Abstract
Background
Infants born to hepatitis B surface antigen (HBsAg) positive mothers are at a higher risk for Hepatitis B virus (HBV) infection. Host genetic background plays an important role in determining the strength of immune response to vaccination. We conducted this study to investigate the association between Tumor necrosis factor (TNF) and Mitogen-activated protein kinase eight (MAPK8) polymorphisms and low response to hepatitis B vaccines.
Methods
A total of 753 infants of HBsAg positive and hepatitis Be antigen (HBeAg) negative mothers from the prevention of mother-to-infant transmission of HBV cohort were included. Five tag single nucleotide polymorphism (SNPs) (rs1799964, rs1800629, rs3093671, rs769177 and rs769178) in TNF and two tag SNPs (rs17780725 and rs3827680) in MAPK8 were genotyped using the MassARRAY platform.
Results
A higher percentage of breastfeeding (P = 0.013) and a higher level of Ab titers were observed in high responders (P < 0.001). The MAPK8 rs17780725 AA genotype increased the risk of low response to hepatitis B vaccines (OR = 3.176, 95% CI: 1.137–8.869). Additionally, subjects with the AA genotype may have a lower Ab titer than subjects with GA or GG genotypes (P = 0.051). Compared to infants who were breastfed, infants who were not breastfed had an increased risk of low response to hepatitis B vaccine (OR = 2.901, 95% CI:1.306–6.441).
Conclusions
MAPK8 polymorphisms are associated with immune response to HBV vaccinations in infants of HBsAg(+)/HBeAg(−) mothers.
Similar content being viewed by others
Background
Hepatitis B virus (HBV) infection is a global health problem with 780,000 related deaths annually [1]. Mother-to-child transmission (MTCT) of HBV remains a major cause of chronic HBV infection. The most effective way to avoid MTCT is by carrying out a standardized and sufficient hepatitis B immunization program in newborns [2, 3]. In China, from 1992 to 2006, the prevalence of hepatitis B surface antigen (HBsAg) has been reduced by 90% among children under 5 years old, as a result of an HBV immunoprophylaxis program [4]. However, approximately 6–20% of infants born to HBsAg(+) mothers exhibited a non- or low- response to the HBV vaccine, which led to increased risk of horizontal transmission of HBV infection [5,6,7,8]. Vaccine type, low birth weight and high maternal viral load have been identified as the most important risk factors for low immune response to HBV vaccine [9,10,1). All participants gave written informed consent. The signed consent was obtained from a parent or guardian on behalf of their infants. Our study was approved by the Medical Ethics Committee of the First Hospital of Jilin University (approval number 2012–098).
Vaccination and laboratory examinations
Infants were injected with 100 IU HBIG (Hualan Biological Engineering, **
Five tag SNPs (rs1799964, rs1800629, rs3093671, rs769177 and rs769178) in TNF and two tag SNPs (rs17780725 and rs3827680) in MAPK8 were selected from two online databases, GVS (http://gvs.gs.washington.edu/GVS147/) and SNPinfo (http://snpinfo.niehs.nih.gov/). DNA was extracted using AxyPrep Blood Genomic DNA Miniprep Kit (Axygen, Union City, CA, USA). Genoty** of each SNP was conducted using the MassARRAY platform (Sequenom, CA, USA) and performed by Bio Miao Biological Technology (Bei**g) Co., Ltd.
Statistical analysis
We tested each SNP for Hardy-Weinberg disequilibrium (HWD). Categorical variables were represented as frequency (percentage) and compared using the χ2 test. Continuous variables with normal distributions were represented as the mean ± standard deviation (SD) and compared using t-tests. Associations between SNPs and low response to HBV vaccine were analyzed via unconditional logistic regression with adjustment for possible confounders. The odds ratios (ORs) and 95% confidence intervals (CIs) were calculated to estimate risk. Ab titers in different groups were compared using analysis of covariance and adjusted for possible confounders. All statistical analyses were performed with the Statistical Package for Social Science (SPSS Inc., Chicago, IL, version 18.0). P < 0.05 was considered statistically significant.
Results
Characteristics of subjects
A total of 709 samples were included in the final analysis. Comparing the characteristics of low- and high responders, a higher percentage of breastfeeding (P = 0.013) and a higher level of Ab titers were observed in high responders (P < 0.001); data shown in Table 1.
Genotype and allele distributions of SNPs
All of the SNPs in high responders were consistent with Hardy-Weinberg equilibrium (P > 0.05, Additional file 1). There were no significant differences in any of the eight SNP genotype or allele frequencies between low responders and high responders (Table 2). The MAPK8 rs17780725 AA genotype seems to be associated with low response to hepatitis B vaccines, but it has not yet reached significance (P = 0.083).
Association between SNPs and low response to hepatitis B vaccines
After adjustment for gestational age, birth weight, gender, delivery mode and feeding pattern, the rs17780725 AA genotype increased the risk of low response to hepatitis B vaccines (OR = 3.176, 95% CI: 1.137–8.869, Table 3). Additionally, subjects with the MAPK8 rs17780725 AA genotype had a lower Ab titer than subjects with GA or GG carriers (P = 0.051, Table 4). Infants who were not breastfed had 2.901 times the odds of low response to the hepatitis B vaccine compared to infants who were breastfed. (95% CI:1.306–6.441).
Haplotype analysis
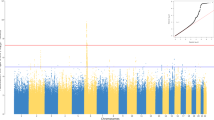
The pattern of pairwise linkage disequilibrium (LD) between the SNPs in TNF and MAPK8 are shown in Additional file 2. The SNPs in TNF and MAPK8 did not exhibit strong linkage disequilibrium, with no r2 greater than 0.8. Our haplotype analysis showed that no haplotype in TNF and MAPK8 genes was significantly associated with low response to hepatitis B vaccines (Additional files 3 and 4).
Discussion
Antibody responses in neonates are usually lower and differ from older children or adults [20, 21]. As a result, infants might have a lower response to HBV vaccination. Meanwhile, infants born to HBsAg(+) mothers have an increased risk of HBV infection compared to infants born to healthy mothers due to a persistent exposure to HBV from their mothers. It is therefore important to investigate the genetic risk factors for low response to hepatitis B vaccination and to improve the antibody level for these infants at high risk for HBV exposure.
The MAPK pathway is activated in innate immune cells in response to microbial infection [22]. MAPK8, also known as JNK1, may promote the phosphorylation of transcription factors following up-regulation in the expression of pro-inflammatory cytokines and chemokines. MAPK8 is mainly involved in the differentiation of helper T cells into Th1 cells during the antiviral immune response. As a result, different variants of the MAPK8 gene could affect the Th1 mediated cellular immune response and ultimately affect the production of vaccine-induced antibodies [23]. Our study found that the MAPK8 rs17780725 AA genotype may increase the risk of low response to hepatitis B vaccines. Rs17780725 is in strong LD with rs2698768 (r2 = 0.94), which is in the transcription factor binding site (TFBS) of MAPK8. This means that the replacement of G by A in rs17780725 might decrease the binding power between transcription factors and MAPK8, leading to down-regulation of MAPK8 transcription and the MAPK8 protein, which could ultimately down-regulate the immune response to HBV vaccination. In fact, our results also show that subjects with the rs17780725 AA genotype had a lower level of Ab titers.
TNF is a pro-inflammatory cytokine that regulates innate immunity. When a vaccine-induced immune response occurs, TNF-α may increase the expression level of certain cytokines, leading to up-regulation of immune reaction [18]. Meanwhile, when HBV infection occurs, HBV-specific CD8+ T cells also secrete TNF-α in the body in order to clear HBV [24]. Dhiman N et al. has found the TNF rs1799964 CC genotype to be associated with a lower measles antibody response in a Somali population [25]. Berran Yucesoy et al. [18] also have shown the TNF rs1800629 AA genotype to be correlated with a lower antibody level after HBV vaccination in a non-Hispanic white childhood cohort. However, in our study, the SNPs in TNF were not found to be associated with low response to hepatitis B vaccination. Different ethnic groups may have different genetic backgrounds. For example, the MAF of rs1800629 in Han Chinese is quite different than that found in non-Hispanic whites (0.05 vs 0.11). Additionally, there were only 41 low responders in our study. The limited number of low responders may have limited statistical power. Thus, a similar study with larger sample size study should be conducted in the future.
Our study has some additional limitations. First, we only enrolled the infants of HBsAg(+)/HBeAg(−) mothers from our MTCT cohort. Infants born to HBsAg(+)/HBeAg(+) mothers were given injections of 20 μg hepatitis B vaccine at 0, 1 and 6 months of age in our cohort, and only 7 low responders were found among these infants. Although the dose of vaccine was the most important factor affecting the immune response to HBV vaccination, too few infants with a low response would limit statistical power. As a result, we only included the infants of HBsAg(+)/HBeAg(−) mothers in this study. Secondly, antibody levels decreased gradually during the follow-up period. For non-responders, a booster immunization still needs to be administered. Therefore, future studies should include a longer follow up time and an analysis of the association between SNPs and the administration of a booster dose.
Conclusions
MAPK8 polymorphisms are associated with immune responsiveness to HBV vaccinations in infants of HBsAg(+)/HBeAg(−) mothers.
Abbreviations
- Ab:
-
Antibody
- CIs:
-
confidence intervals
- CMIA:
-
chemiluminescent microparticle immunoassay
- GWAS:
-
genome-wide association studies
- HBeAg:
-
hepatitis B e antigen
- HBsAg:
-
hepatitis B surface antigen
- HBV:
-
Hepatitis B virus
- HLA:
-
human leukocyte antigen
- MAPK8:
-
Mitogen-activated protein kinase eight
- MTCT:
-
Mother-to-child transmission
- ORs:
-
odds ratios
- SD:
-
standard deviation
- SNP:
-
single nucleotide polymorphism
- TFBS:
-
transcription factor binding site
- TNF:
-
Tumor necrosis factor
References
Goldstein ST, Zhou F, Hadler SC, Bell BP, Mast EE, Margolis HS. A mathematical model to estimate global hepatitis B disease burden and vaccination impact. Int J Epidemiol. 2005;34(6):1329–39.
Wen WH, Lai MW, Chang MH. A review of strategies to prevent mother-to-infant transmission of hepatitis B virus infection. Exp Rev Gastroenterol Hepatol. 2016;10(3):317–30.
Wei KP, Zhu FC, Liu JX, Yan L, Lu Y, Zhai XJ, Chang ZJ, Zeng Y, Li J, Zhuang H. The efficacy of two different dosages of hepatitis B immunoglobulin combined with hepatitis B vaccine in preventing mother-to-child transmission of hepatitis B virus: a prospective cohort study. Vaccine. 2018;36(2):256–63.
Liang X, Bi S, Yang W, Wang L, Cui G, Cui F, Zhang Y, Liu J, Gong X, Chen Y, et al. Evaluation of the impact of hepatitis B vaccination among children born during 1992-2005 in China. J Infect Dis. 2009;200(1):39–47.
Wu Y, Cao D, Qu L, Cao X, Jia Z, Zhao T, Wang Q, Jiang J. PD-1 and PD-L1 co-expression predicts favorable prognosis in gastric cancer. Oncotarget. 2017;8(38):64066–82.
Chen X, Gui X, Zhang L, Huang F, Zhong H, Pang Z, Wang S, Tang L, Fu L, Peng Y, et al. Maternal anti-HBVs suppress the immune response of infants to hepatitis B vaccine. J Viral Hepat. 2016;23(12):955–60.
Coppola N, Corvino AR, De Pascalis S, Signoriello G, Di Fiore E, Nienhaus A, Sagnelli E, Lamberti M. The long-term immunogenicity of recombinant hepatitis B virus (HBV) vaccine: contribution of universal HBV vaccination in Italy. BMC Infect Dis. 2015;15:149.
Weis N, Cowan S, Hallager S, Drose S, Kristensen LH, Gronbaek K, Jensen J, Gerstoft J, Madsen LG, Clausen MR, et al. Vertical transmission of hepatitis B virus during pregnancy and delivery in Denmark. Scand J Gastroenterol. 2017;52(2):178–84.
Wang J, He Y, ** D, Liu J, Zheng J, Yuan N, Bai Y, Yan T, Yang Y, Liu Y, et al. No response to hepatitis B vaccine in infants born to HBsAg(+) mothers is associated to the transplacental transfer of HBsAg. Infect Dis. 2017;49(8):576–83.
Wang C, Wang C, Jia ZF, Wu X, Wen SM, Kong F, Hu KQ, Li J, Jiang J, Niu JQ. Protective effect of an improved immunization practice of mother-to-infant transmission of hepatitis B virus and risk factors associated with immunoprophylaxis failure. Medicine. 2016;95(34):e4390.
Wang B, Xu XX, Wen HX, Hao HY, Yang ZQ, Shi XH, Fu ZD, Wang XF, Zhang F, Wang B, et al. Influencing factors for non/low-response to hepatitis-B vaccine in infants of HBsAg positive mothers. Zhonghua Liu **ng Bing Xue Za Zhi. 2017;38(7):911–5.
Pan L, Zhang L, Zhang W, Wu X, Li Y, Yan B, Zhu X, Liu X, Yang C, Xu J, et al. A genome-wide association study identifies polymorphisms in the HLA-DR region associated with non-response to hepatitis B vaccination in Chinese Han populations. Hum Mol Genet. 2014;23(8):2210–9.
Png E, Thalamuthu A, Ong RT, Snippe H, Boland GJ, Seielstad M. A genome-wide association study of hepatitis B vaccine response in an Indonesian population reveals multiple independent risk variants in the HLA region. Hum Mol Genet. 2011;20(19):3893–8.
Zhang XL, Ni XC, Jia JH, Dong JH, Yu FX, Ma N, Liu XH, Li M, Liu DW. Association of the rs3077 and rs9277535 polymorphisms in HLA-DP with hepatitis B virus infection and spontaneous clearance: a meta-analysis. Scand J Gastroenterol. 2013;48(6):736–44.
Hohler T, Reuss E, Evers N, Dietrich E, Rittner C, Freitag CM, Vollmar J, Schneider PM, Fimmers R. Differential genetic determination of immune responsiveness to hepatitis B surface antigen and to hepatitis a virus: a vaccination study in twins. Lancet (London, England). 2002;360(9338):991–5.
Halayko AJ, Amrani Y. Mechanisms of inflammation-mediated airway smooth muscle plasticity and airways remodeling in asthma. Respir Physiol Neurobiol. 2003;137(2–3):209–22.
Li Q, Verma IM. NF-kappaB regulation in the immune system. Nat Rev Immunol. 2002;2(10):725–34.
Yucesoy B, Johnson VJ, Fluharty K, Kashon ML, Slaven JE, Wilson NW, Weissman DN, Biagini RE, Germolec DR, Luster MI. Influence of cytokine gene variations on immunization to childhood vaccines. Vaccine. 2009;27(50):6991–7.
Ryckman KK, Fielding K, Hill AV, Mendy M, Rayco-Solon P, Sirugo G, van der Sande MA, Waight P, Whittle HC, Hall AJ, et al. Host genetic factors and vaccine-induced immunity to HBV infection: haplotype analysis. PLoS One. 2010;5(8):e12273.
Gans H, Yasukawa L, Rinki M, DeHovitz R, Forghani B, Beeler J, Audet S, Maldonado Y, Arvin AM. Immune responses to measles and mumps vaccination of infants at 6, 9, and 12 months. J Infect Dis. 2001;184(7):817–26.
Plebani A, Ugazio AG, Avanzini MA, Massimi P, Zonta L, Monafo V, Burgio GR. Serum IgG subclass concentrations in healthy subjects at different age: age normal percentile charts. Eur J Pediatr. 1989;149(3):164–7.
Cho SSL, Han J, James SJ, Png CW, Weerasooriya M, Alonso S, Zhang Y. Dual-specificity phosphatase 12 targets p38 MAP kinase to regulate macrophage response to intracellular bacterial infection. Front Immunol. 2017;8:1259.
Arbour N, Naniche D, Homann D, Davis RJ, Flavell RA, Oldstone MB. C-Jun NH(2)-terminal kinase (JNK)1 and JNK2 signaling pathways have divergent roles in CD8(+) T cell-mediated antiviral immunity. J Exp Med. 2002;195(7):801–10.
Pang J, Zhang G, Lin Y, **e Z, Liu H, Tang L, Lu M, Yan R, Guo H, Sun J, et al. Transforming growth factor beta-activated kinase 1 transcriptionally suppresses hepatitis B virus replication. Sci Rep. 2017;7:39901.
Dhiman N, Ovsyannikova IG, Vierkant RA, Pankratz VS, Jacobson RM, Poland GA. Associations between cytokine/cytokine receptor single nucleotide polymorphisms and humoral immunity to measles, mumps and rubella in a Somali population. Tissue Antigens. 2008;72(3):211–20.
Acknowledgements
The authors would like to thank all those who participated in this study, especially Ying Song for her work on the follow-up of subjects.
Funding
This study was supported by the Twelfth National Five-Year Key Projects in infectious diseases of China (2012ZX10002001–001); Health Research Project of Jilin Province (2015Z003); China Hepatitis Prevention Foundation Project (TIAN QING Liver Disease foundation, TQGB20140137).
Availability of data and materials
The database used in this study is available upon request sent to the corresponding author.
Author information
Authors and Affiliations
Contributions
JJ, JL and JQN designed the study and provide the support. MZC, YHW were conducted the SNPs selection, genoty**, analyses and manuscript writing. SMW and YCP were conducted the DNA extraction and laboratory detection. CWa, FK and CWb were enrolled and managed the subjects from the cohort of mother-to-child transmission. All authors have approved the manuscript before submission. CWa, Chong Wang; CWb, Chuan Wang.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All participants gave written informed consent, and the signed consent was obtained from a parent or guardian on behalf of their infants. Our study was approved by the Medical Ethics Committee of the First Hospital of Jilin University (approval number 2012–098).
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Table S1. Hardy-Weinberg equilibrium for SNPs in high responders. (DOCX 14 kb)
Additional file 2:
Figure S1. Linkage disequilibrium of the SNPs in the TNF and MAPK8 genes. The color scale ranges from red to white according to r2 values (r2 values listed inside blocks). A, LD plot for TNF; B, LD plot for MAPK8. (DOCX 117 kb)
Additional file 3:
Table S2. Associations between TNF gene haplotypes and risk of low response to hepatitis B vaccines. (DOCX 13 kb)
Additional file 4:
Table S3. Associations between MAPK8 gene haplotypes and risk of low response to hepatitis B vaccines. (DOCX 13 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Cao, M.Z., Wu, Y.H., Wen, S.M. et al. Mitogen-activated protein kinase eight polymorphisms are associated with immune responsiveness to HBV vaccinations in infants of HBsAg(+)/HBeAg(−) mothers. BMC Infect Dis 18, 274 (2018). https://doi.org/10.1186/s12879-018-3166-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-018-3166-x