Abstract
Background
Good self-management behaviors in patients with knee osteoarthritis can improve disease awareness, treatment effectiveness, quality of life, and reduce medical costs. However, there is a paucity of studies focusing on patients with knee osteoarthritis. Therefore, the purpose of this study was to explore the mediating effect of self-efficacy on aspects of social support and self-management behaviors in this population.
Methods
This study employed a cross-sectional design and convenience sampling to survey patients with knee osteoarthritis in an outpatient department of a regional hospital in northern Taiwan from February 22, 2021, to April 15, 2021. The inclusion criteria for patients were (1) those diagnosed by a physician with knee osteoarthritis and (2) who could communicate in Chinese or Taiwanese. Participants were asked to complete a demographic questionnaire, the Arthritis Self-Efficacy Scale (ASE), the Inventory of Socially Supportive Behavior (including enacted support and perceived social support), and the Arthritis Self-Management Assessment Tool (ASMAT). In addition, the Kellgren-Lawrence Grading Scale was obtained from a chart review. Data were analyzed with descriptive statistics, t-test, one-way analysis of variance, Pearson product-moment correlation, and mediation analysis.
Results
A total of 140 patients met the inclusion criteria. The mean age of participants was 70.21 ± 10.84years; most (73.6%) were female. The mean total score of the ASMAT was 64.27 ± 14.84. Scores for the ASE, enacted support, and perceived social support were significantly positively correlated with ASMAT (all p < .001). The standardized coefficient for total effect and direct effect of perceived social support on ASMAT was 0.899 (p < .001) and 0.754 (p < .05), respectively. After introducing the ASE into the model, the indirect effect was 0.145 (p < .05), which indicated that ASE had a partial mediating effect on the relationship between perceived social support and ASMAT.
Conclusion
Our findings might suggest that perceived social support indirectly affected ASMAT through ASE. Therefore, interventions designed to increase self-efficacy and social support could enhance self-management behaviors for patients with knee osteoarthritis.
Similar content being viewed by others
Background
Knee Osteoarthritis (KOA) is one of the most common chronic diseases, resulting in poor prognosis of physical function and disability. According to the United States Centers for Disease Control and Prevention, approximately 32.5 million adults are diagnosed with degenerative arthritis each year, among which 62% are women [1]. It is estimated that, by 2040, about half of the adults over the age of 65 in the United States will have some degree of arthritis, of which the knee joint will be the most common site of degeneration [2]. The symptoms of osteoarthritis usually are exacerbated with aging, which in turn causes a heavy burden on individuals and society. In particular, patients affected by severe KOA usually report joint pain with a progressive loss of function and subsequent disability, which results in a reduction of health-related quality of life and increased depression [3, 4].
According to 2019 statistics published by Taiwan’s National Health Insurance (NHI) program on medical utilization [5], the number of KOA patients treated in outpatient/emergency clinics was about 863,000 and, on average, 1 in 10 individuals were diagnosed with KOA. The NHI program reimburses healthcare providers on a point system, rather than absolute dollars, to standardize payments over time [18] found that self-efficacy and social support have a significant direct impact on cancer patients’ disease self-management, and social support can also have an indirect impact on self-management via self-efficacy and co** styles. Chan et al. [14] reported social support improved self-efficacy in patients with diabetes, thereby improving self-care behaviors. Oh and Ell [19] evaluated the association between changes in social support and self-management in patients with diabetes, which showed changes in social support were only related to self-efficacy and did not directly affect self-management. Therefore, social support might only function as a buffer in eliminating social and disease stressors.
Self-efficacy is affected by the variability of internal and external environmental resources. Most studies have suggested that self-efficacy is the essential factor that affects self-management behaviors [20]. Some studies have focused on the effect of social support and self-efficacy [14, 21] and found that social support helps patients face life challenges caused by diseases with greater confidence, thereby enhancing healthy behaviors.
Few studies have investigated the relationship between self-efficacy, social support, and self-management in patients with KOA, which are limited to exploring the effect of self-efficacy on self-management of pain control and physical activity [22,23,24], as well as peer support for self-management behaviors [25]. Therefore, underlying mechanisms for associations between social support, self-efficacy and overall self-management behaviors remains unclear. In addition, there is little research on how different dimensions of social support affect self-efficacy and self-management. Taiwan’s comprehensive NHI system makes it easy to quickly seek medical treatment and receive medical services when patients feel unwell or have health concerns. Due to the differences in medical care-seeking behaviors and medical resources, the self-management behaviors of Taiwanese patients may differ compared with other countries. Understanding the factors associated with self-management behaviors from the perspective of patients with KOA in Taiwan will help fill the existing knowledge gap.
Therefore, this study categorized social support dimensions into enacted support and perceived social support to explore the association between self-efficacy, social support, and self-management behavior, as well as the mediating role of self-efficacy. It is hoped that the findings of this study can provide a reference for designing appropriate care plans and measures in the future to improve the self-management behaviors and quality of life of patients with KOA.
Methods
Study design and setting
This was a cross-sectional study reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) recommendations [26]. The study was performed in an outpatient department of a regional hospital in northern Taiwan from February 22, 2021, to April 15, 2021.
Participants and procedure
Patients with KOA were recruited by convenience sampling from an outpatient department of a regional hospital in northern Taiwan. The inclusion criteria for patients were (1) a diagnoses by a physician as having KOA and (2) could communicate in Chinese or Taiwanese. Patients were excluded for any of the following: (1) the presence of non-degenerative arthritis in the knees; (2) diagnosed with dementia or communication disorders; and (3) those who underwent any inpatient surgery within the past six months.
The sample size was estimated using G-power version 3.1, assuming a power of 0.80, and the α level set at 0.05. The effect size was set at a minimum value of 0.19 in reference to the correlation coefficient of 0.19 between social support and self-management behaviors in patients with rheumatoid arthritis [27]. The research framework of this study included nine independent variables and an estimated sample size of 92.
The study objective, research process, and interviewees’ rights were explained to potential participants in detail after initiating contact. After providing informed consent, participants were asked to fill out questionnaires; if they were unable to complete the questionnaires due to illiteracy, blurred vision, or other factors, the investigator read the questions one by one to the participant and then recorded the participant’s choice for the answer. The questionnaires were coded to maintain anonymity and protect patient privacy.
Outcome variables
The primary outcome was self-management behaviors. We used the Arthritis Self-Management Assessment Tool (ASMAT), developed by Oh et al. [11], to evaluate the self-management behaviors of patients with KOA. The scale has three core components about behaviors related to disease self-management: medical, which is comprised of 10 questions regarding adherence to treatment; behavior, which is comprised of 13 questions regarding adoption of general and healthy behaviors; and psycho-emotional, which is comprised of 9 questions about managing arthritis-induced depression, emotional problems and stress. Participants answer each question on a 4-point Likert scale from “never” = 0 points to “always” = 3 points. Total scores range from 0 to 96 points; higher scores indicate more self-management behaviors. The Cronbach’s α of the original scale was 0.88. The Chinese version of the scale was independently translated by two bilingual researchers from different fields and subsequently back translated and revised. The content validity of the revised scale was tested by clinical healthcare experts, and the overall CVI of the questionnaire was 0.97. The Cronbach’s alpha was 0.91 for the overall self-management scale and 0.86, 0.73, and 0.89 for various scales of medical management, behavior management, and psycho-emotional management, respectively.
The secondary outcomes were the Arthritis Self-Efficacy (ASE) and the socially supportive behaviors. The Arthritis Self-Efficacy (ASE) scale, developed by Lorig et al. [9], was used to assess participant’s level of confidence toward practicing specific behavioral goals. The 20-item scale has three components: self-efficacy for pain (5 items), self-efficacy for physical function (9 items), and self-efficacy for other symptoms (6 items). Each item is phrased as a statement and a visual analogue scale is used for the participant’s response, which ranges 0 points for “very uncertain” to 10 points for “very certain”; the total score is 200 points, with higher scores indicating greater self-efficacy. This study used the ASE translated into Chinese by Chen [28] and validated with 129 patients with rheumatoid arthritis in Taiwan. The Cronbach’s alpha for the total scale was determined to be .93, and the Content Validity Index (CVI) was .95 [28]. The Cronbach’s alpha for this study was .94.
Socially supportive behaviors were assessed with the 70-item Inventory of Socially Supportive Behavior (ISSB) instrument, developed by Barrera [29] and translated and edited for use in Taiwan by Yeh [30]. The ISSB is a self-report instrument developed to evaluate an individual’s satisfaction with actual enacted support (60 items) and perceived social support (10 items) provided by six social support networks: spouses, children, relatives, friends, hospital friends, and healthcare professionals. The subscale of enacted support is comprised of 10 questions each for the six support networks about the amount and frequency of support provided. Each question is scored on a 3-point Likert scale: 1 point = never; 2 points = occasionally; and 3 points = often. If any social support network is missing, the item is not scored. Scores range from 0 points, indicating no social support to 180 points indicating high social support from all six networks.
Potential confounders
Potential confounders included participants’ characteristics and Level of knee degeneration. Demographic characteristics were collected with a questionnaire, which included gender, age, educational level, presence of other chronic diseases, the age at which the disease was diagnosed, and whether the patient had received intra-articular injection therapy, surgery, physical therapy, or analgesic medications. Body mass index (BMI) was calculated by the investigator by measuring the participant’s height and weight. Level of knee degeneration was based on the Kellgren-Lawrence Grading Scale (K-L GS), which was obtained from review of the patient’s chart. The K-L GS was evaluated by an orthopedic physician using X-ray images and data extracted from medical records. The degree of knee degeneration is then categorized into four levels, from 0 (not severe) to 4 (severe). The higher the level, the more severe the degeneration [31].
Statistical Analysis
Data processing and analysis were performed using software package SPSS for Windows version 21.0. Statistical analysis methods included descriptive statistics (mean ± SD (standard deviation) and frequency), t-test, one-way analysis of variance, and Pearson product-moment correlation. We employed the SPSS PROCESS procedure to test the mediation model with the model-4 setup. The bias-corrected bootstrap** procedure for 5,000 repeated samplings was used to determine the 0.95 confidence interval (CI). If the CI did not contain zero, the mediating effect was considered significant; if the CI contained 0, the mediating effect was not considered significant [32].
Results
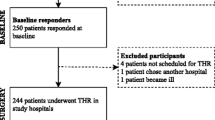
During the study period, 158 potentially eligible patients who met the inclusion criteria were seen in the outpatient clinic and 155 of those were contacted. Among them, 15 patients declined to participate in the study due to their unavailability; consequently, 140 patients who met the inclusion criteria participated in this study (Fig. 1).
Demographic and clinical characteristics of participants are shown in Table 1. The mean age of participants was 70.21 ± 10.84 years, and most were female (73.6%). The mean BMI was 25.37 ± 4.11 kg/m2, mean time since diagnosis was 5.94 ± 5.59 years and most had a grade of level 2 (48.6%) or level 3 (31.4%) for knee degeneration based on the K-L GS. More than 90% of participants had received an intra-articular injection, 35.7% had received knee joint surgery, 40% had received physical therapy, and 44.3% were taking analgesics.
Scores for the self-report instruments are shown in Table 2. The mean total score on the ASMAT was 64.27 ± 14.84 points, suggesting a moderate level of self-management. We used the metrics of % Max for component scores on the ASMAT to determine the highest and lowest overall score, which was highest for medical management (70.17%) and lowest for behavior management (64.64%). The scores on the ASE ranged from 21 to 200 points, with a mean score of 145.90 ± 39.77 points. Metrics indicated the component of functional self-efficacy was the highest score (79.7%), and pain control self-efficacy was lowest (63.14%). The mean score for perceived social support was 26.02 ± 4.58 points, indicating perceived level of social support was high (range = 12–30). The mean score for perceived enacted support was 93.92 ± 27.47 points, indicating social support from the six support networks was moderate (range = 0–180)
Correlation analysis between demographic characteristics and the ASMAT indicated educational level was significantly correlated (F = 14.28, p < .001). Post-hoc analysis showed correlations were lower for participants with an educational level ≤ elementary school, compared with participants who were junior/senior high school graduates, and ≥ college. Participants with other chronic diseases had a significantly lower self-management behavior score compared with those without other chronic diseases (t = 2.37, p < .01). Age (r = − .23, p < .01) and the level of arthritis (r = − .276, p = .001) were significantly negatively correlated with self-management behaviors, indicating that older age and greater severity of osteoarthritis was a barrier to self-management behaviors. Self-efficacy scores were positively correlated with self-management behaviour scores (r = .446, p < .001). In addition, both enacted support and perceived social support scores were positively correlated with total scores for self-management behaviors (r = .438, p < .001 and r = .310, p < .001, respectively), indicating the better the self-efficacy, enacted support, and perceived social support, the higher the scores for self-management behaviors (Table 3).
This study used the PROCESS macro version by Hayes [33] to analyse the mediating effect between self-management behaviors and perceived and enacted social support (Tables 4 and 5, respectively). Path 1 shows perceived social support (β = 0.90, p < .001, Table 4) and enacted support (β = 0.22, p < .001, Table 5) had significant explanatory power for self-management behaviors after controlling for demographic variables. Path 2 shows perceived social support had significant explanatory power for self-efficacy (β = 1.45, p = .046, Table 4); however, enacted support had no significant effect on self-efficacy (β = 0.12, p = .315, Table 5). Path 3 (Table 4) considers the explanatory power of both perceived social support and self-efficacy (β = 0.76, p = .003 and β = 0.10, p = .001, respectively) for self-management behavior as well as the explanatory power of enacted support and self-efficacy (β = 0.21, p < .001 and β = 0.10, p < .001, respectively; Table 5). In summary, all three variables had significant explanatory power for self-management behaviors.
The standardized coefficient for the total effect and direct effect of perceived social support on self-management behavior was 0.899 (95% CI: 0.390, 1.410) and 0.754 (95% CI: 0.255, 1.254), respectively (Table 4). After introducing the mediator variable of self-efficacy into the model, the standardized coefficient of the indirect effect was 0.145 (95% CI: 0.002, 0.360), which was statistically significant, indicating that self-efficacy had a partial mediating effect, accounting for 16.13% of the total effect. As shown in Table 5, the standardized coefficient for the total effect of enacted support on self-management behavior was 0.217 (95% CI: 0.139, 0.296), and the direct effect was 0.205 (95% CI: 0.130, 0.280). After introducing the mediator variable of self-efficacy into the model, the standardized coefficient of the indirect effect was 0.012 (95% CI: − 0.013, 0.040), which was not significant, indicating that enacted support directly affected self-management behaviors with no mediating effect from self-efficacy.
Discussion
This study aimed to explore the mediating effect of self-efficacy on aspects of social support and self-management behaviors in patients with KOA. Our findings showed enacted support, perceived social support and self-efficacy, were significantly positively correlated with self-management behaviors for individuals with KOA. Self-efficacy had a partial mediating effect on the relationship between perceived social support and self-management behaviors. We also found older age and greater severity of KOA were barriers to self-management behaviors.
Scores on the ASMAT indicated participants in our study had a moderate level of self-management behaviors, with scores for medical management highest, and behavior management lowest. The content of the medical management component included questions about whether the participant saw a physician on a regular basis, was compliant about taking prescribed medications, and discussions of treatment plans and medical decisions with healthcare professionals, which suggests participants took responsibility for managing their personal healthcare. The component of behavior management included questions about whether the participant sought healthcare information, attended disease and healthcare seminars, and used non-prescription treatments to reduce pain, such as massage. The low scores for behavior management suggest this area of healthcare was not an important part of participants’ self-management. Due to the successful implementation of the NHI system in Taiwan, the public has easy access to a doctor, low medical expenses, and no barriers to periodic follow-ups or obtaining a prescription, which may explain why medical self-management behaviors scored high. At the same time, the NHI system may explain the low scores for behavior management. The easy access to healthcare allows individuals to seek medical treatment as their first choice when addressing health problems, thus they may not consider daily self-management behaviors to be as important.
Patient age, education level, comorbidities, and the severity of arthritis were significantly associated with self-management behaviors, which echo previous research. Older patients may have reduced muscle strength and joint mobility due to aging. As the prevalence of multiple chronic diseases increases with age, people often lower their expectations of their ability to perform physical activities, which can result in decreased self-efficacy that subsequently affects self-management behaviors [15]. Kang et al. [12] indicated that the self-management of patients with multiple chronic diseases is relatively complex, resulting in poor self-management behaviors. Patients with severe joint degeneration may be more dependent on osteoarthritis medications and thus have poorer self-management behaviors [34]. Consistent with previous research findings, this study found that patients with higher education levels were more likely to actively seek disease-related knowledge and resources and discuss their conditions and treatment plans with healthcare professionals [35].
In this study, self-efficacy was positively correlated with scores for self-management behaviors, implying that when patients had higher confidence toward performing self-management activities, they were more likely to implement self-management behaviors. Previous correlation studies on patient groups, such as those with diabetes and coronary heart disease, had similar results [21, 36]. Improving self-efficacy is an important intervention in clinical care. Healthcare workers can provide information on arthritis care and individualized guidance, encourage and assist in solving individual problems, and create successful experiences related to implementing self-management behaviors [15]. Patients can also be encouraged to join supportive groups and utilize observational learning and vicarious learning skills to discuss health problems caused by disease and co** methods to reduce anxiety or negative emotions [37]. Patients can also discuss specific methods that can successfully relieve pain and delay disability to help improve self-efficacy and enhance self-management behaviors.
Our findings are in line with previous research showing that social support is positively correlated with self-management behaviors [14, 38]. Healthcare workers can formally play a social support role by partnering with patients to provide care information about the disease, elevate their sense of support, and integrate social support into the self-management program curriculum. In addition, healthcare workers can provide patients with an appropriate environment to discuss their conditions or problems, such as follow-ups by phone or software apps to ensure that patients have a supportive environment, a good social network, and support resources. All these measures can promote patients’ physical activities and develop self-management behaviors, which also help reduce the frequency of doctor visits and encourage the efficient use of healthcare resources to reduce healthcare costs and achieve self-management goals [14, 39].
This study investigated the role of self-efficacy in the relationship between enacted support, perceived social support, and self-management behaviors. The results showed that self-efficacy partially mediated the relationship between perceived social support and self-management behaviors but had no significant mediating effect on the relationship between enacted support and self-management behaviors. Perceived social support and self-efficacy are intrinsic psychological resources that enable individuals to regulate their thought process and behavior. According to the self-efficacy theory, an individual’s self-efficacy for healthy behavior may depend in part on psycho-emotional states. A recent study found a positive motivation for achievement influenced older adults’ self-efficacy in their willingness to be reemployed [40]. By contrast, patients troubled by pessimism and emotions often lose confidence in their ability to perform self-management behaviors [37]. On the other hand, perceived social support may be influenced by self-efficacy through psychological factors, enabling patients to overcome their problems by receiving encouragement and emotional and information support. Therefore, greater perceived social support can strengthen personal self-efficacy and indirectly enhance self-management behaviors [14]. Conversely, when a patient’s perceived social support is insufficient, their confidence in self-management behavior may decrease [21]. In this study, enacted support had a direct effect on self-management behavior without the mediation of self-efficacy. Healthcare workers s are one of the important social support networks for patients, and they can put forth practical action to support and enhance patients’ self-management behaviors. By establishing partnerships with patients, they can also strengthen patients’ perceived social support. They can employ strategies that increase self-efficacy to achieve the goal of enhancing patients’ self-management behaviors and improving quality of life.
Study Limitations
Due to time and labor considerations, all participants were recruited from one regional hospital in Taipei City. Therefore, the findings of this study may not be used to infer the self-management behaviors of patients with KOA at different medical institutions in Taiwan. The cross-sectional design of this study only revealed the self-management status of patients at a particular point in time; however, KOA is a long-term chronic disease with a high risk of disability. Thus, it is suggested that use of the International Classification of Functioning, Disability, and Health (ICF) [41] and tracking the long-term changes in self-management behaviors of individuals with KOA be considered for future research.
Conclusion
The results of this study support the association between self-efficacy, social support, and self-management behavior and demonstrated that perceived social support indirectly affected self-management behavior through self-efficacy. In terms of clinical practice, healthcare workers should first evaluate patients’ self-management behaviors and focus on social support and self-efficacy intervention strategies to provide the necessary social support and resources in any insufficient areas. Physicians should help increase patients’ perceived social support and self-efficacy and promote the implementation of self-management behaviors. Enacted support directly affected self-management behaviors without the mediating effect of self-efficacy. Healthcare workers are one of the essential social support networks for patients. They can provide active support to enhance patients’ self-management behaviors. By establishing partnerships with patients, healthcare workers can strengthen patients’ perceived social support and implement strategies designed to improve self-efficacy to achieve the goals of enhancing patients’ self-management behaviors and improving their quality of life.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Centers for Disease Control and Prevention: Arthritis-related statistics. https://www.cdc.gov/arthritis/data_statistics/arthritis-related-stats.htm#projected (2018). Accessed 13 Nov 2020.
Gunnar BJ, Sigurd H, Kenneth L, Michelle CC, Miriam C, Robert M, et al. The impact of musculoskeletal disorders on Americans: opportunities for action. 3rd ed. Bone and Joint Initiative; 2016.
De Sire A, Stagno D, Minetto MA, Cisari C, Baricich A, Invernizzi M. Long-term effects of intra-articular oxygen-ozone therapy versus hyaluronic acid in older people affected by knee osteoarthritis: a randomized single-blind extension study. J Back Musculoskelet Rehabil. 2020. https://doi.org/10.3233/bmr-181294.
Zheng X, Wang Y, ** X, Huang H, Chen H, Wang Y, Shang S. Factors influencing depression in community-dwelling elderly patients with osteoarthritis of the knee in China: a cross-sectional study. BMC Geriatrics. 2022. https://doi.org/10.1186/s12877-022-03117-0.
Ministry of Health and Welfare, Taiwan, R.O.C.: 2016 ~ 2019 Health care utilization of national health insurance. https://dep.mohw.gov.tw/dos/lp-5103-113.html. Accessed 8 May 2022.
Chang CK, **rasagar S, Chen B, Hussey JR, Wang IJ, Chen JC, et al. Provider behavior under global budgeting and policy responses: An observational study on eye care services in Taiwan. Inquiry. 2015. https://doi.org/10.1177/0046958015601826.
de Sire A, Agostini F, Lippi L, Mangone M, Marchese S, Cisari C, et al. Oxygen-Ozone therapy in the rehabilitation field: state of the art on mechanisms of action, safety and effectiveness in patients with musculoskeletal disorders. Biomolecules. 2021. https://doi.org/10.3390/biom11030356.
National Institute for Health and Care Excellence: Osteoarthritis: care and management. https://www.nice.org.uk/guidance/cg177/chapter/1-Recommendations#education-and-self-management-2. Accessed 09 Mar 2022.
Lorig K, Chastain RL, Ung E, Shoor S, Holman HR. Development and evaluation of a scale to measure perceived self-efficacy in people with arthritis. Arthritis Rheum. 1989; https://doi.org/10.1002/anr.1780320107.
Lorig KR, Holman HR. Self-management education: History, definition, outcomes, and mechanisms. Ann Behav Med. 2003. https://doi.org/10.1207/s15324796abm2601_01.
Oh H, Han S, Kim S, Seo W. Development and validity testing of an arthritis self-management assessment tool. Orthopaedic Nurs. 2018. https://doi.org/10.1097/NOR.0000000000000415.
Kang E, Kim S, Rhee YE, Lee J, Yun YH. Self-management strategies and comorbidities in chronic disease patients: associations with quality of life and depression. Psychol Health Med. 2021. https://doi.org/10.1080/13548506.2020.1838585.
Bandura A. The self system in reciprocal determinism. Am Psychol. 1978;33(4):344.
Chan CKY, Cockshaw W, Smith K, Holmes-Truscott E, Pouwer F, Speight J. Social support and self-care outcomes in adults with diabetes: The mediating effects of self-efficacy and diabetes distress. Results of the second diabetes MILES - Australia (MILES-2) study. Diabetes Res Clin Pract. 2020. https://doi.org/10.1016/j.diabres.2020.108314.
Olsson CB, Ekelund J, Degerstedt A, Thorstensson CA. Change in self-efficacy after participation in a supported self-management program for osteoarthritis - an observational study of 11 906 patients. Disabil Rehabil. 2020. https://doi.org/10.1080/09638288.2018.1555616.
Barrera M. Distinctions between social support concepts, measures, and models. Am J Commun Psychol. 1986;14(4):413–45.
Koenders MA, Giltay EJ, Hoencamp E, Elzinga BM, Spinhoven P, Spijker AT. The bidirectional impact of perceived and enacted support on mood in bipolar outpatients: A two-year prospective study. Compr Psychiatry. 2015. https://doi.org/10.1016/j.comppsych.2015.03.009.
Geng Z, Ogbolu Y, Wang J, Hinds PS, Qian H, Yuan C. Gauging the effects of self-efficacy, social support, and co** style on self-management behaviors in Chinese cancer survivors. Cancer Nurs. 2018. https://doi.org/10.1097/ncc.0000000000000571.
Oh H, Ell K. Associations between changes in depressive symptoms and social support and diabetes management among low-income, predominantly hispanic patients in patient-centered care. Diabetes Care. 2018. https://doi.org/10.2337/dc17-2000.
Breland JY, Wong JJ, McAndrew LM. Are common sense model constructs and self-efficacy simultaneously correlated with self-management behaviors and health outcomes: A systematic review. Health Psychol Open. 2020. https://doi.org/10.1177/2055102919898846.
Zhou Y, Huo Q, Du S, Shi X, Shi Q, Cui S, et al. Social support and self-efficacy as mediating factors affecting the association between depression and medication adherence in older patients with coronary heart disease: A multiple mediator odel with a cross-sectional study. Patient Preference Adherence. 2022. https://doi.org/10.2147/PPA.S337634.
Mirmaroofi N, Ghahramanian A, Behshid M, Jabbarzadeh F, Onyeka TC, Asghari-Jafarabadi M, et al. Relationship between self-efficacy and pain control in Iranian women with advanced knee osteoarthritis. Nigerian J Clin Pract. 2019. https://doi.org/10.4103/njcp.njcp_437_17.
Olsson CB, Ekelund J, Degerstedt Å, Thorstensson CA. Change in self-efficacy after participation in a supported self-management program for osteoarthritis – an observational study of 11 906 patients. Disabil Rehabil. 2020. https://doi.org/10.1080/09638288.2018.1555616.
Uritani D, Koda H, Sugita S. Effects of self-management education programmes on self-efficacy for osteoarthritis of the knee: a systematic review of randomised controlled trials. BMC Musculoskeletal Disorders. 2021. https://doi.org/10.1186/s12891-021-04399-y.
Anderson AM, Lavender EC, Dusabe-Richards E, Mebrahtu TF, McGowan L, Conaghan PG, et al. Peer mentorship to improve self-management of hip and knee osteoarthritis: a randomised feasibility trial. BMJ Open. 2021. https://doi.org/10.1136/bmjopen-2020-045389%J BMJ Open.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. PLOS Med. 2007. https://doi.org/10.1371/journal.pmed.0040296.
Chen SY, Wang HH. The relationship between physical function, knowledge of disease, social support and self-care behavior in patients with rheumatoid arthritis. J Nurs Res. 2007;15(3):183–92.
Chen SY. The relationship among disease knowledge, social support, self-efficacy and self-care behavior of the patients with rheumatoid arthritis. In: National Digital Library of Theses and Dissertations in Taiwan. 2003. https://hdl.handle.net/11296/86c8mb. Accessed 20 Oct 2020.
Barrera M, Sandler IN, Ramsay TB. Preliminary development of a scale of social support: Studies on college students. Am J Commun Psychol. 1981;9(4):435–47.
Yeh CL. Relationship between social support and physical health, depression in self-paid care homes. In: National Digital Library of Theses and Dissertations in Taiwan. 1999. https://hdl.handle.net/11296/86c8mb. Accessed 20 Oct 2020.
Park HJ, Kim SS, Lee SY, Park NH, Park JY, Choi YJ, et al. A practical MRI grading system for osteoarthritis of the knee: association with Kellgren-Lawrence radiographic scores. Eur J Radiol. 2013. https://doi.org/10.1016/j.ejrad.2012.02.023.
Ciou HJ. SPSS and R research and statistical analysis: SPSS and data analysis paradigm analysis: Multiple regression, mediation and moderation. 6th ed. Taipei:Wunan; 2019.
Hayes AF. A regression-based approach: Introduction to mediation, moderation, and conditional process analysis. 2nd ed. New York: Guilford Press; 2018.
Alber SM, Musa D, Kwoh CK, Hanlon JT, Silverman M. Self-care and professionally guided care in osteoarthritis:Racial differences in a population-based sample. J Aging Health. 2008. https://doi.org/10.1177/0898264307310464.
Liang SM, Li WY. The relationship between self-efficacy and self-management behaviors among older adults with chronic disease in Macao. Macau J Nurs. 2019. https://doi.org/10.6729/mjn.201912_18(1_2).007.
Chen MF, Wang RH, Hung SL. Predicting health-promoting self-care behaviors in people with pre-diabetes by applying Bandura social learning theory. Appl Nurs Res. 2015. https://doi.org/10.1016/j.apnr.2015.01.001.
Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004. https://doi.org/10.1177/1090198104263660.
Gu L, Wu S, Zhao S, Zhou H, Zhang S, Gao M, et al. Association of social support and medication adherence in Chinese patients with type 2 diabetes mellitus. Int J Environ Res Public Health. 2017. https://doi.org/10.3390/ijerph14121522.
Victoria CT, Jenny MQ, Enriqueta PR, Iris LG, Xavier M, Enrique BG, et al. Understanding knee osteoarthritis from the patients’ perspective: a qualitative study. BMC Musculoskelet Disorders. 2017. https://doi.org/10.1186/s12891-017-1584-3.
Liu S, Hong Z, Zhou W, Fang Y, Zhang L. Job-search self-efficacy and reemployment willingness among older adults: roles of achievement motivation and age. BMC Geriatrics. 2021. https://doi.org/10.1186/s12877-021-02645-5.
World Health Organization. International Classification of Functioning, Disability and Health (ICF). 2001. http://apps.who.int/iris/bitstream/handle/10665/42407/9241545429.pdf;jsessionid=BDC857D30BABAD5C2EB2B762FC38204C?sequence=1. Accessed 26 June 2022.
Acknowledgements
The authors thank all participants for their contributions to the study.
Funding
This research was supported by the Ministry of Science and Technology (MOST 109-2314-B-227 -006 -MY3) and National Taipei University of Nursing and Health Sciences.
Author information
Authors and Affiliations
Contributions
Y.C. contributed to the study conception and design, acquisition of data, analysis and statistics of the data, and drafting of the manuscript. L.W. contributed to the study conception and design, analysis and statistics of the data, and the critical revision of the manuscript. Y.L. contributed to the study conception and design. H.H. contributed to the study conception and design, analysis and statistics of the data, and revising of the manuscript. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All participants provided informed written consent forms before participation in this study. The study protocol complied with the guidelines of the 2013 version of the Helsinki Declaration. The study protocol was approved by the Tri-Service General Hospital Research Ethics Committee prior to data collection (IRB case number: A202105017).
Consent for publication
Not applicable.
Competing interests
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, YY., Weng, LC., Li, YT. et al. Mediating effect of self-efficacy on the relationship between social support and self-management behaviors among patients with knee osteoarthritis: a cross-sectional study. BMC Geriatr 22, 635 (2022). https://doi.org/10.1186/s12877-022-03331-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-022-03331-w