Abstract
Background
Theoretical and empirical evidence indicates the critical role of the default mode network (DMN) in the pathophysiology of the bipolar disorder (BD). This study aims to identify the specific brain regions of the DMN that is impaired in patients with BD.
Methods
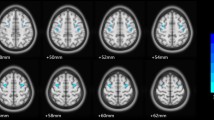
A total of 56 patients with BD and 71 healthy controls (HC) underwent resting-state functional magnetic resonance imaging. Three commonly used functional indices, i.e., fractional amplitude of low-frequency fluctuation (fALFF), regional homogeneity (ReHo), and degree centrality (DC), were utilized to identify the brain region showing abnormal spontaneous brain activity in patients with BD. Then, this region served as the seed region for resting-state functional connectivity (rsFC) analysis.
Results
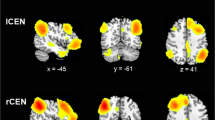
Compared to the HC group, the BD group showed reduced fALFF, ReHo, and DC values in the left precuneus. Moreover, patients exhibited decreased rsFCs within the left precuneus and between the left precuneus and the medial prefrontal cortex. Additionally, there was diminished negative connectivity between the left precuneus and the left putamen, extending to the left insula (putamen/insula). The abnormalities in DMN functional connectivity were confirmed through various analysis strategies.
Conclusions
Our findings provide convergent evidence for the abnormalities in the DMN, particularly located in the left precuneus. Decreased functional connectivity within the DMN and the reduced anticorrelation between the DMN and the salience network are found in patients with BD. These findings suggest that the DMN is a key aspect for understanding the neural basis of BD, and the altered functional patterns of DMN may be a potential candidate biomarker for diagnosis of BD.
Similar content being viewed by others
Background
Bipolar disorder (BD) is a lifelong mood disorder characterized by extreme fluctuations between mania and depression [1]. It affects more than 1% of the world’s population [2] and 0.6% of the Chinese population [3]. However, the pathophysiology of BD is poorly understood. Recent advances in the field of neuroimaging have enhanced our understanding on the neurophysiology of this disease [4]. In particular, the application of resting-state functional magnetic resonance imaging (rs-fMRI), abnormal local spontaneous brain activity, and resting-state functional connectivity (rsFC) have been repeatedly observed in patients with BD [5, 6].
These studies indicate that a brain network, called the default mode network (DMN), is particularly interested in the studies of BD. The DMN consists of the medial prefrontal cortex (MPFC), posterior cingulate cortex (PCC), precuneus [7], inferior temporal and superior frontal cortices, hippocampus, and parahippocampal cortices [8, 9]. When a person is awake, but not actively engaged in a goal-directed task, this network is active with a high degree of rsFC between regions [10]. The DMN is involved in multiple cognitive and affective functions, such as emotional processing, mind wandering, recollection of experiences, self-referential mental activity, social behavior, and episodic memory processes [7], all of which are affected to varying degrees in BD [11]. Broyd and colleagues [12] reviewed the putative mechanisms for DMN-related dysfunction in mental disorders, including BD, from two perspectives. On the one hand, altered rsFC within the DMN indicates that the integrity of DMN is impaired, which may be related to the deficit of working memory and attention, which is often observed in BD. On the other hand, in cognitive tasks that require attention, the activity of certain brain regions increases (referred to as task-positive networks), while the activity of the DMN decreases [13]. This indicates an antagonistic relationship between the two networks [14]. However, in mood disorders, this relationship may be compromised, potentially related to irregular transformation of introspective and extrospective thinking. The disbalance between the DMN and the salience network (SN) (one of the task positive networks) may be associated with emotion, cognitive, and psychomotor symptoms of BD [15].
Empirically, researches have consistently reported that different affective state in BD patients have rsFC abnormalities in the DMN [16,17,18,19,20,21]. For example, one study of drug naive or unmedicated patients with BD-II depression showed decreased rsFC of the PCC with the MPFC and precuneus [19]. Another study found that unmedicated patients with BD during depressive episode exhibited weaker rsFC in the left MPFC and right precuneus compared with healthy controls [22]. Additionally, decreased rsFC between the DMN and the SN was reported in patients with BD, although the sample included patients in different affective states (i.e., manic, depressive, mixed, and euthymic phases) [23]. In these previous studies, researchers often employed independent component analysis (ICA) to investigate the DMN [17, 20,21,22], or selected specific brain regions as seeds for the rsFC analysis of the DMN based on prior hypotheses [15, 19, 23, 24]. While these studies have yielded promising findings, no consistent evidence has emerged regarding the specific brain regions within the DMN that exhibit abnormal spontaneous activity in patients with BD.
In addition to the two methods, other analytical approaches can be applied to the studies of the DMN, such as fractional amplitude of low-frequency fluctuation (fALFF) [25], regional homogeneity (ReHo) [26], and degree centrality (DC) [27]. fALFF measures the magnitude of spontaneous fluctuations in the blood oxygen level-dependent signal (BOLD) at the voxel level, which is considered to reflect spontaneous neural activity [28]. ReHo is defined as the Kendall’s coefficient concordance (KCC) between the time series of voxels and their nearest neighbors, essentially a local FC that reflects the regulation and coordination of local neuronal activity [26]. DC assesses the summed FC of each individual voxel with all voxels in the brain [29], providing an opportunity for an unbiased general search of abnormalities in the entire connectivity matrix of the whole brain functional connectome [30]. With a whole-brain search strategy, these indices can identify abnormalities in the brain. Using these indices, researchers have already found decreased brain activity in the DMN of BD patients [31,32,33]. Therefore, the abnormal spontaneous brain activity in the DMN can be unbiasedly identified using these functional indicators. Finding the abnormal rsFC of the DMN in an unbiased approach is possible by using the regions identified by these functional indicators as the seed region in patients with BD. In a previous study, the researchers have found that the MPFC, an important node of the DMN, showed abnormal brain activity as indicated by ReHo and DC in patients with bipolar mania [34].
Our research hypothesis proposes that BD patients exhibit abnormalities in the DMN, resulting in atypical spontaneous brain activity and altered functional connectivity within distinct brain regions of the DMN. We employed a whole-brain search strategy to identify the regions with specific impairments within the DMN and to examine the rsFC of the DMN in the patients with BD. Specifically, from the point of view of local spontaneous brain activity and functional network, we used multiple brain functional indices including fALFF, ReHo, and DC to unravel abnormal brain spontaneous activities in BD. Subsequently, using the cluster that showed significant between-group differences as a seed, rsFC analyses, which reflect functional interactions of spatially distributed brain regions, were performed to further characterize the abnormal functional connectivity of the seed region in patients with BD.
Methods
Participants
A total of 150 participants were recruited from the community (85 HCs) and the Bei**g Anding Hospital (65 patients with BD); the sample is the same as in our previous publication [35]. In summary, the patients and HC were matched for age, gender, and education. Twenty-three subjects (nine patients with BD and 14 HCs) were excluded from the final analysis due to excessive head motion (details are shown in the “fMRI data preprocessing”). All patients satisfied the diagnostic criteria of the Structured Clinical Interview for DSM-IV (SCID) [36], but in this study, we did not differentiate between BD-I and BD-II. Our inclusion and exclusion criteria were described in our previous study [35]. In this experiment, the Young Mania Rating Scale (YMRS) [37] scores of all patients were less than 7, thereby indicating that all patients were not in a manic mood state. And the Hamilton Depression Rating Scale (HAMD) [38] was used to assess patients’ depressive symptoms. Patients with HAMD scores of ≤ 7 were classified as euthymic patients (EP, n = 30), while those patients with scores above this threshold were considered to be in a depressive state (DP, n = 26).
We focused on patients with BD in a depressive mood state or a euthymic mood state because BD patients spend more than 80% of their time in a non-manic mood state. The current study has been approved by the Institutional Review Board of Brain Image Center, Bei**g Normal University and Bei**g Anding Hospital, Capital Medical University. Written informed consents were obtained from all subjects prior to participation in this study.
fMRI data acquisition
All imaging data were acquired at the Brain Imaging Center of the Bei**g Normal University by using a Siemens TIM Trio 3T scanner (Siemens, Erlangen, Germany). Resting state functional images (240 volumes) were acquired initially, followed by the T1 images. During scanning, subjects were asked to try not to swallow or move their body, especially their heads. During resting state, subjects were also instructed to close their eyes, relax, and remain awake. Resting state functional images were collected using echo-planar imaging (EPI) sequence, as follows: axial scanning, repetition time (TR) = 2000 ms, echo time (TE) = 30 ms, flip angle = 90°, field of view (FOV) = 200 × 200 mm2, matrix size = 64 × 64, slices = 33, interlaced scanning, slice thickness = 3.5 mm, and gap = 0.7 mm. T1 images were collected using T1-weighted sagittal 3D magnetization-prepared rapid gradient echo (MPRAGE) sequence, as follows: TR = 2530 ms, TE = 3.39 ms, flip angle = 7°, FOV = 256 × 256 mm2, matrix size = 192 × 256, slices = 128, thickness = 1.33 mm, and voxel size = 1.33 × 1 × 1 mm3.
fMRI data preprocessing
Resting state fMRI date was preprocessed in the toolbox for the Data Processing and Analysis for (Resting State) Brain Imaging (DPABI v3.1) [39]. The preprocessing steps included removing the first five time points, slice timing, realignment, detrending, removing the head motion effect (using Friston 24-parameter model) [40], regressing out nuisance covariates (the white matter signals, the cerebral spinal fluid signals, and the global mean signals), normalizing the MNI space (using T1 images), resampling (voxel size = 2 × 2 × 2 mm3), smoothing (FWHM = 4 mm, only for the fALFF and rsFC analysis), and band-pass filtering (0.01–0.1 Hz, only for the ReHo, DC, and rsFC analysis). In addition, we used volume-based framewise displacement (FD) [41] to quantify head motion. FD reflects head motion from one volume to the next, and a volume with FD < 0.2 indicates a good time point. Mean FD is calculated by the average of the sum of the absolute values of the differentiated realignment estimates (by backwards differences) at every timepoint [42]. Subjects would be excluded if their mean FD exceeded three standard deviations beyond the mean value of the entire sample or the number of good time points was less than 120.
fMRI data analysis
First, three indices of the fALFF, the ReHo, and the DC were used to unravel abnormal brain activities in the patients with BD. Subsequently, using the overlapped cluster of the significant brain region found in the analysis as seed, rsFC analysis was performed to explore possible brain regions, which showed abnormal rsFC with the overlapped cluster in patients with BD. Finally, two additional strategies were used to reidentify the seed region and then confirmed our rsFC analysis.
fALFF, ReHo, and DC calculation
Using the preprocessed resting state fMRI data, we calculated the fALFF, ReHo, and DC values for each subject in DPABI v3.1. All values were calculated at voxel level. The fALFF value was calculated using the signal strength of the low frequency range (i.e., 0.01–0.1 Hz) to divide the detectable entire frequency range [25]. The ReHo value, also called the Kendall’s coefficient of concordance (KCC), of the time series of a given voxel with its nearest neighbors (27 voxels were considered) was calculated to generate individual ReHo maps [26]. The DC value of a certain voxel was the sum of the Pearson’s correlation coefficients of all possible pairs of voxels (correlation threshold of r0 was set at 0.2) [27, 43]. Lastly, the fALFF, ReHo, and DC maps for each subject were converted into Z-score maps, respectively. For the ReHo and DC maps, smoothing (FWHM = 4 mm) was performed.
Functional connectivity analysis
This analysis was performed in DPABI v3.1. The overlapped brain region, which showed significant group differences in fALFF, ReHo, and DC values between patients with BD and HC, was used as a seed in the following functional connectivity analysis. First, time series of each voxel was extracted within the seed. Second, the mean time series of the seed was calculated by averaging each voxel’s time series. Third, the Pearson correlation coefficients of the mean time series of the seed and all other voxels’ time series were calculated. They were used to construct each subject’s rsFC map. Finally, each subject’s rsFC map was converted into Z-score map.
Statistical analyses
For categorical variables of demographic and clinical data, we used chi-square test for group comparison. For continuous variables, we first used the Shapiro-Wilk test for normality testing. If the variable followed a normal distribution, we used a two sample T-test for group comparison. If it did not follow a normal distribution, the Man-Whitney U test was used to compared the differences between the patients with BD and the HC. The above processes are all calculated in SPSS 20.0.
For each functional index (i.e., the fALFF, the ReHo, the DC, and the rsFC), analyses of the differences between the two groups were conducted in SPM12 (Wellcome Department of Cognitive Neurology, London, UK). In these analyses, two-sample T tests were used with age, gender, education, and mean FD controlled. The significance level was set at the combination of voxel-level uncorrected P < 0.001 and cluster-level Family Wise Error (FWE)-corrected P < 0.05. And in order to further investigate the correlation between imaging indicators and clinical symptoms, we used Pearson correlation analysis to study the correlation between the fALFF, DC, and ReHo of the clusters showing significant inter group differences and the total HAMD score. The significance level was set at 0.05/3 = 0.017. These statistical analyses were limited in a pre-made gray mask. The gray matter mask was generated by averaging the gray matter masks segmented from the T1 images of each subject.
Confirmation analyses of the rsFC
To validate the findings obtained in the rsFC analysis, we used two strategies to confirm the findings. (i) We used the significant cluster obtained in the group analyses of the fALFF and the DC, but not the ReHo (due to the negative finding in a strict statistical threshold) to calculate the overlapped cluster. The overlapped cluster was then used as a seed in the rsFC analysis. (ii). We attempted to map our interested brain regions identified in the analysis of the fALFF, ReHo, and DC to the Brainnetome atlas [S6-A). Then, we used the sum of the brain region Nos. 153 and 154 as a seed in the following rsFC analysis. The rsFC map within each group is shown in Figure S6-B. The whole-brain analysis found a significantly decreased rsFC of the seed with the MPFC (Figure S6-C and Table 3).
Furthermore, in the subgroup analysis, we observed that individuals of the EP group exhibited increased rsFC (indicating decreased negative rsFC) between the precuneus and the left putamen (extended to the left insula), in comparison to HC (Figure S7, Table S1). Subsequently, upon reducing the threshold, we identified that the outcomes for both subgroups were consistent with the comparisons between individuals with BD and HC. Detailed results were presented in the supplementary materials.
Discussion
We used three main functional indices (fALFF, ReHo, and DC) to measure the spontaneous activity from the local activity, local connectivity to network-level functional connectivity. Consistent with our formulated research hypothesis, our findings corroborate the presence of diminished spontaneous activity within the left precuneus, a pivotal node within the DMN, among patients diagnosed with BD. Furthermore, using this overlapped region in the left precuneus as a seed for rsFC, we found the decreased rsFC within the DMN, indicated by the decreased rsFC with the left precuneus and decreased rsFC between the seed precuneus and the MPFC in patients with BD. In addition, we found decreased negative functional connectivity between the left precuneus and the core regions in the SN (i.e., the left putamen/insula), suggesting decreased anticorrelation between the DMN and the SN in patients with BD.
Altered spontaneous activity of the DMN
We used multiple functional indices and found that the patients with BD exhibited decreased fALFF, ReHo, and DC values in the left precuneus (a specific brain region of the DMN) compared with healthy controls. The decrease in the fALFF indicates reduced local BOLD signal fluctuations of the precuneus [25, 45]. The decrease in the ReHo indicates decreased synchronizing ability in relevant voxels within the precuneus [26], and the decrease in DC indicates reduced functional connections of the precuneus with other voxels in the brain [46]. The co-occurrence of abnormalities in fALFF and DC within the precuneus signifies disrupted spontaneous brain activity in this specific brain region. This study revealed a significant correlation (r = 0.671, P < 0.001) between fALFF and DC values in the precuneus across all samples, consistent with findings from Yan’s research that also reported a strong correlation between these two metrics [47]. Our findings are consistent with most previous studies [32], [56] or when they were asked to increase their negative emotions when facing aversive stimuli [57]. One study using a negative emotion task found reduced activation of the left precuneus during negative images condition in the euthymic BD-I patients, with respect to controls [58]. This finding suggested that decreased brain activity of the left precuneus in patients with BD may somehow interfere with their ability to process emotional contents. The results found in the current resting-state fMRI study highlighted the importance of the precuneus, especially its left part, in the pathogenesis of BD. Thus, the patients’ left precuneus was unable to maintain normal signal fluctuation, synchronizing ability, and connectivity with other brain regions.
Decreased rsFC within the DMN
The followed rsFC analysis found hypoconnectivity within the left precuneus in the patients with BD. The results were consistent with previous studies [59, 60]. Wang et al. [44] used FC strength (FCS) to measure the whole-brain FCS patterns, and found that unmedicated patients with BD-II depression showed decreased FCS in the DMN (including the left precuneus). Khadka et al. [60] using ICA found that the rsFC in the posterior DMN consisting mainly of bilateral precuneus was significantly decreased in patients with psychotic BD-I than the HC. Combining these findings with our results, we speculated that the decreased local spontaneous activity of the left precuneus may account for its decreased rsFC. In addition, the precuneus is a functional core of the DMN [61]. It not only shows the highest resting metabolic rate within the network [62], but has widespread connectivity with other brain regions [54]. It suggested that the anomaly of precuneus could have an important effect on the overall functional abnormality of the DMN [54, 61]. The patients with BD also exhibited reduced rsFC between the left precuneus and the MPFC, which is another core node of the DMN [63]. This result was repeated in our confirmation analyses. The current result was, to some extent, consistent with previous report of Wang et al. [64], although two additional studies using smaller sample size (the number of patients with BD is 15 and 30) did not find positive results [24, 65]. In Wang’s study, unmedicated patients with BD under depressive episode were included, and patients showed disrupted intramodular connectivity within the DMN. The reduced rsFC between the MPFC and the left precuneus reflected weaker synchronization of spontaneous neural activities within the DMN, which could reduce the efficiency of the information communication and integration of the network [66]. The precuneus is involved in self-centered mental imagery strategies and episodic memory retrieval [54]. The MPFC is one of the most clearly delineated regions in terms of its functional roles; it serves an important role in emotional experience, social cognition, memory, and decision making [67, 68]. Some researchers suggested that the abnormal rsFC between the anterior (e.g., the MPFC and the superior frontal gyrus) and the posterior (e.g., the PCC/precuneus) components of the DMN sever as the neural basis for the defects of attention and working memory [12]. The patients with BD have been reported to have these cognitive abnormalities [69]. One study on the relationship between the DMN and clinical symptoms of BD found that the decreased rsFC within the posterior DMN in patients with BD depression might be associated with rumination [19], which is a typical symptom for depressed patients. Simply put, rumination is the process in which a ruminant animal continuously regurgitates partially digested food from its stomach for further chewing. From a psychopathological perspective, rumination is defined as a distress response pattern characterized by passive and persistent contemplation of one’s distressing symptoms, their origins, and repercussions, without engaging in active problem-solving to address the underlying causes of the distress [70]. When we engage in rumination, the brain activity of DMN increases [71]. From this aspect, it would be reasonable to speculate that the decreased rsFC between the MPFC and the precuneus may result in the cognitive dysfunction and clinical symptoms for patients with BD. In summary, our findings with all previous studies support that the functional dysconnectivity within the DMN may play a relatively important role in the neural basis of BD.
Decreased anticorrelation between DMN and SN
Decreased negative connectivity was found between the left precuneus and the left putamen/insula, the main nodes of the SN [3, 72], in the patients with BD. This finding reflects the decreased anticorrelation between the DMN and the SN.
In healthy population, resting-state fMRI signals of the DMN are anticorrelated with that of task-positive networks, such as the SN [73,74,75]. The SN generates control signals and causally mediates the “switching” between the DMN and the central executive network [76]. This condition leads to a switch between their functions of introspective and extroversive attention orientation, and then allows individuals to stay vigilant when meeting unexpected environmental events [12]. This anticorrelation between DMN and SN has even been proven more important than the DMN’s own activity [77]. The decreased anticorrelation between these networks may result in the reduction of introspective thinking and attention deficit, which could be the potential interference source of goal-directed behavior [12]. Weaker anticorrelation between the DMN and the SN was also found in many other mental disorders [73, 78]. Our result expanded previous findings of disruption of the DMN-SN functional connectivity in mental disorders [23] by showing that the negative rsFC between the left precuneus and the left putamen/insula was decreased in patients with BD.
Moreover, it is noteworthy that findings obtained from the subgroup analysis were aligned with those obtained from the comparisons between individuals with BD and HC, especially increased rsFC between the precuneus and the left putamen (extended to the left insula). It is suggested that the increased precuneus-left putamen connection may be not unaffected by patients’ mood states, and may be a trait-like feature for BD.
Limitations
Some limitations are as follows. Firstly, although the patients were not in a manic mood state, our sample was still heterogeneous in the subtypes or the different affective status of the illness. Future work should recruit patients in the same mood state (mania, depression, or euthymia) to identify whether the significant results were state-dependent or trait-like characters of BD. Secondly, most patients had taken different types or dosages of drugs. Although no consistent effect of any particular drug was found on BOLD signals, different drugs or dosages may influence BOLD signals in different ways [79], potentially confounding our results. In future studies, unmedicated patients with BD should be recruited or the types and dosages of medication use should be strictly controlled. Thirdly, our study did not examine whether these brain changes could account for any clinical or cognitive symptoms, such as rumination, or whether these brain abnormalities changed over time. Further studies are needed to address these issues.
Conclusions
In summary, using multiple functional indices, we found decreased spontaneous brain activity in DMN, particularly in the left precuneus. We also observed decreased functional connectivity within the DMN and reduced anticorrelation between the DMN and the SN in patients with BD. These findings suggest that the DMN is a key aspect for understanding the neural basis of BD. The altered functional patterns of the DMN may be a potential candidate biomarker for the diagnosis of BD.
Data availability
Data are available from the first and the corresponding authors.
Abbreviations
- DMN:
-
the default mode network
- SN:
-
salience network
- BD:
-
bipolar disorder
- HC:
-
healthy controls
- EP:
-
euthymic patients with bipolar disorder
- DP:
-
depressed patients with bipolar disorder
- rs-fMRI:
-
resting-state functional magnetic resonance imaging
- fALFF:
-
ractional amplitude of low-frequency fluctuation
- ReHo:
-
regional homogeneity.
- DC:
-
degree centrality
- rsFC:
-
resting-state functional connectivity
- MPFC:
-
medial prefrontal cortex
- PCC:
-
posterior cingulate cortex
- YMRS:
-
Young Mania Rating Scale
- HAMD:
-
Hamilton Depression Rating Scale
- EPI:
-
echo-planar imaging
- TR:
-
repetition time
- TE:
-
echo time
- FOV:
-
field of view
- MPRAGE:
-
magnetization-prepared rapid gradient echo
- KCC:
-
Kendall’s coefficient of concordance
- FWE:
-
Family Wise Error
- FCS:
-
FC strength
References
Greenwood TA. Creativity and Bipolar Disorder: A Shared Genetic vulnerability. Annu Rev Clin Psychol. 2020;16:239–64.
Grande I, Berk M, Birmaher B, Vieta E. Bipolar disorder. Lancet (London England). 2016;387(10027):1561–72.
Huang Y, Wang Y, Wang H, Liu Z, Yu X, Yan J, Yu Y, Kou C, Xu X, Lu J, et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry. 2019;6(3):211–24.
Phillips ML, Swartz HA. A critical appraisal of neuroimaging studies of bipolar disorder: toward a new conceptualization of underlying neural circuitry and a road map for future research. Am J Psychiatry. 2014;171(8):829–43.
Townsend J, Altshuler LL. Emotion processing and regulation in bipolar disorder: a review. Bipolar Disord. 2012;14(4):326–39.
Vargas C, Lopez-Jaramillo C, Vieta E. A systematic literature review of resting state network–functional MRI in bipolar disorder. J Affect Disord. 2013;150(3):727–35.
Raichle ME. The brain’s default mode network. Annu Rev Neurosci. 2015;38:433–47.
Buckner RL, Andrews-Hanna JR, Schacter DL. The brain’s default network: anatomy, function, and relevance to disease. Ann N Y Acad Sci. 2008;1124:1–38.
Greicius MD, Krasnow B, Reiss AL, Menon V. Functional connectivity in the resting brain: a network analysis of the default mode hypothesis. Proc Natl Acad Sci USA. 2003;100(1):253–8.
Raichle ME, MacLeod AM, Snyder AZ, Powers WJ, Gusnard DA, Shulman GL. A default mode of brain function. Proc Natl Acad Sci USA. 2001;98(2):676–82.
Zovetti N, Rossetti MG, Perlini C, Maggioni E, Bontempi P, Bellani M, Brambilla P. Default mode network activity in bipolar disorder. Epidemiol Psychiatric Sci. 2020;29:e166.
Broyd SJ, Demanuele C, Debener S, Helps SK, James CJ, Sonuga-Barke EJS. Default-mode brain dysfunction in mental disorders: a systematic review. Neurosci Biobehavioral Reviews. 2009;33(3):279–96.
Fox MD, Snyder AZ, Vincent JL, Corbetta M, Van Essen DC, Raichle ME. The human brain is intrinsically organized into dynamic, anticorrelated functional networks. Proc Natl Acad Sci USA. 2005;102(27):9673–8.
Menon V. Large-scale brain networks and psychopathology: a unifying triple network model. Trends Cogn Sci. 2011;15(10):483–506.
Martino M, Magioncalda P, Huang Z, Conio B, Piaggio N, Duncan NW, Rocchi G, Escelsior A, Marozzi V, Wolff A, et al. Contrasting variability patterns in the default mode and sensorimotor networks balance in bipolar depression and mania. Proc Natl Acad Sci USA. 2016;113(17):4824–9.
Wang Y, Gao Y, Tang S, Lu L, Zhang L, Bu X, Li H, Hu X, Hu X, Jiang P, et al. Large-scale network dysfunction in the acute state compared to the remitted state of bipolar disorder: a meta-analysis of resting-state functional connectivity. EBioMedicine. 2020;54:102742.
Bellani M, Bontempi P, Zovetti N, Gloria Rossetti M, Perlini C, Dusi N, Squarcina L, Marinelli V, Zoccatelli G, Alessandrini F et al. Resting state networks activity in euthymic Bipolar disorder. Bipolar disorders 2020.
Chen G, Zhao L, Jia Y, Zhong S, Chen F, Luo X, Qiu S, Lai S, Qi Z, Huang L, et al. Abnormal cerebellum-DMN regions connectivity in unmedicated bipolar II disorder. J Affect Disord. 2019;243:441–7.
Gong J, Chen G, Jia Y, Zhong S, Zhao L, Luo X, Qiu S, Lai S, Qi Z, Huang L, et al. Disrupted functional connectivity within the default mode network and salience network in unmedicated bipolar II disorder. Prog Neuro-psychopharmacol Biol Psychiatry. 2019;88:11–8.
Liu Y, Wu X, Zhang J, Guo X, Long Z, Yao L. Altered effective connectivity model in the default mode network between bipolar and unipolar depression based on resting-state fMRI. J Affect Disord. 2015;182:8–17.
Ongür D, Lundy M, Greenhouse I, Shinn AK, Menon V, Cohen BM, Renshaw PF. Default mode network abnormalities in bipolar disorder and schizophrenia. Psychiatry Res. 2010;183(1):59–68.
Wang J, Wang Y, Huang H, Jia Y, Zheng S, Zhong S, Chen G, Huang L, Huang R. Abnormal dynamic functional network connectivity in unmedicated bipolar and major depressive disorders based on the triple-network model. Psychol Med. 2020;50(3):465–74.
Magioncalda P, Martino M, Conio B, Escelsior A, Piaggio N, Presta A, Marozzi V, Rocchi G, Anastasio L, Vassallo L, et al. Functional connectivity and neuronal variability of resting state activity in bipolar disorder–reduction and decoupling in anterior cortical midline structures. Hum Brain Mapp. 2015;36(2):666–82.
Nguyen TT, Kovacevic S, Dev SI, Lu K, Liu TT, Eyler LT. Dynamic functional connectivity in bipolar disorder is associated with executive function and processing speed: a preliminary study. Neuropsychology. 2017;31(1):73–83.
Zou QH, Zhu CZ, Yang Y, Zuo XN, Long XY, Cao QJ, Wang YF, Zang YF. An improved approach to detection of amplitude of low-frequency fluctuation (ALFF) for resting-state fMRI: fractional ALFF. J Neurosci Methods. 2008;172(1):137–41.
Zang Y, Jiang T, Lu Y, He Y, Tian L. Regional homogeneity approach to fMRI data analysis. NeuroImage. 2004;22(1):394–400.
Buckner RL, Sepulcre J, Talukdar T, Krienen FM, Liu H, Hedden T, Andrews-Hanna JR, Sperling RA, Johnson KA. Cortical hubs revealed by intrinsic functional connectivity: map**, assessment of stability, and relation to Alzheimer’s disease. J Neuroscience: Official J Soc Neurosci. 2009;29(6):1860–73.
Cattarinussi G, Grimaldi DA, Sambataro F. Spontaneous brain activity alterations in first-episode psychosis: a Meta-analysis of functional magnetic resonance Imaging studies. Schizophr Bull. 2023;49(6):1494–507.
Rong S, Zhang P, He C, Li Y, Li X, Li R, Nie K, Huang S, Wang L, Wang L, et al. Abnormal neural activity in different frequency bands in Parkinson’s Disease with mild cognitive impairment. Front Aging Neurosci. 2021;13:709998.
Cañete-Massé C, Carbó-Carreté M, Peró-Cebollero M, Cui SX, Yan CG, Guàrdia-Olmos J. Abnormal degree centrality and functional connectivity in Down syndrome: a resting-state fMRI study. Int J Clin Health Psychol. 2023;23(1):100341.
Liu CH, Ma X, Li F, Wang YJ, Tie CL, Li SF, Chen TL, Fan TT, Zhang Y, Dong J, et al. Regional homogeneity within the default mode network in bipolar depression: a resting-state functional magnetic resonance imaging study. PLoS ONE. 2012;7(11):e48181.
Qiu M, Zhang H, Mellor D, Shi J, Wu C, Huang Y, Zhang J, Shen T, Peng D. Aberrant neural activity in patients with bipolar depressive disorder distinguishing to the unipolar depressive disorder: a resting-state functional magnetic resonance imaging study. Front Psychiatry. 2018;9:238.
Yang Y, Liu S, Jiang X, Yu H, Ding S, Lu Y, Li W, Zhang H, Liu B, Cui Y, et al. Common and specific functional activity features in Schizophrenia, Major Depressive Disorder, and bipolar disorder. Front Psychiatry. 2019;10:52.
Russo D, Martino M, Magioncalda P, Inglese M, Amore M, Northoff G. Opposing changes in the Functional Architecture of large-scale networks in Bipolar Mania and Depression. Schizophr Bull 2020.
Zhang Z, Bo Q, Li F, Zhao L, Wang Y, Liu R, Chen X, Wang C, Zhou Y. Increased ALFF and functional connectivity of the right striatum in bipolar disorder patients. Prog Neuro-psychopharmacol Biol Psychiatry 2020:110140.
First MB, Spitzer RL, Gibbon M, Williams JBW, Fei LP, Liu XH, editors. Structured clinical interview for DSM-IV-TR Axis I disorders – Patient Edition (SCID- I/P): Biometrics Research. New York: State Psychiatric Institute, New York.;; 2002.
Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry: J Mental Sci. 1978;133:429–35.
Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. 1967;6(4):278–96.
Yan C-G, Wang X-D, Zuo X-N, Zang Y-FJN. DPABI: data processing & analysis for (resting-state) brain imaging. 2016, 14(3):339–351.
Friston KJ, Williams S, Howard R, Frackowiak RS, Turner R. Movement-related effects in fMRI time-series. Magn Reson Med. 1996;35(3):346–55.
Power JD, Barnes KA, Snyder AZ, Schlaggar BL, Petersen SE. Spurious but systematic correlations in functional connectivity MRI networks arise from subject motion. NeuroImage. 2012;59(3):2142–54.
Power JD, Mitra A, Laumann TO, Snyder AZ, Schlaggar BL, Petersen SE. Methods to detect, characterize, and remove motion artifact in resting state fMRI. NeuroImage. 2014;84:320–41.
Zuo XN, Ehmke R, Mennes M, Imperati D, Castellanos FX, Sporns O, Milham MP. Network centrality in the human functional connectome. Cereb Cortex. 2012;22(8):1862–75.
Fan L, Li H, Zhuo J, Zhang Y, Wang J, Chen L, Yang Z, Chu C, **e S, Laird AR, et al. The human Brainnetome Atlas: a New Brain Atlas based on Connectional Architecture. Cereb Cortex. 2016;26(8):3508–26.
Wang JJ, Chen X, Sah SK, Zeng C, Li YM, Li N, Liu MQ, Du SL. Amplitude of low-frequency fluctuation (ALFF) and fractional ALFF in migraine patients: a resting-state functional MRI study. Clin Radiol. 2016;71(6):558–64.
Wang X, Jiao D, Zhang X, Lin X. Altered degree centrality in childhood absence epilepsy: a resting-state fMRI study. J Neurol Sci. 2017;373:274–9.
Yan CG, Yang Z, Colcombe SJ, Zuo XN, Milham MP. Concordance among indices of intrinsic brain function: insights from inter-individual variation and temporal dynamics. Sci Bull (Bei**g). 2017;62(23):1572–84.
Lu D, Jiao Q, Zhong Y, Gao W, **ao Q, Liu X, Lin X, Cheng W, Luo L, Xu C, et al. Altered baseline brain activity in children with bipolar disorder during mania state: a resting-state study. Neuropsychiatr Dis Treat. 2014;10:317–23.
Jiang X, Fu S, Yin Z, Kang J, Wang X, Zhou Y, Wei S, Wu F, Kong L, Wang F, et al. Common and distinct neural activities in frontoparietal network in first-episode bipolar disorder and major depressive disorder: preliminary findings from a follow-up resting state fMRI study. J Affect Disord. 2020;260:653–9.
Liang MJ, Zhou Q, Yang KR, Yang XL, Fang J, Chen WL, Huang Z. Identify changes of brain regional homogeneity in bipolar disorder and unipolar depression using resting-state FMRI. PLoS ONE. 2013;8(12):e79999.
Deng S, Franklin CG, O’Boyle M, Zhang W, Heyl BL, Jerabek PA, Lu H, Fox PT. Hemodynamic and metabolic correspondence of resting-state voxel-based physiological metrics in healthy adults. NeuroImage. 2022;250:118923.
Aiello M, Salvatore E, Cachia A, Pappatà S, Cavaliere C, Prinster A, Nicolai E, Salvatore M, Baron JC, Quarantelli M. Relationship between simultaneously acquired resting-state regional cerebral glucose metabolism and functional MRI: a PET/MR hybrid scanner study. NeuroImage. 2015;113:111–21.
Brooks JO 3rd, Hoblyn JC, Woodard SA, Rosen AC, Ketter TA. Corticolimbic metabolic dysregulation in euthymic older adults with bipolar disorder. J Psychiatr Res. 2009;43(5):497–502.
Cavanna AE, Trimble MR. The precuneus: a review of its functional anatomy and behavioural correlates. Brain. 2006;129(Pt 3):564–83.
Wegbreit E, Cushman GK, Puzia ME, Weissman AB, Kim KL, Laird AR, Dickstein DP. Developmental meta-analyses of the functional neural correlates of bipolar disorder. JAMA Psychiatry. 2014;71(8):926–35.
Meseguer V, Romero MJ, Barrós-Loscertales A, Belloch V, Bosch-Morell F, Romero J, Avila C. Map** the apetitive and aversive systems with emotional pictures using a block-design fMRI procedure. Psicothema. 2007;19(3):483–8.
Ochsner KN, Ray RD, Cooper JC, Robertson ER, Chopra S, Gabrieli JD, Gross JJ. For better or for worse: neural systems supporting the cognitive down- and up-regulation of negative emotion. NeuroImage. 2004;23(2):483–99.
Sepede G, De Berardis D, Campanella D, Perrucci MG, Ferretti A, Salerno RM, Di Giannantonio M, Romani GL, Gambi F. Neural correlates of negative emotion processing in bipolar disorder. Prog Neuro-psychopharmacol Biol Psychiatry. 2015;60:1–10.
Wang Y, Zhong S, Jia Y, Sun Y, Wang B, Liu T, Pan J, Huang L. Disrupted resting-state functional connectivity in nonmedicated bipolar disorder. Radiology. 2016;280(2):529–36.
Khadka S, Meda SA, Stevens MC, Glahn DC, Calhoun VD, Sweeney JA, Tamminga CA, Keshavan MS, O’Neil K, Schretlen D, et al. Is aberrant functional connectivity a psychosis endophenotype? A resting state functional magnetic resonance imaging study. Biol Psychiatry. 2013;74(6):458–66.
Utevsky AV, Smith DV, Huettel SA. Precuneus is a functional core of the default-mode network. J Neuroscience: Official J Soc Neurosci. 2014;34(3):932–40.
Gusnard DA, Raichle ME, Raichle ME. Searching for a baseline: functional imaging and the resting human brain. Nat Rev Neurosci. 2001;2(10):685–94.
Syan SK, Smith M, Frey BN, Remtulla R, Kapczinski F, Hall GBC, Minuzzi L. Resting-state functional connectivity in individuals with bipolar disorder during clinical remission: a systematic review. J Psychiatry Neuroscience: JPN. 2018;43(5):298–316.
Wang Y, Wang J, Jia Y, Zhong S, Zhong M, Sun Y, Niu M, Zhao L, Zhao L, Pan J, et al. Topologically convergent and divergent functional connectivity patterns in unmedicated unipolar depression and bipolar disorder. Translational Psychiatry. 2017;7(7):e1165.
Lois G, Linke J, Wessa M. Altered functional connectivity between emotional and cognitive resting state networks in euthymic bipolar I disorder patients. PLoS ONE. 2014;9(10):e107829.
Fingelkurts AA, Fingelkurts AA, Kähkönen S. Functional connectivity in the brain–is it an elusive concept? Neurosci Biobehav Rev. 2005;28(8):827–36.
Lieberman MD, Straccia MA, Meyer ML, Du M, Tan KM. Social, self, (situational), and affective processes in medial prefrontal cortex (MPFC): causal, multivariate, and reverse inference evidence. Neurosci Biobehav Rev. 2019;99:311–28.
Euston DR, Gruber AJ, McNaughton BL. The role of medial prefrontal cortex in memory and decision making. Neuron. 2012;76(6):1057–70.
Alonso-Lana S, Moro N, McKenna PJ, Sarró S, Romaguera A, Monté GC, Maristany T, Goikolea JM, Vieta E, Salvador R, et al. Longitudinal brain functional changes between mania and euthymia in bipolar disorder. Bipolar Disord. 2019;21(5):449–57.
Nolen-Hoeksema S, Morrow J. A prospective study of depression and posttraumatic stress symptoms after a natural disaster: the 1989 Loma Prieta Earthquake. J Pers Soc Psychol. 1991;61(1):115–21.
Chen X, Chen NX, Shen YQ, Li HX, Li L, Lu B, Zhu ZC, Fan Z, Yan CG. The subsystem mechanism of default mode network underlying rumination: a reproducible neuroimaging study. NeuroImage. 2020;221:117185.
Palaniyappan L, White TP, Liddle PF. The concept of salience network dysfunction in schizophrenia: from neuroimaging observations to therapeutic opportunities. Curr Top Med Chem. 2012;12(21):2324–38.
Muthulingam JA, Hansen TM, Drewes AM, Olesen SS, Frokjaer JB. Disrupted functional connectivity of default mode and salience networks in chronic pancreatitis patients. Clin Neurophysiology: Official J Int Federation Clin Neurophysiol. 2020;131(5):1021–9.
Peng D, Liddle EB, Iwabuchi SJ, Zhang C, Wu Z, Liu J, Jiang K, Xu L, Liddle PF, Palaniyappan L, et al. Dissociated large-scale functional connectivity networks of the precuneus in medication-naive first-episode depression. Psychiatry Res. 2015;232(3):250–6.
Chai XJ, Castanon AN, Ongur D, Whitfield-Gabrieli S. Anticorrelations in resting state networks without global signal regression. NeuroImage. 2012;59(2):1420–8.
Uddin LQ. Salience processing and insular cortical function and dysfunction. Nat Rev Neurosci. 2015;16(1):55–61.
Uddin LQ, Kelly AM, Biswal BB, Castellanos FX, Milham MP. Functional connectivity of default mode network components: correlation, anticorrelation, and causality. Hum Brain Mapp. 2009;30(2):625–37.
Lopez-Larson MP, Shah LM, Weeks HR, King JB, Mallik AK, Yurgelun-Todd DA, Anderson JS. Abnormal functional connectivity between default and salience networks in Pediatric Bipolar Disorder. Biol Psychiatry Cogn Neurosci Neuroimaging. 2017;2(1):85–93.
Hafeman DM, Chang KD, Garrett AS, Sanders EM, Phillips ML. Effects of medication on neuroimaging findings in bipolar disorder: an updated review. Bipolar Disord. 2012;14(4):375–410.
Acknowledgements
None.
Funding
Supported by Bei**g Hospitals Authority Clinical medicine Development of special funding (ZLRK202335), Bei**g Municipal Natural Science Foundation (7192081) and National Natural Science Foundation of China (81901355, 82001408). No investigator benefited from participating in the study.
Author information
Authors and Affiliations
Contributions
Conceptualization, Formal analysis, Writing- original draft: LZ. Data curation, Funding acquisition, Resources, Supervision, Writing – review & editing: QB. Funding acquisition, Methodology, Software: ZZ. Investigation: FL. Conceptualization, Methodology, Supervision: YZ. Data curation, Resources, Project administration: CW.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocols were approved by the clinical research ethics committees of Bei**g Anding Hospital, Capital Medical University. And written informed consents were obtained from all subjects prior to participation in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhao, L., Bo, Q., Zhang, Z. et al. Disrupted default mode network connectivity in bipolar disorder: a resting-state fMRI study. BMC Psychiatry 24, 428 (2024). https://doi.org/10.1186/s12888-024-05869-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-024-05869-y