Abstract
Background
The occurrence of severe intraventricular hemorrhage (sIVH) was high in the very preterm infants (VPIs) in China. The management strategies significantly contributed to the occurrence of sIVH in VPIs. However, the status of the perinatal strategies associated with sIVH for VPIs was rarely described across the multiple neonatal intensive care units (NICUs) in China. We aim to investigate the characteristics of the perinatal strategies associated with sIVH for VPIs across the multiple NICUs in China.
Methods
This was a retrospective analysis of data from a prospective cohort of Chinese Neonatal Network (CHNN) dataset, enrolling infants born at 24+0—31+6 from 2019 to 2021. Eleven perinatal practices performed within the first 3 days of life were investigated including antenatal corticosteroids use, antenatal magnesium sulphate therapy, intubation at birth, placental transfusion, need for advanced resuscitation, initial inhaled gas of 100% FiO2 in delivery room, initial invasive respiratory support, surfactant and caffeine administration, early enteral feeding, and inotropes use. The performances of these practices across the multiple NICUs were investigated using the standard deviations of differences between expected probabilities and observations. The occurrence of sIVH were compared among the NICUs.
Results
A total of 24,226 infants from 55 NICUs with a mean (SD) gestational age of 29.5 (1.76) and mean (SD) birthweight of 1.31(0.32) were included. sIVH was detected in 5.1% of VPIs. The rate of the antenatal corticosteroids, MgSO4 therapy, and caffeine was 80.0%, 56.4%, and 31.5%, respectively. We observed significant relationships between sIVH and intubation at birth (AOR 1.52, 95% CI 1.13 to 1.75) and initial invasive respiratory support (AOR 2.47, 95% CI 2.15 to 2.83). The lower occurrence of sIVH (4.8%) was observed corresponding with the highest utility of standard antenatal care, the lowest utility of invasive practices, and early enteral feeding administration.
Conclusions
The current evidence-based practices were not performed in each VPI as expected among the studied Chinese NICUs. The higher utility of the invasive practices could be related to the occurrence of sIVH.
Similar content being viewed by others
Introduction
Intraventricular hemorrhage (IVH) is one of the serious threats to survival for preterm infants [1]. Severe intraventricular hemorrhage (sIVH) has historically been defined as greater than or equal to grade 3 according to the Papile criteria [2]. The incidence of sIVH was approximately 11.6% (19,781/170, 031) in very preterm infants (VPIs) globally [3]. China has the second largest number of preterm infants globally [18,19,20,21,22]. Other studies suggest that there is lower mortality of VPIs at 2 years or better neurological outcomes in the NICUs with higher proportions of free of mechanical ventilation at 24 h of life, early enteral feeding, and consistent neurodevelopmental care practices [3, 23].
In China, there is a large number of NICUs [24], therefore, the practice variations can be quite substantial across the different units [24]. As stated above [5, 14], decreasing the occurrence of sIVH in China is still a big challenge, and quality improvement projects aimed at reducing the number of sIVH in VPIs is necessary. Nonadherence to evidence based best practices may contribute to adverse outcomes in VPIs. However, little data exists to systematically describe the practice differences across Chinese NICUs. After reviewing a systematic review and meta-analysis [25], we planned to analyze common perinatal practices associated with sIVH or preterm mortality which were available in the CHNN dataset. Therefore, our main objective was to characterize the performance of the perinatal practices including antenatal corticosteroids use, antenatal magnesium sulphate (MgSO4) therapy, intubation at birth, placental transfusion, need for advanced resuscitation, initial inhaled gas of 100% FiO2 in delivery room, initial invasive respiratory support, surfactant and caffeine administration, early enteral feeding administration, and inotropes use which are associated with sIVH based on data from the Chinese Neonatal Network.
Method
Population and data source
A retrospective, hospital-based cohort of all infants born at gestational age of 24+0—31+6 were derived from the CHNN database between January, 1st, 2019, through December, 31st, 2021. This cohort included 77 participating Chinese children’s or maternal and children’s hospitals where the levels of NICUs were level III [5]. The CHNN view board approved the study and waived consent.
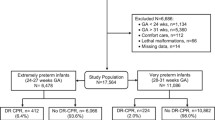
To prevent referral and recalled bias because of the uncertainty of the clinical practice in the delivery room of referring hospital, we only included infants who were inborn and admitted into NICU within 24 h of life and the data of each infant was complete. Considering the annual volume of the VPIs associated with death or sIVH [26], we only included the NICUs which had an average 50 VPI admissions per year or more in order to limit the bias of experience and ability of hospitals. Exclusion criteria were infants with major congenital anomalies, and infants without the results of head ultrasound (Fig. 1).
Data collection and datasets
The CHNN database contains a record of maternal demographics, procedures, medication administration, nutrition and respiratory support for each day of an infant’s hospitalization. The initial head ultrasound was routinely performed after day 3 of life, and sIVH is diagnosed mostly within 4–7 days of life [15, 27]. Therefore, we focused primarily on clinical practices in the first 3 DOL.
The classification of early perinatal practices and definitions
After reviewing a systematic review and meta-analysis [25], we planned to analyze common perinatal practices associated with sIVH or preterm mortality which were available in the CHNN dataset. We extracted eleven practice variables including antenatal corticosteroid use, antenatal MgSO4 therapy, intubation at birth, placenta transfusion, advanced resuscitation, initial inhaled gas of 100% FiO2 in delivery room, initial invasive respiratory support, surfactant administration, treatment with caffeine within 3 DOL, enteral feeding administration within 3 DOL, and inotropes usage. The definitions of the above early perinatal practices were described in Supplemental materials.
The perinatal clinical characteristics and definitions
Perinatal clinical characteristics included maternal age, assisted conception, maternal diabetes, maternal hypertension, clinical chorioamnionitis, preterm premature rupture of membranes (more than 24 h prior to delivery), delivery mode, prenatal antibiotics exposure, and singleton, gestational age (GA), birthweight (BW), sex, order of delivery (for multiples), and APGAR score at 5 min, abnormal temperature at admission, respiratory status, response to noxious stimuli, diagnosis of respiratory distress syndrome, pneumothorax, and early onset sepsis (EOS). The definitions of the above perinatal clinical characteristics were described in Supplemental materials.
Outcomes
sIVH was defined as greater than or equal to grade 3 according to the Papile criteria [2]. The non-sIVH group was defined as infants without IVH or grade 1 or grade 2 IVH according to the Papile criteria [2].
Standardization of early perinatal practices across the multiple neonatal intensive care units
To compare the practices across the multiple NICUs, we standardized each practice according to the perinatal clinical characteristics associated sIVH (SupFig. 1). We first calculated the expected probabilities of each practice. The expected probabilities were obtained using logistic regression models including a priori identified confounders for each practice. We reviewed the European Consensus Guidelines on the management of respiratory distress syndrome (2022 update) [28] and discussed each practice with experienced neonatologists to identify the confounders (see detail in the Supplementary materials). Among the studied practices, the antenatal corticosteroids, antenatal MgSO4 therapy, and caffeine treatment are the most evidence-based practice for VPIs currently, therefore, the expected probabilities for these three practices are 100%. In this study we did not account that the placenta transfusion was the most evidence-based practice, because the placenta transfusion was defined as receiving delayed cord clam** or cord milking. Delayed cord clam** is beneficial for VPIs [29], while the evidence of the cording milking for reducing IVH in VPIs is lacking [30]. The European guideline suggested that when delayed cord clam** is not feasible, consider umbilical cord milking in infants with GA more than 28 weeks [28]. Moreover, a noninferiority randomized controlled trial concluded that there was no difference in the rates of severe IVH between the umbilical cord milking versus delayed cord clam** in preterm infants born 28 to 32 weeks [31]. Therefore, we consider both in the practice of placenta transfusion. The expected model of inotropes given is difficult to build logistic regression models based on the limited information from the CHNN database (SupFigure 1 and SupFigure 2). Thus we could not standardize the practice of the inotropes given.
Clustering the standardized practices
Furthermore, we investigated the patterns of these standardized practices associated with sIVH. We used ten practices with the exception of inotropes given for clustering these standardized practices (SupFigure 1 and SupFigure 2). The K-means algorithm was used to cluster these standardized practices into K-distinct clusters and Silhouette analysis was used to identify the best K value.
Statistical analysis
Continuous variables were expressed as mean with SD, and categorical variables were expressed as numbers and percentages. Comparisons of clinical factors were performed by using the Welch’s t test or Wilcoxon rank sum test for continuous variables and the Chi-squared test or Fisher’s exact probability test for categorical variables. P < 0.05 was considered statistically significant. The odds ratios (ORs) and 95% confidence intervals were estimated in the multiple logistic regression. We performed all analyses using R software (version 4.0.3).
Result
Perinatal clinical factors among the enrolled very preterm infants with or without sIVH
The study cohort consisted of 24,226 VPIs from 55 participating NICUs with a mean (SD) GA of 29.5 (1.76) weeks and a mean (SD) BW of 1.31(0.32) kg. The rate of sIVH was 5.1% (1,231/24,226) (Table 1 and SupTable 1). A higher proportion of VPIs in sIVH group were male (62.6% vs 57.9%), lower BW (1.25[0.33] vs 1.31[0.32]), and lower GA (29.04[1.94] vs 29.53 [1.74]), and had APGAR score < 5 at five minutes (5.6% vs 3.3%).
Characterizing perinatal practices among the enrolled very preterm infants
Regarding the eleven practices (Fig. 2A), 80.0% (19,389/24,226) of the VPIs received antenatal corticosteroids, 56.4% (13,672/24,226) had antenatal MgSO4 therapy, 44.9% (10,868/24,226) had placental transfusion, and 31.5% (7,623/24,226) received caffeine within 3 DOL. After standardizing the performance of each practice across the multiple NICUs, the largest variation among the eleven practices was the practice of the placental transfusion (SD 0.17) (Fig. 2B).
The performances of the early care practices among the enrolled very preterm infants. A The percentage of utility of the care practices among the enrolled very preterm infants. B The standard deviation of the performance of the care practices among the enrolled very preterm infants. The higher SD meant higher variation. The expected model of inotropes given is difficult to build logistic regression models based on the limited information from the CHNN database. Therefore, we could not standardize the practice of the inotropes given
Practices associated with severe intraventricular hemorrhage in this cohort
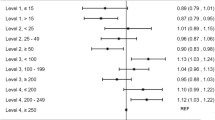
In this large cohort, we investigated the practices associated with sIVH via multiple logistic regression. Compared to the VPIs with non-sIVH, the VPIs with sIVH were more likely to be intubated at birth (AOR 1.15, 95% CI 1.01 to 1.32), receive initial invasive respiratory support (AOR 2.50, 95% CI 2.20 to 2.83), require surfactant (AOR 2.15, 95% CI 1.83 to 2.53), given caffeine (AOR 1.15, 95% CI 1.01 to 1.30) and inotropes (AOR 2.83, 95% CI 2.50 to 3.19). While, infantes with early enteral feeding (AOR 0.50, 95% CI 0.44 to 0.57) or initially inhaled gas of 100% FiO2 (AOR 0.69, 95% CI 0.58 to 0.81) less likely diagnosed with sIVH (Fig. 3).
The risk-adjusted odds ratios of the care practices for severe intraventricular hemorrhage after adjustment for the perinatal clinical characteristics. The regressions of the antenatal corticosteroids and MgSO4 therapy controlled for birthweight, gestational age, Apgar 5 score less than 5, EOS, inotropes given, invasive respiratory support; The regressions of the intubation at birth, placenta transfusion, advanced resuscitation, initially inhaled gas of 100% FiO2 controlled for birthweight, gestational age, EOS, inotropes given, Apgar 5 score less than 5, invasive respiratory support; The regressions of the invasive respiratory support controlled for birthweight, gestational age, Apgar 5 score less than 5, EOS, inotropes given; The regressions of the caffeine given controlled for birthweight, gestational age, EOS, inotropes given, Apgar 5 score less than 5, invasive respiratory support; The regression of the early enteral feeding controlled for birthweight, gestational age, EOS, inotropes given, Apgar 5 score less than 5, invasive respiratory support; The regression of the inotropes given controlled for birthweight, gestational age, EOS, Apgar 5 score less than 5, invasive respiratory support. The regression of the surfactant given controlled for birthweight, gestational age, EOS, Apgar 5 score less than 5, inotropes given, invasive respiratory support
Identifying two clusters of the practices in NICU level
According to the standardizing practices, there were the significant practice variations across the 55 NICUs (SupFigure 3). We further clustered these practices, and two clusters were identified (k = 2) (SupFigure 4), including 8,204 VPIs from 20 NICUs, and 16,022 VPIs from 35 NICUs in the cluster 1, and cluster 2, respectively (Fig. 4A, and SupTable 2).
Cluster 2 had the highest use of antenatal MgSO4 therapy (60.8%), placenta transfusion (52.0%), caffeine given within 3 DOL (32.2%), and enteral feeding within 3 DOL (89.5%); but the lowest rates of initial inhaled gas of 100% FiO2 (8.9%), advanced resuscitation (3.0%), intubation at birth (24.8%), invasive ventilation support within 3 DOL (28.2%), surfactant given (54.6%) and inotropes give (17.3%) (SupTable 2).
Regarding the variations of the practices among the two clusters (SupFigure 3), the cluster 2 showed lowest variation in the initial inhaled gas of 100% FiO2 (SD = 0.238, p < 0.05), but higher variation in the placenta transfusion (SD = 0.421, p < 0.05), and caffeine given (SD = 0.393, p < 0.05). The variations of the remaining practices were not significantly different among the two clusters.
Regarding the outcomes (Fig. 4B), the lowest rate of sIVH (4.8%) was observed in the cluster 2 (SupTable 2). Comparing to the perinatal clinical characteristics in the cluster 1, the VPIs in the cluster 2 were the higher GA but lower BW. Furthermore, we compared the sIVH of VPIs among the two clusters after stratifying two major perinatal clinical characteristics including gestational age, and early onset sepsis (SupTable 2). We observed that the rate of sIVH was still the lower (4.2%) in cluster 2 among the VPIs with GA of more than 28 weeks but higher among the VPIs with GA of less than 28 weeks (SupTable 3). While, the rate of the sIVH was consistently lower in the cluster 2 among the VPIs with EOS (SupTable 4).
Discussion
In this large VPIs cohort from the multiple NICUs, we found that 5.1% of VPIs had sIVH. The occurrence of sIVH in this cohort was not high possibly due to the higher gestational age admitted to NICUs in the CHNN database.
China has a vast territory and with great heterogeneity of population and medical care. Therefore, we standardized the studied practices to compare the performance of these practices across the multiple NICUs from China. Among these practices, we observed that the antenatal corticosteroids and MgSO4 therapy were not performed in each VPI as expected. We also observed that most NICUs started enteral feeding within 3 DOL. Regarding the other beneficial practice of caffeine administration, the percentage of this practice was not high and the variation of this practice was large. This finding indicated that the caffeine given within 3 DOL was not routine practice in VPIs of the Chinese NICUs.
The percentage of the utility of the advanced resuscitation was lowest, which could suggest the improvement of the resuscitation for VPIs. However, the percentages of the utilities of the invasive respiratory support and intubation at birth were relatively low, indicating that the invasive procedure tended to be limited in Chinese NICU currently.
Studies suggest that optimal care practices [32] or the application of neonatal care bundles [18] could significantly reduce risk of develo** sIVH and the critical care time was from the perinatal period to the first 3 DOL [27]. However, there are few studies to systemically investigate the associations between the practices and the occurrences of sIVH in detail. Different from the study [33], we did not find the practices of the antenatal corticosteroids and MgSO4 therapy were associated with the lower rate of sIVH. However, another systematic review indicated that although the antenatal MgSO4 could decreased the rate of IVH in preterm infant, this effect was not statistically significant. This could be related to the dosage, timing and gestational age [34]. In our study, our primary outcome was sIVH other than IVH. Moreover, the other invasive practices could contribute more to the occurrence of sIVH in our cohort. We addressed intubation at birth, and within 3 DOL the practices of: invasive respiratory support, caffeine administration, inotropes use, and enteral feeding. Among the studied care practices, the invasive practices (intubation at birth, invasive respiratory support, surfactant given) and inotropes use were risk factors for sIVH. This finding is consistent with other studies [35, 36]. The study suggests that the underlying pathophysiology of invasive practices may be related to the inflammatory and hemodynamic pathway [37]. Interestingly [38], caffeine given within 3 DOL was risk factor of sIVH in our study, however the OR was close to 1. Previous studies indicated that caffeine given on day 1 or day 2 was a protective factor of preterm brain injury (sIVH, cystic periventricular leukomalacia, and posthaemorrhagic ventricular dilatation) [38]. Therefore, the possible reason could be that the caffeine was given to the VPIs with apnea caused by sIVH in China. Further analysis should be conducted on the associations between the time of caffeine given and sIVH.
Consist with the study [39], we found initiation of enteral feeding within 3 DOL was a protective factor for develo** sIVH. Physiologically, studies showed that early feeding was associated with increased superior mesenteric artery blood flow, and decreased intestinal vascular resistance, which has uncertain association with the occurrence of sIVH [40, 41].
Regarding the variations of the practices among the two clusters, a lower variation meant that the observation was closer to the expected probability, which indicated that the neonatologists could perform the practices as the newborns required. However, the absolute values for the difference between expected and observed probabilities cannot give more information regarding whether these interventions were unnecessarily performed or omitted when necessary. In our results, we found that the practice of placental transfusion showed higher deviation in the cluster 2 where the incidence of sIVH was low, while the rate of performance of placental transfusion in the cluster 2 NICUs (52.0%) was higher than that in the cluster 1(30.9%). These could be explained that this high variability could potentially lead to a reduced incidence of sIVH. This might also indicate that the performance of the placental transfusion should depend on the neonates’ current conditions and physicians’ personal skills in practice.
Furthermore, we observed two clusters of the care practices amongst multiple NICUs. Among the two clusters, the practice in the cluster 2 was consistent with target practices as described in quality improvements on IVH [32]. Comparing the perinatal clinical characteristics and outcomes among these clusters, we observed that the sIVH was lower in the cluster 2, even though the cluster 2 had the more VPIs with risk profiles (such as EOS). These findings suggest closer adherence to best practices could reduce the occurrence of sIVH.
Limitations
The rate of sIVH was as high as 50% in some NICUs, therefore, some NICUs could not upload the cases completely. We extracted the practices within 3 DOL, such as caffeine use, inotropes given, and invasive ventilation. However, the sIVH could occur before these practices are performed. More evidence has showed that the prophylaxis with intravenous indomethacin in extremely low birth weight infants may reduce sIVH. However, there was only 3 infants with intravenous indomethacin in our cohort. Lastly, we did not consider the quality of interventions in each NICU because it is difficult to be estimated based on the current dataset. We also adjusted for as many confounders as possible, but we likely were not able to adjust for all.
Conclusion
The current evidence-based practices including the antenatal corticosteroids, MgSO4 therapy, and caffeine given within 3 DOL were not performed in each VPI as expected. Moreover, there were practical variations across multiple NICUs in China. In this large VPIs cohort study, invasive practice, inotropes given may increase the risk of sIVH, while, starting the enteral feeding early may reduce the risk of sIVH. These findings would help to better understand the current status of the care practices for VPIs in China, and target further quality improvement initiatives on reducing sIVH in Chinese NICUs.
Availability of data and materials
Data are available to the corresponding author upon a reasonable request.
Abbreviations
- NICUs:
-
Neonatal intensive care units
- IVH:
-
Intraventricular hemorrhage
- sIVH:
-
Severe intraventricular hemorrhage
- VPIs:
-
Very preterm infants
- CHNN:
-
Chinese Neonatal Network
- DAMA:
-
Discharge against medical advice
- DOL:
-
Days of life
- MgSO4:
-
Antenatal magnesium sulphate
- GA:
-
Gestational age
- BW:
-
Birthweight
- EOS:
-
Early onset sepsis
- ORs:
-
Odds ratios
References
Lim J, Hagen E. Reducing germinal matrix-intraventricular hemorrhage: perinatal and delivery room factors. NeoReviews. 2019;20(8):e452–63.
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92(4):529–34.
Lai GY, Shlobin N, Garcia RM, et al. Global incidence proportion of intraventricular haemorrhage of prematurity: a meta-analysis of studies published 2010–2020. Arch Dis Child Fetal Neonatal Ed. 2022;107(5):513–9.
Chen C, Zhang JW, **a HW, et al. Preterm birth in china between 2015 and 2016. Am J Public Health. 2019;109(11):1597–604.
Cao Y, Jiang S, Sun J, et al. Assessment of neonatal intensive care unit practices, morbidity, and mortality among very preterm infants in China. JAMA Netw Open. 2021;4(8):e2118904.
Sheth RD. Trends in incidence and severity of intraventricular hemorrhage. J Child Neurol. 1998;13(6):261–4.
Stoll BJ, Hansen NI, Bell EF, et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993–2012. JAMA. 2015;314(10):1039–51.
Yeo KT, Thomas R, Chow SS, et al. Improving incidence trends of severe intraventricular haemorrhages in preterm infants <32 weeks gestation: a cohort study. Arch Dis Child Fetal Neonatal Ed. 2020;105(2):145–50.
Handley SC, Passarella M, Lee HC, Lorch SA. Incidence trends and risk factor variation in severe intraventricular hemorrhage across a population based cohort. J Pediatr. 2018;200(24–29):e23.
Larroque B, Marret S, Ancel PY, et al. White matter damage and intraventricular hemorrhage in very preterm infants: the EPIPAGE study. J Pediatr. 2003;143(4):477–83.
Jeon GW, Lee JH, Oh M, Chang YS. Serial short-term outcomes of very-low-birth-weight infants in the Korean Neonatal Network From 2013 to 2020. J Korean Med Sci. 2022;37(29):e229.
Mukerji A, Shah V, Shah PS. Periventricular/intraventricular hemorrhage and neurodevelopmental outcomes: a Meta-analysis. Pediatrics. 2015;136(6):1132–43.
**u W, Bai R, Gu X, et al. Discharge against medical advice among infants with 24–31 weeks’ gestation admitted to Chinese neonatal intensive care units: a multicenter cohort study. Front Pediatr. 2022;10:943244.
Jiang S, Huang X, Zhang L, et al. Estimated survival and major comorbidities of very preterm infants discharged against medical advice vs treated with intensive care in China. JAMA Netw Open. 2021;4(6):e2113197.
Law JB, Wood TR, Gogcu S, et al. Intracranial hemorrhage and 2-year neurodevelopmental outcomes in infants born extremely preterm. J Pediatr. 2021;238(124–134):e110.
Howes A, Hilditch C, Keir A. What clinical practice strategies have been shown to decrease incidence rates of intraventricular haemorrhage in preterm infants? J Paediatr Child Health. 2019;55(10):1269–78.
Mohamed MA, Aly H. Transport of premature infants is associated with increased risk for intraventricular haemorrhage. Arch Dis Child Fetal Neonatal Ed. 2010;95(6):F403-407.
de Bijl-Marcus K, Brouwer AJ, De Vries LS, Groenendaal F, Wezel-Meijler GV. Neonatal care bundles are associated with a reduction in the incidence of intraventricular haemorrhage in preterm infants: a multicentre cohort study. Arch Dis Child Fetal Neonatal Ed. 2020;105(4):419–24.
Sauer CW, Kong JY, Vaucher YE, et al. Intubation attempts Increase the risk for severe intraventricular hemorrhage in preterm infants-a retrospective cohort study. J Pediatr. 2016;177:108–13.
Tataranno ML, Vijlbrief DC, Dudink J, Benders M. Precision medicine in neonates: a tailored approach to neonatal brain injury. Front Pediatr. 2021;9:634092.
Abdel-Latif ME, Adegboye O, Nowak G, et al. Variation in hospital morbidities in an Australian neonatal intensive care unit network. Arch Dis Child Fetal Neonatal Ed. 2023;108(4):400–7.
Travers CP, Gentle S, Freeman AE, et al. A quality improvement bundle to improve outcomes in extremely preterm infants in the first week. Pediatrics. 2022;149(2):e2020037341.
Pierrat V, Burguet A, Marchand-Martin L, et al. Variations in patterns of care across neonatal units and their associations with outcomes in very preterm infants: the French EPIPAGE-2 cohort study. BMJ Open. 2020;10(6):e035075.
Li Q, Li X, Zhang Q, et al. A cross-sectional nationwide study on accessibility and availability of neonatal care resources in hospitals of china: current situation, mortality and regional differences: neonatal care resources and newborn mortality in China. Lancet Reg Health West Pac. 2021;14:100212.
Kleinhout MY, Stevens MM, Osman KA, et al. Evidence-based interventions to reduce mortality among preterm and low-birthweight neonates in low-income and middle-income countries: a systematic review and meta-analysis. BMJ Glob Health. 2021;6(2):e003618.
Jensen EA, Lorch SA. Effects of a birth hospital’s neonatal intensive care unit level and annual volume of very low-birth-weight infant deliveries on morbidity and mortality. JAMA Pediatr. 2015;169(8):e151906.
Al-Abdi SY, Al-Aamri MA. A systematic review and meta-analysis of the timing of early intraventricular hemorrhage in preterm neonates: clinical and research implications. J Clin Neonatol. 2014;3(2):76–88.
Sweet DG, Carnielli VP, Greisen G, et al. European Consensus Guidelines on the Management of Respiratory Distress Syndrome: 2022 Update. Neonatology. 2023;120(1):3–23.
American College of O, Gynecologists’ Committee on Obstetric P. Delayed umbilical cord clam** after birth: ACOG Committee Opinion, Number 814. Obstet Gynecol. 2020;136(6):e100–6.
Katheria A, Reister F, Essers J, et al. Association of umbilical cord milking vs delayed umbilical cord clam** with death or severe intraventricular hemorrhage among preterm infants. JAMA. 2019;322(19):1877–86.
Katheria A, Szychowski J, Carlo WA, et al. Umbilical cord milking versus delayed cord clam** in infants 28 to 32 weeks: a randomized trial. Pediatrics. 2023;152(6):e2023063113.
Kramer KP, Minot K, Butler C, et al. Reduction of severe intraventricular hemorrhage in preterm infants: a quality improvement project. Pediatrics. 2022;149(3):e2021050652.
Razak A, Patel W, Durrani NUR, Pullattayil AK. Interventions to reduce severe brain injury risk in preterm neonates: a systematic review and meta-analysis. JAMA Netw Open. 2023;6(4):e237473.
Moradi Y, Khateri R, Haghighi L, et al. The effect of antenatal magnesium sulfate on intraventricular hemorrhage in premature infants: a systematic review and meta-analysis. Obstet Gynecol Sci. 2020;63(4):395–406.
Abdul Aziz AN, Thomas S, Murthy P, et al. Early inotropes use is associated with higher risk of death and/or severe brain injury in extremely premature infants. J Matern Fetal Neonatal Med. 2020;33(16):2751–8.
Vesoulis ZA, Herco M, El Ters NM, Whitehead HV, Mathur A. Cerebellar hemorrhage: a 10-year evaluation of risk factors. J Matern Fetal Neonatal Med. 2020;33(21):3680–8.
Chan KY, Tran NT, Papagianis PC, et al. Investigating pathways of ventilation induced brain injury on cerebral white matter inflammation and injury after 24 h in preterm lambs. Front Physiol. 2022;13:904144.
Szatkowski L, Fateh S, Abramson J, et al. Observational cohort study of use of caffeine in preterm infants and association between early caffeine use and neonatal outcomes. Arch Dis Child Fetal Neonatal Ed. 2023.
Huo M, Liu C, Mei H, et al. Intervention effect of oropharyngeal administration of colostrum in preterm infants: a meta-analysis. Front Pediatr. 2022;10:895375.
Fang S, Kempley ST, Gamsu HR. Prediction of early tolerance to enteral feeding in preterm infants by measurement of superior mesenteric artery blood flow velocity. Arch Dis Child Fetal Neonatal Ed. 2001;85(1):F42-45.
Elgendy MM, El Sharkawy HM, Elrazek HA, Zayton HA, Aly H. Superior mesenteric artery blood flow in parenterally fed versus enterally fed preterm infants. J Pediatr Gastroenterol Nutr. 2021;73(2):259–63.
Acknowledgements
We thank the data abstractors from the Chinese Neonatal Network. We thank all the staff at the Chinese Neonatal Network coordinating center for providing organizational support (Lin Yuan, PhD; Tongling Yang, RN; Hao Yuan, RN; Li Wang, RN; Yulan Lu, PhD).
Group Information of the Chinese Neonatal Network: Chairmen: Shoo K. Lee, MBBS, Mount Sinai Hospital, University of Toronto; Chao Chen, MD, Children’s Hospital of Fudan University. Vice-Chairmen: Lizhong Du, MD, Children's Hospital of Zhejiang University School of Medicine; Wenhao Zhou, Children’s Hospital of Fudan University.
Site principle investigators of the Chinese Neonatal Network: Children's Hospital of Fudan University: Yun Cao, MD; The Third Affiliated Hospital of Zhengzhou University: ** Han, MD; The First Bethune Hospital of Jilin University: Hui Wu, MD; The First Affiliated Hospital of Anhui Medical University: Lili Wang, MD; Women and Children's Hospital of Guangxi Zhuang Autonomous Region: Qiufen Wei, MD; The First Affiliated Hospital of ** ** Qiu, MD; Hebei Children’s Hospital: Li Ma, MD; Hainan Women and Children’s Hospital: Ling Yang, MD; The second ** Chen, MD; ** Zhu
Consortia
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethics review board of Children’s Hospital of Fudan University (2018–296) and endorsed by all participating hospitals. Due to the retrospective nature of the study, the requirement of informed consent to participate was waived by the ethics review board of Children’s Hospital of Fudan University.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
**ao, T., Hu, L., Chen, H. et al. The performance of the practices associated with the occurrence of severe intraventricular hemorrhage in the very premature infants: data analysis from the Chinese neonatal network. BMC Pediatr 24, 394 (2024). https://doi.org/10.1186/s12887-024-04664-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-024-04664-8