Abstract
Background
Climate change has significant implications for health, yet healthcare provision itself contributes significant greenhouse gas emission. Medical students need to be prepared to address impacts of the changing environment and fulfil a key role in climate mitigation. Here we evaluate the effectiveness of an online module on climate-change and sustainability in clinical practice designed to achieve learning objectives adapted from previously established sustainable healthcare priority learning outcomes.
Methods
A multi-media, online module was developed, and 3rd and 4th year medical students at Brighton and Sussex Medical School were invited to enrol. Students completed pre- and post-module questionnaires consisting of Likert scale and white space answer questions. Quantitative and qualitative analysis of responses was performed.
Results
Forty students enrolled and 33 students completed the module (83% completion rate). There was a significant increase in reported understanding of key concepts related to climate change and sustainability in clinical practice (p < 0.001), with proportion of students indicating good or excellent understanding increasing from between 2 – 21% students to between 91 – 97% students. The majority (97%) of students completed the module within 90 min. All students reported the module was relevant to their training. Thematic analysis of white space responses found students commonly reported they wanted access to more resources related to health and healthcare sustainability, as well as further guidance on how to make practical steps towards reducing the environmental impact within a clinical setting.
Conclusion
This is the first study to evaluate learner outcomes of an online module in the field of sustainable health and healthcare. Our results suggest that completion of the module was associated with significant improvement in self-assessed knowledge of key concepts in climate health and sustainability. We hope this approach is followed elsewhere to prepare healthcare staff for impacts of climate change and to support improving the environmental sustainability of healthcare delivery.
Trial registration
Study registered with Brighton and Sussex Medical School Research Governance and Ethics Committee (BSMS RGEC). Reference: ER/BSMS3576/8, Date: 4/3/2020.
Similar content being viewed by others
Background
Anthropogenic climate change has been described as the greatest global health threat of the 21st century [1] and disproportionately affects vulnerable populations [2], contributing to global injustice. It is predicted 250,000 additional deaths per year by 2030 will be attributable to climate sensitive diseases [3]. Air pollution is the biggest environmental cause of death, predicted to contribute towards seven million deaths annually [4]. Whilst planetary health impacts human health, the healthcare sector itself contributes to climate change, representing an estimated 4.4% of global greenhouse gas emissions [5]. In many nations, including the UK, health services have set targets to reach net zero carbon emissions [6, 7].
There are calls to embed climate-health and sustainability education into medical curricula, and the General Medical Council (GMC) 2018 outcomes for graduates [8] stipulate that ‘newly qualified doctors must be able to apply the principles, methods and knowledge of population health and the improvement of health and sustainable healthcare to medical practice. The Greener NHS programme identifies that staff ‘will need to be supported to learn, innovate and embed sustainable development into everyday actions’ [6]. Hence, medical students need to be prepared to address and manage the impacts of the changing environment [9] as well as to fulfil a key role in climate mitigation and health service adaptation [10]. Along with the American Medical Association which supports teaching on climate change in undergraduate curricula [11], the association for Medical Education in Europe (AMEE) recommends integration of climate-health and sustainability education and finds that graduates are not prepared for these roles [12]. In fact, globally only 15% of Medical Schools include climate change in their curricula [13]. While the Planetary Health Report Card Initiative (PHRC), an advocacy tool that allows medical schools to measure progress towards programmatic improvement, describes some progress on integration of climate change into curricula in 5 countries [14], PHRC has not yet been taken up in the rest of the world. As a result, medical students continue to call for their education to be adapted [15].
Discussions on the optimum approach to integrating climate-health and sustainability into medical curricula are ongoing [12, 16, 17] but the importance of mainstreaming education for sustainable healthcare as a transdisciplinary theme throughout undergraduate curricula has been emphasized [12, 17]. Tun et al. identified a lack of knowledgeable educators as the biggest barrier to implementation of teaching and learning on climate-health and sustainability and recommend pooling of resources (including online modules) to support delivery of teaching [16]. Walpole et al. also found lack of faculty expertise, and additionally highlighted difficulties in securing an allocation of core curriculum time and resources [17]. It has been pointed out that expert material is available [10] with organisations including the Global Consortium on Climate and Health Education (GCCHE) working to develop, pool and share resources and educational practices worldwide [18], as well as initiatives such as the PHRC providing a platform to share ideas and resources as well as evaluate and compare medical schools engagement with education of sustainable healthcare [14, 19].
Online teaching has been successfully employed in various other aspects of the medical curriculum, and meta-analyses show that students perform at least as well, or better, after online learning compared to face-to-face sessions [20, 21]. Large scale adoption of online teaching formats throughout the early stages of the COVID-19 pandemic [22] highlight the potential feasibility of these approaches. Whereas there are a number of online training platforms for climate and health [18], we do not know of any study to date that has evaluated a climate-health and sustainability module for medical students or other healthcare staff. Such a module could be a useful tool to support student learning, would not require faculty for delivery, and could be easily disseminated.
The primary aim of our study was to design and evaluate an online module aimed at 3rd and 4th year UK medical students entitled ‘Climate Change and Sustainability in Clinical Practice’. Secondary aims were to assess students’ attitudes towards education on themes related to climate change and sustainability in healthcare.
Methods
Study design
This was an uncontrolled, before and after study design to evaluate a pilot module on climate change. Students were enrolled into the E-learning module: ‘Climate Change and Sustainability in Clinical Practice’ and completed a pre-module questionnaire, post-module questionnaire, and module evaluation.
Intervention and content
With support from experts in medical education, learning technology, and sustainable healthcare, we designed and developed an E-learning module using WordPress© software, titled: ‘Climate Change and Sustainability in Clinical Practice’ (hereafter referred to as ‘the module’). As recommended by expert groups [23], Mayer’s design principles of multimedia learning [24] were used in develo** the module, as well as computer-based teaching module design principles outlined by Lau et al. [25] The module aimed to achieve learning objectives adapted from previously established priority learning outcomes [26], namely for learners to be able to describe the interactions of the environment and human health at different levels, and to develop knowledge in how to improve the environmental impact and sustainability of clinical pathways.
The module consists of four chapters (Fig. 1 and supplementary material 1, 2, 3, 4 and 5):
-
‘Climate Change: Sustainability Driver in Healthcare’ outlines the direct and indirect health threats of climate change, and key global and local commitments to climate mitigation.
-
‘Environmental Impacts of Healthcare and Healthcare’s Carbon Hotspots’ examines the environmental impact of health and social care in the UK, illustrated using example clinical pathways.
-
‘Principles of Sustainable Clinical Practice’ describes four previously described sustainable clinical principles [25] and invites students to consider how these can be applied in various healthcare settings.
-
‘Health Co-Benefits of Climate Mitigation’ uses case-based scenarios to examine how clinicians can advise patients to take steps that improve both their individual health and environmental impact.
Each chapter concludes with a quiz followed by detailed explanations of the answers including links to further reading. There was no grading or recording of results.
Participants and enrolment
An email was circulated fortnightly in June and July 2020 inviting all 3rd and 4th year medical students (including students intercalating between their 3rd and 4th year) at Brighton & Sussex Medical School (BSMS) to enrol in the pilot study (n = 316). Students who enrolled were entered into a prize draw for two £20 vouchers, and those who completed the module were able to download a certificate.
Survey
Online pre- and post-module surveys were developed using Qualtrics© Software with input from medical educators at University Hospitals Sussex, and BSMS. The pre- module survey used 5-point Likert scale questions to assess students’ attitudes to sustainability in healthcare, as well as subjective, self-reported understanding of four key concepts linked to the module learning objectives. These same questions were included in the post-module survey, alongside module evaluation questions to assess the ease of use and the relevance and appropriateness of modules content. Survey completion was voluntary and anonymous. (See supplementary material).
Statistical analysis
Survey responses were converted into numerical values and tested for normality using a Shapiro–Wilk test. Differences between pre- and post-module responses regarding understanding of each of the four key concepts were assessed using Mann Whitney U tests (SPSS v26, IBM New York), with significance set at p < 0.05.
Thematic analysis of free text responses was performed using a general inductive approach [27]. Multiple readings were performed, and categories identified and defined by investigators. Responses within each category were coded into themes. This process was performed independently by investigator HD and TT, their analyses were compared, and final categories and themes agreed.
Results
There were 55 responses to the pre-module questionnaire and 33 for the post module questionnaire. Of the 33 students that completed the post-module questionnaire, around two thirds of students (21/33; 63%) completed this module in one attempt, with 10 students taking two attempts, one student took three attempts, and another took four. Students were required to take the pre-module questionnaire on each attempt, therefore, 40 students enrolled onto the module (40/316 = 13% response rate). Of these, 33 completed the module and post-module surveys (33/40 = 83% completion rate).
Three of the 55 responses to the pre-module questionnaire were left blank and were excluded from analysis.
Module performance and participant’s motivations
The majority of students (32/33; 97%) reported completing the module within 90 min, and most frequently in 30–60 min (19/33, 58%). All students agreed that the module was: appropriate for their level of training; relevant to their training; and that ‘all students should enrol in the E-module during their training’. Almost all students (32/33; 97%) agreed that the module was easy to use. Students’ motivation to participate was assessed. Common themes in students’ responses to the question: ‘Why did you choose to participate in this pilot study?’ were identified (Fig. 2).
Module impact on student reported understanding of key themes
The post-module evaluation demonstrated a significant increase in understanding of each of the four key concepts related to climate change, health, and sustainability in healthcare (p < 0.001) Table 1. Pre-module understanding of each theme was rated as good 1/52 (2%) or excellent by 11/52 (21%) students, this improved to between 30 – 32/52 (91 – 97%) students after completion of the module. Prior to undertaking the module ‘the environmental impact of clinical pathways’ was the least well understood theme with most students (41/52; 79%) reporting terrible or poor understanding. After the module no students reported terrible or poor understanding and 31/33 (94%) reported good or excellent understanding.
Module impact on attitudes towards sustainability and healthcare
Prior to completing the module, the majority of the students felt that they had received ‘far too little’ (28/52; 54%), or ‘too little’ (22/52; 42%) teaching on climate change and health. On completion of the module all students felt that both ‘understanding the implication of climate change on health and healthcare’, and ‘improving the sustainability of clinical practice’ were very important. Almost all students (32/33; 97%) agreed with the statement ‘healthcare workers have a responsibility to reduce the environmental impact of the NHS’.
Module evaluation white space answers
Free text responses to white space questions were almost entirely positive. Responses to the questions ‘What did you like the most about this module?’ and ‘Any other comments’ were classified into four categories: function, value, content, and teaching devices (Fig. 3). Common themes included positive comments surrounding the module interactivity and use of integrated videos, as well as students highlighting the importance of the topics covered and perceived relevance to their training.
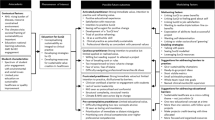
Responses to the questions ‘What things could be improved?’ and ‘What other teaching of sustainable healthcare would you value?’ were classified into three categories: function, content, and practical application (Fig. 4). Here we found students commonly reported a desire for more resources related to the topics covered, as well as further guidance on how to make practical steps towards achieving a net-zero health service. Students indicated that their user experience would have been improved through inclusion of a ‘go back’ button within quizzes, and we have been able to implement this.
Module evaluation Thematic analysis: ‘What things could be improved?’ and ‘What other teaching of sustainable healthcare would you value?. Legend: wheel infographics that present categories and themes identified and agreed by investigators in the thematic analysis of student’s feedback. Categories, into which responses were coded are represented in the centre circle of the wheel (green) The three most significant themes within each category are displayed in the second circle (grey). A direct quotation from student’s responses coded into relevant categories is displayed in the outer circle (blue)
Discussion
Here we describe development of an online self-directed learning resource which sought to introduce medical students to important concepts in climate health and sustainability, aligned with identified priority learning outcomes [26, 28]. To our knowledge, this is the first study to evaluate learner outcomes of an online module in the field of sustainable health and healthcare. Student feedback indicated good module usability and applicability, and our results suggest that completion of the module was associated with significant improvement in self-assessed knowledge of key concepts in climate health and sustainability.
Our findings also support the notion that medical students recognise the importance of climate-health and sustainability but feel that their current curriculum does not include sufficient teaching on the topic [29]. Our module sought to address this, takes around 1.5 h to complete, and because it is delivered online and does not require physical resources or expert faculty for its delivery, can easily be integrated into medical curricula.
Several students commented that they would value teaching on practical applications of the modules content, including how individuals can make a difference to sustainability of healthcare, and this would add value to future iterations of this module. As understanding of key concepts in health and climate change increases amongst healthcare professionals, this should be aligned with teaching and learning in sustainable quality improvement to support real-world action [26, 30].
The module has been further developed based on student feedback provided from this study and is being integrated into the undergraduate curriculum at BSMS medical school. The online module will be available to students to supplement their learning alongside the sustainability in healthcare modules which are incorporated throughout the curriculum [31]. We intend to expand access to the module to support learning on climate change and sustainable clinical practice amongst healthcare professionals at our local hospitals. As knowledge in this field is relatively independent of clinical seniority, this module may also prove be helpful at a postgraduate level. This aligns with plans by the team at the Greener NHS [6] for an online module to build sustainable development knowledge and capability in all healthcare staff.
There are some limitations to this study. We did not perform any formative assessment to assess understanding of key themes, and instead have interpreted students perceived improvement of understanding. We did not receive the same number of pre- and post- module responses, which limited some analyses. Despite this, differences between pre- and post-module scores were significant at p < 0.001. The questionnaire method was limited by the fact that students who took more than one attempt to complete the module had to complete the pre-module questionnaire on each attempt. The low response rate indicates probable selection bias, and it is likely that students who are interested in the topic were more likely to participate. However, almost four fifths of participants rated their understanding of each of four key concepts related to climate change and sustainable clinical practice as worse than average. This reported low knowledge even amongst those predisposed to such learning further supports the need to develop more teaching and learning on this topic.
We hope that our approach is emulated elsewhere, as this will help to support making delivery of health and healthcare more environmentally sustainable.
Availability of data and materials
The datasets used and/or analysed during the current study are available included in this published article and its supplementary information files.
Abbreviations
- NHS:
-
National Health Service
- GMC:
-
General Medical Council
- BSMS:
-
Brighton and Sussex Medical School
- AMEE:
-
Association for Medical Education in Europe
- GCCHE:
-
Global Consortium on Climate and Health Education
- PHRC:
-
Planetary Health Report Card
References
Costello A, Abbas M, Allen A, Ball S, Bell S, Bellamy R, et al. Managing the health effects of climate change: Lancet and University College London Institute for Global Health Commission. Lancet. 2009;373(9676):1693–733.
Watts N, Amann M, Arnell N, Ayeb-Karlsson S, Belesova K, Boykoff M, et al. The 2019 report of The Lancet Countdown on health and climate change: ensuring that the health of a child born today is not defined by a changing climate. Lancet. 2019;394(10211):1836–78.
Climate change. World Health Organisation Website. https://www.who.int/health-topics/climate-change#tab=tab_1 Accessed 20 Feb 2021.
World Health Organization. Ambient air pollution: a global assessment of exposure and burden of disease. Geneva: Switzerland; 2016.
Lenzen M, Malik A, Li M, Fry J, Weisz H, Pichler PP, et al. The environmental footprint of health care: a global assessment. Lancet Planet Health. 2020;4(7):e271–9.
England N, Improvement N. Delivering a ‘net zero’ national health service. London: NHS England and NHS Improvement; 2020.
Wise J. COP26: Fifty countries commit to climate resilient and low carbon health systems. British Med J Publishing Group. 2021;9:375:n2734.
Council GM. Outcomes for graduates. London: General Medical Council; 2018.
Walpole SC, Mortimer F. Evaluation of a collaborative project to develop sustainable healthcare education in eight UK medical schools. Public Health. 2017;150:134–48.
Maxwell J, Blashki G. Teaching About Climate Change in Medical Education: An Opportunity. J Public Health Res. 2016;5(1):673.
Association AM. Resolution #A19–302: Climate Change Education Across the Medical Education Continuum. In: 2020. https://www.psr.org/wp-content/uploads/2019/07/ama-climate-change-education-policy-2019.pdf Accessed 20 June 2022
Shaw E, Walpole S, McLean M, Alvarez-Nieto C, Barna S, Bazin K, Behrens G, Chase H, Duane B, El Omrani O, Elf M. AMEE consensus statement: planetary health and education for sustainable healthcare. Med Teach. 2021;43(3):272–86.
Omrani OE, Dafallah A, Paniello Castillo B, Amaro BQ, Taneja S, Amzil M, Sajib MR, Ezzine T. Envisioning planetary health in every medical curriculum: an international medical student organization’s perspective. Med Teach. 2020;42(10):1107–11.
Hampshire K, Islam N, Kissel B, Chase H, Gundling K. The Planetary Health Report Card: a student-led initiative to inspire planetary health in medical schools. Lancet Planetary Health. 2022;6:e449–54.
International Federation of Medical Students’ Associations (IFSMA). Policy on Climate Change and Health (2018) https://ifmsa.org/wpcontent/uploads/2018/09/GS_AM2018_Policy_Climate-Change-and-Health_final.pdf. Accessed 16 Apr 2022.
Tun MS. Fulfilling a new obligation: Teaching and learning of sustainable healthcare in the medical education curriculum. Med Teach. 2019;41(10):1168–77.
Walpole SC, Barna S, Richardson J, Rother HA. Sustainable healthcare education: integrating planetary health into clinical education. Lancet Planet Health. 2019;3(1):e6–7.
Global consortium climate and health education website and mission statement. https://www.publichealth.columbia.edu/research/global-consortium-climate-and-health-education. Accessed 16 Apr 2021.
Chase H, Hampshire K, Tun S. Improving the medical curriculum on planetary health and sustainable healthcare. BMJ. 2022;376:o209.
Richmond H, Copsey B, Hall AM, Davies D, Lamb SE. A systematic review and meta-analysis of online versus alternative methods for training licensed health care professionals to deliver clinical interventions. BMC Med Educ. 2017;17(1):1–4.
Pei L, Wu H. Does online learning work better than offline learning in undergraduate medical education? A systematic review and meta-analysis. Med Educ Online. 2019;24(1):1666538.
Wayne DB, Green M, Neilson EG. Medical education in the time of COVID-19. Sci Adv. 2020;6(31):eabc7110.
Candler C, editor Effective use of educational technology in medical education. Colloquium on educational technology: recommendations and guidelines for medical educators Washington, DC: AAMC Institute for Improving Medical Education; 2007.
Mayer R, Mayer RE. The Cambridge handbook of multimedia learning. Cambridge: Cambridge university press; 2005.
Lau KH. Computer-based teaching module design: principles derived from learning theories. Med Educ. 2014;48(3):247–54.
Thompson T, Walpole S, Braithwaite I, Inman A, Barna S, Mortimer F. Learning objectives for sustainable health care. Lancet. 2014;384(9958):1924–5.
Thomas DR. A general inductive approach for analyzing qualitative evaluation data. Am J Eval. 2006;27(2):237–46.
Walpole SC, Mortimer F, Inman A, Braithwaite I, Thompson T. Exploring emerging learning needs: a UK-wide consultation on environmental sustainability learning objectives for medical education. Int J Med Educ. 2015;6:191–200.
Ryan EC, Dubrow R, Sherman JD. Medical, nursing, and physician assistant student knowledge and attitudes toward climate change, pollution, and resource conservation in health care. BMC Med Educ. 2020;20(1):200.
Mortimer F, Isherwood J, Wilkinson A, Vaux E. Sustainability in quality improvement: redefining value. Future Healthc J. 2018;5(2):88–93.
Teaching and Learning on Sustainable Healthcare. BSMS Sustainable Healthcare Group website. https://www.bsms.ac.uk/about/sustainability.aspx. Accessed 4 Apr 2022.
Acknowledgements
Not applicable
Funding
No sources of funding were used for this research project.
Author information
Authors and Affiliations
Contributions
HD developed the online module, undertook the research and data collection, performed analysis of the data, prepared the manuscript. CR, AJ, MB, and MO were major contributors to preparation of the manuscript and development of the module. CR and TT supported the quantitative and qualitative analysis of the results. SB and CJT and CR were major contributors to the development of the online module and planning data collection. All authors read and approved the final manuscript.
Author’s information
Henry Dunne is a Core Surgical Trainee (ENT Themed) in East of England. He was an academic foundation trainee at Brighton and Sussex University Hospital trust, and an honorary clinical education fellow at Brighton and Sussex Medical School. While completing his PGCert in Medical Education he led the development of this online module on climate change and sustainable clinical practice. In his clinical, and academic work he has special interest in improving sustainability of healthcare delivery.
Chantelle Rizan is an ENT Research Fellow at University Hospitals Sussex NHS Trust and Honorary Clinical Lecturer at Brighton and Sussex Medical School (BSMS), and former Sustainable Surgery Fellow at CSH. Chantelle is in the last year of her PhD at BSMS in which she uses carbon footprinting and life cycle assessment methods to identify carbon hotspots within the operating theatre, and to evaluate alternative products and processes with lower environmental impact. This PhD was funded by Health Education England and a Surgical Research Fellowship from the Royal College of Surgeons of England (RCSEng). Chantelle seeks to translate her research into practice and to influence policy as a founding member of the RCSEng Sustainability in Surgery working group and is working with the UK Health and Climate Change Alliance as an academic advisor on a national report on how to meet Net Zero Carbon within surgery.
Anna Jones, is a public health consultant and clinical teaching fellow at Brighton and Sussex Medical School where she is currently the project lead for sustainable healthcare in undergraduate medical education.
Professor Mahmood F Bhutta is the Chair in ENT Surgery at Brighton & Sussex Medical School and has a longstanding interest in health systems and sustainability. In partnership with the UK Health Alliance on Climate Change he is chairing a national report into sustainable surgery and working with the Royal College of Surgeons of England and the Centre for Sustainable Healthcare to develop educational resources on this topic.
Tom Taylor is an Academic Clinical Fellow and Ophthalmology Trainee in the Wessex Deanery. He has previously worked at the Wolfson Institute of Preventive Neurology at Queen Mary University of London and went to medical school at the University of Oxford.
Stefi Barna MPH, is the Director of Education at the Centre for Sustainable Healthcare (UK) and Associate Professor of Public Health and Sustainability at Azim Premji University (India) and Queen Mary University of London (UK).
CJ Taylor is a learning technologist at Brighton and Sussex Medical School. She undertakes technology-based teaching projects and provided pedagogic advice and guidance and support on the use of technology in teaching and learning to academic staff. Research area technology enhanced learning.
Professor Michael Okorie is a Clinical Academic at Brighton and Sussex Medical School with a background in clinical pharmacology & therapeutics. He has an interest in the teaching and learning of safe, effective, and sustainable prescribing and is keen to utilise education and training to equip students and healthcare professionals with appropriate knowledge, skills and attitude in relation to climate change. Mike is also a Consultant Physician and the Associate Medical Director for Medicines Safety and Prescribing at University Hospitals Sussex.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval to undertake this study was granted by Brighton and Sussex Medical School Research, Governance and Ethics Committee (RGEC) Reference: ER/BSMS3576/8, Date: 4/3/2020. All methods were performed in accordance with relevant guidelines and regulations.
Informed consent was obtained from all participating subjects.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dunne, H., Rizan, C., Jones, A. et al. Effectiveness of an online module: climate-change and sustainability in clinical practice. BMC Med Educ 22, 682 (2022). https://doi.org/10.1186/s12909-022-03734-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-022-03734-8