Abstract
Background
Non-alcoholic fatty liver disease (NAFLD) is diagnosed increasingly in children and adolescents. We aimed to investigate the prevalence and related influencing factors of NAFLD in school-aged children and adolescents in Shenyang, Liaoning Province. Furthermore, we analyzed the relationship between lifestyle and fatty liver.
Methods
We conducted aprospective cohort study of 1309 school-aged children and adolescents between the ages of 7 and 18 years who underwent physical examination from November to December 2019. In addition, they were collected age, gender, learning stage, height, weight, BMI, waist circumference, hip circumference, and waist-hip ratio. Finally, a portion of the population was selected to complete a questionnaire survey to explore the impact of lifestyle habits on fatty liver disease.
Results
NAFLD was present in 23.83% of subjects. The prevalence of children and adolescents was 22.73% and 24.43%, respectively. Fatty liver prevalence differs significantly by gender and learning stages. The highest rate of fatty liver was seen in obese children (71.68%). Moreover, exercise, diet, and parental factors can affect children with fatty liver.
Conclusions
NAFLD is very prevalent in children and adolescents in Shenyang city. Due to the close relationship between NAFLD and obesity, lifestyle plays a major role in the occurrence of NAFLD.
Trial registration
The First Affiliated Hospital of China Medical University, [2020] 2020–258-2. Registered 6 June 2020—Retrospectively registered.
Similar content being viewed by others
Background
Nonalcoholic fatty liver disease (NAFLD) is the most common chronic liver disease in children and adolescents [1]; it refers to the abnormal accumulation of fat in the liver caused by reasons other than alcohol. The main risk factors include obesity, hyperlipidemia, hypertension, and insulin resistance [2]. The common clinical manifestations include irritability, fatigue, muscle soreness, cramps and headache [3]. However, most children and adolescents with NAFLD showed no symptoms. If nonalcoholic fatty liver is not controlled, it will further develop into nonalcoholic steatohepatitis (NASH), liver fibrosis, cirrhosis, and even liver cancer [4]. Furthermore, NAFLD is related not only to intrahepatic diseases but also to many extrahepatic diseases. One report showed that NAFLD could increase the risk of type 2 diabetes and atherosclerosis in children and adolescents and, in some cases, could even change the structure of the left ventricle of the heart and systolic and diastolic function [5]. It was currently found that NAFLD might also be correlated with changes in intestinal flora, obstructive sleep, apnea, and polycystic ovary syndrome [6]. Liver biopsy is the gold standard for the diagnosis of NAFLD [7]. However, it is rarely used in clinical practice. At present, the most universal test is liver ultrasound. For treatment, weight loss is the most effective method for the treatment of nonalcoholic fatty liver disease in children and adolescents. Although drug treatment options are relatively limited, they show great promise for development. Moreover, vitamin E has now been proven to improve the histology of NASH in children and adolescents [8].
School age is a critical period of growth and development. Therefore, the physical state at this stage is particularly important and is the basis of a normal learning life [9]. However, due to the improvement of modern socioeconomic conditions and changes in dietary patterns, the prevalence of NAFLD in this part of the population is increasing [10]. This phenomenon seriously affects normal life and learning, which has become an urgent problem. There are few epidemiological studies on NAFLD in children. In a meta-analysis [11], the global prevalence of NAFLD in children is 7.6%. The prevalence of NAFLD is different in children of different genders and ages, and even the prevalence of obese children is as high as 34.2%. At the same time, the prevalence of NAFLD in children in different regions is still different. The prevalence rate in Asia is 5.9%. Among obese children, the prevalence rate of NAFLD in Asia is higher than that in Europe and North America [12]. There is no report on the NAFLD data of school-aged children and adolescents in Shenyang, Liaoning Province. Therefore, this article reports the prevalence of NAFLD for the first time. By analyzing the associated risk factors and lifestyle, we explored the factors affecting the occurrence of NAFLD. This study can provide new ideas for the diagnosis and treatment of NAFLD in school-aged children and adolescents.
Methods
Study data
This study was conducted in Shenyang, Liaoning province from November to December 2019 as a prospective cohort study. By stratified random sampling, we numbered 10 districts and 2 districts were randomly selected. Then, each district randomly selected one elementary school, one middle school, and one high school. Finally, two classes were randomly selected at each grade level of the selected school. All students aged between 7 to 18 years old and had been living in Shenyang for a period of 5 years or more. At last, 1309 students were conducted physical examination. The following students were excluded: (1) Those who were allergic to the couplant; (2) Those who did not cooperate examination; (3) Thoses who had incomplete datawere. Thus, the data analysis was only performed on the remaining 1301 students, accounting for 1.58‰ of total student population in Shenyang. The study was approved by the First Affiliated Hospital of China Medical University ([2020]258).
Anthropometric measurement
We used a homemade epidemiological questionnaire to record school attendance, grade, education, gender, and age. Height, weight, waist circumference, hip circumference were measured in the morning on an empty stomach. Body mass index (BMI) was calculated by using height and weight (BMI = weight (kg)/square of height (m2)). Waist-to-hip ratio (WHR) was calculated by using waist circumference and hip circumference (WHR = waist circumference (cm)/hip circumference (cm)).
Fatty liver examination
Fatty liver examination was performed by two well-trained doctors, using transient elastography (Fibroscan). Fibroscan is newly noninvasive device for liver examination. The detection is fast and accurate, especially in the detection of fatty liver. It can not only provide quantitative results of fat but also display information on liver stiffness. Refering to the user manual, the subjects were divided into non-NAFLD (CAP value < 238 dB /m), mild fatty liver (238 dB /m ≤ CAP value < 259 dB /m), moderate fatty liver (259 dB /m ≤ CAP value < 292 dB /m) and severe fatty liver (CAP value ≥ 292 dB /m) according to the controlled attenuation parameter (CAP) value [13].
Questionnaire
We randomly selected three classes from elementary school, middle school and high school among the enrolled students; the parients completed the questionnaire created by the First Affiliated Hospital of China Medical University on the lifestyles of children and adolescents. The questionnaire included basic information and information on the respondents’ birth, movement, entertainment, diet, learning condition, and awareness of parents. The valid questionnaires were divided into a fatty liver group and a non-fatty liver group according to the test results. The relationship between fatty liver disease and living habits was compared in children (7–12 years) and adolescents (13–18 years).
Statistics analysis
The students included in the study were grouped according to gender, learning stage, overweight, obesity and NAFLD. The data of the study were analyzed by SPSS 23 statistical software. Measurement data were expressed as the mean ± standard deviation, and the t-test was performed. The count data were expressed as percentages (%) or proportions, and Chi square test was performed. If p < 0.05, the difference was statistically significant. Univariate and Multivariate Statistical Analysis were used for the risk factors of fatty liver. In univariate analysis, factors with p < 0.05 were included in multivariate analysis. If p < 0.05 in multivariate analysis, the OR value is statistically significant. OR > 1 indicates that this factor is a risk factor for fatty liver. OR < 1 indicates that this factor is a protective factor for fatty liver.
Results
Basic information
The average of age among the participants was 13.31 ± 2.98 years old. The number of patients with fatty liver was 310, and the total prevalence was 23.83% (95% CI: 26.1% -21.5%); 22.73% (95% CI: 18.9%-26.6%) of the children and 24.43% (95% CI: 21.5%- 27.3%) of the adolescents were diagnosed with NAFLD. The age, height, weight, BMI, waist circumference, hip circumference, WHR, CAP, liver stiffness, and prevalence of mild to severe fatty liver are detailed in Table 1.
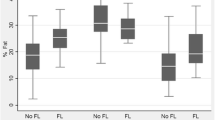
Different learning stages, gender and NAFLD
In this study, there were 395 elementary school students, 427 middle school students, and 479 high school students, among whom there were 91, 107, and 112 fatty liver patients, respectively; the prevalence rates were 23.04% (95% CI: 0.189–0.272), 25.06% (95% CI: 0.209–0.292) and 23.38% (95% CI: 0.196–0.272), respectively. The results showed that there was no significant difference in the prevalence of the three stages (p > 0.05). Most of the elementary school students with fatty liver had mild fatty liver, accounting for 15.19%. However, the proportion of junior high school students with moderate fatty liver was the highest. Nonetheless, there was no significant difference in the prevalence of moderate fatty liver among the three grades (p = 0.023). The prevalence of severe fatty liver increased significantly with higher education (p < 0.001). The univariate analysis showed that there was no difference between junior high school students and senior high school students in CAP or liver stiffness. However, both groups were significantly higher on these measures than were elementary school students (p < 0.001). In addition, the other factors increased significantly with the improvement of academic qualifications (p < 0.001) (Table 2).
The 1301 study subjects included 625 boys and 676 girls. There were 182 boys with fatty liver, and the prevalence was 29.12% (95% CI: 0.255–0.327); there were 128 girls with fatty liver, and the prevalence was 18.93% (95% CI: 0.160–0.219). The prevalence of boys was significantly higher than that of girls (p < 0.001), which was mainly reflected in the prevalence of severe fatty liver. The results of univariate analysis showed that there was no statistically significant difference in age between the two groups. However, the values of height, weight, BMI, waist circumference, hip circumference, WHR, CAP (p < 0.001), and liver stiffness (p < 0.01) indicators were significantly higher in boys (Table 2). The overall prevalence of fatty liver increases with age; for instance, the prevalence of fatty liver in students younger than 8 years old is 2.38%, and the prevalence in students older than 17 years old is 24.76%. The prevalence was also different for boys and girls of different ages. After stratification by sex and age, only the 13–14 age group showed that the prevalence among boys was significantly higher than that among girls (p < 0.001). In addition, although the prevalence among boys was higher than that among girls at other ages, there was no statistical significance. Similarly, after stratification by gender and education, the prevalence of boys in elementary school and middle schools was significantly higher than that of girls (p < 0.05). However, there was no difference between the two groups in high school (Table 3).
Analysis of risk factors for NAFLD
According to the Fibrotouch results, 1301 study subjects were divided into NAFLD group (310 cases) and non-NAFLD group (991 cases). After univariate statistical analysis, the results showed that in children, adolescents or all students, height, weight, waist and hip circumference, BMI, and WHR in NAFLD group were significantly higher than those in the non-NAFLD group (p < 0.001). The number of obesity and the proportion of boys in NAFLD group were more than those in the non-NAFLD group (p < 0.001). However, there was no statistically significant difference between the two groups in terms of age and the number of overweight. Furthermore, in the multivariable logistic regression analysis, it was also shown that boys, height, weight, BMI, waist and hip circumference, obesity are risk factors for NAFLD in children, adolescents or all students (Tables 4 and 5).
Questionnaire
The questionnaire was valid for 117 of the 123 students. Supplementary table 1 and 2 present the statistical and correlation analyses of various factors in the fatty liver group and non-fatty liver group. The basic information of children is consistent with that shown in the epidemiological survey. More fathers graduated from high school and below in the NAFLD group (p < 0.05). Regarding exercise habits, the proportion of students in the NAFLD group who did not exercise or who had poor grade was higher. In terms of eating habits, the students in the NAFLD group ate breakfast less frequently than those in the non-NAFLD group (p < 0.05). However, the frequency of fast food and snacks was higher (p < 0.05). Furthermore, the ratio of eating carefully and slowly was higher in the non-NAFLD group. Parents of adolescents who had NAFLD had higher BMI. Similar to children, more students ate breakfast every day in non-NAFLD group (p < 0.05). In particular, parents of adolescents with NAFLD received less information on nutrition and health from the community. Finally, no statistically significant differences were found between the two groups in basic conditions of birth, recreation and learning (p > 0.05).
Discussion
Many studies have investigated the prevalence of NAFLD. Jeffery conducted a retrospective survey of 742 children aged 2–19 years old from 1993 to 2003. The study found that the average prevalence of fatty liver was 9.6% [14]. A 15-year meta-analysis showed that the average prevalence of fatty liver in children and adolescents aged 1–19 years was 7.6% [7]. Different races have different prevalence rates; the prevalence among children and adolescents in Asia was 10.2% [9]; the prevalence rate in Europe was 2.5% [15]; and the prevalence rate among Hispanics was 11.8%, which is the highest prevalence rate. Ajay Jain also demonstrated this point in a recent dissertation [16], and different countries also have different prevalence rates; for example, in Haryana, India, 22.4% of children aged 5–10 years had fatty liver [17], and the average prevalence of fatty liver in Chinese children is 9.03% [18]. In our study, the prevalence among school-aged children and adolescents in Shenyang was 23.83%, which is higher than the national average. This phenomenon is likely to be related to diet and lifestyle. Many children and adolescents in this area prefer sweets and meaty diets. In addition, the weather in the area is generally cold, which causes most children and adolescents to spend more time indoors, and indoor exercise is limited.
This study found that 64.93% of overweight children and adolescents in Shenyang had fatty liver, which is significantly higher than that of non-overweight people. A study in Bei**g showed that 174 of 387 obese children and adolescents had nonalcohol fatty liver, with a prevalence of 45.0% [21]. Obese children and adolescents will have increased levels of fatty acids entering the liver, which will exceed the liver's metabolism. Thus, it can cause the deposition of a large number of fat droplets in the liver, which make liver dysfunction and promote the formation of fatty liver. In addition, free fatty acids will also increase the release of inflammatory mediators and insulin resistance [22]. These factors increase the production of intrahepatic fat [23]. Among obese people, central obesity (abdominal obesity) mainly reflects the amount of visceral fat, which is more dangerous than peripheral obesity is. In our research, non-overweight children and adolescents still had a 9% prevalence of fatty liver. Fatty liver in non-overweight people increases the risk of cardiac metabolic disease, causing more serious consequences. On the one hand, it may be related to genetic factors. Many genetic variations have been found to be associated with fatty liver. PNPLA3 gene polymorphisms can increase liver fat content, increase the risk of NAFLD and even be related to the severity of NAFLD [34]. This may be the reason why these students are prone to fatty liver. Furthermore, chewing as slowly as possible and eating carefully during meals can prevent excessive dietary intake and fat accumulation. At present, the relationship between sleep and NAFLD has not been determined. Some studies suggest that a short sleep time increases the risk of fatty liver, but our study did not find any correlation between sleep time and NAFLD. Finally, in our research, information that is publicly shared in communities and other places is obviously effective in preventing fatty liver. In that case, more parents can be aware of the harm of obesity and hope to obtain more health knowledge. So we need to strengthen the popularization of science to prevent the occurence of NAFLD in school-aged children and adolescents. As our survey results show, health promotion is very important for children and adolescents to prevent fatty liver. Therefore, schools should pay attention to regular education on fatty liver knowledge. In addition, while educating children, schools should pay attention to educating children’s parents, because the influence of family on children’s fatty liver is very important.
Conclusions
The prevalence of NAFLD among school-aged children and adolescents aged 7 to 18 in Shenyang is higher than the national average. Through questionnaires, our study confirmed that NAFLD was closely related to lifestyle habits and parental factors. A larger amount of data are needed to more thoroughly explore the prevalence of NAFLD and lifestyle in children and adolescents in Shenyang.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available because the public data has not obtained the consent of the participants’ guardian, but the data acquisition and analysis have obtained the consent of the participants’ guardian. But they are available from the corresponding author on reasonable request.
Abbreviations
- MAFLD:
-
Metabolic-associated fatty liver disease
- NAFLD:
-
Nonalcoholic fatty liver disease
- NASH:
-
Nonalcoholic steatohepatitis
- BMI:
-
Body mass index
- WHR:
-
Waist-to-hip ratio
References
Smith SK, Perito ER. Nonalcoholic Liver Disease in Children and Adolescents. Clin Liver Dis. 2018;22:723–33.
Özcan HN, Oğuz B, Haliloğlu M, Orhan D, Karçaaltıncaba M. Imaging patterns of fatty liver in pediatric patients. Digan Interv Radiol. 2015;21:355–60.
Goyal NP, Schwimmer JB. The Progression and Natural History of Pediatric Nonalcoholic Fatty Liver Disease. Clin Liver Dis. 2016;20:325–38.
Nier A, Brandt A, Conzelmann IB, Özel Y, Bergheim I. Non-Alcoholic Fatty Liver Disease in Overweight Children: Role of Fructose Intake and Dietary Pattern. Nutrients 2018;10.
Pacifico L, Chiesa C, Anania C, De Merulis A, Osborn JF, Romaggioli S, et al. Nonalcoholic fatty liver disease and the heart in children and adolescents. World J Gastroenterol. 2014;20:9055–71.
Björklund J, Laursen TL, Kazankov K, Thomsen KL, Hamilton-Dutoit S, Stenbøg E, et al. [Non-alcoholic fatty liver disease in children and adolescents]. Ugeskr Laeger 2017;179.
Anderson EL, Howe LD, Jones HE, Higgins JP, Lawlor DA, Fraser A. The Prevalence of Non-Alcoholic Fatty Liver Disease in Children and Adolescents: A Systematic Review and Meta-Analysis. PLdS One 2015;10.
Conjeevaram Selvakumar PK, Kabbany MN, Alkhouri N. Nonalcoholic Fatty Liver Disease in Children: Not a Small Matter. Paediatr Drugs. 2018;20:315–29.
Fang YL, Chen H, Wang CL, Liang L. Pathogenesis of non-alcoholic fatty liver disease in children and adolescence: From “two hit theory” to “multiple hit model.” World J Gastroenterol. 2018;24(27):2974–83.
Nobili V, Alisi A, Valenti L, Miele L, Feldstein AE, Alkhouri N. NAFLD in children: new genes, new diagnostic modalities and new drugs. Nat Rev Gastroenterol Hepatol. 2019;16(9):517–30.
Anderson EL, Howe LD, Jones HE, Higgins JP, Lawlor DA, Fraser A. The Prevalence of Non-Alcoholic Fatty Liver Disease in Children and Adolescents: A Systematic Review and Meta-Analysis. PLoS One 2015;10(10).
Li J, Ren WH. Diagnosis and therapeutic strategies for non-alcoholic fatty liver disease in children. Zhonghua Gan Zang Bing Za Zhi. 2020;28(3):208–12.
Sasso M, Beaugrand M, de Ledinghen V, Douvin C, Marcellin P, Poupon R, Sandrin L, et al. Controlled attenuation parameter (CAP): a novel VCTE guided ultrasonic attenuation measurement for the evaluation of hepatic steatosis: preliminary study and validation in a cohort of patients with chronic liver disease from various causes. Ultrasound Med Biol. 2010;36:1825–35.
Schwimmer JB, Deutsch R, Kahen T, Lavine JE, Stanley C, Behling C. Prevalence of Fatty Liver in Children and Adolescents. Pediatrics. 2006;118:1388–93.
Lawlor DA, Callaway M, Macdonald-Wallis C, Anderson E, Fraser A, Howe LD, et al. Nonalcoholic fatty liver disease, liver fibrosis, and cardiometabolic risk factors in adolescence: a cross-sectional study of 1874 general population adolescents. J Clin Endocrinol Metab. 2014;99:E410–7.
Jain A. Pediatric Fatty Liver Disease. Mo Med. 2019;116:123–8.
Das MK, Bhatia V, Sibal A, Gupta A, Gopalan S, Sardana R, et al. Prevalence of Nonalcoholic Fatty Liver Disease in Normal-weight and Overweight Preadolescent Children in Haryana. India Indian Pediatr. 2017;54:1012–6.
Song P, Yu J, Wang M, Chang X, Wang J, An L. Prevalence and Correlates of Suspected Nonalcoholic Fatty Liver Disease in Chinese Children. Int J Environ Res Public Health 2017;14.
Zhou X, Hou DQ, Duan JL, Sun Y, Cheng H, Zhao XY, et al. [Prevalence of nonalcoholic fatty liver disease and metabolic abnormalities in 387 obese children and adolescents in Bei**g, China]. Zhonghua Liu **ng Bing Xue Za Zhi 2013;34:446–50.
Shi HB, Fu JF, Liang L, Wang CL, Zhu JF, Zhou F, et al. [Prevalence of nonalcoholic fatty liver disease and metabolic syndrome in obese children]. Zhonghua Er Ke Za Zhi 2009;47:114–8.
Fabbrini E, Sullivan S, Klein S. Obesity and Nonalcoholic Fatty Liver Disease: Biochemical. Metabolic and Clinical Implications Hepatology. 2010;51:679–89.
Fang YL, Chen H, Wang CL, Liang L. Pathogenesis of non-alcoholic fatty liver disease in children and adolescence: From “two hit theory” to “multiple hit model.” World J Gastroenterol. 2018;24:2974–83.
Kitade H, Chen G, Ni Y, Ota T. Nonalcoholic Fatty Liver Disease and Insulin Resistance: New Insights and Potential New Treatments. Nutrients. 2017;9:387.
Li J, Hua W, Ji C, Rui J, Zhao Y, **e C, et al. Effect of the patatin-like phospholipase domain containing 3 gene (PNPLA3) I148M polymorphism on the risk and severity of nonalcoholic fatty liver disease and metabolic syndromes: A meta-analysis of paediatric and adolescent individuals. Pediatr Obes 2020;2.
Nobili V, Alisi A, Valenti L, Miele L, Feldstein AE, Alkhouri N. NAFLD in children: new genes, new diagnostic modalities and new drugs. Nat Rev Gastroenterol Hepatol. 2019;16:517–30.
Kumar R, Mohan S. Non-alcoholic Fatty Liver Disease in Lean Subjects: Characteristics and Implications. J Clin Transl Hepatol. 2017;5:216–23.
Zheng X, Gong L, Luo R, Chen H, Peng B, Ren W, et al. Serum uric acid and non-alcoholic fatty liver disease in non-obesity Chinese adults. Lipids Health Dis. 2017;16:202.
Ballestri S, Nascimbeni F, Baldelli E, Marrazzo A, Romagnoli D, Lonardo A. NAFLD as a Sexual Dimorphic Disease: Role of Gender and Reproductive Status in the Development and Progression of Nonalcoholic Fatty Liver Disease and Inherent Cardiovascular Risk. Adv Ther. 2017;34:1291–326.
van der Windt DJ, Sud V, Zhang H, Tsung A, Huang H. The Effects of Physical Exercise on Fatty Liver Disease. Gene Expr. 2018;18:89–101.
Mansour-Ghanaei R, Mansour-Ghanaei F, Naghipour M, Joukar F. The Lifestyle Characteristics in Non-Alcoholic Fatty Liver Disease in the PERSIAN Guilan Cohort Study. Open Access Maced J Med Sci. 2019;7:3313–8.
Hashida R, Kawaguchi T, Bekki M, Omoto M, Matsuse H, Nago T, et al. Aerobic vs. resistance exercise in non-alcoholic fatty liver disease: A systematic review. J Hepatol. 2017;66:142–52.
Jeznach-Steinhagen A, Ostrowska J, Czerwonogrodzka-Senczyna A, Boniecka I, Shahnazaryan U, Kuryłowicz A. Dietary and Pharmacological Treatment of Nonalcoholic Fatty Liver Disease. MEdicina(Kaunas) 2019;55.
Ullah R, Rauf N, Nabi G, Ullah H, Shen Y, Zhou YD, et al. Role of Nutrition in the Pathogenesis and Prevention of Non-alcoholic Fatty Liver Disease: Recent Updates. Int J Biol Sci. 2019;15:265–76.
Zalewska M, Maciokowska E. Selected nutritional habits of teenagers associated with overweight and obesity. ReerJ 2017;5.
Acknowledgements
Not applicable
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Contributions
GL and XZ carried out drafting and revising the article, HT and XJ carried out acquisition of data, DL and NW carried out designing the experiment, JS and XW carried out analysis of data, ZZ carried out interpretation of data, YL carried out final approval of the article.All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the First Affiliated Hospital of China Medical University ([2020]2020–258-2). Parents of all participants agreed to participate in this project by written consent. And written informed consent for participation in the study was obtained from their guardian (all guardian are their parents).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Table 1.
Questionnaire of children
Additional file 2:
Supplementary Table 2. Questionnaire of adolescents
Additional file 3:
Supplementary Table 3. Comparision of lifestyle between boys andgirls
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lin, G., **nhe, Z., Haoyu, T. et al. Epidemiology and lifestyle survey of non-alcoholic fatty liver disease in school-age children and adolescents in Shenyang, Liaoning. BMC Pediatr 22, 286 (2022). https://doi.org/10.1186/s12887-022-03351-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-022-03351-w