Abstract
Background
Fractures involving the posterior acetabulum with its rich vascular and neural supply present challenges in trauma orthopedics. This study evaluates the effectiveness of 3D printing technology with the use of custom-made metal plates in the treatment of posterior wall and column acetabular fractures.
Methods
A retrospective analysis included 31 patients undergoing surgical fixation for posterior wall and column fractures of the acetabulum (16 in the 3D printing group, utilizing 3D printing for a 1:1 pelvic model and custom-made plates based on preoperative simulation; 15 in the traditional group, using conventional methods). Surgical and instrument operation times, intraoperative fluoroscopy frequency, intraoperative blood loss, fracture reduction quality, fracture healing time, preoperative and 12-month postoperative pain scores (Numeric Rating Scale, NRS), hip joint function at 6 and 12 months (Harris scores), and complications were compared.
Results
The surgical and instrument operation times were significantly shorter in the 3D printing group (p < 0.001). The 3D printing group exhibited significantly lower intraoperative fluoroscopy frequency and blood loss (p = 0.001 and p < 0.001, respectively). No significant differences were observed between the two groups in terms of fracture reduction quality, fracture healing time, preoperative pain scores (NRS scores), and 6-month hip joint function (Harris scores) (p > 0.05). However, at 12 months, hip joint function and pain scores were significantly better in the 3D printing group (p < 0.05). Although the incidence of complications was lower in the 3D printing group (18.8% vs. 33.3%), the difference did not reach statistical significance (p = 0.433).
Conclusion
Combining 3D printing with individualized custom-made metal plates for acetabular posterior wall and column fractures reduces surgery and instrument time, minimizes intraoperative procedures and blood loss, enhancing long-term hip joint function recovery.
Clinical Trial Registration
12/04/2023;Trial Registration No. ChiCTR2300070438; http://www.chictr.org.cn.
Similar content being viewed by others
Introduction
The anatomical structure of acetabular fractures is exceptionally complex, particularly in cases involving fractures of the posterior wall and column. Due to the abundant vascular and neural supply in the posterior acetabulum, surgical procedures pose significant risks and challenges, even for experienced orthopedic surgeons [1, 2]. Surgical treatment is commonly employed for posterior wall and column fractures of the acetabulum, with anatomical reduction being a crucial determinant for achieving favorable postoperative functional recovery [3, 4]. Traditional surgical treatment of complex acetabular fractures involves assessing the fracture type based on the physician’s experience and imaging data, and then formulating surgical plans. During surgery, doctors often temporarily bend conventional anatomical plates to better match the reduced position of the acetabular fracture. This process involves significant surgical risks and challenges. With the advancement of digital orthopedic technology, 3D printing has found increasing application in the clinical treatment of complex fractures in recent years. Physicians can intuitively understand the extent and type of fracture injury through 3D models, facilitating preoperative surgical planning and aiding in comparing intraoperative fracture reduction, with some positive outcomes [5,2).
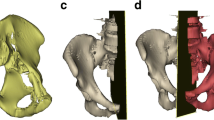
Computer-aided three-dimensional modeling of fracture patterns and the production of individualized custom-made metal plates (a) Three-dimensional fracture model simulated using Mimics software (b) Three-dimensional fracture model after computerized virtual reduction (c) Confirmation of the screw directions and lengths for individualized custom-made metal plates, ensuring that the implanted screws will not enter the joint cavity (d) Positioning of individualized custom-made metal plates on the virtually reduced fracture model, along with the recommended lengths for each screw on the metal plates
Surgical technique
All surgeries were performed by an experienced trauma orthopedic surgeon. After the patient was placed under general anesthesia, they were positioned in the lateral decubitus position, and the hip area and the affected limb were disinfected with iodine. Sterile drapes were used to cover the area. Both groups of patients underwent the Kocher-Langenbeck approach, with an incision starting from the posterior superior iliac spine and curving downward over the apex of the greater trochanter of the femur, extending vertically for approximately 15 cm. During the surgery, the incision could be extended as needed to adequately expose the acetabular posterior wall and column fractures (Fig. 3).
In the 3D printing group, the fractures were reduced based on the preoperative 3D physical models, and individualized custom-made metal plates, designed and fabricated beforehand, were applied. The metal plates were fixed in place by adhering to the pre-designed bony landmarks according to the model (Fig. 4). In the traditional surgery group, the fractures were reduced based on the surgeon’s experience, and conventional metal plates were contoured and fixed based on the reduced fractures. In both the 3D printing group and the traditional surgery group, the lengths of the screws were measured and implanted at appropriate positions. Intraoperative fluoroscopy was used to assess the reduction of the fractures, determine the positioning of the metal plates, ensure that the screws did not penetrate into the acetabulum, and conduct multidirectional mobility tests of the affected hip joint. The stability of the fracture fragments was observed to ensure the success of the surgery.
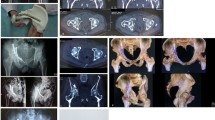
A 21-year-old patient with a right acetabular posterior wall and column fracture (3D printing group) (a) Preoperative X-ray (anteroposterior view) (b) three-dimensional reconstructed computed tomography (CT) images (c) 3D-printed model of the fracture (anteroposterior and lateral views) (d) 3D-printed models after computer virtual reduction and customized individualized metal plate fitting (anteroposterior and lateral views) (e) Postoperative day one pelvic X-ray (anteroposterior view) (f) Follow-up pelvic X-ray at 3 months postoperatively (anteroposterior view)
Postoperative management
On the first day after surgery, both groups of patients underwent pelvic anteroposterior X-ray examination. During hospitalization, routine analgesic medication and subcutaneous injections of anticoagulants were administered. After discharge, oral anticoagulants were prescribed for 2 weeks to prevent deep venous thrombosis in the lower limbs. Follow-up visits were scheduled every month during the postoperative period, and pelvic anteroposterior X-ray images were obtained, with a minimum follow-up time of 12 months. On the day of the surgery, active rehabilitation exercises were initiated for the affected side hip joint, followed by partial weight-bearing exercises after 6 weeks. At 3 months postoperatively, full weight-bearing exercises were allowed based on the X-ray findings.
Evaluation indicators
Compare the data between the two groups, including patient age, gender, BMI, length of hospital stay, time from injury to surgery, and average follow-up time.The surgical time and instrument operation time were recorded for both groups. Surgical time was defined as the time from skin incision to suture completion, while instrument operation time was defined as the time from the beginning of adjusting and placing the metal plate to the insertion of the last screw. The 3D printing model time referred to the time from design to the printing of the physical model of the fracture. The custom-made metal plate production time was defined as the time from design to the processing of the individualized custom-made metal plate. Intraoperative blood loss and the number of intraoperative fluoroscopy procedures were also recorded. Intraoperative blood loss was calculated by measuring the volume of flushing fluid, blood in the suction bottle, and blood in the gauze. The number of intraoperative fluoroscopy procedures referred to the total number of times fluoroscopy was performed during the surgery. Radiological evaluations were conducted by two experienced orthopedic surgeons, and the radiological results were scored based on the maximum residual displacement of the postoperative fracture: fracture reduction quality was classified as good (0–2 mm displacement) or fair (≥ 2 mm displacement). Both groups of patients utilized the Numeric Rating Scale (NRS) to assess fracture pain preoperatively, employing a scale from 0 (“no pain”) to 10 (“unbearable fracture pain”), where each integer denoted one unit of pain intensity. Subsequently, 12 months after the operation, patients underwent follow-up assessments for NRS pain scoring. At 6 and 12 months postoperatively, hip joint function was evaluated using the Harris scoring system [10]: hip joint function was considered excellent/good (Harris score ≥ 80 points) or fair/poor (Harris score < 80 points). Complications included inflammatory reactions, heterotopic ossification, infection, nonunion of the fracture, iatrogenic nerve symptoms, and traumatic arthritis.
Statistical analysis
Statistical analysis was performed using SPSS software (version 26.0, USA). Categorical variables were presented as numbers or percentages, while continuous variables were presented as mean ± standard deviation. Fisher’s exact test was used to assess categorical variables. The Shapiro-Wilk test was used to assess whether continuous variables followed a normal distribution. For normally distributed continuous variables, such as age, BMI, time from injury to surgery, instrument operation time, and fracture healing time, independent sample t-tests were used for analysis. For non-normally distributed continuous variables, such as length of hospital stay, average follow-up time, surgical time, number of X-ray fluoroscopy procedures, and intraoperative blood loss, Mann-Whitney U tests were used for analysis. The significance level for all statistical tests was set at p < 0.05.
Results
Demographic and clinical data
This study included a total of 31 patients, with 16 patients in the 3D printing group (13 males and 3 females), with a mean age of 35.2 ± 9.5 years and a mean BMI of 25.0 ± 3.1 kg/m². The traditional group comprised 15 patients (10 males and 5 females) with a mean age of 37.3 ± 10.8 years and a mean BMI of 24.5 ± 2.4 kg/m². Demographic characteristics between the two groups were similar (all p > 0.05). The length of hospital stay in the 3D printing group (mean 11.6 ± 1.7 days) was slightly longer than that in the traditional group (mean 10.9 ± 1.8 days), but the difference was not statistically significant (p = 0.276). The time from injury to surgery in the 3D printing group (mean 154.3 ± 21.5 h) was longer than that in the traditional group (mean 142.8 ± 20.9 h), but the difference was not statistically significant (p = 0.146). The average follow-up time for both groups exceeded 12 months (Table 1).
Surgical data
In the 3D printing group, the average time required to print the physical model was 15.9 ± 3.5 h, and the average time to produce the individualized custom-made metal plates was 32.9 ± 6.3 h. The 3D printing group had shorter average surgical time, instrument operation time, X-ray fluoroscopy times, and intraoperative blood loss compared to the traditional group (X-ray fluoroscopy times p = 0.001, all other indicators p < 0.001). Specifically, the average surgical time in the 3D printing group was (110.0 ± 12.6 min), compared to (166.0 ± 6.4 min) in the traditional group; the average instrument operation time in the 3D printing group was (34.2 ± 6.2 min), compared to (58.1 ± 8.6 min) in the traditional group; the average X-ray fluoroscopy times in the 3D printing group was (6 ± 2 times), compared to (8 ± 2 times) in the traditional group; the average intraoperative blood loss in the 3D printing group was (254.9 ± 57.2 mL), compared to (401.6 ± 46.6 mL) in the traditional group (Table 2).
Postoperative functional and radiological data
The postoperative fracture reduction quality in the 3D printing group (good rate: 15/16, 93.8%) was numerically higher than in the traditional group (good rate: 12/15, 80%), but the difference was not statistically significant (p = 0.333). The average healing time in the 3D printing group, 14.2 ± 1.1 weeks, was numerically shorter than in the traditional group, 14.8 ± 1.4 weeks, but the difference was not statistically significant (p = 0.215). The preoperative NRS score in the 3D printing group was 8.0 ± 1.1, which did not significantly differ from the preoperative NRS score in the traditional group (7.5 ± 0.8) (p = 0.153). However, the 12-month NRS score in the 3D printing group (0.8 ± 0.8) was significantly lower than that in the traditional group (1.7 ± 1.0), with a statistically significant difference (p = 0.017). The 6-month hip joint function (Harris score) in the 3D printing group (excellent/good rate: 14/16, 87.5%) was numerically higher than in the traditional group (excellent/good rate:11/15, 73.3%), but the difference was not statistically significant (p = 0.394). However, the 12-month hip joint function (Harris score) in the 3D printing group (excellent/good rate:15/16, 93.8%) was significantly better than in the traditional group (excellent/good rate:9/15, 60.0%), and the difference was statistically significant (p = 0.037) (Table 3).
Complications
The incidence of complications was similar between the two groups (p = 0.433), and no cases of bone infection or nonunion were observed in either group. In the 3D printing group (complication rate: 3/16, 18.8%), two patients experienced inflammatory reactions, and one patient developed heterotopic ossification one month after surgery. In the traditional group (complication rate: 5/15, 33.3%), two patients experienced inflammatory reactions, one patient developed heterotopic ossification two months after surgery, one patient developed traumatic arthritis, and one patient experienced iatrogenic nerve symptoms, which resolved six months after surgery (Table 3).
Discussion
Posterior column acetabular fractures are a relatively common type of acetabular fracture and are typically treated using the Kocher-Langenbeck approach. When facing acetabular fractures, fracture reduction remains the most challenging step [4, 8]. Traditional surgical methods often rely on the surgeon’s experience for fracture reduction and fixation, where conventional plates are manually contoured and shaped to fix the reduced fracture. In recent years, computer simulation surgery and 3D printing technology have been applied to many complex types of fractures, including acetabular fractures. Through 3D-printed physical fracture models, surgeons can better understand the fracture type and determine the optimal reduction sequence, ultimately achieving a strong fixation of the fracture [11, 12]. Huang et al. [13] applied 3D printing technology in the teaching of acetabular fractures, and the results indicated that 3D printed models were beneficial in promoting morphological understanding and subjective interest in acetabular fractures. This advantage arises not only from the three-dimensional display of the fracture morphology but also from the tactile feedback of the real fracture. Currently, the mainstream approach for using 3D printing technology in the treatment of acetabular fractures involves pre-bending and sha** plates based on the fracture model or virtually reduced fracture model, and then using the pre-bent plates for fixation during surgery. Ansari et al. [14] applied traditional surgical methods and 3D printing technology with pre-bent plates in 27 cases of complex acetabular fractures, and the results showed that 3D printing technology helped to better understand the anatomical structure of acetabular fractures, resulting in reduced surgical time, intraoperative blood loss, and fluoroscopy procedures. Chen et al. [17, 18, 23, 24]. However, the study by Bouabdellah et al. [8] showed no significant differences in surgical time and intraoperative blood loss between the two methods. The potential reason for this disparity may be associated with the utilization of individualized custom-made metal plates in our study. However, there has not been a comparative study employing customized plates versus pre-bent plates using 3D printing technology. This could be a direction for more comprehensive research in the future for our research group.
In our study, the process of computer-assisted virtual reduction of acetabular posterior column fractures and 3D printing of the physical models took an average of 15.9 ± 3.5 h. The design and production of individualized custom-made metal plates took an average of 32.9 ± 6.3 h. Clinically, patients with acetabular fractures are often in a state of trauma stress, and early surgery may lead to increased intraoperative blood loss and venous thrombosis due to the patient’s hypercoagulable state. Therefore, patients with acetabular and pelvic fractures are usually recommended for surgery 4 to 10 days after the injury [25, 26]. There were no significant differences in hospitalization time and time from injury to surgery between the two groups (p = 0.276 and p = 0.146, respectively), and the production of 3D printed models and individualized custom-made metal plates did not result in any significant time delays.
In this study, although the healing time of fractures in the 3D printing group was numerically lower than that in the traditional group, no statistically significant difference was observed (p = 0.215). This result may be associated with the rich blood supply in the posterior region of the acetabulum, suggesting a potentially crucial role of this blood supply in the process of fracture healing. It is noteworthy that the 3D printing group exhibited higher numerical values in postoperative fracture reduction quality and 6-month Harris scores compared to the traditional group, but these differences did not reach statistical significance (p = 0.333 and p = 0.394, respectively). The 3D printing group did not demonstrate a significant advantage over the traditional group in these two indicators. We consider that this may be attributed to the critical role played by the surgical team’s reduction techniques or the relatively small sample size in this study. However, in terms of the 12-month Harris score and the 12-month NRS score, the 3D printing group showed significantly better performance than the traditional group, with statistically significant differences (p = 0.037 and p = 0.017, respectively). This suggests that the combination of 3D printing technology with individualized custom-made metal plates can significantly improve the long-term recovery quality of hip joint function. There was no significant difference in complications between the two groups of patients (p = 0.433). It is noteworthy that the complications in the 3D group were unrelated to the 3D printing technology and individualized custom-made metal plates.
This study has some limitations. First, it is a retrospective and non-randomized study. Second, the measurement of postoperative fracture reduction quality may be more accurate on CT scans than on plain X-rays. Finally, due to the rarity of posterior column acetabular fractures, the sample size in this study is relatively small, and future studies with larger sample sizes are needed to further validate the effectiveness of 3D printing technology combined with individualized custom-made metal plates in the treatment of posterior column acetabular fractures.
Conclusion
Combining 3D printing with individualized custom-made metal plates for acetabular posterior wall and column fractures reduces surgery and instrument time, minimizes intraoperative procedures and blood loss, enhancing long-term hip joint function recovery.
Data availability
Due to ethical approval restrictions involving patient data and anonymity, the data in this study will not be publicly released but can be made available upon reasonable request from the corresponding author.
References
Cimerman M, Kristan A, Jug M, Tomazevic M. Fractures of the acetabulum: from yesterday to tomorrow. Int Orthop. 2021;45(4):1057–64.
Hsu CL, Chou YC, Li YT, Chen JE, Hung CC, Wu CC, et al. Pre-operative virtual simulation and three-dimensional printing techniques for the surgical management of acetabular fractures. Int Orthop. 2019;43(8):1969–76.
Ziran N, Soles GLS, Matta JM. Outcomes after surgical treatment of acetabular fractures: a review. Patient Saf Surg. 2019;13:16.
Chana-Rodriguez F, Mananes RP, Rojo-Manaute J, Gil P, Martinez-Gomiz JM, Vaquero-Martin J. 3D surgical printing and pre contoured plates for acetabular fractures. Injury. 2016;47(11):2507–11.
Cao J, Zhu H, Gao C. A Systematic Review and Meta-Analysis of 3D Printing Technology for the Treatment of Acetabular Fractures. Biomed Res Int. 2021; 2021:5018791.
Huang JH, Liao H, Tan XY, **ng WR, Zhou Q, Zheng YS, et al. Surgical treatment for both-column acetabular fractures using pre-operative virtual simulation and three-dimensional printing techniques. Chin Med J (Engl). 2020;133(4):395–401.
Hung CC, Li YT, Chou YC, Chen JE, Wu CC, Shen HC, et al. Conventional plate fixation method versus pre-operative virtual simulation and three-dimensional printing-assisted contoured plate fixation method in the treatment of anterior pelvic ring fracture. Int Orthop. 2019;43(2):425–31.
Bouabdellah M, Bensalah M, Kamoun C, Bellil M, Kooli M, Hadhri K. Advantages of three-dimensional printing in the management of acetabular fracture fixed by the Kocher-Langenbeck approach: randomised controlled trial. Int Orthop. 2022;46(5):1155–63.
Challa ST, Appleton P, Rodriguez EK, Wixted J. The efficacy of an anti-protrusio plate in patients with anterior column posterior hemitransverse and associated both column acetabular fractures. J Clin Orthop Trauma. 2020;11(6):1158–61.
Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51(4):737–55.
Leemhuis JF, Assink N, Reininga IHF, De Vries JPM, Ten Duis K, Meesters AML et al. Both-Column Acetabular fractures: does Surgical Approach Vary based on using virtual 3D reconstructions? Diagnostics (Basel). 2023; 13(9).
Wang P, Kandemir U, Zhang B, Fei C, Zhuang Y, Zhang K. The effect of new preoperative preparation method compared to conventional method in complex acetabular fractures: minimum 2-year follow-up. Arch Orthop Trauma Surg. 2021;141(2):215–22.
Huang Z, Song W, Zhang Y, Zhang Q, Zhou D, Zhou X, et al. Three-dimensional printing model improves morphological understanding in acetabular fracture learning: a multicenter, randomized, controlled study. PLoS ONE. 2018;13(1):e0191328.
Ansari S, Barik S, Singh SK, Sarkar B, Goyal T, Kalia RB. Role of 3D printing in the management of complex acetabular fractures: a comparative study. Eur J Trauma Emerg Surg. 2021;47(5):1291–6.
Chen K, Yang F, Yao S, **ong Z, Sun T, Zhu F, et al. Application of computer-assisted virtual surgical procedures and three-dimensional printing of patient-specific pre-contoured plates in bicolumnar acetabular fracture fixation. Orthop Traumatol Surg Res. 2019;105(5):877–84.
Wang C, Chen Y, Wang L, Wang D, Gu C, Lin X, et al. Three-dimensional printing of patient-specific plates for the treatment of acetabular fractures involving quadrilateral plate disruption. BMC Musculoskelet Disord. 2020;21(1):451.
Upex P, Jouffroy P, Riouallon G. Application of 3D printing for treating fractures of both columns of the acetabulum: benefit of pre-contouring plates on the mirrored healthy pelvis. Orthop Traumatol Surg Res. 2017;103(3):331–4.
Maini L, Sharma A, Jha S, Sharma A, Tiwari A. Three-dimensional printing and patient-specific pre-contoured plate: future of acetabulum fracture fixation? Eur J Trauma Emerg Surg. 2018;44(2):215–24.
Li YT, Hung CC, Chou YC, Chen JE, Wu CC, Shen HC et al. Surgical Treatment for Posterior Dislocation of Hip Combined with Acetabular Fractures Using Preoperative Virtual Simulation and Three-Dimensional Printing Model-Assisted Precontoured Plate Fixation Techniques. Biomed Res Int. 2019; 2019:3971571.
Merema BJ, Kraeima J, Ten Duis K, Wendt KW, Warta R, Vos E, et al. The design, production and clinical application of 3D patient-specific implants with drilling guides for acetabular surgery. Injury. 2017;48(11):2540–7.
Robinson DL, Bucknill A, Ferragina A, Campbell C, Lee PVS. Fixation of pelvic acetabular fractures using 3D-printed fracture plates: a cadaver study. J Orthop Surg Res. 2023;18(1):360.
Tomazevic M, Kristan A, Kamath AF, Cimerman M. 3D printing of implants for patient-specific acetabular fracture fixation: an experimental study. Eur J Trauma Emerg Surg. 2021;47(5):1297–305.
Lee AK, Lin TL, Hsu CJ, Fong YC, Chen HT, Tsai CH. Three-Dimensional Printing and Fracture Map** in Pelvic and Acetabular Fractures: A Systematic Review and Meta-Analysis. J Clin Med. 2022; 11(18).
Papotto G, Testa G, Mobilia G, Perez S, Dimartino S, Giardina SMC, et al. Use of 3D printing and pre-contouring plate in the surgical planning of acetabular fractures: a systematic review. Orthop Traumatol Surg Res. 2022;108(2):103111.
Katsoulis E, Giannoudis PV. Impact of timing of pelvic fixation on functional outcome. Injury. 2006;37(12):1133–42.
Sharpe JP, Magnotti LJ, Gobbell WC, Huang X, Perez EA, Fabian TC, et al. Impact of early operative pelvic fixation on long-term self-reported outcome following severe pelvic fracture. J Trauma Acute Care Surg. 2017;82(3):444–50.
Funding
This study was supported by the Innovation Fund of National Clinical Research Center for Orthopedics and Sports Medicine (Grant no. 2021-NCRC-CXJJ-PY-02), the Science and Technology Fund of the Education Department of Liaoning Province (Grant no. JYTMS20231396), the Science and Technology Plan Project of Shenyang City (Grant no. 22-321-32-13), and the Graduate Student Science and Technology Innovation Fund of Shenyang Medical College (Grant no. Y20220525).
Author information
Authors and Affiliations
Contributions
Z-CC designed the study and interpreted the data. HZ and R-DX analyzed the data. H-RL and S-YD collected the data. HZ and H-PG wrote the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures complied with the ethical standards of institutional and/or national research councils. The study received approval from the Ethics Committee of the Central Hospital affiliated with Shenyang Medical College (Approval No: 2022018). Written informed consent has been obtained from all subjects and/or their legal guardians. Furthermore, this study has been registered with the Chinese Clinical Trial Registry (ChiCTR) under the registration number ChiCTR2300070438.
Consent for publication
Informed consent for publication has been obtained from all participants.
Conficts of interest
The authors declare that they have no conficts of interest concerning this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, H., Guo, HP., Xu, RD. et al. Surgical treatment outcomes of acetabular posterior wall and posterior column fractures using 3D printing technology and individualized custom-made metal plates: a retrospective study. BMC Surg 24, 157 (2024). https://doi.org/10.1186/s12893-024-02451-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12893-024-02451-x