Abstract
Background
Shared decision making (SDM) improves the health status of patients with chronic diseases, especially in the condition of poly-medicated patients. This study aims to find the factors associated with participation of patients with chronic diseases in SDM on medication.
Methods
A total of 1,196 patients with chronic diseases were selected in Hubei Province of China using cluster sampling methods. The random forest method was applied to rank the importance of independent variables by Mean Decrease Gini and out-of- bag (OOB) curve. Multivariate logistic regression was used to explore the independent variables’ effect direction and relative hazard.
Results
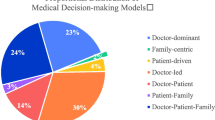
In this study, 5.18% of patients used patient-directed decision making (PDM, a decision-making model led by patients), 37.79% of patients used SDM (a collaborative decision-making model by patients and doctors), and 57.02% of patients used doctor-directed decision making (DDM, or paternalistic decision making, a decision-making model led by doctors). The random forest analysis demonstrated that the top 5 important factors were age, education, exercise, disease course, and medication knowledge. The OOB curve showed that the error rate reached minimum when top 5 variables in importance ranking composed an optimal variable combination. In multivariate logistic regression, we chose SDM as a reference group, and identified medication knowledge (OR = 2.737, 95%CI = 1.524 ~ 4.916) as the influencing factor between PDM and SDM. Meanwhile, the influencing factors between DDM and SDM were age (OR = 0.636, 95%CI = 0.439 ~ 0.921), education (OR = 1.536, 95%CI = 1.122 ~ 2.103), exercise (OR = 1.443, 95%CI = 1.109 ~ 1.877), disease course (OR = 0.750, 95%CI = 0.584 ~ 0.964), and medication knowledge (OR = 1.446, 95%CI = 1.120 ~ 1.867).
Conclusion
Most Chinese patients with chronic diseases used DDM during their medication decision-making, and some patients used PDM and SDM. The participation in SDM should be taken seriously among elderly patients with lower education levels. The SDM promotion should focus on transformation of patients’ traditional perception and enhance their medication knowledge.
Similar content being viewed by others

Background
Chronic diseases are a group of diseases with insidious onset, long duration, and persistent symptoms [3, 4], ultimately resulting in an increased incidence of adverse drug reactions (ADRs) [5].
Our previous study has discovered a negative correlation between polypharmacy behaviors and shared decision making (SDM) among chronic disease patients in community [6]. This study was conducted to further explore the factors influencing chronic disease patients’ participation in SDM on medication based on a similar cohort. SDM refers to a collaborative process in which patients and their doctors discuss the pros and cons of various medical regimens, consider patients’ values and preferences, and finally make medical decision together [7]. Furthermore, participants in SDM may also involve multiple medical staff and patients’ social networks [8]. However, some evidences have showed that most patients reported lower levels of SDM and retained doctor-led views on decision-making, especially engrained in the elderly [9, 10]. Although low levels of SDM among elderly patients with chronic diseases have garnered attention from researchers, several studies focused on implementing programs to enhance patients’ experience in the SDM process, rather than figuring out what factors stimulate patients to participate in this process [11,12,13]. Considering that patients' participation is the foundation of SDM, we believe that the first step is to identify the factors that promote patients to participate in SDM, and then take corresponding measures to improve the participation in SDM among elderly patients with chronic diseases.
China has the largest elderly population in the world, facing the critical challenge of chronic diseases [15]. Current studies indicated that the chronic disease population in China showed improvements in health knowledge, medication compliances, and health habits [3, 6]. Firstly, we categorized Hubei Province into urban and rural areas, and then randomly selected 2 cities in each of category. Wuhan and Yichang were selected as sample urban areas, while Zhijiang and Qianjiang were selected as sample rural areas. Secondly, we followed the same simple randomization process to choose 3 districts in each of the four selected cities, resulting in a total of 12 districts for our survey. In each of the selected districts, we recruited patients with hypertension or diabetes from primary health care providers. Inclusion criteria included: (1) adults aged 18 years and above. (2) ability to express themselves clearly. (3) taking medicines for a long time (more than 3 months) due to chronic diseases. A total of 1,260 invitations were sent to patients with chronic diseases through primary care in all sample districts, resulting in 1205 patients agreeing to participate, a response rate of 95.6%. All of participants completed the questionnaires, 9 of which were excluded due to incomplete information. Effective responsive rate was 99.3%. All participants in this survey were required to complete an informed consent form or provide verbal consent to participate in the survey.
Demographic data
Demographic and disease-related data, including age, gender, education, domicile, residence status, job type, medical insurance, disease course, exercise, and drink, were collected through our questionnaire. In addition, according to Age-Based Grou** Criteria of World Health Organization and the average life expectancy in China at the end of 2019 [18, 19], we categorized participants into three age groups: adults (< 65 years), young-old (65–75 years), and oldest-old (≥ 75 years). We categorized patients’ residence status as living alone or not living alone according to whether they live with family.
Measurement of variables
We used the Control Preference Scale-Post (CPSpost) [20, 21], a modified version of Control Preference Scale (CPS), to assess the type of decision-making models of patients with chronic diseases, that is, the actual control of doctors and patients over medication decisions, which was perceived by patients. Previous studies indicated that CPSpost is a valid and reliable scale to measure the participation of patients in medical decision-making [21, 22]. A total of five entries are included as follows: (1) I made my medication decision alone; (2) I made my medication decision alone considering what my doctor said; (3) I shared the medication decision with my doctor; (4) My doctor decided considering my preferences; (5) My doctor made the medication decision. (1) and (2) were categorized as PDM (a process in which the patient is the initiative role in the decision-making), (3) was categorized as SDM, (4) and (5) were categorized as DDM (a process in which the doctor is the initiative role in the decision-making) [23]. We asked patients to answer based on two experiences as follows: (1) communication with doctors when prescribed medications for the first time; (2) communication with doctors during medication adjustments over the past three months.
Medication knowledge was evaluated through a questionnaire adapted from the study by McPherson et al., a total of seven entries and codes were shown in Table 1. According to McPherson’s classification method, we used the median score as the threshold to separate medication knowledge into high and low score groups of medication knowledge [24].
Medication compliance was examined using the 4-item Morisky medication adherence scale (MMAS-4) [25], which was widely used to measure the medication compliance of patients with chronic diseases and has presented favorable among Chinese patients [26]. The detailed entries of the scale were as follows: (1) Do you ever forget to take your medicine? (2) Are you careless at times about taking your medicine? (3) When you feel better do you sometimes stop taking your medicine? (4) Sometimes if you feel worse when you take the medicine, do you stop taking it? For each item, we assigned the answer of “Yes” as 0 point, and assigned the answer of “No” as 1 point. We divided medication compliance into high and low score groups on medication compliance according to the distribution of total score.
Depression symptom was measured by Short Version of Center for Epidemiological Studies Depression Scale (CESD10), which met strict clinical requirement [27].
Statistical analysis
We used Pearson’s χ2 test to conduct descriptive analysis of demographic characteristics and other variables in different decision-making model groups.
Random forest (RF) is a machine learning method for noise immunity, prevention of overfitting, and independence from co-linearity, which showed a preference for important predictor variables by Gini coefficient, and applied to any significance tests and variable selection [28]. We used the RF method for two main reasons. Firstly, when compared with other variable selection models, RF is a machine learning method that covers the impact of each predictor variable individually as well as in multivariate interactions with other predictor variables and thus work towards the global optimality of the variable selection [29]. Secondly, RF provides relative importance among variables, which is of great value in targeting interventions. In this study, we used Mean Decrease Gini (MDG) and out-of-bag (OOB) curve to select variables, which was proposed by Hong Han et al. [29]. Gini coefficient is an indicator reflecting to the degree of inconsistency in the sample categories on the node, the lower of Gini coefficient, the better results of classification [30]. MDG refers to the total decrease of Gini from splitting on the variable averaged over all trees, which is used to indicate the importance of the predictor variable to the response variable [29]. OOB error rate is used to estimate the prediction error of current model by using the set of remaining samples which are not included in current tree [29]. We firstly referred to MDG to rank the importance of predictor variables, then selected the most appropriate number of variables to be included in the multivariate logistic regression model according to OOB curve. The multivariate logistic regression with P value, OR, and 95% CIs was used for analyzing the predictor variables’ effect direction and relative hazard.
Moreover, due to the proportion of decision-making models is unbalanced (62 PDMs, 452 SDMs and 741 DDMs). The imbalance of categories will affect the classification effect of RF —— the classification result tends to favor the majority category. Therefore, we used the synthetic minority sample oversampling method (SMOTE) to balance the data. The SMOTE method is a data preprocessing technique applied to imbalance problems proposed by Chawla et al. [31], which uses the K- nearest neighbors and linear interpolation to add minority class samples to balance the class distribution [32]. In R’s smotefamily package, we set the K parameter to 3 and dup_size to 6, which means the minority class will generate 6 times as many new samples based on 3 original samples from random nearest neighbors. Finally, we obtained 372 new PDMs, a total of 432 PDMs included in RF.
R (version 4.0.3, R Project for Statistical Computing) and SPSS (version 24.0) were used for all statistical analyses in this study.
Results
Among 1196 participants, 57.94% participants were female, 48.33% resided in the urban area, and 62.63% were manual workers. The average age of participants was 68.55 years old (ranging from 26 to 92 years). The majority of patients used DDM (57.02%), while some patients used SDM (37.79%), and a smaller percentage opted for PDM (5.18%). Other detailed information was shown in Table 2.
Importance ranking of the independent variables
Ten independent variables with a p-value less than 0.05 in univariate analysis were included in RF analysis, with ntree as 500. Figure 1 showed the visualization results of the importance ranking of 10 variables. According to the results of MDG, the top 5 important variables were age, education, exercise, disease course, and medication knowledge.
Figure 2 showed that OBB error rate was lowest when model contained 5 variables. The top 5 variables in order of importance ranking were: age, education, exercise, disease course, and medication knowledge.
According to the importance ranking and OOB curve of RF, 5 independent variables (age, education, exercise, disease course, and medication knowledge) were included in multivariate logistic regression.
Influencing factors of decision-making model
We chose the SDM group as a reference group in multivariate logistic regression analysis since SDM was considered to be a hallmark of patient-centered care and more advocated during the clinical encounter compared with other two decision-making models.
Table 3 showed the significance of factors influencing chronic patients’ participation in medication decision-making. The patients with lower medication knowledge (OR = 2.737, P < 0.05) were more likely to use PDM than SDM.
When compared with DDM, the patients under 65 years (OR = 0.636, P < 0.005) and disease course under 10 years (OR = 0.750, P < 0.005) were more likely to participate in the SDM during the medication decision-making process. By contrast, patients with infrequent exercise (OR = 1.443, P < 0.05), lower educational levels (OR=1.536, P<0.05) and poor medication knowledge (OR = 1.446, P < 0.05), were more likely to use DDM.
Discussion
In this study, 57.02% of patients used DDM during their decision-making process, which was lower than similar research conducted in other Asian countries, such as the United Arab Emirates and Japan [33, 34]. It may be related to the success of the National Essential Public Health Service launched by the Chinese government in the last decade, which enhanced the family doctor signing rate and residents’ health literacy [62], while previous studies reported that there was limited effectiveness of education in SDM process due to pressurized healthcare environment and inadequate capacities of medical staff [13, 63]. Therefore, better preparation for decision-making, such as providing patient decision aids (PDAs), was more advocated [13]. Although PDAs have attracted the attention of researchers since the 1990s [64]. Few PDAs were designed for chronic disease patients in mainland China at present, esecially for their medication decision-making [65]. Therefore, develo** PDAs for medication decision-making in the context of Chinese cultural background and healthcare system would be a meaningful research direction in the future.
Strengths and limitations
In this study, we used a combination of RF and logistic regression model to find out the key factors associated with the participation in medication decision-making of patients with chronic diseases. This was a special feature compared with other SDM related research. The data were collected from 12 districts of 4 cities in the Hubei Province, China, which are representative of all patients with chronic disease in entire Hubei Province. However, there are still several limitations in this study. Firstly, this study only focused on the impact factors of participation in decision-making from the patients’ perspective, not paying much attention to the factors from healthcare providers. Secondly, this study recruited patients voluntarily. The patients who weren’t willing to participate were not surveyed, which may generate some data bias. Finally, logistic regression did not reported significance in some PDM results, which may be attributed to the small sample size of patients using PDM (only 62 cases, 5.18% of the total sample). It is important to expand the PDM sample in future studies.
Conclusion
According to the findings in this study, the key factors associated with SDM were age, education, exercise, disease course, and medication knowledge. Based on the results, several corresponding interventions could be taken to improve patients' participation in medication decision-making. Firstly, doctors should pay more attention to elderly patients with lower education levels, and encourage them to participate in SDM. Secondly, health education should focus on transforming patients’ traditional perceptions and behaviors to enhance their awareness of participation in SDM. Finally, development and application of PDAs to improve patients' medication knowledge and promote them to participate in SDM will be an important topic in further research and clinical practice.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- SDM:
-
Shared decision making
- IHME:
-
Institute of Health Metrics and Evaluation
- PDAs:
-
Patient decision aids
- PDM:
-
Patient-directed decision making
- DDM:
-
Doctor-directed decision making
- RF:
-
Random forest
- MDG:
-
Mean Decrease Gini
- OOB:
-
Out-of-bag
References
Luo **, Chen Chaoyi, Gu Zhichun, et al. Does Having a Usual Primary Care Provider Reduce Polypharmacy Behaviors of Patients With Chronic Disease? A Retrospective Study in Hubei Province, China. Front Pharmacol 2022; 12. https://doi.org/10.3389/fphar.2021.802097
Viswanathan M, Golin CE, Jones CD, Ashok M, Blalock SJ, Wines RCM, et al. Interventions to Improve Adherence to Self-administered Medications for Chronic Diseases in the United States A Systematic Review. Ann Int Med. 2012;157(11):785. https://doi.org/10.7326/0003-4819-157-11-201212040-00538.
Hanlon JT, Pieper CF, Hajjar ER, Sloane RJ, Lindblad CI, Ruby CM, et al. Incidence and predictors of all and preventable adverse drug reactions in frail elderly persons after hospital stay. J Gerontol A Biol Sci Med Sci. 2006;61(5):511–5. https://doi.org/10.1093/gerona/61.5.511.
Zong Q., Feng Z. C., Wang J., Zheng Z. H., Chen C. Y., Feng D. Is shared decision-making a determinant of polypharmacy in older patients with chronic disease? A cross-sectional study in Hubei Province, China. BMC Geriatrics 2023; 23(1). https://doi.org/10.1186/s12877-023-03968-1
Jan B, Hans-Joerg E, Andrzej G. Ethics codes and medical decision making. Patient Educ Couns. 2021;104(6):1312–6. https://doi.org/10.1016/j.pec.2020.10.034.
Chmielowska M, Zisman-Ilani Y, Saunders R, Pilling S. Trends, challenges, and priorities for shared decision making in mental health: The first umbrella review. Int J Soc Psychiatry. 2023;69(4):823–40. https://doi.org/10.1177/00207640221140291.
Thevelin Stefanie, Petein Catherine, Metry Beatrice, Adam Luise, van Herksen Anniek, Murphy Kevin, et al. Experience of hospital-initiated medication changes in older people with multimorbidity: a multicentre mixed-methods study embedded in the OPtimising thERapy to prevent Avoidable hospital admissions in Multimorbid older people (OPERAM) trial. BMJ quality & safety 2022. https://doi.org/10.1136/bmjqs-2021-014372
Moreau A, Carol L, Dedianne MC, Dupraz C, Perdrix C, Laine X, et al. What perceptions do patients have of decision making (DM)? Toward an integrative patient-centered care model A qualitative study using focus-group interviews. Patient Educ Couns. 2012;87(2):206–11. https://doi.org/10.1016/j.pec.2011.08.010.
Tooth LR. Shared decision making and patient decision aids: An update and tips for health care providers working in midlife health and beyond. Maturitas. 2022;160:68–9. https://doi.org/10.1016/j.maturitas.2022.02.001.
Zisman-Ilani Y, Byrne L. Shared Decision Making and Peer Support: New Directions for Research and Practice. Psychiatr Serv. 2023;74(4):427–8. https://doi.org/10.1176/appi.ps.20220407.
Joseph-Williams Natalie, Edwards Adrian, Elwyn Glyn. Power imbalance prevents shared decision making. BMJ 2014; 348. https://doi.org/10.1136/bmj.g3178
Yuan Yang, Wen Li, Qinge Zhang, Ling Zhang, Teris Cheung, Yu-Tao **ang. Mental health services for older adults in China during the COVID-19 outbreak. LANCET Psychiatry. 2020;7(4):E19-E. https://doi.org/10.1016/S2215-0366(20)30079-1.
Health Ministry of. National Guideline of Basic Public Health Services (2009) Available online at: http://www.nhc.gov.cn/zwgk/wtwj/201304/b175eb09dfd240f6bae36d2fb67c8619.shtml (Accessed on 13 Dec 2022).
Li Daxu, Luo Meixuan, Liu Yu, Dong **g, Geng Wei, Li **aoliu, et al. Increased Rates of Health Management and Health Education on Hypertension and Diabetes in Inner Mongolia, China: 10-Year Population Level Trends (2009–2018). Int J Environ Res Public Health 2022; 19(20). https://doi.org/10.3390/ijerph192013048
Cheng L. W., Tan L., Zhang L., Wei S., Liu L., Long L., et al. Chronic disease mortality in rural and urban residents in Hubei Province, China, 2008–2010. BMC Public Health 2013; 13. https://doi.org/10.1186/1471-2458-13-713
Nations United. The aging of population and its economicsocial implications Available online at: https://xueshu.baidu.com/usercenter/paper/show?paperid=2866d032736055717c6ec3e5619d75fa&site=xueshu_se (Accessed on 10 Dec 2022).
Statistic China National Bureau of. China statistical Yearbook Available online at: http://www.stats.gov.cn/sj/ndsj/2020/indexch.htm (Accessed on 10 Dec 2022 ).
Brom Linda, Hopmans Wendy, Pasman H. Roeline W., Timmermans Danielle R. M., Widdershoven Guy A. M., Onwuteaka-Philipsen Bregje D. Congruence between patients' preferred and perceived participation in medical decision-making: a review of the literature. BMC Med Inform Dec Making 2014; 14. https://doi.org/10.1186/1472-6947-14-25
Rencz F, Tamasi B, Brodszky V, Gulacsi L, Weszl M, Pentek M. Validity and reliability of the 9-item Shared Decision Making Questionnaire (SDM-Q-9) in a national survey in Hungary. Eur J Health Econ. 2019;20:S43–55. https://doi.org/10.1007/s10198-019-01061-2.
Kasper Juergen, Heesen Christoph, Koepke Sascha, Fulcher Gary, Geiger Friedemann. Patients' and Observers' Perceptions of Involvement Differ. Validation Study on Inter-Relating Measures for Shared Decision Making. Plos One 2011; 6(10). https://doi.org/10.1371/journal.pone.0026255
Puschner B., Steffen S., Slade M., Kaliniecka H., Maj M., Fiorillo A., et al. Clinical Decision Making and Outcome in Routine Care for People with Severe Mental Illness (CEDAR): Study protocol. BMC PsychiatrY 2010; 10. https://doi.org/10.1186/1471-244X-10-90
McPherson Mary Lynn, Smith Sheila Weiss, Powers Atsuko, Zuckerman Ilene H. Association between diabetes patients' knowledge about medications and their blood glucose control. Res Soc Adm Pharm 2008; 4(1):37-45. https://doi.org/10.1016/j.sapharm.2007.01.002
Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67–74. https://doi.org/10.1097/00005650-198601000-00007.
Lo Suzanne H. S., Chau Janita P. C., Woo Jean, Thompson David R., Choi Kai Chow. Adherence to Antihypertensive Medication in Older Adults With Hypertension. J Cardiovasc Nurs 2016; 31(4):296-303 https://doi.org/10.1097/JCN.0000000000000251
Boey KW. Cross-validation of a short form of the CES-D in Chinese elderly. Int J Geriatr Psychiatry. 1999;14(8):608–17. https://doi.org/10.1002/(SICI)1099-1166(199908)14:8%3c608::AID-GPS991%3e3.0.CO;2-Z.
Archer KJ, Kirnes RV. Empirical characterization of random forest variable importance measures. Comput Stat Data Anal. 2008;52(4):2249–60. https://doi.org/10.1016/j.csda.2007.08.015.
Han Hong, Guo **aoling, Yu Hua, Ieee. Variable Selection Using Mean Decrease Accuracy And Mean Decrease Gini Based on Random Forest. Proceedings of 2016 IEEE 7th international conference on SOFTWARE Engineering and service science (ICSESS 2016); 20162016. p. 219–24. Available online at: https://ieeexplore.ieee.org/document/7883053
Strobl Carolin, Boulesteix Anne-Laure, Kneib Thomas, Augustin Thomas, Zeileis Achim. Conditional variable importance for random forests. BMC Bioinform 2008; 9. https://doi.org/10.1186/1471-2105-9-307
Chawla NV, Bowyer KW, Hall LO, Kegelmeyer WP. SMOTE: Synthetic minority over-sampling technique. J Artif Intell Res. 2002;16:321–57. https://doi.org/10.1613/jair.953.
Alahmari Fahad. A Comparison of Resampling Techniques for Medical Data Using Machine Learning. J Inform Knowl Manage 2020; 19(1). https://doi.org/10.1142/S021964922040016X
Alzubaidi Hamzah, Samorinha Catarina, Saidawi Ward, Hussein Amal, Saddik Basema, Scholl Isabelle. Preference for shared decision-making among Arabic-speaking people with chronic diseases: a cross-sectional study. BMJ Open 2022; 12(4). https://doi.org/10.1136/bmjopen-2021-058084
Ogawa T, Fujimoto S, Omon K, Ishigaki T, Morioka S. Shared decision-making in physiotherapy: a cross-sectional study of patient involvement factors and issues in Japan. BMC Med Inform Decis Mak. 2023;23(1). https://doi.org/10.1186/s12911-023-02208-1.
Li **nru, Li **ghua, Shao Weiya, Ma **gyu, Zhou Angdi, Song Yiwen, et al. The Relationship between Family Doctor Contract Services Policy and Perceived Participation in Primary Health Care among Chronic Disease Patients in China: The Mediating Role of the Patient Trust. Health Soc Care Commun 2023; 2023. https://doi.org/10.1155/2023/6854131
Chao W, Shijiao Y, Heng J, Zhiqiang N, Mia M, Yan He, et al. Residents’ Willingness to Maintain Contracts with Family Doctors: a Cross-sectional Study in China. J Gen Intern Med. 2021;36(3):622–31. https://doi.org/10.1007/s11606-020-06306-y.
Driever EM, Stiggelbout AM, Brand PL, P. Shared decision making: Physicians’ preferred role, usual role and their perception of its key components. Patient Educ Couns. 2020;103(1):77–82. https://doi.org/10.1016/j.pec.2019.08.004.
Driever EM, Stiggelbout AM, Brand PLP. Patients’ preferred and perceived decision-making roles, and observed patient involvement in videotaped encounters with medical specialists. Patient Educ Couns. 2022;105(8):2702–7. https://doi.org/10.1016/j.pec.2022.03.025.
De las Cuevas C, Peñate W. Validity of the Control Preferences Scale in patients with emotional disorders. Patient Prefrence Adherence. 2016;10:2351–6. https://doi.org/10.2147/PPA.S122377.
Lehmann Birthe A, de Melker Hester E, Timmermans DRM, Mollema L. Informed decision making in the context of childhood immunization. Patient Educ Couns. 2017;100(12):2339–45. https://doi.org/10.1016/j.pec.2017.06.015.
Ekdahl AW, Andersson L, Wiréhn AB, Friedrichsen M. Are elderly people with co-morbidities involved adequately in medical decision making when hospitalised? A cross-sectional survey. BMC Geriatr. 2011;11. https://doi.org/10.1186/1471-2318-11-46.
Sellars M, Tran J, Nolte L, White B, Sinclair C, Fetherstonhaugh D, et al. Public knowledge, preferences and experiences about medical substitute decision-making: a national cross-sectional survey. BMJ Support Palliat Care. 2021. https://doi.org/10.1136/bmjspcare-2020-002619.
Townsend A., Leese J., Adam P., McDonald M., Li L. C., Kerr S., et al. eHealth, Participatory Medicine, and Ethical Care: A Focus Group Study of Patients' and Health Care Providers' Use of Health-Related Internet Information. J Med Internet Res 2015; 17(6). https://doi.org/10.2196/jmir.3792
Benetoli A, Chen TF, Aslani P. How patients’ use of social media impacts their interactions with healthcare professionals. Patient Educ Couns. 2018;101(3):439–44. https://doi.org/10.1016/j.pec.2017.08.015.
Cima Robert R., Anderson Kari J., Larson David W., Dozois Eric J., Hasson Imran, Sandborn William J., et al. Internet use by patients in an inflammatory bowel disease specialty clinic Inflamm Bowel Dis 2007;13(10):1266-70 https://doi.org/10.1002/ibd.20198
Agbadje Titilayo Tatiana, Rahimi Samira Abbasgholizadeh, Cote Melissa, Tremblay Andree-Anne, Diallo Mariama Penda, Elidor Helene, et al. Evaluation of a prenatal screening decision aid: A mixed methods pilot study. Patient Educ Couns 2022; 105(2):474-85. https://doi.org/10.1016/j.pec.2021.05.025
Huei-Lan C, Fang-Shan Li, Chiou-Fen L. Factors Influencing Implementation Of Shared Medical Decision Making In Patients With Cancer. Patient Prefer Adherence. 2019;13:1995–2005. https://doi.org/10.2147/PPA.S217561.
García-Sánchez FJ, Martínez-Vizcaíno V, Rodríguez-Martín B. Patients' and Caregivers' Conceptualisations of Pressure Ulcers and the Process of Decision-Making in the Context of Home Care. Int J Environ Res Public Health. 2019;16(15). https://doi.org/10.3390/ijerph16152719.
Yilin W, Li Z, Fangfei C. An active health behavior scale for hypertensive patients: development and reliability and validity evaluation. China J Public Health 2023;39(3):370–4. https://doi.org/10.11847/zgggws1139802.
Can S, Shang-feng T, Chao-yi CH. Connotation of active health: a literature analysis. China J Public Health. 2023;39(1):68–72. https://doi.org/10.11847/zgggws1139565.
Van de Velde Dominique, De Zutter Freya, Satink Ton, Costa Ursula, Janquart Sara, Senn Daniela, et al. Delineating the concept of self-management in chronic conditions: a concept analysis. BMJ Open 2019; 9(7). https://doi.org/10.1136/bmjopen-2018-027775
Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002;288(19):2469–75. https://doi.org/10.1001/jama.288.19.2469.
Battersby Malcolm, Von Korff Michael, Schaefer Judith, Davis Connie, Ludman Evette, Greene Sarah M., et al. Twelve evidence-based principles for implementing self-management support in primary care. Joint Commission journal on quality and patient safety 2010; 36(12):561–70. https://doi.org/10.1016/S1553-7250(10)36084-3
Glyn E, Amy P, Ariel FJV, Pal G. The limits of shared decision making. BMJ Evid Based Med. 2023;28(4):218–21. https://doi.org/10.1136/bmjebm-2022-112089.
Shen Hsiu-Nien, Lin Chia-Chen, Hoffmann Tammy, Tsai Chia-Yin, Hou Wen-Hsuan, Kuo Ken N. The relationship between health literacy and perceived shared decision making in patients with breast cancer. Patient Educ Couns 2019; 102(2):360-6. https://doi.org/10.1016/j.pec.2018.09.017
Sabrina D, Morgan P, Sarah N, Laysha O. User Perspectives on Professional Support and Service Use During Psychiatric Medication Discontinuation. Community Ment Health J. 2022;58(7):1416–24. https://doi.org/10.1007/s10597-021-00933-3.
Nicola M, Kiran A, Sonia J, Joanna M. The least worst option: user experiences of antipsychotic medication and lack of involvement in medication decisions in a UK community sample. J Ment Health. 2018;27(4):322–8. https://doi.org/10.1080/09638237.2017.1370637.
Ying W, Zhang **na Hu, Bo WJ, Laixiang Z, **aohua Li, et al. Influencing factors of lung cancer patients’ participation in shared decision-making: a cross-sectional study. J Cancer Res Clin Oncol. 2022;148(12):3303–12. https://doi.org/10.1007/s00432-022-04105-y.
Al Sayah Fatima, Williams Beverly, Pederson Jenelle L., Majumdar Sumit R., Johnson Jeffrey A. Health Literacy and Nurses' Communication With Type 2 Diabetes Patients in Primary Care Settings. Nurs Res 2014; 63(6):408-17. https://doi.org/10.1097/NNR.0000000000000055
Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353(12):1209–23. https://doi.org/10.1056/NEJMoa051688.
Atinga Roger A., Yarney Lily, Gavu Narissa Minta. Factors influencing long-term medication non-adherence among diabetes and hypertensive patients in Ghana: A qualitative investigation. Plos One 2018; 13(3). https://doi.org/10.1371/journal.pone.0193995
Wijngaarde R. O., Hein I., Daams J., Goudoever J. B. Van, Ubbink D. T. Chronically ill children's participation and health outcomes in shared decision-making: a sco** review. Eur J Pediatr 2021:1-13. https://doi.org/10.1007/s00431-021-04055-6
Mortelmans L., Bosselaers S., Goossens E., Schultz H., Dilles T. Shared decision making on medication use between nurses and patients in an oncology setting: A qualitative descriptive study. Eur J Oncol 2023; 64. https://doi.org/10.1016/j.ejon.2023.102321
O'Connor AM, Tugwell P, Wells GA, Elmslie T, Jolly E, Hollingworth G, et al. A decision aid for women considering hormone therapy after menopause: decision support framework and evaluation. Patient Educ Couns. 1998;33(3):267–79. https://doi.org/10.1016/S0738-3991(98)00026-3.
Xu RHM, Guo H. Status and Challenges of Doctor-Patient Shared Decision Making in China. Natl Med J China. 2020;100(30):2346–50. https://doi.org/10.3881/i.issn.1000-503X.15133.
Acknowledgements
We would like to thank the patients who participated in this research for their co-operation in the data collection, and Prof. Shaodong Guo from Texas A&M University for English editing assistance.
Funding
This study was funded by the National Key R&D Program of China (Grant number: 2020YFC2006500), National Natural Science Youth Fund of China (Grant number: 71804052), National Natural Science Foundation of China (Grant number: 72274071), and the Health Commission of Henan Province scientific research project (Grant Number: SBGJ202103044). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
DF conceived and designed the study and reviewed the manuscript. QH completed the data analysis and drafted the initial manuscript. ZF, QZ, JW, ZZ critically reviewed and gave advice on the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki. All procedures were performed in compliance with relevant laws and adhered to the key ethical principles, including voluntary participation, informed consent, and confdentiality. Written informed consent was obtained from all patients. This study was approved by the Medical Ethics Committee of Tongji Medical College of Huazhong University of Science and Technology, and the approval number is 2020 (S223).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hu, Q., Feng, Z., Zong, Q. et al. Analysis of factors that promote the participation of patients with chronic diseases in shared decision making on medication: a cross-sectional survey in Hubei Province, China. BMC Public Health 23, 2440 (2023). https://doi.org/10.1186/s12889-023-17099-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-17099-0