagement and learning outcomes. Recognizing and optimizing the facilitator’s role in virtual environments will be an important aspect of future research, especially given the rapid shift to online education.
The current study offers valuable insights into optimizing online TBL for facilitating laboratory courses. This is particularly useful for settings where there are a large number of students but limited faculty resources, or where logistical challenges exist. This educational approach not only equips students with essential skills for collaborating and learning in a digital environment but also prepares them for a healthcare sector increasingly reliant on remote and online services. The comparative analysis of online and in-class TBL in this study contributes to the novel understanding of how different teaching methodologies impact student learning, particularly in virtual simulation environments. Our findings provide a fresh perspective on the adaptability and effectiveness of TBL strategies, enriching the dialogue on educational methods in the digital age.
Limitations
This study presents several limitations warranting consideration. The focus was solely on virtual patient experiments related to the respiratory system, which may introduce a specific bias related to the source of knowledge. Coupled with the absence of random group assignments, this narrows the generalizability of the findings. Additionally, the research’s short duration could have impacted the outcomes, especially in terms of long-term retention and knowledge applicability. It’s also important to note that the study was conducted during the pandemic, a time when students were already accustomed to online learning. This could have influenced their receptiveness to the online TBL methodology. These aspects suggest that the observed differences might not solely be attributable to the instructional methods used but could also be influenced by these contextual factors. Future research addressing these constraints is necessary to provide a more comprehensive understanding of the relative effectiveness and implications of different instructional approaches in virtual simulation courses.
Conclusion
Our comparative analysis revealed that both online and in-class TBL strategies outperformed the FC method in a virtual simulation experiments setting. Students demonstrated comparable academic performance in both TBL environments, with no significant difference in learning outcomes. The online TBL approach achieved similar scores in experiment reports and final exams as its face-to-face counterpart. Students exhibited a preference for the TBL format—whether online or in-class—over FC teaching for its ability to enhance learning interest and the practical application of knowledge. Nonetheless, they also pinpointed areas for refinement in the online version, including the need for improvements in discussion efficiency, platform convenience, and student-instructor interaction. Overall, our study underscores the adaptability and effectiveness of the online TBL, especially its capacity to nurture collaboration in virtual environments, priming students for challenges in the evolving realm of digital healthcare and education.
Data availability
Datasets underpinning this study’s conclusions are provided in the article. While individual student data isn’t publicly accessible to protect student privacy, they can be obtained from the corresponding author upon a reasonable request.
Abbreviations
- FC:
-
Flipped classroom
- FTF:
-
Face-to-face
- IRAT:
-
Individual readiness assurance test
- TBL:
-
Team-based learning
- TRAT:
-
Team readiness assurance test
- VP:
-
Virtual patient
References
Grainger R, Liu Q, Gladman T. Learning technology in health professions education: realising an (un)imagined future. Med Educ.; 2023.
Plch L. Perception of technology-enhanced learning by medical students: an integrative review. Med Sci Educ. 2020;30(4):1707–20.
Al-Teete R, Hassan II, Abdul Kadir A, AbuAIRub R. Nursing lecturers’ perception toward E-learning approaches used in nursing colleges: sco** review. J Prof Nurs. 2023;46:102–10.
Tabatabaeichehr M, Babaei S, Dartomi M, Alesheikh P, Tabatabaee A, Mortazavi H, et al. Medical students’ satisfaction level with e-learning during the COVID-19 pandemic and its related factors: a systematic review. J Educ Eval Health Prof. 2022;19:37.
Chen F, Lui AM, Martinelli SM. A systematic review of the effectiveness of flipped classrooms in medical education. Med Educ. 2017;51(6):585–97.
Hew KF, Lo CK. Flipped classroom improves student learning in health professions education: a meta-analysis. BMC Med Educ. 2018;18(1):38.
Barranquero-Herbosa M, Abajas-Bustillo R, Ortego-Mate C. Effectiveness of flipped classroom in nursing education: a systematic review of systematic and integrative reviews. Int J Nurs Stud. 2022;135:104327.
Ni Gabhann-Dromgoole J, Murphy CC, Boland F, Doyle AJ, Pawlikowska T. How has medical student learning changed with the pivot to online delivery of ophthalmology in the pandemic? PLoS ONE. 2023;18(3):e0282829.
Malik PRV, Nakhla N. Instructor-blinded study of Pharmacy Student Learning when a flipped Online Classroom was implemented during the COVID-19 pandemic. Pharm (Basel) 2022;10(3).
Hew KF, Jia C, Gonda DE, Bai S. Transitioning to the new normal of learning in unpredictable times: pedagogical practices and learning performance in fully online flipped classrooms. Int J Educ Technol High Educ. 2020;17(1):57.
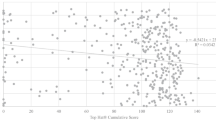
Xu Y, Chen C, Ji M, **ang Y, Han Y, Feng D, et al. An online flipped classroom approach improves the physiology score and subsequent course scores of the top-performing students. Adv Physiol Educ. 2023;47(3):538–47.
Du J, Chen X, Wang T, Zhao J, Li K. The effectiveness of the fully online flipped classroom for nursing undergraduates during the COVID-19: historical control study. Nurs Open. 2023;10(8):5766–76.
Michaelsen L, Richards B. Drawing conclusions from the team-learning literature in health-sciences education: a commentary. Teach Learn Med. 2005;17(1):85–8.
Fatmi M, Hartling L, Hillier T, Campbell S, Oswald AE. The effectiveness of team-based learning on learning outcomes in health professions education: BEME Guide No. 30. Med Teach. 2013;35(12):e1608–1624.
Burgess AW, McGregor DM, Mellis CM. Applying established guidelines to team-based learning programs in medical schools: a systematic review. Acad Med. 2014;89(4):678–88.
Dolmans D, Michaelsen L, van Merrienboer J, van der Vleuten C. Should we choose between problem-based learning and team-based learning? No, combine the best of both worlds! Med Teach. 2015;37(4):354–9.
Shen J, Qi H, Chen Y, Mei R, Sun C, Wang Z. Incorporating modified team-based learning into a flipped basic medical laboratory course: impact on student performance and perceptions. BMC Med Educ. 2022;22(1):608.
Kang HY, Kim HR. Impact of blended learning on learning outcomes in the public healthcare education course: a review of flipped classroom with team-based learning. BMC Med Educ. 2021;21(1):78.
Gopalan C, Klann MC. The effect of flipped teaching combined with modified team-based learning on student performance in physiology. Adv Physiol Educ. 2017;41(3):363–7.
Reimschisel T, Herring AL, Huang J, Minor TJ. A systematic review of the published literature on team-based learning in health professions education. Med Teach. 2017;39(12):1227–37.
Subedi N, Hirachan N, Paudel S, Shrestha B, Pradhan A, Subedee A, et al. The effectiveness of online team-based learning in introduction to medical ethics education for medical students at a medical college of Nepal: a pilot study. BMC Med Educ. 2022;22(1):766.
Jumat MR, Wong P, Foo KX, Lee ICJ, Goh SPL, Ganapathy S, et al. From trial to implementation, bringing Team-based Learning Online-Duke-NUS Medical School’s response to the COVID-19 pandemic. Med Sci Educ. 2020;30(4):1649–54.
Babenko O, Ding M, Lee AS. In-Person or online? The Effect of Delivery Mode on Team-based learning of clinical reasoning in a Family Medicine Clerkship. Med Sci (Basel) 2022;10(3).
Silva ECE, Lino-Neto T, Ribeiro E, Rocha M, Costa MJ. Going virtual and going wide: comparing Team-based learning in-class versus online and across disciplines. Educ Inf Technol (Dordr). 2022;27(2):2311–29.
DeMasi J, Harvan RA, Luca M. Online and In-class team-based learning in undergraduate immunology: a comparative analysis. Med Sci Educ. 2019;29(4):1193–9.
Shoair OA, Smith WJ, Abdel Aziz MH, Veronin MA, Glavy JS, Pirtle SJ. Pharmacy students’ perceptions and attitudes toward face-to-face vs. virtual team-based learning (TBL) in the didactic curriculum: a mixed-methods study. Med Educ Online. 2023;28(1):2226851.
Tabatabai S. COVID-19 impact and virtual medical education. J Adv Med Educ Prof. 2020;8(3):140–3.
Zhao J, Xu X, Jiang H, Ding Y. The effectiveness of virtual reality-based technology on anatomy teaching: a meta-analysis of randomized controlled studies. BMC Med Educ. 2020;20(1):127.
Berman NB, Durning SJ, Fischer MR, Huwendiek S, Triola MM. The role for virtual patients in the future of Medical Education. Acad Med. 2016;91(9):1217–22.
Kononowicz AA, Woodham LA, Edelbring S, Stathakarou N, Davies D, Saxena N, et al. Virtual Patient Simulations in Health Professions Education: systematic review and Meta-analysis by the Digital Health Education Collaboration. J Med Internet Res. 2019;21(7):e14676.
Li Yanjun HD, Guan Peng Y, Qi HC, Yanming L. Visualization analysis of knowledge structure in medical education in China by virtual simulation technology. Chin J Med Educ. 2020;40(12):992–6.
Yonghua LSW, Song Y. Application and exploration of virtual simulation experiment teaching in medical colleges and universities. High Med Educ China. 2021;2:64–5.
Yuan YB, Wang JJ, Lin MH, Gao XY. Building virtual simulation teaching platform based on electronic standardized patient. Sheng Li Xue Bao. 2020;72(6):730–6.
Chen AD, Wang JJ, Gao XY. A preliminary study on the construction of the triad medical experimental system. Sheng Li Xue Bao. 2020;72(6):724–9.
Malik AS, Malik RH. Twelve tips for conducting team-based learning session online in synchronous setting. Med Teach. 2022;44(5):486–93.
Virginia BVC. Using thematic analysis in psychology. Qualitative Res Psychol. 2006;3(2):77–101.
Lockee BB. Online education in the post-COVID era. Nat Electron. 2021;4:5–6.
Martin F, Sun T, Westine CD. A systematic review of research on online teaching and learning from 2009 to 2018. Comput Educ. 2020;159:104009.
Venkatesh S, Rao YK, Nagaraja H, Woolley T, Alele FO, Malau-Aduli BS. Factors influencing medical students’ experiences and satisfaction with blended Integrated E-Learning. Med Princ Pract. 2020;29(4):396–402.
Richards S. Faculty Perception of Student Engagement in online anatomy Laboratory courses during the COVID-19 pandemic. Med Sci Educ. 2023;33(2):465–80.
Gordon M, Patricio M, Horne L, Muston A, Alston SR, Pammi M, et al. Developments in medical education in response to the COVID-19 pandemic: a rapid BEME systematic review: BEME Guide No. 63. Med Teach. 2020;42(11):1202–15.
Daniel M, Gordon M, Patricio M, Hider A, Pawlik C, Bhagdev R, et al. An update on developments in medical education in response to the COVID-19 pandemic: a BEME sco** review: BEME Guide No. 64. Med Teach. 2021;43(3):253–71.
Regmi K, Jones L. A systematic review of the factors - enablers and barriers - affecting e-learning in health sciences education. BMC Med Educ. 2020;20(1):91.
Shimizu I, Matsuyama Y, Duvivier R, van der Vleuten C. Perceived positive social interdependence in online versus face-to-face team-based learning styles of collaborative learning: a randomized, controlled, mixed-methods study. BMC Med Educ. 2022;22(1):567.
Valaitis RK, Sword WA, Jones B, Hodges A. Problem-based learning online: perceptions of health science students. Adv Health Sci Educ Theory Pract. 2005;10(3):231–52.
Acknowledgements
The authors wish to express their profound gratitude to the Faculty Development Center of Zhejiang University School of Medicine for its generous support.
Funding
This work was supported by the Zhejiang Province “14th Five-Year” Teaching Reform Research Project (jg20220038); and the Zhejiang University School of Medicine High-level Education and Teaching Achievement Award Cultivation Project (cgyb20192001).
Author information
Authors and Affiliations
Contributions
JS was integral in study design, data analysis, and manuscript drafting. JS and HQ collaborated on data collection, analysis, and manuscript review. RM and CS assisted in data collection. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Zhejiang University School of Medicine (IRB 2023-002). Before participating, all individuals provided their informed consent. All research procedures adhered to the guidelines set by the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shen, J., Qi, H., Mei, R. et al. A comparative study on the effectiveness of online and in-class team-based learning on student performance and perceptions in virtual simulation experiments. BMC Med Educ 24, 135 (2024). https://doi.org/10.1186/s12909-024-05080-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-024-05080-3