Abstract
Background
Vitamin D deficiency has been examined as a risk factor for severity and progression of kidney disease due to its immunomodulatory effects. There is paucity of data about its impact in IgA nephropathy (IgAN).
Methods
In a retrospective cohort study, 25 (OH) vitamin D assay was performed in bio-banked baseline serum samples collected during kidney biopsy of 105 adult patients with primary IgAN diagnosed between 2015 and 2019. A level of < 10 ng/mL was defined as Vitamin D deficiency.
Results
Mean age of patients was 34 ± 10.6 years, 69.5% were males. Mean baseline 25(OH) Vitamin D levels was 15.9 ± 11.9 ng/mL and 41(39%) patients had vitamin D deficiency. Serum albumin level was lower in vitamin D deficient patients compared to those who had higher vitamin D levels (3.7 ± 0.9 vs 4.1 ± 0.7 g/dl, p = 0.018)but there was no significant difference in baseline proteinuria and eGFR. Crescentic lesions were more frequent in vitamin D deficient group (19.5% vs 6.3%, p = 0.022). At median follow up of 21.5 months (6 – 56 months), there was no difference in remission (68.3% vs 65.6%, p = 0.777) and disease progression (12.5% vs 9.4%, p = 0.614) in those with and without Vitamin D deficiency respectively. On multivariate cox proportional hazard analysis, vitamin D deficiency was not a significant risk factor for renal survival (HR-1.79, 95% confidence interval:0.50–6.34, p = 0.368).
Conclusion
There was no association between vitamin D deficiency and disease profile as well as renal outcome in Indian patients with IgAN.
Similar content being viewed by others
Introduction
IgA nephropathy (IgAN) is the most frequently diagnosed primary glomerular disease on renal biopsy in adults [1]. 20–30% of the patients progress to end stage kidney disease (ESKD) over a span of 10 to 20 years [2, 3]. However, we lack optimal non-invasive biomarkers to assess disease severity and prognosticate the outcome. Age, gender, hypertension, baseline renal function and proteinuria have been conventionally used as predictors of disease severity in clinical practice [4]. At present, therapeutic options comprise of supportive therapy with angiotensin converting enzyme inhibitor (ACEi) or an angiotensin receptor blocker (ARB) and blood pressure control followed by steroids and other immunosuppressive agents being used in those with progressive disease [5].
IgAN has been recognized to have an aggressive disease phenotype in Indians with 10-year survival reported to be around 35% [6,7,8].
Recent observations have highlighted the pleiotropic effects of Vitamin D. In patients with wide range of renal dysfunction, vitamin D deficiency was associated with vascular calcification, vascular endothelial function, cardiovascular events, and cardiovascular mortality [9,10,11,12,13,14]. Experimental data indicate that vitamin D analogues mediate a decrease in albuminuria and slow the progression of renal injury through activation of vitamin D receptor. Vitamin D insufficiency upregulates the renin-angiotensin system (RAS) and the NF-κB pathway, decreases the nitric oxide synthase transcription in vascular endothelial cells, increases inflammation and oxidative stress, and therefore may be a risk factor for progression of kidney disease. Vitamin D has been reported to play a role in preventing diabetic nephropathy and supplementation has shown to reduce proteinuria in these patients [15,16,17].
Vitamin D deficiency has been shown to corelate with severity of disease in IgAN [18]. Vitamin D supplementation with renin-angiotensin system blockade has been shown to reduce proteinuria in these patients [19,20,21,22,23]. Most of this information is from Chinese cohorts. Since there is considerable ethnic variability in the disease phenotype, role of Vitamin D on disease severity and outcome still remains uncertain in other populations. Vitamin D deficiency is widely prevalent in India [24, 25]. Being easily available, vitamin D assessment could serve as a useful additional factor to guide therapy if it affects disease outcome in IgAN patients.
Methods
In a retrospective cohort study, we included adult patients (≥ 18 years) with biopsy proven primary IgAN diagnosed between 2015 and 2019 at a tertiary care referral institute in North India with a minimum follow-up of 6 months. We excluded patients who had (1) history of immunosuppression use in the previous 6 months before biopsy (2) secondary causes of IgAN like chronic liver disease, Henoch-Schonlein purpura (3) a second coexisting disease on kidney biopsy like diabetic nephropathy (4) inadequate/missing clinical records (5) inadequate kidney biopsy (6) follow up less than 6 months (7) no baseline serum sample available.
Serum 25-OH Vitamin D level was measured in serum samples drawn at the time of biopsy. These samples were obtained from a biorepository where we routinely store sera of patients collected at the time of kidney biopsy with their consent at -800C until analysis with minimal freezing and thawing.
Serum 25(OH) vitamin D level was measured using the ARCHITECT™ assay which is a chemiluminescent microparticle immunoassay (CMIA). Vitamin D deficiency was defined as 25 (OH) vitamin D level < 10 ng/ml(severe deficiency). There is lack of consensus regarding the 25(OH) vitamin D level used to define vitamin D deficiency and the optimal target levels for different health outcomes [26, 27]. The prevalence of vitamin D deficiency is very high in India ranging from 70–100% in otherwise health populations using the standard definition of serum level of 25(OH)D < 20 ng/ml [24, 25]. In our study also 78(74.3%) patients had vitamin D deficiency based on this definition. So we decided to focus on patients with severe deficiency (25(OH)D < 10 ng/mL) to assess whether their outcome varied from the sub-group with higher levels.
Patients’ baseline demographic and clinical data and investigations including serum creatinine, albumin, presence of hematuria and proteinuria estimated by urine protein creatinine ratio (g/day), details of kidney biopsy and treatment given were retrieved from medical records. Estimated glomerular filtration rate (eGFR) was calculated by the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) formula.
The primary outcome was renal disease progression defined as at least 50% decline in eGFR or progression to ESKD (eGFR < 10 ml/min/1.73m2 or requiring renal replacement therapy). Remission was defined as 24-h urine protein < 1 g/day with at least 50% decline from baseline and a stable renal function (≤ 25% decline in eGFR). The study was approved by the institute ethics committee, AIIMS, New Delhi and they provided a waiver of consent. The study was conducted according to the principles of declaration of Helsinki.
Statistical analysis
Data were summarized as mean ± SD, frequency (%) or median (range). Chi-square test was used to compare the categorical variables while the continuous variables were compared between the groups using independent t-test or Wilcoxon rank-sum test. multivariate cox proportional hazards model was used to determine predictors of renal survival. Kaplan Meier event-free survival curves for patients with and without vitamin D deficiency were derived and compared. P values < 0.05 were considered significant. All analyses were performed using STATA 14.0 (StataCorp, College Station, TX).
Results
One hundred and five patients with biopsy proven IgAN were enrolled in this study. The baseline profile of the study cohort is shown in Table 1. Their mean age was 34 ± 10.6 years and 69.5% were males. A significant proportion of our patients (65, 62%) were hypertensive. The baseline serum creatinine was 1.4 ± 0.5 mg/dl and eGFR was 72.2 ± 33.5 mL/min/1.73 m2. The mean serum albumin was 4.0 ± 0.8 g/dL with a proteinuria of 3.1 ± 2.5 g/day. The mean vitamin D level was 15.9 ± 11.9 ng/ml. 41 (39%) patients had vitamin D deficiency.
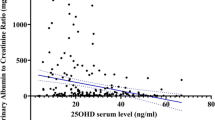
The study cohort was divided into 2 groups based on vitamin D levels – vitamin D deficient group (25(OH)D < 10 ng/mL) and vitamin D replete group (25(OH)D ≥ 10 ng/mL). The various clinical and laboratory parameters were compared between these groups (Table 2). The vitamin D deficient group was younger (31.8 ± 9.3 vs 35.5 ± 11.2 years, p = 0.082), had more females [18 (43.9%) vs 14(21.9%), p = 0.017] and had higher eGFR though it was not statistically significant (78.0 ± 37.1 vs 68.4 ± 36.9 ml/min/1.73m2, p = 0.326) compared to the vitamin D replete group. Both groups had similar levels of proteinuria, but the vitamin D deficient group had lower serum albumin level (3.7 ± 0.9 vs 4.1 ± 0.7 g/dl, p = 0.018). Both groups had similar prevalence of hypertension. The use of ACEi/ARBs was also similar in both groups. Table 3 shows the Oxford MEST-C scores of the kidney biopsies of patients in the two groups. There was no difference in the proportion of M1, E1, S1 and T1/2 lesions between the two groups. Crescentic lesions were more frequent in the vitamin D deficient group (19.51% vs 6.25%, p = 0.022).
As shown in table 2, at follow-up, 5(12.5%) patients with vitamin D deficiency had progressed to the primary outcome as compared to 6(9.4%) patients with no vitamin D deficiency (p = 0.614). There was no difference in proportion of patients who achieved remission in those with and without vitamin D deficiency (68.3% vs 65.6%, p = 0.777). Univariate cox proportional hazard analysis of potential predictors of disease progression are shown in Table 4.Vitamin D deficiency at time of diagnosis was not a significant risk factor for renal disease progression (HR-1.79, 95% confidence interval:0.52–6.21, p = 0.357). Baseline vitamin D levels were also not predictive of disease progression on multivariate cox regression analysis(HR-1.79, 95% confidence interval:0.50–6.34, p = 0.368)There was no difference in time to adverse event i.e., loss of renal survival between patients with and without vitamin D deficiency as can be seen in the Kaplan Meier curve (Fig. 1).
Discussion
IgA nephropathy(IgAN) can become a challenging condition to manage as it is a smoldering disease. Considering the significant variability in clinical presentation and progression, many non-invasive biomarkers have been explored as prognostication tools with limited success. Vitamin D is known to have immune-modulatory effects. Due to its interaction with the renin angiotensin system and the NFkB pathways it may play a role in progression of kidney diseases with proteinuria. Baseline 25(OH) vitamin D level has been reported to be a predictor of disease progression and death in patients with stage 2–5 chronic kidney disease [9]. Vitamin D deficiency has also been co-related with proteinuria and worsening of kidney function in diabetics [15,16,17]. There is a paucity of information pertaining to the impact of vitamin D deficiency in IgAN and data mostly comes from Chinese studies. Li et al. found that lower baseline 25(OH) vitamin D levels not only had a significant correlation with poorer clinical outcomes and more severe renal pathological features but was also strongly associated with increased risk of renal progression [18]. Patients who had 25(OH) vitamin D level less than 15 ng/ml were categorized as being vitamin D deficient in this study. There were more females in the Vitamin D deficient group. The degree of proteinuria was similar in both groups though hypoalbuminemia was slightly more common in the deficient group. The mean eGFR was actually higher in those with vitamin D deficiency though it was not significant. The proportion of patients who achieved remission and had renal survival were similar in both groups. Li et al. [18] also showed a significant inverse association between vitamin D status and blood pressure which was not observed in our cohort. Tubulointerstitial chronicity(T1/T2) was more frequent in the vitamin D deficient subgroup(p = 0.008) in the Chinese study [18]. We did not observe this in our cohort. However, we found a y higher prevalence of crescentic lesions in our patients with Vitamin D deficiency.
Our study has certain limitations. It is retrospective, with a small cohort. It is not feasible to study the impact of baseline vitamin D deficiency on the outcome of patients unless bio-banked samples can be tested retrospectively. In a prospective to study it would be unethical to measure baseline 25(OH) vitamin D levels and not replenish those who are deficient thus making it difficult to interpret the impact on outcome. There is significant variability in vitamin D levels across geographies, ethnic groups and also different sampling seasons(winter vs summer months) leading to lack of agreement on cut-offs used to define deficiency and optimal target levels for different health outcomes. The prevalence of vitamin D deficiency is very high in India ranging from 70–100% in otherwise healthy populations using the standard definition of serum level of 25(OH)D < 20 ng/ml [24, 25]. In our study also 78(74.3%) patients had vitamin D deficiency based on this definition. So, we stratified patients based on the presence or absence of severe Vitamin D deficiency [26] to assess its prognostic significance. Li et al. [16] classified patients of IgAN with 25 (OH) vitamin D levels < 15 ng/ml as vitamin D deficient as in the Third National Health and Nutrition Examination Survey (NHANES III) cohort, this was associated with a higher risk for all-cause mortality in CKD patients [28]. The targets used to define vitamin D deficiency in different studies vary widely making comparisons difficult.
We also did not study the impact of vitamin D therapy on the outcome. In a randomized controlled trial of 50 patients, oral calcitriol with ACEi/ARB was found to reduce proteinuria in IgAN [20]. Whether this is due to the effect of vitamin D deficiency in the pathogenesis of IgAN or due to its interaction with the renin-angiotensin system needs to be determined. Our study suggests that vitamin D deficiency per se may not impact disease outcome in IgAN patients. Unnecessary treatment may lead to adverse effects due to vitamin D intoxication. We need to study larger cohorts with longer follow-up to ascertain its role in the disease pathway of IgAN.
Availability of data and materials
All data required for this study and the relevant analysis are included in the manuscript. Any additional data required may be made available from the corresponding author on reasonable request.
References
McGrogan A, Franssen CFM, de Vries CS. The incidence of primary glomerulonephritis worldwide: a systematic review of the literature. Nephrol Dial Transplant. 2011;26(2):414–30.
D’Amico G. Natural history of idiopathic IgA nephropathy and factors predictive of disease outcome. Semin Nephrol. 2004;24(3):179–96.
Wyatt RJ, Julian BA. IgA nephropathy. N Engl J Med. 2013;368(25):2402–14.
Trimarchi H, Barratt J, Cattran DC, Cook HT, Coppo R, Haas M, Liu ZH, Roberts IS, Yuzawa Y, Zhang H, Feehally J, IgAN Classification Working Group of the International IgA Nephropathy Network and the Renal Pathology Society; Conference Participants. Oxford Classification of IgA nephropathy 2016: an update from the IgA Nephropathy Classification Working Group. Kidney Int. 2017;91(5):1014–21.
Kidney Disease: Improving Global Outcomes (KDIGO) Glomerular Diseases Work Group. KDIGO 2021 Clinical Practice Guideline for the Management of Glomerular Diseases. Kidney Int. 2021;100(4S):S1–276. https://doi.org/10.1016/j.kint.2021.05.021. PMID: 34556256.
Chacko B, John GT, Neelakantan N, Korula A, Balakrishnan N, Kirubakaran MG, Jacob CK. Presentation, prognosis and outcome of IgA nephropathy in Indian adults. Nephrology (Carlton). 2005;10(5):496–503.
Mittal N, Joshi K, Rane S, Nada R, Sakhuja V. Primary IgA nephropathy in north India: is it different? Postgrad Med J. 2012;88(1035):15–20.
Bagchi S, Singh G, Yadav R, Kalaivani M, Mahajan S, Bhowmik D, Dinda A, Agarwal SK. Clinical and histological profile of patients with primary IgA nephropathy seen in a tertiary hospital in India. Ren Fail. 2016;38(3):431–6.
Ravani P, Malberti F, Tripepi G, Pecchini P, Cutrupi S, Pizzini P, Mallamaci F, Zoccali C. Vitamin D levels and patient outcome in chronic kidney disease. Kidney Int. 2009;75(1):88–95.
Allegretto EA, Shevde N, Zou A, Howell SR, Boehm MF, Hollis BW, Pike JW. Retinoid X receptor acts as a hormone receptor in vivo to induce a key metabolic enzyme for 1,25-dihydroxyvitamin D3. J Biol Chem. 1995;270(41):23906–9.
Mehrotra R, Kermah DA, Salusky IB, Wolf MS, Thadhani RI, Chiu YW, Martins D, Adler SG, Norris KC. Chronic kidney disease, hypovitaminosis D, and mortality in the United States. Kidney Int. 2009;76(9):977–83. https://doi.org/10.1038/ki.2009.288.
Mizobuchi M, Morrissey J, Finch JL, Martin DR, Liapis H, Akizawa T, Slatopolsky E. Combination therapy with an angiotensin-converting enzyme inhibitor and a vitamin D analog suppresses the progression of renal insufficiency in uremic rats. J Am SocNephrol. 2007;18(6):1796–806. https://doi.org/10.1681/ASN.2006091028.
Yang S, Li A, Wang J, Liu J, Han Y, Zhang W, Li YC, Zhang H. Vitamin D Receptor: A Novel Therapeutic Target for Kidney Diseases. Curr Med Chem. 2018;25(27):3256–71.
Satirapoj B, Limwannata P, Chaiprasert A, Supasyndh O, Choovichian P. Vitamin D insufficiency and deficiency with stages of chronic kidney disease in an Asian population. Bmc Nephrol. 2013;14:206.
Deb DK, Sun T, Wong KE, Zhang Z, Ning G, Zhang Y, Kong J, Shi H, Chang A, Li YC. Combined vitamin D analog and AT1 receptor antagonist synergistically block the development of kidney disease in a model of type 2 diabetes. Kidney Int. 2010;77(11):1000–9. https://doi.org/10.1038/ki.2010.22.
Hu X, Liu W, Yan Y, Liu H, Huang Q, **ao Y, Gong Z, Du J. Vitamin D protects against diabetic nephropathy: Evidence-based effectiveness and mechanism. Eur J Pharmacol. 2019;15(845):91–8.
Agarwal R. Vitamin D, proteinuria, diabetic nephropathy, and progression of CKD. Clin J Am Soc Nephrol. 2009;4(9):1523–8.
Li XH, Huang XP, Pan L, Wang CY, Qin J, Nong FW, Luo YZ, Wu Y, Huang YM, Peng X, Yang ZH, Liao YH. Vitamin D deficiency may predict a poorer outcome of IgA nephropathy. BMC Nephrol. 2016;17(1):164.
**aowei L, Bo W, Li L, Peng Z. Comparison of the effects of valsartan plus activated vitamin D versus valsartan alone in IgA nephropathy with moderate proteinuria. Int Urol Nephrol. 2020;52(1):129–36.
Liu LJ, Lv JC, Shi SF, Chen YQ, Zhang H, Wang HY. Oral calcitriol for reduction of proteinuria in patients with IgA nephropathy: a randomized controlled trial. Am J Kidney Dis. 2012;59(1):67–74. https://doi.org/10.1053/j.ajkd.2011.09.014. Epub 2011 Oct 22.
Yuan D, Fang Z, Sun F, Chang J, Teng J, Lin S, Liu X. Effect of Vitamin D and Tacrolimus Combination Therapy on IgA Nephropathy. Med Sci Monit. 2017;29(23):3170–7.
Szeto CC, Chow KM, Kwan BC, Chung KY, Leung CB, Li PK. Oral calcitriol for the treatment of persistent proteinuria in immunoglobulin a nephropathy: an uncontrolled trial. Am J Kidney Dis. 2008;51(5):724–31.
Deng J, Zheng X, **e H, Chen L. Calcitriol in the treatment of IgA nephropathy with non-nephrotic range proteinuria: a meta-analysis of randomized controlled trials. Clin Nephrol. 2017;87((2017)1):21–7.
Trilok Kumar G, Chugh R, Eggersdorfer M. Poor Vitamin D Status in Healthy Populations in India: A Review of Current Evidence. Int J Vitam Nutr Res. 2015;85(3–4):185–201.
G R, Gupta A. Vitamin D deficiency in India: prevalence, causalities and interventions. Nutrients. 2014;6(2):729–75. https://doi.org/10.3390/nu6020729. PMID: 24566435; PMCID: PMC3942730.
Kennel KA, Drake MT, Hurley DL. Vitamin D deficiency in adults: when to test and how to treat. Mayo Clin Proc. 2010;85(8):752–7; quiz 757–8 https://doi.org/10.4065/mcp.2010.0138. PMID: 20675513; PMCID: PMC2912737.
Institute of Medicine (US) Committee to Review Dietary Reference Intakes for Vitamin D and Calcium. Dietary Reference Intakes for Calcium and Vitamin D. Ross AC, Taylor CL, Yaktine AL, Del Valle HB, editors. Washington (DC): National Academies Press (US); 2011. PMID: 21796828.
Mehrotra R, Kermah DA, Salusky IB, Wolf MS, Thadhani RI, Chiu YW, Martins D, Adler SG, Norris KC. Chronic kidney disease, hypovitaminosis D, and mortality in the United States. Kidney Int. 2009;76(9):977–83. https://doi.org/10.1038/ki.2009.288. Epub 2009 Aug 5. PMID: 19657329; PMCID: PMC3791220.
Acknowledgements
Part of the study was presented in ASN renal week 2020.
Funding
The study did not receive any funding.
Author information
Authors and Affiliations
Contributions
NF- wrote the protocol (under supervision), interpreted the data, wrote the manuscript, AS-patient follow up, supervision, PC- supervised, responsible for Vitamin D testing, GS-reported the kidney biopsies, HS-statistical analysis, DB- supervision, patient follow up, SB-conceptualized and wrote the protocol, supervised study implementation and analysis and wrote the manuscript SKA-supervised the study and contributed to the manuscript. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Institute Ethics Committee of All India Institute of Medical Sciences, New Delhi and Ethics Committee of All India Institute of Medical Sciences, New Delhi has provided a waiver for informed consent since it was a retrospective study. The study was performed in accordance with the Helsinki Declaration.
Consent for publication
Not applicable.
Competing interests
None of the authors have any competing interests to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Farooqui, N., Subbiah, A., Chaturvedi, P. et al. Association of vitamin D status with disease severity and outcome in Indian patients with IgA nephropathy. BMC Nephrol 24, 15 (2023). https://doi.org/10.1186/s12882-023-03061-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12882-023-03061-0