Abstract
Background
Falls are common among adults aged 60 years and older because of physiological changes. Most falls in older adults occur most often at home. Coupled with the lack of awareness and knowledge of preventing falls, the proportion of injuries and deaths among older adults due to falls is increasing yearly. Our study developed a WeChat mini-program for urban elderly to implement teach-back health education (TBHE) that a repeated cycle process of health education, assessment, and re-education in preventing falls at home.
Objectives
This study aimed to evaluate the application effect of the TBHE-based WeChat mini-program on health education knowledge for fall prevention at home for urban older adults.
Design
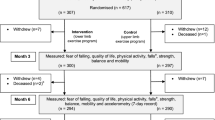
A single-blinded, two-arm parallel-group, randomized controlled trial was conducted.
Setting
Three residential communities, named Hot Spring Apartment, Hualinyuan, and Dongtang Community in Gulou District, Fuzhou, China.
Participants
Participants were older adults recruited from communities in Fuzhou from January to March 2021.
Methods
Fifty-nine participants agreed to participate and were assigned randomly to the intervention group (n = 29) or the control group receiving traditional health education (n = 30). Each participant in the intervention group received twice a week for a total of 8 weeks of health education interventions performed by the first author that she is intervenor according to specific themes. The trial statistician, recruiters, and participants were blinded to group allocation. The intervenor (first author) was blinded to the study hypotheses. To evaluate the effects of the intervention, we assessed participants’ knowledge total score and scores of physiology and disease; drug application; mental, cognitive, and spiritual well-being; lifestyle; and house environment at baseline and 1-week post-intervention and compared scores between two groups. A two-way repeated-measures analysis of variance was conducted to examine the effects of time, group, and their interaction.
Results
There was a significant difference in knowledge of house environment (p = 0.003) between the two groups. Within groups, total and five dimensions knowledge scores had a significant difference (p < 0.001). Moreover, interaction effects were significant on drug application (p = 0.012) and mental, cognitive, and spiritual well-being (p = 0.015).
Conclusions
The TBHE can improve knowledge on fall prevention at home among urban older adults. The TBHE based on the WeChat mini-program could enhance the efficiency and effectiveness of being educated among urban older adults.
Trial registration
Chinese Clinical Trial Register: ChiCTR2100052946; reg date: 06/11/2021.
Similar content being viewed by others
Background
China has the largest elderly population in the world. The seventh census [1] showed that at the beginning of November 2020, the number of people aged 60 years and above in China was 264 million, accounting for 18.70% of the total population. Falls are common among adults aged 60 years and above due to physiological changes [2, 3]. Thus, the incidence of falls increases with age. Approximately one-third of individuals above 65 years fall each year, and the incidence of falls in persons above 80 years is as high as 50% [4]. In addition, 71.20% of older adults will experience contusion, abrasion, sprain, fracture, and even death after falling [5]. Falls have become the leading cause of injury among older adults and the second leading cause of death due to injury in older adults [6]. The most common place where falls occur for older adults is at home. Jiayuan [7] conducted a survey on the status of falls among 561 older adults in urban communities and found that falls were more likely to occur at home than anywhere else, accounting for 45.6%. Tolulope [8] reviewed and analyzed the case data of elderly patients in the U.S. National Trauma Database from 2003 to 2006 and found that more than 42% of older adults fell at home. Therefore, to reduce the overall incidence of falls in the elderly, it is required to start by preventing falls at home.
According to the China Health and Retirement Longitudinal Study [9] that screened 4736 eligible older adults, the incidence of falls in rural areas (22.00%) is higher than that of urban areas (18.70%), even the incidence of severe falls in both urban and rural areas are comparable. Rural older adults are engaged in long-term agricultural work and have a low awareness of fall prevention [11] and has received extensive attention due to its cost-effectiveness, simplicity, and ease of implementation [12]. Minglong [25]. Baduan** could effectively improve balance, leg muscle strength, mobility, and fall prevention [26]. The TBHE intervention process was as follows: (a) The gaps in theoretical knowledge and practical skills in the fall-related lifestyle of older adults was assessed. FA informed participants that they needed to enter the WeChat mini-program every Tuesday to watch 5 min and 14 s of lifestyle animation videos and complete five practice questions related to lifestyle. After completing the questions, FA immediately reported errors to participants. According to a standard answer, FA explained the correct content to the participants and rightly guided them. Participants needed to record a video of themselves completing Baduan** before the coming Friday and send it to FA in advance through WeChat. FA combined the participants’ previous practice questions and recorded exercise videos to manually analyze whether the participants fully mastered the theoretical knowledge and sports skills according to the correct answers and standard exercise movements. Finally, FA scanned and evaluated the total distribution of wrong questions and each person’s sports practices in the WeChat mini-program background, which recorded weak points in each person’s theory and practice. (b) Feedback on weak points in theory and practice were given to the older adults, and they were educated to re-examine gaps to improve. FA asked the participants to watch the Baduan** animation video on Friday and complete the same five exercises again. Then, FA corrected the weak points of each person’s theoretical knowledge and practical skills one-to-one through pictures, voice, and videos. Participants recited the health education content in their language in voice format, gave feedback on sports skills to be mastered in video format, and sent them to FA again. (c) Re-evaluation and re-education: FA re-evaluated participants’ retelling voice and sports video, corrected them again according to the unified standard, and repeated the above process. The TBHE intervention ended only when the participants could correctly repeat all the right knowledge points taught to them during the health education and complete the whole set of Baduan** movements skillfully and standardly, which indicated that they mastered the theoretical knowledge and sports skills. Finally, participants rated their satisfaction after learning the entire health education content on the topic of lifestyle on Friday.
Control group
Traditional health education was used for participants in the control group. Participants were reminded to enter the WeChat mini-program at 8 am every Tuesday to learn health education content on the topic of preventing falls at home and completed the same five exercises as the intervention group. During this research, FA did not perform any active interventions and only responded to participants who had questions, which was also ethical. On Friday, FA urged them to re-enter the WeChat mini-program to learn the health education content on fall prevention at home consistent with the theme of Tuesday. Finally, participants rated their satisfaction after learning the entire health education content on the topic of lifestyle on Friday. After 8 weeks, participants finished learning eight topics content, and traditional health education ended.
Instruments
Socio-demographic questionnaire
A self-designed questionnaire was used to collect sociodemographic information about older adults. Older adults’ sociodemographic data included age, gender, marital status, children number, education, having chronic diseases or not, living with children or not, public officials or not, primary caregiver, monthly income, self-care ability, and smoking, drinking, and exercise frequency.
Home-based fall prevention knowledge (HFPK) questionnaire
The HFPK was developed based on the Health Belief Model (HBM) [27], Expert Consensus on Fall Risk Assessment of Older Adults in China (draft) [28], and Fall Prevention Knowledge, Attitude, and Practice Questionnaire [29, 30]. The HFPK assessed urban older adults’ knowledge of fall prevention, including physiological diseases, application of drugs, psychological cognition and mental status, lifestyle and behavior, and knowledge of the house environment that older adults should be aware of to prevent falls. We emailed 15 community or aged care specialists for comments on the initial questionnaire using Delphi Method. After two rounds of consultation and revision of the questionnaire, we tested the reliability and validity of the HFPK among 374 community-based older adults aged 60 years and above in Fuzhou. The formal HFPK comprises 68 items grouped into five subscales, including physiology & disease (19 items, 0 ~ 19 scores), drug application (8 items, 0 ~ 8 scores), mental, cognitive, and spiritual well-being (12 items, 0 ~ 12 scores), lifestyle (8 items, 0 ~ 8 scores), and house environment (21 items, 0 ~ 21 scores). Its score ranges from 0 to 68. All items are positive, with three answers including yes, uncertain, and no, which are all multiple-choice questions. If answer is Yes, the response is correct and gets 1 point. If answer is unclear or no, the response is incorrect and gets 0. The higher the score, the higher the knowledge level of older adults in preventing falls at home. According to the 100-point scale, 85 ~ 100 is excellent, 75 ~ 84 is good, 60 ~ 74 is medium, and 60 below is poor [31]. Knowledge on preventing falls at home was categorized as follows: 58 ~ 68 as excellent, 51 ~ 57 as good, 41 ~ 50 as medium, and 40 below as poor. After expert evaluations, I-CVI ranged from 0.867 to 1, and S-CVI was 0.985, which achieved the content validity criterion [36] conducted a seven-month teach-back combined with video health education intervention on pulmonary inhalant usage in 163 COPD patients. She found that the teach-back health education could significantly improve participants’ knowledge of pulmonary inhalers usage in the intervention group. Likewise, in our study, a higher knowledge score in the intervention group further confirms the effectiveness of TBHE in drug application knowledge. Before the intervention, two groups had low scores with fall-prevention knowledge regarding their drug application knowledge, which was consistent with the finding of Li** [37] that the awareness rate of drug application knowledge among older adults was lower than 30%. After the intervention, the drug application knowledge score of the intervention group was significantly improved and better than that of the control group. Factually, the meaning of receiving teach-back health education could remind older adults to pay attention to the relationship between drugs and falls when taking various medicines daily so that they are more careful and correct to take pills as directed by their doctors.
In terms of mental, cognitive, and spiritual well-being, the incidence of mental illness, like depression, is increasing year in the elderly population [38]. Compared to other clinical diseases in older adults, depression may be underdiagnosed. People with depression are less likely to seek therapy due to the stigma of mental illness in some areas of China [39]. This study makes older adults realize that they need to attach importance to their mental state by educating them that abnormal psychological states such as emotional stress can easily lead to falls. An interesting finding of this study is that, despite the interaction of time and group on mental, cognitive, and spiritual well-being, the control group scored higher than the intervention group after the intervention. There are two possible reasons as follows. First, the baseline data for mental, cognitive, and spiritual well-being are unbalanced. Before the intervention, the mental, cognitive, and spiritual well-being scores of the intervention group were higher than those of the control group, and the difference was statistically significant (t = 2.410, p = 0.019). After the intervention, the score increase of the intervention group was lower than that of the control group. Second, the intervention in the control group affected the participants. The interventions in the control group were self-learning, and the FA did not engage in any active interventions and responded only to problematic participants. In the satisfaction and feedback, participants mentioned that they thanked the FA for spending time to help them improve their knowledge, patiently answering their questions, and soothing their emotions when they encountered WeChat use obstacles. These measures stimulated their interest in learning and maintained it until the end of the study, creating conditions for participants to learn knowledge, consistent with a comparison within groups results. Self-contrast found that two groups in mental, cognitive, and spiritual well-being were statistically significant (t = − 3.448, p = 0.002; t = − 8.438, p < 0.001), showing that TBHE and traditional health education intervention could increase scores in this dimension. Thus, our project helps to remind participants to value their mental health, maintain a peaceful mind, actively seek psychological treatment, and prevent falls.
In terms of lifestyle and the household environment, participants in the intervention group had significantly higher knowledge scores for fall prevention than those in the control group; however, there was no interaction effect. Zhihong [40] pointed out that a restricted household environment and an unhealthy lifestyle were predisposing factors for falls in older adults and that reducing the per capita housing area and drinking alcohol would increase the incidence of falls. In addition, technical guidelines for fall interventions in older adults [41] pointed out that it is necessary to improve living environments to be suitable for older adults to prevent home-based injuries. Our study suggests that TBHE reinforces older adults’ fall prevention knowledge about their lifestyle and household environment and reminds them to keep healthy living habits and improve their household environment. It is worth mentioning that there was no significant difference in physiology and disease (t = − 0.904, p = 0.370). A study [42] showed that older adults were aware of their decreased physical performance and reduced ability to cope with physical challenges, such as balance, which increased their fear of falling. Fear of falling may cause them to seek out a lot of fall prevention knowledge about physical health. Therefore, learning fall prevention knowledge in physiology and disease is still significant.
Limitations
This study has some limitations. First, the implementation and evaluation process of TBHE were all completed in WeChat without having to meet the participants face-to-face. The authenticity of feedback from participants could not be guaranteed, which was likely to affect the quality of TBHE. Second, we do have not a larger study sample, a higher intervention frequency, and a longer study duration. Scholars in the future can consider increasing the size of the study sample and extending the intervention’s duration to better explore the effect of the intervention. Finally, the WeChat mini-program could only be used on smartphones, which hinders some older adults who use outdated phones from benefiting from such health education. Future researchers need to design more rational health education programs for older adults who do not use smartphones.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due this article is part of the first author’s master’s thesis within two years of confidentiality. The datasets are not suitable for publication now but are available from the corresponding author on reasonable request.
References
National Bureau of Statistics (2021). The Seventh National Census Bulletin (No. 5). Online submission. Available online at: http://www.stats.gov.cn/tjsj/tjgb/rkpcgb/qgrkpcgb/202106/t20210628_1818824. html (Accessed 1 Mar 2022).
Bei**g Hospital, National Geriatrics Center, China Geriatrics Research Association Aging Health Service and Standardization Branch, et al. Guidelines for home (nursing) elderly falls intervention. Chin J Geriatr Care. 2018;16(3):32–4.
Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35(2):ii37-ii41.
Ganz DA, Latham NK. Prevention of falls in community-dwelling older adults. N Engl J Med. 2020;382(8):734–43.
Ming Z. Analysis on the status of fallings and related risk factors among the community-dwelling older adults in 2 districts in Zhejiang. Master Thesis. Hangzhou: Zhejiang University; 2017.
Ming Z, Min Y, Shankuan Z. The epidemiology and prevention for falls in community-dwelling older age. Inj Med (Electron Ed). 2018;7(01):61–6.
Jiayuan Z, Huiying C, Yumei L. Status of falls and related risk factors in older adults in Fuzhou community. Chin J Gerontology. 2015;35(22):6538–40.
Tolulope A, Sharon K, Oluwaseyi B, Dani O, Edward E, Adil H. Epidemiologic trend in elderly domestic injury. J Surg Res. 2012;173(2):206–11.
Junying L, Dongxia G, Fangwei L, Yi Z, Bin Y, Yiming Z, et al. Chinese elderly fall Occurrence status and influencing factors. J Zhengzhou Univ (Medical Sciences). 2020;55(05):662–7.
**aojun W, Yang X, Yuanyuan Z, Yanxia G. Meta-analysis on the incidence of falls among the elderly in Chinese community. Evid-Based Nurs. 2020;6(11):1149–54.
Zhao F, Lijun Y, Min H, Hua L. Study on influencing effect of health education on knowledge, attitude and behavior of elderly inpatients about fall prevention. Chin Gen Pract Nurs. 2013;11(08):675–8.
Qian W, Yan W. Research progress in fall preventing methods at home and abroad. J Nurs Sci. 2013;28(05):87–90.
Minglong W, **aoqi Z, Hui L, **ngli D. Influence of different health education models on prevention of fall of the elderly in community. Chin Nurs Res. 2012;26(02):186–7.
Qiong Y, Ting L, Yuting Y. Research progress of health education methods for preventing the elderly from falling at home. Chin Nurs Res. 2021;35(11):1944–6.
Hong YR, Jo A, Cardel M, Huo J, Mainous AG. Patient-provider communication with teach-back, patient-centered diabetes care, and diabetes care education. Patient Educ Couns. 2020;S0738-3991(20):30315–3.
Choi S, Choi J. Effects of the teach-back method among cancer patients: a systematic review of the literature. Support Care Cancer. 2021;29(12):7259–68.
Hong YR, Cardel M, Suk R, Vaughn IA, Deshmukh AA, Fisher CL, et al. Teach-Back experience and hospitalization risk among patients with ambulatory care sensitive conditions: a matched cohort study. J Gen Intern Med. 2019;34(10):2176–84.
Yong W, Huaicang L. A review of the ontology function and application of WeChat in China. J Kunming Univ Sci Technol (Social Science Edition). 2014;14(02):100–8.
**g Z, Bei L. A preliminary study on the development status of WeChat public platform. Media Rev. 2013;08:8–10.
China Internet Network Information Center (2011). The 28th "statistical report on internet development in China" (full text). Online submission. Available online at: http://www.cnnic.cn/gywm/xwzx/rdxw/2011nrd/201207/t20120709_30886.htm (Accessed 1 May 2022).
China Internet Network Information Center (2022). The 49th "statistical report on internet development in China" (full text). Online submission. Available online at: http://www.cnnic.cn/gywm/xwzx/rdxw/20172017_7086/202202/t20220225_71724.htm (Accessed 1 May 2022).
Tencent Research Institute (2018). The domain of my old: WeChat life for the elderly and family WeChat feedback. Online submission. Available online at: https://www.doc88.com/p-13473345912554.html (Accessed 1 May 2022).
Mengchao W, Jia Q, Hanling G. Nursing intervention and effect evaluation of WeChat propaganda for elderly patients in family hospital beds. Chin J Geriatr Care. 2017;15(05):95–7.
Yakhno NN, Zakharov VV, Lokshina AB. Impairment of memory and attention in the elderly. Neurosci Behav Physiol. 2007;37(3):203–8.
Zou L, Pan Z, Yeung A, Talwar S, Wang C, Liu Y, et al. A review study on the beneficial effects of Baduan**. J Altern Complement Med. 2018;24(4):324–35.
Yuen M, Ouyang HX, Miller T, Pang MYC. Baduan** qigong improves balance, leg strength, and mobility in individuals with chronic stroke: a randomized controlled study. Neurorehabil Neural Repair. 2021;35(5):444–56.
Rosenstock IM. Historical origins of the health belief model. Ph.D. dissertation. Michigan: School of Public Health, University of Michigan; 1974. p. 328–35.
Chinese Journal of Geriatric Care. Expert consensus on fall risk assessment of older adults in China (draft). Chin J Geriatr Care. 2019;17(4):47–48,50.
Yu C. Investigation on the status of fall prevention knowledge, attitude and behaviors on nursing home residents. Master Thesis. Fuzhou: Fujian Medical University; 2016.
Huimin L. Effect of dual mode health education on knowledge, reliability, behavior of fall and falling efficiency in elderly patients. Master Thesis. Chongqing: Chongqing Medical University; 2017.
Dou T. Experiment design and exploration of innovative teaching of other subjects in primary schools in the 21st century (volume 1). Tongliao: Inner Mongolia Children's Publishing; 1999. p. 144.
**gzheng S, **ankun M, Zhenqiu S. Content validity index in scale development. J Cent South Univ (Med Sci). 2012;37(02):49–52.
Minglong M. Statistical analysis of questionnaires: operation and application of SPSS. Chongqing: Chongqing University Publishing; 2010. 158-193, 194-236, 237-265
Sui Y, Wang T, Wang X. The impact of WeChat app-based education and rehabilitation program on anxiety, depression, quality of life, loss of follow-up, and survival in non-small cell lung cancer patients who underwent surgical resection. Eur J Oncol Nurs. 2020;45:101707.
Quan Y, Wenbing Y. Influencing factors and preventive measures of falls in older adults. Chin J Gerontology. 2017;37(17):4373–5.
Ai** Y, Jie C, Yuqing L. Effect of teach-back method combined with video education on the application of lung inhalants in patients with COPD. Chin J Mod Nurs. 2017;23(30):3902–5.
Li** Z, Kun X, Yanfang S, Yadan L, Fangru Z, Juan D, et al. Current status analysis of pre-hospital fall prevention knowledge, attitudes and behavior of long-term caregivers for elderly in military sanitarium for cadres in Bei**g. Nurs J Chin PLA. 2016;33(17):1–5.
Yu J, Li J, Cuijpers P, Wu S, Wu Z. Prevalence and correlates of depressive symptoms in Chinese older adults: a population-based study. Int J Geriatr Psychiatry. 2012;27(3):305–12.
Fang EF, Scheibye-Knudsen M, Jahn HJ, Li J, Ling L, Guo H, et al. A research agenda for aging in China in the 21st century. Aging Res Rev. 2015;24(Pt B):197–205.
Zhihong D, Shuran D, Mingxin W. Fall and its risk factors among the urban aged in China. Popul Dev. 2018;24(04):120–8.
National Ministry of Health. Technical guidelines for fall intervention in older adults. Bei**g: People's Medical Publishing House; 2011. p. 1.
Su Q, Gao Y, Zhang J, Tang J, Song M, Song J, et al. Prevalence of fear of falling and its association with physical function and fall history among senior citizens living in rural areas of China. Front Public Health. 2021;9:766959.
Acknowledgements
The authors would like to thank all the participants who joined this research. And they thank all the teachers and students of the School of Nursing of Fujian Medical University for their help.
Funding
This study belonged to the Provincial Lifelong Education Research Project of Fujian Province in 2020 (No. ZS20126).
Author information
Authors and Affiliations
Contributions
QY was responsible for implementing interventions and manuscript drafting. YuY was responsible for data collection, analysis, interpretation and manuscript drafting. MY and YoY were responsible for recruitment and data collection. TL was responsible for the study conception and design, supervision of the study, provision of administrative and material support, analysis and interpretation of the data, and drafting and critical review of the manuscript. All authors have contributed significantly and agree with the content of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study involving human participants was reviewed and approved by the Ethics Review Committee of Fujian Medical University ([2020] Fujian Medical University Ethics Review No. 81). The corresponding author is a teacher from the School of Nursing, Fujian Medical University, and the remaining authors are graduate students from the School of Nursing, Fujian Medical University. We confirm that all methods were performed according to the relevant guidelines and regulations. In addition, we ensured that each participant received a written inform consent, and after confirming its content, agreed to participate in the study and signed it.
Authors have published a related paper, and the citation information is as follows: Qiong, Y., Ting, L., & Yuting, Y. (2021). Research progress of health education methods for preventing the elderly from falling at home. Chin Nurs Res, 35(11):1944-1946. This manuscript reporting the main findings is original. Trial registration: ChiCTR2100052946 and reg date: 06/11/2021.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ye, Q., Yang, Y., Yao, M. et al. Effects of teach-back health education (TBHE) based on WeChat mini-programs in preventing falls at home for urban older adults in China: a randomized controlled trial. BMC Geriatr 22, 611 (2022). https://doi.org/10.1186/s12877-022-03297-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-022-03297-9