Abstract
Background
With the development of assisted reproductive technology, the twinning rate in China has been increasing. However, little is known about twinning from 2014 onwards. In addition, previous studies analysing optimal gestational times have rarely considered maternal health conditions. Therefore, whether maternal health conditions affect the optimal gestational time remains unclear.
Methods
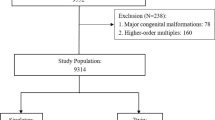
Data of women delivered between January 2012 and December 2020 were collected through China’s National Maternal Near Miss Surveillance System. Interrupted time series analysis was used to determine the rates of twinning, stillbirth, smaller than gestational age (SGA), and low Apgar scores (< 4) among twins in China. To estimate the risk of each adverse perinatal outcome for separate gestational weeks, a multivariate generalised linear model was used. Infants born at 37 weeks of gestational age or foetuses staying in utero were used as reference separately. The analyses were adjusted for the sampling distribution of the population and the cluster effect at the hospital and individual levels were considered.
Results
There were 442,268 infants enrolled in this study, and the adjusted rates for twinning, stillbirth, SGA, and low Apgar scores were 3.10%, 1.75%, 7.70%, and 0.79%, respectively. From 2012 to 2020, the twinning rate showed an increasing trend. Adverse perinatal outcomes, including stillbirth, SGA, and low Apgar scores showed a decreasing trend. A gestational age between 34 and 36 weeks decreased most for rate of stillbirth (average changing rate -9.72%, 95% confidence interval [CI] -11.41% to -8.00%); and a gestational age of between 37 and 38 weeks decreased most for rates of SGA (average changing rate -4.64%, 95% CI -5.42% to -3.85%) and low Apgar scores (average changing rate -17.61%, 95% CI -21.73% to -13.26%). No significant difference in changes in twinning rate or changes of each perinatal outcome was observed during periods of different fertility policies. Infants born at 37 weeks of gestation had a decreased risk of stillbirth, SGA, and low Apgar scores. Maternal antepartum or medical complications increased the risk of SGA and low Apgar scores in different gestational weeks.
Conclusion
China’s twinning rate showed an increasing trend, while adverse perinatal outcomes decreased from 2012 to 2020. Fertility policy changes have had little effect on the twinning rate or the rate of adverse perinatal outcomes such as stillbirth, SGA, or low Apgar scores. The optimal gestational age for twins was 37 weeks. Women pregnant with twins and with antepartum or medical complications should be cautious due to an increased risk of SGA and low Apgar scores.
Similar content being viewed by others
Introduction
Since the 1970s, twin births have increased rapidly in developed countries [1]. However, due to an insufficient registration system, the condition of twins is rarely reported in less developed countries. ** countries, has remained constant during 1993–2005 [2]. Deng et al. reported an increasing trend in the Chinese twinning rate from 2007 to 2014 [3]. However, little is known about the trend in twins after 2014. Research has shown that changes in the Fertility policy in 2016, namely, the introduction of the “universal two child policy”, have had an effect on the number of new-born infants. There were 5.4 million new-borns promoted by the new policy, but this change seemed to have little effect on the outcomes of perinatal health [4]. Whether the policy change has had an effect on twin births remains unknown.
Evidence has shown that the relative risk of adverse outcomes may depend on gestational age [5, 6]. Women with a twin pregnancy are more likely to undergo preterm birth, and approximately only half of women will give birth after 37 weeks of gestation [7]. Thus, the optimal gestational age for twin pregnancies may differ from that of singletons. The United Kingdom (UK) clinical guidelines support a policy of elective delivery from 37 weeks 0 days in dichorionic pregnancies (two placentae and two separate chorions) and 36 weeks 0 days in monochorionic pregnancies (one placenta and either one or two chorions) in order to reduce adverse short-term outcomes in twins, such as perinatal mortality [8]. Previous multiple population-based studies have indicated that births delivered between 37 and 39 weeks had the lowest risk of perinatal mortality and morbidity [9, 10]. However, these studies rarely took maternal and perinatal complications into consideration and concluded the “optimal gestational delivery week” specifically on “women with an uncomplicated twin pregnancy” [11, 12]. Whether maternal complications can have an effect on the recommended optimal gestational week is largely unknown. On the other hand, a significant number of twin-analysis research has suffered from small sample sizes and low twinning birth rates, making it difficult to accumulate a large set of twin data. This study, based on China’s National Maternal Near Miss Surveillance System (NMNMSS), collected data from 2012 to 2020, covering 30 provinces of mainland China. The system has helped in policy development and disease burden assessments in both China and worldwide [13,14,35] and higher than in developed countries such as the US (15.8‰, 2005–2006) [36] and the UK (6.16‰ in 2016) [37]. From 2012 to 2020, the stillbirth, SGA, and low Apgar score rates showed decreasing trends. However, the fertility policy has been observed to have little effect on the adverse perinatal outcomes of twins. These parameters may have benefited from China’s social and economic development, and government strategies for strengthening pregnancy health management and improving maternal and neonatal outcomes, such as maternal and foetal physical examinations and health evaluations; referral of women having a high risk pregnancy, equal access to basic public health services, the establishment of near miss new-born care centres, and guidance for the clinical management of twin pregnancies [38, 39]. China’s government made significant efforts to improve maternal and perinatal outcomes by promoting perinatal examinations. The National Basic Public Health Service Project has offered rural pregnant women five times of the perinatal examination appointments for free [40]. Our results showed that 84.17% of the twin infants underwent at least five times prenatal examinations during pregnancies. Infants born with inadequate prenatal examinations (i.e., less than five) had higher risk of stillbirth, SGA, and low Apgar scores. Besides, the National Health Commission of China has promoted health education by popularizing basic health knowledge applicable to women pre-marriage, pre-pregnancy and during pregnancy using several mediums, thereby increasing the knowledge and awareness of health care for women and families. The National Health Commission of China has also organized the “Neonatal Asphyxia Resuscitation Training Program” to reduce the mortality and disability rates of neonatal asphyxia since 2004. The training was first conducted in the “Reducing Maternal Mortality and Eliminating Neonatal Tetanus” program province, and was subsequently expanded to other provinces by offering provincial teacher training, teaching materials, and technical support [41]. Now, the “Neonatal Asphyxia Resuscitation Techniques” have been adopted as a basic skill test for midwives and doctors. Additionally, standardized training of obstetricians during their first three years of practice in China has enhanced the standardization of obstetric practices and the improvement of overall obstetrics technology and service quality.
While the stillbirth, SGA, and low Apgar score rates were on a decreasing trend over the years, the annual decreasing rate for various gestational ages was different, decreasing the most between 37 and 38 weeks. A previous multiple-population based study indicated that births delivered between 37 and 39 weeks had the lowest risk of perinatal mortality and morbidity [9]. However, the “optimal gestational age” rarely considered maternal and perinatal complications [11, 12]. In this study, we classified enrolled women as having uncomplicated pregnancies (including those with maternal health conditions), pregnancies with medical diseases, and pregnancies with antepartum complications. To select the optimum gestational age with the lowest risk of stillbirth, SGA, and a low Apgar score, we used two methods to estimate the risk of each adverse outcome. One was comparing foetuses delivered at different gestational weeks with foetuses delivered at 37 gestational weeks (the conventional method); the other was comparing foetuses delivered at any gestational week with ongoing pregnancies. The latter method was used as a measurement of short-term risk [42]. Using this method of risk estimation, infants born at any time between 37 and 39 gestational weeks were associated with a decreased risk of stillbirth. And in the conventional method, infants born at 37 weeks of gestational age were associated with the lowest risk of stillbirth. Our results for stillbirth were generally consistent with those of previous studies [8, 42]. Our results showed that infants born at around 37 weeks of gestation had the lowest risk of stillbirth, while infants born at shorter or longer gestational ages, especially those born at extremely short gestational ages had higher risks of stillbirth. This is possibly due to twin pregnancies being associated with increased risks of stillbirth and preterm labour. Monochorionic pregnancies negatively affect the in-utero survival of twins, even in monochorionic-diamniotic twins without abnormalities [43]. Monochorionic twins also experience complications like twin to twin transfusion syndrome and selective intrauterine growth retardation. These complications increase the risk of stillbirths. Premature infants have higher risk of stillbirth [44]. Twin pregnancies have higher risk of preterm labour than singleton pregnancies, to the extent that over half of the women pregnant with twins give birth before 37 weeks of gestation [7]. Furthermore, twin pregnancies are generally more likely when using ART [45]. The women who underwent ART were either of advanced age or had declining fertility. It is well-established that advanced age is an independent risk factor for adverse maternal and perinatal outcomes [31]. Women of advanced ages had higher risk of stillbirth. In our results, women with antepartum complications had increased risks of stillbirth when the gestational age was less than 33 weeks. We assumed that these could possibly be a form of natural selection of the implanted embryos to alleviate the additional burden of not successfully sustaining twin pregnancies in women with antepartum complications, leading to stillbirths at an early gestational age. Research has showed that ART-conceived pregnancies were associated with higher risk of birth defects and stillbirths [45, 46]. One study found that in comparison with the gestational ages of stillborn infants of women who conceived spontaneously, the mean gestational age at stillbirth was lower for infants conceived through fertility treatments, suggesting different aetiologies of stillbirth [47]. In addition, we found that live-born twins delivered at a gestational age between 37 and 38 weeks were associated with a lower risk of SGA and low Apgar scores. Furthermore, we found that in reference to uncomplicated pregnancies, women with antepartum complications were associated with an increased risk of giving birth to SGA infants in different gestational weeks compared with ongoing pregnancies. Live-born infants born at any time between 28 and 39 weeks among women with medical diseases, and 28 and 34 weeks among women with antepartum complications were associated with an increased risk of low Apgar scores. Although the increased risk of SGA or low Apgar scores were in accordance with previous research, few of them analysed these associations at different gestational ages [48,49,50,51]. Besides, in subgroup analysis, infants born at 37 or 38 weeks of gestational age were associated with a decreased risk of stillbirth, SGA, and low Apgar score when compared with ongoing pregnancies. Thus suggesting that 37 and 38 weeks were the optimal gestational ages for decreased risk of stillbirth, SGA, and low Apgar scores when compared with ongoing pregnancies.
The strength of this study was in demonstrating the twinning rate and health condition of twins in an adequate sample size from 2012 to 2020 and analysing the health conditions of twins at different gestational ages. However, there are still limitations to this study. Firstly, the weighting method of population distribution may not have been fully adjusted for the oversampling of high-level hospitals when estimating the stillbirth, SGA, and low Apgar rate of twins. Secondly, we could not distinguish whether the twins were monochorionic or dichorionic, and the type of chorionicity was an important factor for stillbirth and perinatal health in twin born infants. Further studies could explore different types of twins.
Conclusions
The twinning rate in China showed an increasing trend from 2012 to 2020, and the adverse perinatal outcomes of twins showed a decreasing trend during the same period. Changes in the fertility policy have little effect on the twinning rate or the rate of adverse perinatal outcomes such as stillbirth, SGA, or rate of low Apgar scores. The optimal gestational age for twins to lower the risk of stillbirth, SGA, and low Apgar scores was 37 weeks. Women with medical diseases or antepartum complications should be more cautious as they have an increased risk of adverse outcomes.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due to the terms of our contract with the Chinese National Health Commission but are available from the corresponding author on reasonable request.
Abbreviations
- SGA:
-
Small-for-gestation-age
- NMNMSS:
-
National Maternal Near Miss Surveillance System
- ITSA:
-
Interrupted Time Series Analysis
- GLM:
-
Generalised Linear Model
- aORs:
-
Adjusted odds ratios
- CIs:
-
Confidence intervals
References
Pison G, D’Addato AV. Frequency of twin births in developed countries. Twin Res Hum Genet. 2006;9(2):250–9.
Lu X, Zhang J, Liu Y, Wang T, Lu Y, Li Z. Epidemiology of twin births in southeast China: 1993–2005. Twin Res Hum Genet. 2013;16(2):608–13.
Deng C, Dai L, Yi L, Li X, Deng K, Mu Y, Wang K, Tao J, Li Q, Xu L. Temporal trends in the birth rates and perinatal mortality of twins: A population-based study in China. PLoS ONE. 2019;14(1): e0209962.
Li HT, Xue M, Hellerstein S, Cai Y, Gao Y, Zhang Y, Qiao J, Blustein J, Liu JM. Association of China’s universal two child policy with changes in births and birth related health factors: national, descriptive comparative study. BMJ. 2019;366: l4680.
Shinar S, Walsh L, Roberts N, Melamed N, Barrett J, Riddell C, et al. Timing of cesarean delivery in women with ≥2 previous cesarean deliveries. Am J Obstet Gynecol. 2022;226(1):110.e1-110.e10. https://doi.org/10.1016/j.ajog.2021.07.018.
Jensen EA, Foglia EE, Dysart KC, Simmons RA, Aghai ZH, Cook A, Greenspan JS, DeMauro SB. Adverse effects of small for gestational age differ by gestational week among very preterm infants. Arch Dis Child Fetal Neonatal Ed. 2019;104(2):F192–8.
2009 LPSE: Australia’s mothers and babies 2007. In: Perinatal statistics series no 23. vol. Cat. no. PER 48. Sydney: AIHW National Perinatal Statistics Unit; 2009.
Visintin C, Mugglestone MA, James D, Kilby MD, Guideline Development G. Antenatal care for twin and triplet pregnancies: summary of NICE guidance. BMJ. 2011;343: d5714.
Cheung YB, Yip P, Karlberg J. Mortality of twins and singletons by gestational age: a varying-coefficient approach. Am J Epidemiol. 2000;152(12):1107–16.
Murray SR, Bhattacharya S, Stock SJ, Pell JP, Norman JE. Gestational age at delivery of twins and perinatal outcomes: a cohort study in Aberdeen. Scotland Wellcome Open Res. 2019;4:65.
Dodd JM, Crowther CA, Haslam RR, Robinson JS. Twins Timing of Birth Trial G: Elective birth at 37 weeks of gestation versus standard care for women with an uncomplicated twin pregnancy at term: the Twins Timing of Birth Randomised Trial. BJOG. 2012;119(8):964–73.
Murray S, MacKay D, Stock S, Pell J, Norman J. Association of Gestational Age at Birth With Risk of Perinatal Mortality and Special Educational Need Among Twins. JAMA Pediatr. 2020;174(5):437–45.
Liang J, Li X, Kang C, Wang Y, Kulikoff XR, Coates MM, Ng M, Luo S, Mu Y, Wang X, et al. Maternal mortality ratios in 2852 Chinese counties, 1996–2015, and achievement of Millennium Development Goal 5 in China: a subnational analysis of the Global Burden of Disease Study 2016. Lancet. 2019;393(10168):241–52.
Liang J, Mu Y, Li X, Tang W, Wang Y, Liu Z, Huang X, Scherpbier RW, Guo S, Li M, et al. Relaxation of the one child policy and trends in caesarean section rates and birth outcomes in China between 2012 and 2016: observational study of nearly seven million health facility births. BMJ (Clinical research ed). 2018;360: k817.
**ong T, Mu Y, Liang J, Zhu J, Li X, Li J, Liu Z, Qu Y, Wang Y, Mu D. Hypertensive disorders in pregnancy and stillbirth rates: a facility-based study in China. Bull World Health Organ. 2018;96(8):531–9.
Mu Y, Wang X, Li X, Liu Z, Li M, Wang Y, Li Q, Deng K, Zhu J, Liang J. The national maternal near miss surveillance in China: A facility-based surveillance system covered 30 provinces. Medicine (Baltimore). 2019;98(44): e17679.
Zhu J, Liang J, Mu Y, Li X, Guo S, Scherpbier R, Wang Y, Dai L, Liu Z, Li M, et al. Sociodemographic and obstetric characteristics of stillbirths in China: a census of nearly 4 million health facility births between 2012 and 2014. Lancet Glob Health. 2016;4(2):e109-118.
Dai L, Deng C, Li Y, Zhu J, Mu Y, Deng Y, Mao M, Wang Y, Li Q, Ma S, et al. Birth weight reference percentiles for Chinese. PLoS ONE. 2014;9(8): e104779.
Miller J, Chauhan SP, Abuhamad AZ. Discordant twins: diagnosis, evaluation and management. Am J Obstet Gynecol. 2012;206(1):10–20.
Deng K, Liang J, Mu Y, Liu Z, Wang Y, Li M, Li X, Dai L, Li Q, Chen P, et al. Preterm births in China between 2012 and 2018: an observational study of more than 9 million women. Lancet Glob Health. 2021;9(9):e1226–41.
Population and Family Planning Law of the People's Republic of China [http://www.nhc.gov.cn/fzs/s3576/201808/0779015e232d4860a2867439e52018a1.shtml]. Accessed 30 Aug 2018.
Galatas B, Saute F, Marti-Soler H, Guinovart C, Nhamussua L, Simone W, Munguambe H, Hamido C, Montana J, Muguande O, et al. A multiphase program for malaria elimination in southern Mozambique (the Magude project): A before-after study. PLoS Med. 2020;17(8): e1003227.
Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, Laptook AR, Sanchez PJ, Van Meurs KP, Wyckoff M, et al. Trends in Care Practices, Morbidity, and Mortality of Extremely Preterm Neonates, 1993–2012. JAMA. 2015;314(10):1039–51.
Stock SJ, Ferguson E, Duffy A, Ford I, Chalmers J, Norman JE. Outcomes of elective induction of labour compared with expectant management: population based study. BMJ. 2012;344: e2838.
Knight HE, Cromwell DA, Gurol-Urganci I, Harron K, van der Meulen JH, Smith GCS. Perinatal mortality associated with induction of labour versus expectant management in nulliparous women aged 35 years or over: An English national cohort study. PLoS Med. 2017;14(11): e1002425.
Khalil A. The rate of twin birth is declining. Ultrasound Obstet Gynecol. 2021;58(5):784–5.
Monden C, Pison G, Smits J. Twin Peaks: more twinning in humans than ever before. Hum Reprod. 2021;36(6):1666–73.
Chiware TM, Vermeulen N, Blondeel K, Farquharson R, Kiarie J, Lundin K, Matsaseng TC, Ombelet W, Toskin I. IVF and other ART in low- and middle-income countries: a systematic landscape analysis. Hum Reprod Update. 2021;27(2):213–28.
Malamitsi-Puchner A, Voulgaris K, Sdona E, Christou C, Briana DD. Twins and socioeconomic factors: changes in the last 20 years. The journal of maternal-fetal & neonatal medicine : the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstet. 2019;32(3):455–60.
Hur YM. Changes in Multiple Birth Rates and Parental Demographic Factors in South Korea During the Last Four Decades: 1981–2019. Twin Res Hum Genet. 2021;24(3):163–7.
Saccone G, Gragnano E, Ilardi B, Marrone V, Strina I, Venturella R, et al. Maternal and perinatal complications according to maternal age: A systematic review and meta-analysis. Int J Gynaecol Obstet. 2022 Jan 19. https://doi.org/10.1002/ijgo.14100. Epub ahead of print. PMID: 35044694.
Joseph KS, Marcoux S, Ohlsson A, Liu S, Allen AC, Kramer MS, Wen SW. Fetal, Infant Heath Study Group of the Canadian Perinatal Surveillance S: Changes in stillbirth and infant mortality associated with increases in preterm birth among twins. Pediatrics. 2001;108(5):1055–61.
Allen VM, Wilson RD, Cheung A, Genetics C, Reproductive E, Infertility C. Pregnancy outcomes after assisted reproductive technology. J Obstet Gynaecol Can. 2006;28(3):220–33.
Hu Y, Wu Q, Liu J, Hong D, Zou Y, Lu J, Wang Y, Chen D, Qi L, Liang Z. Risk factors and incidence of third trimester stillbirths in China. Sci Rep. 2021;11(1):12701.
Stringer EM, Chibwesha C, Stoner M, Vwalika B, Joseph J, Chi BH, Kaunda E, Goodnight W, Stringer JS. A population-based cohort study of stillbirth among twins in Lusaka, Zambia. Int J Gynaecol Obstetr. 2015;130(1):74–8.
Getahun D, Demissie K, Marcella SW, Rhoads GG. The impact of changes in preterm birth among twins on stillbirth and infant mortality in the United States. J Perinatol. 2014;34(11):823–9.
Kilby MD, Gibson JL, Ville Y. Falling perinatal mortality in twins in the UK: organisational success or chance? BJOG. 2019;126(3):341–7.
Fetal medicine Subgroup CSoP, Chinese Medical Association. Obstetrics Subgroup, Chinese Society of Obstetrics Gynecology, Chinese Medical Association. : Guidelines for the clinical management of twin pregnancy. Chin J Obstetr Gynecol 2015;50(8):7.
Standard for risk assessment and management of pregnant women [http://www.nhc.gov.cn/cms-search/xxgk/getManuscriptXxgk.htm?id=9c3dc9b4a8494d9a94c02f890e5085b1]. Accessed 09 Nov 2017.
Notice on completing the work of the National Basic Public Health Service Project in 2013 [http://www.nhc.gov.cn/jws/s3577/201306/b035feee67f9444188e5123baef7d7bf.shtml]. Accessed 17 June 2013.
Neonatal asphyxia resuscitation training programs will cover the whole country [http://www.nhc.gov.cn/wjw/zcjd/201304/9fee068b0e2c40e6a3c4584ba9a134cc.shtml]. Accessed 27 May 2005.
Cheung YB. On the definition of gestational-age-specific mortality. Am J Epidemiol. 2004;160(3):207–10.
Lee YM, Wylie BJ, Simpson LL, D’Alton ME. Twin chorionicity and the risk of stillbirth. Obstet Gynecol. 2008;111(2 Pt 1):301–8.
Hure AJ, Powers JR, Mishra GD, Herbert DL, Byles JE, Loxton D. Miscarriage, preterm delivery, and stillbirth: large variations in rates within a cohort of Australian women. PLoS ONE. 2012;7(5): e37109.
Yang M, Fan XB, Wu JN, Wang JM. Association of assisted reproductive technology and multiple pregnancies with the risks of birth defects and stillbirth: A retrospective cohort study. Sci Rep. 2018;8(1):8296.
Sarmon KG, Eliasen T, Knudsen UB, Bay B. Assisted reproductive technologies and the risk of stillbirth in singleton pregnancies: a systematic review and meta-analysis. Fertil Steril. 2021;116(3):784–92.
Wisborg K, Ingerslev HJ, Henriksen TB. IVF and stillbirth: a prospective follow-up study. Hum Reprod. 2010;25(5):1312–6.
Wang Y, Wu N, Shen H. A Review of Research Progress of Pregnancy with Twins with Preeclampsia. Risk Manag Healthc Policy. 2021;14:1999–2010.
Lyu S, Gao L, Sun J, Zhao X, Wu Y, Hua R, Wang Y: The association between maternal complications and small for gestational age in twin pregnancies using singleton and twin birth weight references. J Maternal-fetal Neonatal Med. 2021:1–7.
Unal C, Tanacan A, Ziyadova G, Fadiloglu E, Beksac MS. Effect of viral load on pregnancy outcomes in chronic hepatitis B infection. J Obstet Gynaecol Res. 2019;45(9):1837–42.
Ding G, Vinturache A, Yu J, Lu M, Pang Y, Tian Y, Zhang J. Optimal delivery timing for twin pregnancies: A population-based retrospective cohort study. Int J Clin Pract. 2021;75(5): e14014.
Acknowledgements
The authors acknowledge the institutions and staff of the National Maternal Near Miss Surveillance System for data collection, data entry, and data verification.
Funding
This study was supported by the National Key R&D Program of China (Grant No. 2019YFC1005100), the National Health Commission of the People’s Republic of China, the China Medical Board (Grant No. 11–065), the WHO (Grant No. CHN-12-MCN-004888), and UNICEF (Grant No. 2016EJH016). We thank the institutions and staff of the National Maternal Near Miss Surveillance System for data collection.
Author information
Authors and Affiliations
Contributions
P.C., M.L., J.L., and Y.X. designed the study with contribution from all authors. P.C. and M.Y. did the statistical analysis with support from Z.L., Y.W., X.L, Q.L., J.Z. and L.D., P.C., M.L., J.L., and Y.X. prepared the first draft and all authors contributed to critical interpretation of the results and development of the report. All authors saw and approved the final version.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Review Committee of West China Second University Hospital, Sichuan University, and conducted in accordance with the principles of the Declaration of Helsinki. Because of the retrospective design of this study, the Ethics Review Committee of West China Second University Hospital, Sichuan University has waived the requirement of the informed consent for this study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Supplementary Figure 1. Incidence of stillbirth by year and gestational age.
Additional file 2: Supplementary Figure 2.
Incidence of SGA by year and gestational age.
Additional file 3:
Supplementary Figure 3. Incidence of Low Apgar score by year and gestational age.
Additional file 4: Supplementary Figure 4.
Association between maternal complications and adverse perinatal outcomes in women of advanced ages.* *Foetuses staying in utero were used as reference in separate gestational ages, women in medical diseases group or antepartum complications group were compared with uncomplicated women. All results were adjusted for the sampling distribution of the population and clustered of births within hospitals and pregnant woman individuals. Covariates were adjusted as area classification, geographic location, hospital level, infants birth year, education, marriage, parity, prenatal examination, twins born sequence and weight imbalance.
Additional file 5:
Supplementary Table 1.Risk of stillbirth at Each Week of Gestation Compared with Remaining in Utero categorized by maternal complication condition. Supplementary Table 2.Risk of SGA at Each Week of Gestation Compared with Remaining in Utero categorized by maternal complication condition. Supplementary Table 3.Risk of low apgar score (<4) at Each Week of Gestation Compared with Remaining in Utero categorized by maternal complication condition.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, P., Li, M., Mu, Y. et al. Temporal trends and adverse perinatal outcomes of twin pregnancies at differing gestational ages: an observational study from China between 2012–2020. BMC Pregnancy Childbirth 22, 467 (2022). https://doi.org/10.1186/s12884-022-04766-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-022-04766-0