Abstract
Background
With an intensified aging population and an associated upsurge of informal care need in China, there is an ongoing discussion around what factors influence this need among older adults. Most existing studies are cross-sectional and do not focus on older people living in the community. Conversely, this study empirically explores the factors that affect informal care need of Chinese community-dwelling older individuals based on longitudinal data.
Methods
This study constructed panel data using the China Health and Retirement Longitudinal Research Study (CHARLS) from 2011 to 2018 for analysis. Generalized linear mixed models were used to analyze the factors affecting reception of informal care, and linear mixed models were used to analyze the factors affecting informal care sources and intensity.
Results
During the follow-up period, 7542, 6386, 5087, and 4052 older adults were included in 2011–2018, respectively. The proportion receiving informal care increased from 19.92 to 30.78%, and the proportion receiving high-intensity care increased from 6.42 to 8.42% during this period. Disability (estimate = 4.27, P < 0.001) and living arrangement (estimate = 0.42, P < 0.001) were the critical determinants of informal care need. The rural older adults reported a greater tendency to receive informal care (estimate = 0.14, P < 0.001). However, financial support from children did not affect informal care need (P > 0.05).
Conclusions
At present, there is a great demand for the manpower and intensity of informal care, and the cost of informal care is on the rise. There are differences in informal care needs of special older groups, such as the oldest-old, living alone and severely disabled. In the future, the region should promote the balance of urban and rural care service resources, rationally tilt economic support resources to rural areas, reduce the inequality of long-term care resources, improve the informal care support system, and provide a strong community guarantee for the local aging of the older adults.
Similar content being viewed by others
Background
Given the rapid growth of informal care need, which global population aging results in, it raises serious concerns about what factors influence this need and how to safeguard the sustainability of informal care system. Since 2000, China has become an aging society, progressing faster than low- and middle-income countries. According to the seventh national census in 2020, the population aged 60 years and older was up to 264 million, accounting for 18.7% of the total population in China. By 2030, the population aged 60 years and older is expected to reach 400 million, and the disabled population aged 65 years and older is estimated to reach 24.9 million [1, 2]. At the same time, informal care needs and costs for older individuals will increase significantly due to the inevitable population aging trends and highly rapid increase of the oldest-old [2].
Influenced by Confucianism’s filial culture, China relies on children and relatives to provide informal care [3]. Simultaneously, Chinese older adults tend to receive home-based care because informal care can improve their life satisfaction and quality of life [4]. Aging-in-place is to obtain continuous and comprehensive services in familiar family and community, which meets the psychological needs of the elderly and combines community-based care and home-based care. As well as the number of disabled older adults growing dramatically, there are a series of issues that make it hard for China to fully meet the care needs of older adults on multiple levels. These issues include family structure miniaturization, caregivers’ increasing financial burden, children’s continuing reduced ability to provide informal care, and a high risk of COVID-19 infection in nursing homes [5, 6]. Despite China’s substantial investment in develo** nursing facilities, many beds remain unoccupied. Furthermore, nursing homes are frequently costly and distant from family, and many older adults fear losing face by transferring to a nursing home since this may imply that their offspring are not caring enough. Thus, China is experiencing challenges of imbalance between supply and need in informal care system.
Even though informal care is an integral part of long-term care, very little is known in the existing literature about factors impacting its receipt, sources and intensity in the Chinese older population. Most countries of the Organization for Economic Cooperation and Development (OECD) also emphasize the importance of community-based long-term care services and promote informal care to delay institutional care needs among older adults [7]. Therefore, it’s highly urgent for us to look into the determinants affecting informal care need and then provide evidence for the development of informal care support system.
The importance and influencing factors of informal care
Informal care is the provision of care services by relatives, friends, neighbors, and volunteers to older people who have developed care requirements as a result of a partial or complete loss of self-care competence [8]. Confucianism, China’s primary value system, places a premium on family harmony and filial devotion. Informal care is provided to parents or spouses under this value system not only out of emotional dependence but also out of a strong sense of obligation to take on caregiving responsibilities as a family member, which has resulted in the predominance of children and spouses as informal care sources in China [9]. In terms of the factors, the location of an older adult’s living in urban or rural settings has a direct effect on their choice of care sources. Traditional values in rural areas have not changed as much as in urban areas where nuclear families are more common, so rural older people are more likely to receive informal care from their relatives than urban ones [10]. Moreover, Chinese children tend to provide financial support to their parents, which, according to Kemper’s theory [11], alters older adults’ economic status and then influences their preference for informal care sources. However, other scholars find that financial support has no effect on the informal care needs of Chinese older adults [12,13,14]. Additionally, women often bear more care responsibilities and face more enormous financial, physical, and emotional pressures than men, even though older women have greater care requirements than older men, leading to gender inequality in informal care [15,16,17]. Consequently, it is critical to improve supply capacity of care sources and refine informal care support system.
Informal care hours are used to associated with caregiver productivity and leisure time sacrifices, hence raising financial strain on families and lowering life quality. Angeles [18] found that providing temporary skilled nursing support to caregivers of older adults with dementia could reduce care hours and financial burden in OECD countries based on a systematic review of 307 studies. Wei Huang [19] predicted that informal care intensity for older adults with disabilities would increase annually from 2019 to 2028 in **njiang pastoral areas, with the highest cost of caregiving time and the fastest growth among older adults with mild disabilities. Hu [20] demonstrated that informal care sources were unequally distributed among older adults aged 80 years and older, and that oldest individuals who lived in urban areas or had with higher educational attainment received more care hours from their children. Furthermore, Hu [20] also highlighted that there were 27 million oldest adults in China and that every 1% increase in prediction accuracy could provide a more targeted allocation of care resources to 300,000 older adults. Altogether, figuring out what factors influence informal care intensity can enhance the accuracy of future prediction models. The development of prediction models can definitely promote personalized care service planning and efficient allocation of care resources.
The premise for perfecting informal care support system is to conduct a scientific and reasonable health economics evaluation of informal care, that is, to scientifically quantify the cost of care based on the assumption that informal care meets the quantity and quality of care needs of community-dwelling older adults. As key indicators of informal care needs, care sources and intensity can indirectly represent the cost of informal care, and determining their influencing factors is critical for the prediction of informal care cost. Accordingly, this study probes the influencing factors of informal care need among community-dwelling older adults in the context of Chinese characteristics, in order to provide a theoretical foundation for the improvement of informal care system. It also has implications for the construction of informal care systems in other countries.
Current study on informal care needs
Theoretical and empirical evidence suggest that based on the Andersen’s model, predisposing, enabling, and need factors induced can affect informal care need among older adults. Chinese law and filial piety culture urge children to support their parents [21]. Meanwhile increased financial assistance will further significantly enhance the utilization of professional medical, healthcare, and nursing services among older adults [22]. However, the one-child policy and urbanization have resulted in the miniaturization of family structure, and then more children no longer dwell with older adults, making informal care less accessible. Little is known about whether the influence of these factors will change over time [14]. A study in Québec revealed that men are more inclined than women to prefer informal care, while individuals with lower income are less likely to favor formal care [23]. Also, there is an absence of research that focuses on community-dwelling older people and refines their informal care need [24]. Hence, this study examines the impact of predisposing, enabling, and need factors on the informal care need of Chinese community-dwelling older adults using the longitudinal data. We hypothesize that.
-
1.
Among the predisposing factors, older adults who reside in the community, are of advanced age, female, living in rural areas, have lower levels of education, and are cohabiting or married are more likely to receive informal care compared to other types of older individuals. They require a greater number of informal care sources and higher intensity of informal care.
-
2.
Community-dwelling older adults with higher income are less likely to receive informal care and require less informal care sources and lower informal care intensity.
-
3.
Community-dwelling older adults whose children provide more financial support are less likely to receive informal care and require less informal care sources and lower informal care intensity.
-
4.
Community-dwelling older adults with more chronic diseases, greater loneliness, poorer self-rated health, or severer disability tend to receive informal care and need more informal care sources and higher care intensity.
Method
Data and sample
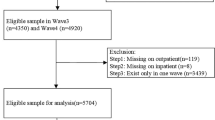
Data come from the four follow-up data for older adults in China: the China Health and Retirement Longitudinal Research Study (CHARLS), a longitudinal survey of individuals aged 45 years and older [25]. The national baseline survey was conducted in 2011–2012, with wave 2 in 2013, wave 3 in 2015, and wave 4 in 2018, with multistage sampling and probability proportional to size sampling approaches. To ensure sample representativeness, the CHARLS baseline survey covered 150 countries/districts, 450 villages/urban communities, across the country, involving 17,708 individuals in 10,257 households, reflecting the mid-aged and older Chinese population collectively. The response rate for each wave was over 80%. We constructed panel data using the four waves of the CHARLS survey. Our sample was Chinese community-dwelling older adults aged 60 years and older in 2011, with those who chose to live in nursing homes, died, or were lost to follow-up in 2013–2018 excluded. Finally, 7542, 6386, 5087, and 4052 older adults were included in 2011–2018, respectively (Fig. S1).
Measures
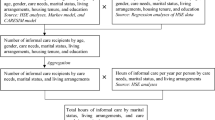
Informal care need is assessed using receipt of informal care, informal care sources, and informal care intensity [26]. Receipt of informal care was a dichotomous categorical variable comprised of the categories receiving informal care and not receiving informal care. There were five forms of care sources from which CHARLS respondents with a long-term disabled condition could choose, including care from a spouse, children, parents, other relatives, and the community, which resulted in many caregiving combinations. In this study, informal care sources referred to the number of care sources that older adults received, ranging from 0 to 5, and higher number of care sources indicated that older people need more human resource to provide assistance with ADL. Informal care intensity was measured by the number of care hours received in a week from their children, and more care hours indicated more caregiving time.
Age, education level, marital status, place of residence, economic status, internal and external care resource provision (informal family support network, provision of resources outside the home such as community-based care), and personal health status all influence older adults’ utilization of informal care services [27, 28]. As one of the most classic models for health service utilization research, Andersen’s model provides an excellent summary of inter-individual differences in the health service utilization behavior. This model is applicable to the study of long-term care, life quality of patients with chronic diseases, and health cost [29].
Under the guideline of Andersen’s model, in which an individual’s use of healthcare services and associated outcomes are viewed as a function of predisposing, enabling, and need factors, we selected independent variables. Firstly, sociodemographic traits and social structure were considered predisposing factors since they reflected an older individual’s sociocultural preferences and influence their informal care service utilization behavior. Secondly, enabling factors included the family resources available to an individual adult, which have an effect on the accessibility and availability of informal care services, which in this study referred to annual household income and regular financial support provided by children. Most researchers agree that the higher older adults’ objective purchasing power, the larger their ability to transform potential need into actual need, and the lesser their proclivity for informal care. Thirdly, the need factors were measured by objective health status and subjective health status, affecting the likelihood of seeking and utilizing informal care. The objective health status was subdivided into two components: the prevalence of chronic diseases and the independence in ADL function. The functional disability basic ADLs was divided into four health statues: healthy (0 ADL), mild disability (1–2 ADL), moderate disability (3–4 ADL), and severe disability (5–6 ADL), using the Katz Index where six ADLs were bathing, dressing, grooming, transferring, eating, and toileting [30]. The subjective health status was measured by the self-perceived loneliness and the self-perceived health based on two CHARLS entries: “I feel lonely” and “How do you feel about your health”.
Data analytic procedure
STATA version 15.1 was used for data cleaning and R version 4.1.2 was used for data analyses. Predisposing factors, enabling factors, need factors, receipt of informal care, and the most common combinations of informal care sources and the different degrees of informal care intensity in 2011–2018 were shown in Table 1. Besides, bivariate analyses were conducted to examine group differences (gender and place of residence) across all variables at the baseline (Table S1).
The Generalized Linear Mixed Models (GLMMs, models 1–2) was applied to analyze receipt of informal care among selected participants. The Linear Mixed Models (LMMs, models 3–6) was used to perform informal sources and intensity among selected participants. Both GLMMs and LMMs are designed to analyze longitudinal data due to their merits in adjusting the random effects from repeated measures on the same subject, and the within-subject and between-subject variability. During the modeling, GLMMs and LMMs could capture the effect of both time-invariant factors (e.g., gender) and the time-variant factors (e.g., residence type). The CHARLS survey timepoints (2011, 2013, 2015, 2018) was also included in the data analysis to model change in informal care need. In addition to exploring what factors determine informal care needs, we were interested in the effects of gender, residence, and financial support from children on estimates of informal care needs over time. Therefore, this study evaluated the interaction terms between these three independent variables and the survey timepoint in the GLMMs (model 2) and LMMs (model 4,6), so as to model the effects of the three primary variables on the change in informal care needs among community-dwelling older adults between 2011 and 2018 in China.
The Akaike Information Criterion (AIC) was compared to estimate the model fit, and a lower number indicates a better model fit. In addition, the full model was tested among each sub-group based on gender (female and male), and place of residence (urban and rural) to explore the group-specific associations. For the mixed models, the sampling probabilities varied exogenously by design. In this study, both the weighted and unweighted coefficients were consistent, but the weighted results tended to be less precise (e.g. larger standard errors). Therefore, it only reported the unweighted results in this paper.
Results
Descriptive statistics
At present, Chinese community-dwelling older adults have a growing need for informal care in terms of sources and intensity, while informal care costs are increasing. As shown in Table 1, and 30.58% of community-dwelling older adults received informal care, 28.64% chose informal care provided by their spouse or children, and 8.42% required high intensity care hours (30 + h/week) in 2018. It was worth noting that 90.4% of older adults required regular financial support from their children, and financial support in this study did not include hidden costs incurred by children providing informal care due to database limitations, such as medical subsidies, reduced wage income, nutrition costs, and transportation costs associated with caring for the elderly, demonstrating that informal care costs should not be underestimated [31].
Rural-urban migration is a significant characteristic of China. In the trend toward growing urbanization and urban-rural mobility, older adults in rural areas have a lower degree of economic development and retirement security than those in urban areas. According to Table 1, the proportion of community-dwelling older people in rural regions reached 82.18% in 2018, a considerable increase from the proportion in 2011, and in brief the rural retirement situation is not positive. Between 2011 and 2018, the proportion of oldest adults aged 80 years and older climbed from 8.6 to 14.16%, while the proportion of elderly people with two or more chronic conditions increased from 45.86 to 68.21%. Although the proportion of older adults in healthy status has remained around 90%, only 18.29% of all have self-perceived good health status, and the proportion of older adults receiving informal care increased from 19.92 to 30.78%, indicating that older adults, even if they live alone, have informal care needs, including life care and mental health needs.
Generalized linear mixed models and linear mixed models
Figures 1 and 2 show that age, gender, place of residence, education, living arrangement, household income, chronic conditions, loneliness, self-perceived health, and disability are associated with receipt of informal care among older individuals living in the community. Compared to the young age group (60 to 69 years old), the middle age group (70 to 79 years old) and the old age group (80 years and older) were more likely to receive informal care and had more care sources and higher care intensity, due to deteriorating physical condition in the aging process (Table 2). Older women reported more care resources and more care hours than older men (estimate = 0.08, P < 0.001 for care sources, and estimate = 1.34, P < 0.001 for care intensity). Based on the fixed effect for gender and its interaction effects with the survey timepoints, older women reported more care sources than older men during 2011–2018 (Table 2). Also, it found that rural participants got more care sources than urban participants in the longitudinal study. In addition, all models indicated that a greater level of education was associated with a decreased propensity for older adults to receive informal care, as well as a reduced need for care resources and shorter care hours. It was supported that older people living with others got more care sources than those living alone (Figs. S1 and S2). However, it did not find marital status could influence informal care need of older adults in full models.
Compared to older adults without income, those who had higher income were less likely to receive informal care (¥1 to ¥19,999: estimate=−0.37, P < 0.001;¥20,000 and more: estimate=−0.14, P < 0.001). Although, there was no evidence to support the interaction between financial support from children and the survey timepoints. Moreover, need factors are predictive of informal care needs during 2011–2018, for example, where it is observed that self-rated fair health status (estimate = 5.10, P < 0.001) and self-rated bad health status (estimate = 1.87, P < 0.05) are associated with higher levels of informal care intensity. Refer to the supplementary figures for detailed results.
Discussion
Our findings further show that the factors influencing informal care needs for community-dwelling older adults in China based on CHARLS data from 2011 to 2018. The study demonstrated an increasing trend of informal care needs among community-dwelling older adults as they age and experience more functional disabilities. This trend holds implications for long-term care policies internationally, as populations globally are experiencing rapid population aging. Other countries should monitor changing dynamics of elderly care needs over time. Place of residence (urban vs. rural) and economic status were found to influence older adults’ choices of informal care sources. A balanced consideration of diverse regional and income-level needs is warranted when allocating care resources across populations. Family structural changes have weakened children’s capacity for elderly care. Strengthening community support is vital to compensate for vulnerabilities in family caregiving systems, an issue exacerbated by ongoing transformation of family structures worldwide. Gender emerged as an impact factor, with women tending to have greater care requirements while primarily shouldering care responsibilities, potentially leading to caregiver burden. Other nations must also address gender inequities in elderly care provision and outcomes. Sustaining an equitable and efficient informal care support system necessitates a holistic perspective accounting for multiple influencing factors. This holds lessons for develo** sustainable elderly care models to meet basic living needs while alleviating family caregiver strain, crucial objectives for aging societies globally.
For Hypothesis 1, our findings support that age, gender, place of residence, education, and living arrangement were associated with informal care need among older adults. Among them, those who are older, female, live in rural areas, have higher education levels, and live alone have higher care resource and intensity needs. Interestingly, the association between marital status and informal care need was not established. Aging is associated with a loss of muscle mass, leading to frailty and functional disability, making older adults require daily life support [33]. In the Chinese context, women tend to assume caregiving roles and take on more physical and mental stress [14]. During the pandemic, it has been reported that female informal caregivers are more negatively affected than male informal caregivers, as indicated by higher levels of anxiety and lower quality of life [34]. It is unequal that older women have higher levels of informal care needs and experience a more extended period of end-of-life disability than older men, but they have higher caregiving burdens and more caregiving responsibilities than older men [41,42,37]. In rural areas, community-based care facilities are poorly developed, the number of nursing homes is low, and their cost is beyond the affordability of rural households. Moreover, older adults have less access to informal care when their children live farther away [38]. Thus, place of residence and living arrangements determine the availability of informal care. Older adults with lower educational attainment tend to have lower abilities to pay and are more likely to choose lower-cost informal care when informal care is needed [14].
This study also supports Hypothesis 2, that community-dwelling older adults with lower income were more likely to receive informal care, although the effect of income on informal care intensity was not supported. Higher-income level has been negatively associated with the receipt of informal care among older adults [39, 40]. However, Hypothesis 3 was not supported, that financial support from children affects informal care needs. In China, informal care cost is usually underestimated, and the hidden financial loss of children is always ignored, because it is considered children’s duty to support their parents [31, 32, 41].
Our findings also support Hypothesis 4, that need factors were the primary force behind informal care need, including chronic conditions, self-perceived loneliness, self-perceived health, and disability. It is shown that older persons with a poorer health status are more likely to receive informal care with greater care resources and greater care intensity, which is consistent with the findings of other researchers [3, 26, 42].
The findings of this study contribute to a growing body of research identifying factors that determine receipt, sources, and intensity of informal care. This longitudinal study demonstrates that different dimensions of informal care need are affected by different factors. This study points to the need for innovative community-based programs that establish daycare centers, give daily life support to older people, and teach children professional nursing skills, especially older women and female informal caregivers [8]. What is more, there are urban-rural differences in both the supply and need of informal care due to the dual socioeconomic structure of the urban-rural divide [43]. Policymakers should consider the differences in income, perceptions and service provision between urban and rural older people when develo** policies for improving informal care support systems, such as constructing community-based service facilities, develo** teams of nursing professionals, and expanding long-term care insurance coverage. Additionally, informal care costs need to be taken seriously, with uniform quantitative evaluation indicators and financial subsidies in different proportions according to the actual situation of urban and rural areas and special populations [31, 44]. It is recommended that the subsidies include both the elderly and informal caregivers. This aims to improve the material conditions of older people and stimulate informal caregivers to take care of older people, thus alleviating the pressure of caregiving on families and maintaining the sustainability of informal care system.
The identified factors associated with informal care needs among community-dwelling older individuals provide valuable insights into the potential determinants of informal care requirements in different cultural and social-economic contexts. Understanding these factors can help inform policies and interventions aimed at supporting informal caregivers and meeting the care needs of older adults in various countries, especially in develo** countries. Furthermore, recognizing the vital role of informal caregivers in the healthcare system is crucial across nations. Informal caregivers play a significant role in providing essential care and support to older adults. Their contribution to the health services industry should be acknowledged and supported through appropriate policies, resources, and recognition of their valuable work. By understanding the dynamics of informal care, countries can work towards creating sustainable and comprehensive support systems that enhance the health and quality of life of older adults while recognizing and supporting the invaluable role of informal caregivers.
Conclusions
This study revealed that the factors including age, gender, place of residence, education, living arrangement, household income, chronic conditions, loneliness, self-perceived health, and disability are associated with informal care need among community-dwelling older individuals in China from 2011 to 2018. Older adults who are female, the oldest, living rural, living alone, having lower income, feeling lonely, and severely disabled require more informal care need. Informal caregivers are the backbone of the healthcare system to the extent that their contribution to health services industry is essential. Further study is needed to forecast the trajectory of informal care need among community-dwelling older adults, as well as development and implement of informal care support system aimed at fostering better health and well-being.
Of course, this study still has certain limitations. Firstly, we were limited by the availability of sample size, and therefore, we were unable to address the issue of regional heterogeneity. Secondly, there might be some potential influencing factors that we did not include. Thirdly, since the data is not first-hand information, the selection bias and other potential random errors in sample selection weaken our inference to a certain extent. Lastly, due to the self-report nature of the questionnaire collection, there may also be some biases in the data collection process.
Data availability
The datasets analyzed during the current study are publicly available in the CHARLS repository at http://charls.pku.edu.cn/en.
References
Sun R, Cao H, Zhu X, Liu J-P, Dong E. Current aging research in China. Protein Cell. 2015;6(5):314–21.
Zeng Y, Chen HS, Wang ZL, Land KC. Implications of changes in households and living arrangements for Future Home-Based Care needs and costs for disabled elders in China. J Aging Health. 2015;27(3):519–50.
Zhang L, Shen S, Guo Y, Fang Y. Forecasting future demand of nursing staff for the Oldest-Old in China by 2025 based on Markov Model. Int J Health Policy Manag 2021.
Qi X. Filial Obligation in Contemporary China: evolution of the culture-system. J Theory Soc Behav. 2015;45(1):141–61.
Shen S, Zhang L, Fang Y. Predicting demand of informal care for disabled elderly in China–a review on research progress. Chin J Public Health. 2022;38(6):821.
Reyné B, Selinger C, Sofonea MT, Miot S, Pisoni A, Tuaillon E, Bousquet J, Blain H, Alizon S. Analysing different exposures identifies that wearing masks and establishing COVID-19 areas reduce secondary-attack risk in aged-care facilities. Int J Epidemiol 2021:dyab121.
Organization WH. WHO guidelines on integrated care for older people (ICOPE). Geneva: WHO World Health Organization; 2017.
Cascella Carbó GF, García-Orellán R. Burden and gender inequalities around Informal Care. Invest Educ Enferm 2020, 38(1).
Hu B, Li L. The Protective effects of Informal Care receipt against the progression of functional limitations among Chinese Older people. J Gerontol B Psychol Sci Soc Sci. 2020;75(5):1030–41.
Silverstein M, Cong Z, Li S. Intergenerational transfers and living arrangements of older people in rural China: consequences for psychological well-being. J Gerontol B Psychol Sci Soc Sci. 2006;61(5):256–66.
Kemper P. The use of formal and informal home care by the disabled elderly. Health Serv Res. 1992;27(4):421–51.
Bo H, Sai M. Receipt of informal care in the Chinese older population. Ageing Soc. 2018;38(4):766–93.
Wang Y, Yang W, Avendano M. Income-related inequalities in Informal Care: evidence from the Longitudinal Healthy Longevity Survey in China. J Gerontol B Psychol Sci Soc Sci. 2021;76(8):1691–6.
Hu B, Ma S. Receipt of informal care in the Chinese older population. Ageing Soc. 2018;38(4):766–93.
Pinquart M, Sörensen S. Associations of stressors and uplifts of caregiving with caregiver burden and depressive mood: a meta-analysis. J Gerontol B Psychol Sci Soc Sci. 2003;58(2):P112–128.
Pinquart M, Sörensen S. Gender differences in caregiver stressors, social resources, and health: an updated meta-analysis. J Gerontol B Psychol Sci Soc Sci. 2006;61(1):P33–45.
Ma J, Yang H, Hu W, Khan HTA. Spousal Care Intensity, Socioeconomic Status, and Depression among the older caregivers in China: a study on 2011–2018 CHARLS Panel Data. Healthc (Basel) 2022, 10(2).
Angeles RC, Berge LI, Gedde MH, Kjerstad E, Vislapuu M, Puaschitz NG, Husebo BS. Which factors increase informal care hours and societal costs among caregivers of people with dementia? A systematic review of resource utilization in dementia (RUD). Health Econ Rev. 2021;11(1):37.
Huang W. Time cost prediction of informal care for the elderly with disability at home in **njiang Animal husbandry area. Master Shihezi University; 2020.
Hu B. Trajectories of informal care intensity among the oldest-old Chinese. Soc Sci Med. 2020;266:113338.
Zhan HJ, Montgomery RJ. Gender and elder care in China: the influence of filial piety and structural constraints. Gend Soc. 2003;17(2):209–29.
Hu B, Shin P, Han E-j, Rhee Y. Projecting Informal Care demand among older koreans between 2020 and 2067. Int J Environ Res Public Health. 2022;19(11):6391.
Lee K, Revelli M, Dickson D, Marier P. Who cares? Preferences for formal and Informal Care among older adults in Québec. J Appl Gerontol. 2022;41(1):227–34.
Pickard L, Wittenberg R, Comas-Herrera A, Davies B, Darton R. Relying on informal care in the new century? Informal care for elderly people in England to 2031. Ageing Soc. 2000;20(6):745–72.
Zhao Y, Strauss J, Chen X, Wang Y, Gong J, Meng Q, Wang G, Wang H. China Health and Retirement Longi- Tudinal Study Wave 4 user’s guide. National School of Development, Peking University; 2020.
Hu B. Projecting future demand for informal care among older people in China: the road towards a sustainable long-term care system. Health Eco Policy Law. 2019;14(1):61–81.
Wang Y, Yang W. Does receiving Informal Care lead to Better Health Outcomes? Evidence from China Longitudinal Healthy Longevity Survey. Res Aging 2021:1640275211052834.
Kjaer AA, Siren A. Formal and informal care: trajectories of home care use among Danish older adults. Ageing Soc. 2020;40(11):2495–518.
Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Q. 1973;51(1):95–124.
Palmer RF, Espino DV, Dergance JM, Becho J, Markides K. The role of physical activity and diabetes status as a moderator: functional disability among older Mexican americans. Age Ageing. 2012;41(6):752–8.
Chen L, Fan HL, Chu LL. The hidden cost of informal care: an empirical study on female caregivers’ subjective well-being. Soc Sci Med. 2019;224:85–93.
Hu B, Wang J. Unmet long-term care needs and depression: the double disadvantage of community-dwelling older people in rural China. Health Soc Care Community. 2019;27(1):126–38.
Zhang J, Zhao A, Wu W, Ren Z, Yang C, Wang P, Zhang Y. Beneficial effect of Dietary Diversity on the risk of disability in activities of Daily living in adults: a prospective cohort study. Nutrients. 2020;12(11):3263.
Zwar L, König H-H, Hajek A. Gender Differences in Mental Health, Quality of Life, and Caregiver Burden among Informal Caregivers during the Second Wave of the COVID-19 Pandemic in Germany: A Representative, Population-Based Study. Gerontology 2022:1–14.
Li QX, Zhang HF, Zhang M, Li T, Ma WX, An CX, Chen YM, Liu S, Kuang WH, Yu X et al. Prevalence and risk factors of anxiety, Depression, and sleep problems among caregivers of people living with neurocognitive disorders during the COVID-19 pandemic. Front Psychiatry 2021, 11.
Kwak M, Kim B, Lee H, Zhang J. Does gender matter in the receipt of Informal Care among Community-Dwelling older adults? Evidence from a cross-national comparative study across the United States, South Korea, and China. J Gerontol B Psychol Sci Soc Sci. 2021;76(Suppl 1):64–s75.
Smith AK, Walter LC, Miao Y, Boscardin WJ, Covinsky KE. Disability during the last two years of life. JAMA Intern Med. 2013;173(16):1506–13.
Fu YY, Chui EWT. Determinants of patterns of need for Home and Community-Based Care services among Community-Dwelling Older people in Urban China: the role of living arrangement and filial piety. J Appl Gerontol. 2020;39(7):712–21.
Lera J, Pascual-Sáez M, Cantarero-Prieto D. Socioeconomic inequality in the Use of Long-Term Care among European older adults: an empirical Approach using the SHARE Survey. Int J Environ Res Public Health 2020, 18(1).
Larsson K, Silverstein M. The effects of marital and parental status on informal support and service utilization: a study of older swedes living alone. J Aging Stud. 2004;18(2):231–44.
Beckman AL, Gondi S, Barnett ML. The hidden costs of moving Care Home. Am J Manag Care. 2021;27(3):E64–5.
Cai JL, Zhang L, Guerriere D, Coyte PC. The determinants of the intensity of home-based informal care among cancer patients in receipt of home-based palliative care. Palliat Med. 2021;35(3):574–83.
Chen X, Su D, Chen X, Chen Y. Effect of informal care on health care utilisation for the elderly in urban and rural China: evidence from China health and retirement longitudinal study (CHARLS). BMC Health Serv Res. 2022;22(1):271.
Alwin J, Karlson BW, Husberg M, Carlsson P, Ekerstad N. Societal costs of informal care of community-dwelling frail elderly people. Scand J Public Health. 2021;49(4):433–40.
Acknowledgements
We are grateful to the National Natural Science Foundation of China, the Science and Technology Innovation Think Tank Youth Program and the Social Science Foundation of Fujian Province, China for their support and to all the teachers and students at the Centre for Health Economics and Policy Research, **amen University for their help.
Funding
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute. This study was supported by the National Natural Science Foundation of China (No. 81973144), the Science and Technology Innovation Think Tank Youth Program (No. 2021ZZZLFZB1207146), and the Social Science Foundation of the Fujian Province, China (FJ2022C047).
Author information
Authors and Affiliations
Contributions
LZ and SS planned the study, performed all statistical analyses, and drafted the manuscript. LZ and WZ assisted with statistical analyses and contributed to revising the manuscript. YF supervised and critically revised the manuscript. All authors have read and approved the final version of the manuscrip.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The current study is a secondary analysis of the de-identified China Health and Retirement Longitudinal Study (CHARLS) public data. The protocol of the CHARLS was approved by the Ethical Review Committee at Peking University. The ethical approval number was IRB00001052–11015. Ethics approval for the use of CHARLS data was obtained from the University of Newcastle Human Research Ethics Committee (H-2015-0290). Written informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, L., Shen, S., Zhang, W. et al. What determines informal care need among community-dwelling older adults in China? Results from a longitudinal study. BMC Geriatr 24, 597 (2024). https://doi.org/10.1186/s12877-024-04843-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-04843-3