Abstract
Background
Gastrointestinal (GI) motility disorders are common in clinical settings, but physicians still lack sufficient understanding and effective management of these conditions.
Methods
This research assessed Egyptian physicians’ knowledge, practices, and attitudes towards GI motility disorders. A cross-sectional survey employing a self-administered questionnaire was carried out among physicians in Egypt. The questionnaire addressed various aspects of physicians’ understanding, practices, and attitudes regarding GI motility disorders. Data analysis was conducted using descriptive statistics and presented as frequencies and percentages.
Results
A total of 462 physicians took part in the study. Although nearly two-thirds of them knew about GI motility studies, a notable proportion lacked adequate knowledge about GI motility disorders. Notably, 84.2% correctly identified dysphagia as a critical symptom suggestive of an upper GI motility disorder. However, 13.4% incorrectly linked hematemesis with an upper GI motility disorder, and 16.7% expressed uncertainty. In terms of practice, around half of the participants encountered a small number of patients with GI motility disorders (less than 5 per week or even fewer). Only 29.7% felt confident in managing patients with motility disorders. Most participating physicians expressed a willingness to participate in training programs focused on motility disorders.
Conclusions
This study underscores a knowledge gap among Egyptian physicians concerning GI motility disorders. It suggests the necessity of tailored education and training programs to improve their competency and practice in this domain.
Similar content being viewed by others
Background
Gastrointestinal (GI) motility disorders such as gastroparesis, functional dyspepsia, enteric dysmotility, irritable bowel syndrome, and constipation have a substantial global impact, reducing quality of life and imposing significant burdens on health insurance systems [1, 2].
GI motility disorders manifest as unexplained symptoms affecting various parts of the GI tract. These include the upper oesophagal sphincter, oesophagal peristalsis, lower oesophagal sphincter, gastric emptying, small intestinal motility, colonic transit, colonic dysbiosis, and anorectal issues such as dyssynergia and anal sphincter defects. Distinguishing GI motility disorders from organic conditions (such as inflammatory or malignant diseases) heavily relies on patient history, which poses diagnostic challenges [3, 4].
GI motility disorders pose a diagnostic challenge. They manifest as unexplained symptoms affecting various parts of the GI tract, including the upper oesophagal sphincter, oesophagal peristalsis, lower oesophagal sphincter, gastric emptying, small intestinal motility, colonic transit, colonic dysbiosis, and anorectal issues such as dyssynergia and anal sphincter defects [3]. In clinical practice, the first step to assess GI symptoms is to exclude organic diseases, mainly if there are any concerning signs such as weight loss, bloody stool, abdominal masses, lymphadenopathy, or anemia [5]. Motility tests are usually performed for patients with persistent complaints associated with GI motility disorders, significantly affecting their quality of life, nutrition, social functioning, and work productivity, or occasionally elevating mortality risk [6, 7]. Furthermore, distinguishing GI motility disorders from organic conditions (such as inflammatory or malignant diseases) relies heavily on patient history [4].
Recent progress has brought forth sophisticated diagnostic instruments to evaluate GI motility and function [8, 9]. The International Working Group on Disorders of GI and Function strongly encourages the consistent use of these diagnostic tests to detect clinically relevant problems and guide treatment decisions [10, 11]. Despite advancements in this particular area, there remains a lack of overall agreement on the proper protocols for diagnosing and treating extremely severe gastrointestinal motility disorders. This absence of agreement has triggered debates among experts globally, leading to considerable variability in clinical practice [12]. Unfortunately, this circumstance may have increased the number of intestinal failures as a result of severe GI motility disorders [13].
In Egypt, similarly, despite numerous global publications, there is a limited emphasis on GI motility research. We hypothesized that insufficient awareness, ambiguity, and inconsistencies in defining and investigating GI motility disorders might contribute to physicians’ hesitancy in ordering GI motility studies. Consequently, Egyptian patients with such disorders are likely to be underdiagnosed. To comprehensively address this issue, we interviewed Egyptian physicians to explore their attitudes toward adult patients with GI motility disorders, evaluate their clinical practices, and pinpoint specific knowledge gaps in this domain.
Methods
An observational cross-sectional study was conducted in Egypt to examine physicians’ knowledge, practice, and attitudes towards adult patients with GI motility disorders.
Data collection
Physicians were invited to answer a questionnaire. The questionnaire was uploaded online (Microsoft Forms or Google Forms) to be self-employed for physicians to answer. They were invited through several social media platforms (Facebook, Twitter, and Whatsapp).
Questionnaire structure
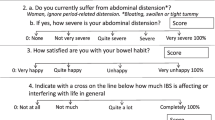
The questionnaire administered in this study comprised two primary sections. Part I gathered data related to socio-demographic characters of the study participant, including age, gender, residence, educational qualifications, specialty, and workplace details. Part II inquired into assessing participants’ knowledge, practices, and attitudes about GI motility disorders. It included questions about understanding and preferences regarding motility disorders, exploration of clinical practices, and evaluation of attitudes towards these conditions.
Questionnaire validation
We ensured that our questionnaire achieved content validity and was well-prepared for further assessment in real-world settings. The following steps were taken: (1) Content Validation Form Preparation: The content validation form was developed to ensure the review panel understood their task clearly. This form served as a guide for evaluating the questionnaire. (2) Expert Review Group Selection: A review group of experts with specific knowledge of the subject matter was meticulously formed. The committee comprised seven professors: two gastroenterologists (MA and MAG), one public health expert (SWE), one specialist in endemic medicine (ME), and three tropical medicine professors (HMA, MAS, and IFM). (3) Pilot Testing and Cognitive Interviewing: Trained team members (EAS) administered the translated questionnaire to 20 participants. Participants’ understanding, readability, language usage, wording, cultural appropriateness of items, and clarity of response instructions were assessed during these interviews. Some interviewees encountered difficulties comprehending certain modified items. Additionally, participants provided valuable feedback on specific questions. (4) Final Version Approval: The questionnaire was refined based on insights from pilot testing and cognitive interviews. Subsequently, the researchers approved the final version, preparing it for field testing.
Statistical analysis
Data were presented as mean ± SD for quantitative variables and percentages and frequencies for qualitative variables. Statistical tools from the Epi website were utilized to determine the sample size. The sample size calculation considered a 5% margin of error, a 95% confidence interval, and an estimated design effect (DEFF) of one (n = [DEFF*Np(1-p)]/[(d2/Z21-α/2*(N-1) + p*(1-p)]). Initially, the estimated minimum sample size was 384 participants. However, the actual collected sample size was 462 participants.
Ethical consideration
The study obtained approval from the Ethics Committee of the National Liver Institute, Menoufia University, Egypt (IRB No: 00416/2022). It adhered to the International Ethical Guidelines for Epidemiological and Descriptive Studies.
Results
Study’s demographics and participant characteristics
Our study had a diverse pool of physicians. All Egyptians, the majority from Greater Cairo (35%). Males participated more than female physicians (56.9% to 43.1%). Physicians aged 30 to 34 were more than any other age group (37.2%). Most study participants held master’s degrees (30.3%) or MDs (33.3%), indicating high education and expertise. Participants averaged 8.45 years of specialty field experience, with 40.3% having fewer than five years. Most participants had diagnostic (52.4%) and therapeutic (29.7%) upper GI endoscopic experience (Table 1).
Participants’ knowledge of GI motility studies and symptoms
Approximately 67.1% of participants indicated familiarity with GI motility studies, while 31.6% responded that they did not know, and only a small percentage (1.3%) were unsure. Dysphagia, odynophagia, reflux symptoms, non-cardiac chest pain, vomiting, eructation, and epigastric pain were recognized as symptoms of upper GI motility disorders by the majority of participants, with percentages ranging from 48.7% to 84.2%. Although not typically associated with upper GI motility disorders, hematemesis was identified as such by a small percentage (13.4%) of participants (Table 2, Fig. 1).
Symptoms such as constipation, bloating, diarrhea, bloody diarrhea, incontinence, the need to strain, a sense of obstruction, and long periods between motions were identified as symptoms of lower GI motility disorders. Notably, while constipation was recognized as a symptom by the majority (85.1%) of participants, bloody diarrhea, which is not typically associated with lower GI motility disorders, was acknowledged by 21.6% of participants (Table 2, Fig. 2).
Participants’ knowledge of GI motility diagnostic methods
A significant portion of participants (63.8%) emphasized the importance of endoscopy as a primary investigative tool for diagnosing various GI motility disorders. The study also revealed overwhelming agreement among participants (84.9%) regarding the indispensable nature of manometry in diagnosing GI motility disorders. Furthermore, participants collectively acknowledged other investigative modalities relevant to diagnosing GI motility disorders. Most (59.1%) recognized pH studies as crucial for assessing acid reflux and esophageal motility. Similarly, a notable percentage (67.1%) affirmed the importance of the barium study, indicating its value in highlighting structural abnormalities and functional issues within the GI tract. Scintigraphy garnered significant recognition, with 74.7% of participants acknowledging its relevance in diagnosing motility disorders and emphasizing its utility in evaluating gastric emptying and transit times. However, opinions regarding the utility of computed tomography (CT) were more diverse, with 65% agreeing or strongly agreeing on its importance, while 34.8% expressed neutral or disagreeing perspectives. This divergence suggests varying participant interpretations regarding CT’s role in diagnosing GI motility disorders. Additionally, endoscopic ultrasound emerged as a priority investigation modality, with 63.2% of participants recognizing its significance (Table 3).
Participants practice for GI motility disorders
Many participants saw GI motility problems, with 24.7% seeing 1–5 and 24.7% seeing 6–10. This highlights the substantial caseload and the importance of effective diagnostic and management strategies. Also, most doctors (34.0%) who think a patient has a GI motility disorder first do endoscopy and imaging, then manometry. This demonstrates a standard, step-by-step method for diagnosing GI motility disorder in clinical practice.
The data demonstrates varying physician practices in referrals and interventions. Most participants refer patients to endoscopy (58.0%), whereas 6.8% and 7.4% suggest surgery and psychiatry. Similarly, 78.5% and 67.2% of physicians commonly manage achalasia and gastroparesis medically, while GERD and constipation receive more diverse management frequencies (Table 4, Fig. 3).
Attitude of the participants about motility disorder
A significant proportion of hospitals lack dedicated motility units or machines, with 56.9% of participants reporting their absence. The reasons cited for this absence vary, including financial constraints, lack of expertise, and perceived lack of necessity due to nearby units. Despite these challenges, participants are strongly inclined to participate in research studies on motility disorders, with 71.2% expressing interest. Additionally, the overwhelming majority (77.9%) of participants affirm the importance of diagnosing GI motility disorders, highlighting the recognition of these conditions as significant health concerns. Furthermore, the belief in the benefits of early diagnosis is prevalent, with 79.7% of participants acknowledging the potential benefits to patients. However, perceived barriers to motility practice, including the complexity of the branch, lack of experts, and expensive investigations, suggest ongoing challenges in effectively addressing GI motility disorders (Table 5).
Discussion
The field of GI tract motility is dynamic and promising, with significant progress made over the past century, particularly in the last five decades. This progress is attributed to integrating various aspects, including electrophysiology, smooth muscle physiology, flow dynamics, neurohormonal physiology, and pharmaceutical research [14]. Interest in GI motility science surged in Egypt after adopting third-space endoscopic techniques in 2019, following the introduction of manometry devices in the 1990s [15].
This study represents a pioneering effort in Egypt and the broader Middle East to assess physicians’ knowledge, attitudes, and practices regarding GI motility studies. A total of 462 Egyptian physicians participated actively by answering the study questionnaire. The participant characteristics revealed a diverse demographic profile. According to the Association of American Medical Colleges, 56.9% of the participants were male, consistent with global trends, as males constitute over 80% of gastroenterologists [16]. Our study also underscores the diverse expertise and backgrounds of the participants, enriching the study’s insights and perspectives. One-third of the participants belonged to the 35–39 age group, with a significant portion falling within the 25–29- and 35–39-year brackets. Gastroenterologists dominated the study, constituting nearly two-thirds of the participants, while most were affiliated with university hospitals. Qualification-wise, around a third held either an MD, with a similar proportion possessing diplomas or fellowships. Specialty experience ranged widely from 0 to 50 years, with a mean of 8.45 ± 6.6, with 40% having less than 5 years of experience. Conversely, endoscopy experience ranged from 0 to 35 years, with a mean of 5.43 ± 5.25 (Table 1).
Our study indicates varying levels of knowledge and recognition among participants regarding GI motility studies and symptoms associated with upper and lower GI motility disorders. Dysphagia, a distressing oesophagal symptom, poses diagnostic challenges, particularly when functional causes are implicated after excluding organic factors [17]. Notably, vomiting is a hallmark symptom of gastroparesis [18], underlining the intricate relationship between GI motility and symptomatology. Moreover, gastroesophageal reflux disease (GERD) manifests through a spectrum of symptoms, including chest pain, dysphagia, odynophagia, epigastric pain, and nausea [19], mirroring a broader spectrum of motility disorders [20]. In our study, nearly 84.2% identified dysphagia as an essential symptom indicating an upper GI motility disorder, followed by 77.1% for non-cardiac chest pain, 72.5% for odynophagia, and 69% for vomiting as an upper GI motility disorder symptom.
Primary constipation is a significant subset of chronic constipation, often resulting from neuromuscular incoordination and frequently overlapped by dyssynergic defecation [21]. Regarding diarrhea, after excluding the presence of alarm symptoms such as bleeding, malnutrition, nocturnal diarrhea, and positive family history of colorectal cancer, dysmotility and functional causes should be investigated to diagnose irritable bowel disease with diarrhea and functional diarrhea [22]. In our study, 85.1% identified chronic constipation as an essential symptom indicating a lower GI motility disorder, followed by 74.5% for the need to strain, 70.6% for diarrhea, and 86.8% for bloating as lower GI motility disorder symptoms (Fig. 2).
GIT bleeding is a red flag of organic causes like inflammation, ulcers, varices, arteriovenous malformations, or malignancy [3]. Surprisingly, 13.4% said hematemesis is a sign of upper GI motility problems, while 16.7% didn’t know. While 16% didn’t know, 21.6% mistakenly replied that reduced GI motility problems cause bloody diarrhea. Nearly one-third of interviewees were unfamiliar with GI motility disorders (Table 2).
High-resolution manometry is well-known as the gold standard for diagnosing oesophagal motor dysfunction [23], especially when combined with impedance sensors [24]. pH studies are the most suitable, advanced method to diagnose GERD and are considered the gold standard [25]. Barium studies remain an essential diagnostic test in patients with motility disorders since they can identify structural lesions such as strictures and help identify significant motility disorders [26]. Gastric scintigraphy is a standard diagnostic tool for gastric dysmotility [27]. Our study findings suggest that participants generally recognize the importance of various investigation modalities in diagnosing GI motility disorders, with endoscopy, manometry, pH study, and scintigraphy particularly emphasized. Nearly two-thirds strongly agreed, and an additional 29.7% agreed that manometry is very important in the diagnosis of different GI motility disorders. However, a lesser percentage showed agreement for other investigations. One third strongly agreed, and an additional 28.8% agreed that pH studies are important in diagnosis, with nearly the same percent for barium studies. Unfortunately, due to wrong beliefs or lack of scientific basis, one-third strongly agreed that CT and abdominal ultrasound play a role in diagnosing GI motility disorders (Table 3, Fig. 3).
Our study findings shed light on physicians’ clinical practices and decision-making processes regarding GI motility disorders in Egypt; nearly half of the participants saw few patients with any GI motility disorders, less than 5 per week, or may not see one weekly. About one-third of them perform endoscopy, imaging at first, and then manometry when suspecting a GI motility disorder. About 24% may even try to treat and re-evaluate before imaging. More than 50% of them very frequently or consistently referred their suspected patient for endoscopy, and 47.9% for manometry. Unfortunately, only 26.9% of studied participants very frequently or consistently referred their suspected GI motility disorder patient to undergo a barium study, and only 13.8% were referred to psychiatry ((Table 4). The most frequent disorders that the participating physicians managed in their clinics were GERD and constipation, which is consistent with the global prevalence of constipation at fourteen percent [28], and the estimated global prevalence of GERD at 15%–25% [29].
When asked about having a motility unit/machine in their hospitals, more than half of the participants stated that they didn’t, in addition to 9.5% who didn’t know. They said this is due to financial problems or non-availability of experts. More than two-thirds of the studied participants paid attention. They were interested in participating in research concerning motility fields, stating that it is essential to diagnose GI motility disorders early. It is worth mentioning that most of the participants had a positive attitude towards GI motility practice. However, only 22.1% felt comfortable when dealing with a patient with a motility disorder. Most of the participating physicians were willing to attend training about motility disorders (96% for how to manage motility disorders medically, 94.6% for how to read a manometry report/topography, and 89.5% for investigations) rather than manometry [e.g., radiological] training (Table 5). This indicates potential gaps in resources and expertise within the healthcare infrastructure, suggesting a need for investment and capacity building to address GI motility disorders in Egypt better.
Standardized guidelines and improved coordination among healthcare providers are highlighted for patient care optimization. Training must be enhanced for suspecting, diagnosing, and managing motility disorders. Resource limitations, expertise boosts, and research initiatives are crucial in managing GI motility disorders in Egypt. The study reveals a lack of knowledge among Egyptian physicians about GI motility disorders, including symptom awareness and understanding of diagnostic modalities. Despite the lack of knowledge, most participants believe early diagnosis of GI motility disorders is important. Addressing knowledge deficits and improving physicians’ practice is essential for better patient outcomes in managing GI motility disorders. Training programs are needed to enhance physicians' knowledge and practice, covering the importance of medical and endoscopic management, early diagnosis, and various investigative modalities. Further research is required to evaluate training programs' effectiveness and identify barriers to GI motility practice in different regions. Studies should be conducted in other countries to understand physicians’ knowledge and practices regarding GI motility disorders.
Limitations
Self-reported questionnaires may cause recall bias. The study had a diverse pool of physicians with different clinical backgrounds, expertise, and specialties, which can affect the level of data interpretation. Despite these challenges, the study aimed to study various responses, reflecting Egyptian physicians’ knowledge, attitudes, and practices about GI motility disorders.
Conclusions
This study provides important insights into the current state of knowledge, practice, and attitudes of physicians regarding GI motility disorders in Egypt. The study highlights the urge for more training and educational programs to improve awareness among physicians regarding GI motility disorders. To achieve proper diagnosis and management of patients with GI motility disorders.
Availability of data and materials
The study data can be made available upon request from the primary or corresponding author.
Abbreviations
- GI:
-
Gastrointestinal
- SD:
-
Standard deviation
- CT:
-
Computed tomography
- GERD:
-
Gastroesophageal reflux disease
- POEM:
-
Peroral Endoscopic Myotomy
- APC:
-
Argon plasma coagulation
References
Mearin F, Lacy BE, Chang L, Chey WD, Lembo AJ, Simren M, Spiller R. Bowel disorders. Gastroenterology. 2016;150:S0016–5085.
Stanghellini V, Chan FK, Hasler WL, Malagelada JR, Suzuki H, Tack J, Talley NJ. Gastroduodenal disorders. Gastroenterology. 2016;150(6):1380–92.
Anderson P, Dalziel K, Davies E, Fitzsimmons D, Hale J, Hughes A, Pockett R. Survey of digestive health across Europe: final report. Part 2: the economic impact and burden of digestive disorders. United European Gastroenterol J. 2014;2(6):544–6.
Mari A, Savarino E. Advances on neurogastroenterology and motility disorders: pathophysiology, diagnostics and management. J Clin Med. 2022;11(10):2911.
Mari A, Mahamid M, Amara H, Baker FA, Yaccob A. Chronic constipation in the elderly patient: Updates in evaluation and management. Korean J Fam Med. 2020;41(3):139.
Amiot A, Joly F, Alves A, Panis Y, Bouhnik Y, Messing B. Long-term outcome of chronic intestinal pseudo-obstruction adult patients requiring home parenteral nutrition. Off J Am Coll Gastroenterol (ACG). 2009;104(5):1262–70.
Jung HK, Locke GR, Schleck CD, Zinsmeister AR, Szarka LA, Mullan B, Talley NJ. The incidence, prevalence, and outcomes of patients with gastroparesis in Olmsted County, Minnesota, from 1996 to 2006. Gastroenterology. 2009;136(4):1225–33.
Ambartsumyan L, Khlevner J, Nurko S, Rosen R, Kaul A, Pandolfino JE, Darbari A. Proceedings of the 2018 advances in motility and in neurogastroenterology: AIMING for the future single topic symposium. J Pediatr Gastroenterol Nutr. 2020;71(2):e59.
De-Madaria E, Mira JJ, Carrillo I, Afif W, Ang D, Antelo M, Drenth JP. The present and future of gastroenterology and hepatology: an international SWOT analysis (the GASTROSWOT project). Lancet Gastroenterol Hepatol. 2022;7(5):485–94.
Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJ, International Working Group for Disorders of Gastrointestinal Motility and Function. Advances in the management of esophageal motility disorders in the era of high-resolution manometry: a focus on achalasia syndromes. Nat Rev Gastroenterol Hepatol. 2017;14(11):677–88.
Savarino E, Bredenoord AJ, Fox M, Pandolfino JE, Roman S, Gyawali CP, International Working Group for Disorders of Gastrointestinal Motility and Function. Advances in the physiological assessment and diagnosis of GERD. Nat Rev Gastroenterol Hepatoly. 2017;14(11):665–76.
Vasant DH, Pironi L, Barbara G, Bozzetti F, Cuerda C, Joly F, Lal S. An international survey on clinicians’ perspectives on the diagnosis and management of chronic intestinal pseudo-obstruction and enteric dysmotility. Neurogastroenterol Motil. 2020;32(12):e13937.
Pironi L, Joly F, Forbes A, Colomb V, Lyszkowska M, Baxter J. Long-term follow-up of patients on home parenteral nutrition in Europe: implications for intestinal transplantation. Gut. 2011;60(1):17–25.
Parkman H, McCallum RW. Historical perspectives on gastric motility and gastroparesis. In: Gastroparesis. 2021. p. 3–11.
Al Lehibi A, Elkholy S, Gouda M, Al Dabbagh A, Al Balkhi A, Almtawa A, Al Otaibi N, El-Sherbiny M, Essam K, Alzahrani MA, Al Ghamdi A, Al Ghamdi A, AlEid A, Qutub A, Alamr A, Ahmad S, Al Sayari K, Al Ibrahim B, Al Khathlan A, Alkhiari RE. Peroral endoscopic myotomy (POEM) for the treatment of achalasia: a multicenter Middle Eastern experience. Saudi J Gastroenterol. 2022;28(1):74–9.
Association of American Medical Colleges. Table B-3: Total U.S. Medical School Enrollment by Race/Ethnicity and Sex, 2014–2015 through 2018–2019. 2019.
Mascarenhas A, Mendo R, O'Neill C, Franco AR, Mendes R, Simão I, Rodrigues JP. Current Approach to Dysphagia: A Review Focusing on Esophageal Motility Disorders and Their Treatment. GE Port J Gastroenterol. 2023;30(6):403–13. https://doi.org/10.1159/000529428.
Cangemi DJ, Lacy BE. Gastroparesis. Curr Opin Gastroenterol. 2021;37(6):596–601.
Kahrilas PJ. Clinical practice. Gastroesophageal reflux disease. N Engl J Med. 2008;359(16):1700–7.
Stein E, Sloan J, Sonu I, Kathpalia P, Jodorkovsky D. GERD for the nongastroenterologist: Successful evaluation, management, and lifestyle-based symptom control. Ann N Y Acad Sci. 2020;1482(1):106–12.
Al Shuaibi TA, Faidah SO, Bannani AB, Nafadi KK, Khalofi TNA, Alsaeed NA, Al Jarad FAS. Constipation causes and management. Indo Am J Pharm Sci. 2019;6(1):681–5.
Singh P, Lee HN, Rangan V, Ballou S, Lembo J, Katon J, Lembo A. Similarities in clinical and psychosocial characteristics of functional diarrhea and irritable bowel syndrome with diarrhea. Clin Gastroenterol Hepatol. 2020;18(2):399–405.
Yadlapati R, Kahrilas PJ, Fox MR, Bredenoord AJ, Prakash Gyawali C, Roman S, Pandolfino JE. Esophageal motility disorders on high-resolution manometry: Chicago classification version 4.0©. Neurogastroenterol Motil. 2021;33(1):e14058.
Tack J, Pauwels A, Roman S, Savarino E, Smout A, ESNM HRM consensus group, Zerbib F. European Society for Neurogastroenterology and Motility (ESNM) recommendations for the use of high-resolution manometry of the esophagus. Neurogastroenterol Motil. 2021;33(5):e14043.
Săraru ER, Enciu V, Peagu R, Fierbinţeanu-Braticevici C. Advances in the diagnosis of GERD. Rom J Intern Med. 2021;59(1):3–9.
Patel DA, Yadlapati R, Vaezi MF. Esophageal motility disorders: Current approach to diagnostics and therapeutics. Gastroenterology. 2022;162(6):1617–34.
Ora M, Nazar AH, Parashar A, Kheruka S, Gambhir S. Gastric emptying scintigraphy: Beyond numbers–an observational study to differentiate between various etiologies and a step toward personalized management. Indian J Nucl Med. 2019;34(3):194.
Suares NC, Ford AC. Prevalence of, and risk factors for, chronic idiopathic constipation in the community: systematic review and meta-analysis. Am J Gastroenterol. 2011;106(9):1582–91.
Al Ghadeer HA, Alabbad ZE, AlShaikh SB, Ahmed SU, Bu-Khamseen AA, Alhashem AT, Alhamrani AH, AlGhadeer MR, Alibrahim DA, Alkishi BM. Prevalence of gastroesophageal reflux disease and associated risk factors in the Eastern Region, Saudi Arabia. Cureus. 2021;13(11):e19599.
Acknowledgements
The research team expresses their deep gratitude to the expert committee professors (Mohamed Alboraie (MA), Muhammed Abdel-Gawad (MAG) from Al-Azhar University, Heba Mohamed Abdella (HMA), Mohammed Amin Sakr (MAS), Imam Fawzy Montasser (IFM) from Ain shams university and Mohamed El Kassas(ME) Helwan University) for their valuable time and effort in reviewing the study questionnaire were greatly appreciated.
Informed consent
Informed consent was provided to all participants, offering a succinct overview of the study’s objectives, advantages, and associated risks at the commencement of the questionnaire. Participants were duly informed of their prerogative to either accept or decline involvement.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). No external funds, grants, or assistance were received in preparing this manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualization, E.A.M.; methodology, E.A.M. and S.W.E.; data collection E.A.M., M.A.K., S.W.E., M.B.H., A.E., S.A.S., and M.A.K.; data analysis, S.W.E.; data curation S.W.E.; writing—original draft preparation, E.A.M., A.E., S.A.S. and S.W.E.,; writing—review and editing,, E.A.M. M.A.K. and S.W.E.; visualization, E.A.M, S.W.E. and M.A.K. All the authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval and consent to participate were ensured in this study, by the guidelines delineated in the Declaration of Helsinki. Approval was granted by the Ethics Committee of the National Liver Institute, Menoufia University (Approval Date: September 2022; IRB No: NLI IRB 00003413; FWA 0000227).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Al Mowafy, E.A., AboKresha, M.M., Elkhadry, S.W. et al. Insights into the current state of knowledge, practice, and attitudes of physicians regarding gastrointestinal motility disorders in Egypt. BMC Gastroenterol 24, 215 (2024). https://doi.org/10.1186/s12876-024-03296-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-024-03296-7