Abstract
Background
Acute Myeloid Leukaemia (AML) is a highly heterogeneous disease. Studies in adult AML have identified epigenetic changes, specifically DNA methylation, associated with leukaemia subtype, age of onset and patient survival which highlights this heterogeneity. However, only limited DNA methylation studies have elucidated any associations in paediatric AML.
Methods
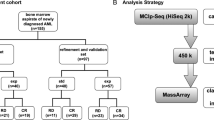
We interrogated DNA methylation on a cohort of paediatric AML FAB subtype M5 patients using the Illumina HumanMethylation450 (HM450) BeadChip, identifying a number of target genes with p <0.01 and Δβ >0.4 between leukaemic and matched remission (n = 20 primary leukaemic, n = 13 matched remission). Amongst those genes identified, we interrogate DLEU2 methylation using locus-specific SEQUENOM MassARRAY® EpiTYPER® and an increased validation cohort (n = 28 primary leukaemic, n = 14 matched remission, n = 17 additional non-leukaemic and cell lines). Following methylation analysis, expression studies were undertaken utilising the same patient samples for singleplex TaqMan gene and miRNA assays and relative expression comparisons.
Results
We identified differential DNA methylation at the DLEU2 locus, encompassing the tumour suppressor microRNA miR-15a/16-1 cluster. A number of HM450 probes spanning the DLEU2/Alt1 Transcriptional Start Site showed increased levels of methylation in leukaemia (average over all probes >60%) compared to disease-free haematopoietic cells and patient remission samples (<24%) (p < 0.001). Interestingly, DLEU2 mRNA down-regulation in leukaemic patients (p < 0.05) was independent of the embedded mature miR-15a/16-1 expression. To assess prognostic significance of DLEU2 DNA methylation, we stratified paediatric AML patients by their methylation status. A subset of patients recorded methylation values for DLEU2 akin to non-leukaemic specimens, specifically patients with sole trisomy 8 and/or chromosome 11 abnormalities. These patients also showed similar miR-15a/16-1 expression to non-leukaemic samples, and potential improved disease prognosis.
Conclusions
The DLEU2 locus and embedded miRNA cluster miR-15a/16-1 is commonly deleted in adult cancers and shown to induce leukaemogenesis, however in paediatric AML we found the region to be transcriptionally repressed. In combination, our data highlights the utility of interrogating DNA methylation and microRNA in combination with underlying genetic status to provide novel insights into AML biology.
Similar content being viewed by others
Background
Acute myeloid leukaemia (AML) is the third most common form of leukaemia in children, typically characterised by the rapid proliferation of primitive haematopoietic myeloid progenitor cells[1]. Paediatric AML is a highly heterogeneous disease, which presents a major barrier towards the development of accurate disease classification, risk stratification and targeted therapies within the clinic. The French-American-British (FAB)[2] and more recently World Health Organisation (WHO)[3] classifications of leukaemia take into account cell morphology, cytogenetic aberrations and common genetic lesions. However, not all patients fall into these well-defined categories. Additionally, the recurrent chromosomal and genetic lesions frequently found in AML fail to induce leukaemogenesis and do not explain the recognised clinical heterogeneity[4, 5].
One of the hallmarks of nearly all human cancers is the disruption of the epigenetic profile, including gross aberrations in DNA methylation. Increasing evidence in adult AML has indicated that epigenetic events play critical roles in the onset, progression, and outcome of AML[6] and may help tailor disease treatment. However, the need for similar elucidations in childhood disease is paramount. Aberrant methylation of cytosine residues at palindromic CpG sites (often clustered in dense CpG ‘islands’) near gene promoter regions is widely studied in carcinogenesis and haematological malignancies[6, 7]. It is now well established that elevated DNA methylation is an important mechanism of gene transcriptional inactivation[8, 9] and genes such as ESR1, IGSF4 and CDKN2B/p15 are epigenetically silenced in adult leukaemia[6]. Previous studies have subdivided adult AML into 16 epigenetic sub-groups based on DNA methylation signatures, correlating with patient clinical outcome and distinct from both normal haematopoietic cells and normal stages of myeloid differentiation[4]. Despite such emerging findings in an adult context, the utility of individual DNA methylation disruptions in paediatric AML has yet to be fully evaluated[6].
MicroRNA (miRNA) represent an alternative epigenetic regulator, having been implicated in the regulation of critical gene expression networks in plants and animals. The role of miRNA in haematopoiesis, cancer and disease is also beginning to be appreciated[10, 11]. The global influence of individual miRNA on the genome is difficult to dissect, as miRNA can modulate the expression of hundreds of genes, and each gene can harbour binding sites for several miRNA[12]. Human miRNA are initially transcribed (pri-miRNA), and processed by several complexes to form a 70 bp hairpin-loop (pre-miRNA)[13]. After successive enzymatic steps, a miRNA:miRNA* complementary duplex is formed where the ‘functional’ strand is combined with RISC (RNA Induced Silencing Complex) and Argonaute proteins to guide, and inhibit, specific target messenger RNA (mRNA) through base pair recognition[14, 15]. However, the miRNA transcriptome is becoming increasingly complex, emphasised by Next Generation Sequencing (NGS) technologies. NGS has highlighted that alternate miRNA* transcripts, as well as miRNA sequence variants (isomiRs[16]) may play a biological role, similar to their canonical miRNA relatives[17, 18].
Links between miRNA deregulation and cancer diagnosis were first identified in adult Chronic Lymphoblastic Leukaemia (CLL), where the loss or down-regulation of tumour-suppressing miRNA cluster miR-15a/16-1 directly caused leukaemic transformation[19, 20]. At present, no such association has been identified for childhood leukaemia. The expression of paediatric disease-associated miRNA has to date only identified a distinction between leukaemia of different lineages and the differentiation of rearranged AMLs within a limited number of cytogenetic subtypes[21, 22]. Paediatric MLL can be distinguished from others by differentially expressed miR-126, miR-146a, miR-181a/b/d, miR-100, miR-21, miR-196a/b, miR-29 and miR-125b[21]. However concordance among studies is often low and the mechanism of deregulation is often unknown[22, 23].
Genes encoding miRNA can be regulated epigenetically in a similar manner to protein coding genes[22]. Studies have demonstrated epigenetically regulated miRNA in adult AML, including hypermethylation and down-regulation of miR-124a and associated deregulation of target mRNA EVI1, CEBPA and CDK6 independent of diagnostic cytogenetic subtype (reviewed in[22]). Additionally, miR-193a targeting KIT, and miR-14b targeting CREB have been identified in adult investigations as specifically controlled by DNA methylation (reviewed in[22]). However, the identification of DNA methylation and miRNA expression connections in paediatric leukaemia is lacking.
Paediatric AML has distinct cytogenetic and clinical features relative to their adult counterparts[5, 21, 24–26]. Therefore, there is a critical need to improve our understanding of the biology of childhood leukaemia as separate entities, distinct from adult disease. Cognisant of this, we aimed to identify differential DNA methylation within paediatric AML on a genome-scale using defined clinical subtypes and age-matched controls. We identified a number of significantly altered DNA methylation loci, with associated gene and miRNA expression change, between paediatric AML and non-leukaemic counterparts. Specifically we describe here the epigenetic deregulation of DLEU2, which has associated alterations in downstream miR-15a/16-1 miRNA cluster expression.
Results and discussion
The DLEU2 gene is specifically hypermethylated and repressed in paediatric AML subtype M5
The FAB subtype M5 (monocytic/blastic leukaemia) is a distinct subtype with characteristic chromosomal abnormalities including t(8; 16), +8 and various translocations involving 11q23 and the MLL locus such as t(9;11), t(10;11), t(11;19) and others[27]. AML subtype M5 also has a high proportion of cytogenetically normal (CN-AML) patients[27], and those with complex karyotypes[28]. A combination of these factors add to the overall unfavourable outcome of paediatric M5 diagnosis[29]. Genome-scale methylation profiling of AML M5 bone marrow samples identified 3,352 significantly differentially methylated probes (DMPs) between paediatric AML FAB M5 (n = 20) and matching non-leukaemic (n = 17) samples. Applying more stringent feature selection criteria of an adjusted p-value <0.01 and ∆β of >0.4 reduced the number of DMPs to 137 (Additional file1).
The list of DMPs included several localising to the long non-coding RNA DLEU2 and the embedded miRNA cluster miR-15a/16-1[19, 20], previously implicated in adult leukaemic[19, 20, 30]. To date, disruption of this region has not been observed in paediatric cancers and as such we chose to focus on DLEU2 in subsequent analysis. A total of three DLEU2 DMPs had an adjusted p-value <0.01 and ∆β of >0.4 (cg05394800, cg20529344, cg12883980). These probes were located within three CpG islands (Chr 13: 50, 690,000-50,708,000: UCSC human hg19 assembly) at the DLEU2/Alt1 transcriptional start site (TSS) and ‘north shore’ (Figure 1), a region up to 2 kb upstream from the DLEU2/Alt1 TSS CpG island under investigation[31]. Henceforth this will be referred to as the DLEU2 promoter.
Regional interrogation of the DLEU2 gene including significantly differentially methylated probes identified by HM450 analysis. Bottom : Distribution of HM450 methylation probes across the DLEU2 region of 13q4. Genes located in this region include: DLEU1, DLEU2, miR15a/16-1 microRNA cluster, TRIM13, KCNRG and miR-3613. Top : HM450 probes identified as significantly differentially methylated between paediatric AML (FAB subtype M5) and non-leukaemic specimens have been plotted against genomic location. The leukaemic group (n = 16) refers to diagnostic bone marrow from paediatric patients. Non-leukaemic group (n = 11) consists of CD sorted cell populations (CD19+, CD33+, CD34+, CD45+) and patient remission specimens. Differential methylation is concentrated in the promoter region of the DLEU2/Alt1 long transcript, which also falls into the body region of DLEU1 within 3 CpG islands (Chr 13: 50, 690,000-50,708,000). Mean methylation β values and 95% CI are shown. Data for leukaemic samples are red and non-leukaemic samples in green. Methylation values range from 0 (0%, no detected methylation) to 1.0 (100% fully methylated). Significantly differentially methylated regions between leukaemic and non-leukaemic samples to p < 0.001 are highlighted with **.
A divergent DNA methylation profile was observed between all cases of paediatric AML with elevated methylation (mean 64% (48-80% CI) across significant probes and non-leukaemic samples (23% methylation; 7-39% CI of mean) (p < 0.001 for all significant probes) (Figure 1; Additional file2). DNA methylation levels at CpG sites interrogated by cg05394800, cg20529344, cg12883980 were confirmed using SEQUENOM EpiTYPER MassArray (Additional file3 and Additional file4) in the discovery sample set of 20 leukaemic patients and 17 non-leukaemic controls, as well as a validation set of paediatric AML M5 patients with heterogeneous cytogenetic diagnoses (n = 19) (CN-AML (n = 5), MLL (n = 7), RUNX1 (n = 2), WT1 (n = 1)) (Additional file5). This analysis confirmed specific DLEU2 promoter hypermethylation in paediatric AML patients (p < 0.001) (Additional file4), with additional genes in this region, including DLEU1, hsa-miR-15a/16-1 microRNA cluster, TRIM13, KCNRG and hsa-miR-3613 showing no differences in methylation between cases and controls (Additional file6). This highlights the potential regional specificity of the observed DLEU2 methylation change in association with AML.
We observed a significant down-regulation of DLEU2 gene expression in paediatric AML (0.07 Fold Change (FC); p = 0.014), and a significant inverse correlation between promoter DNA methylation and gene expression levels (p = 0.0001, Additional file7). Recent studies in adult CLL have also identified a negative correlation between DLEU2 promoter methylation (DLEU2/Alt1) and gene expression[32]. Interestingly there was no change in gene expression for any other genes in this region (TRIM13 = 1.75 FC; DLEU1 = 1.05 FC. Figure 2A).
Expression analysis of DLEU2 and miR-15/16 in paediatric AML. Here we interrogate the gene, miRNA and precursor miRNA expression in paediatric AML compared to non-leukaemic. This interrogation includes DLEU2 and embedded miR-15a/16-1 on chromosome 13q4. The leukaemic group refers to diagnostic bone marrow from paediatric patients. The non-leukaemic group consists of CD sorted cell populations (CD19+, CD33+, CD34+, CD45+) and patient remission specimens, and is represented by the dashed line at Y = 1. Fold Change (FC) is plotted using normalized data and the 2-ΔΔCt method ± SD, and shows the fold change calculated from the means of each group. A. Gene expression including DLEU1, DLEU2 and TRIM13 in paediatric AML (n = 10) compared to non-leukaemic (n = 13) expression. DLEU2 shows a significant down-regulation in AML compared to non-leukaemic expression (0.07 FC, p = 0.014 represented by **), however there is no significant change in expression for TRIM13 or DLEU1. B. Mature microRNA expression, including primary precursor transcript (PRI) and alternate miRNA expression (*), from the miR-15a/16-1 miRNA cluster embedded within DLEU2 for paediatric AML (n = 28, including the 10 used in Figure 2A) compared to non-leukaemic specimens (n = 30, including the 13 used in Figure 2A). Here the miR-15a/16-1 PRI transcript is 3.03-fold higher in expression compared to non-leukaemic expression. Additionally, miR-16-1* (2.52 FC), miR-15a* (2.24 FC) and miR-15a (1.5 FC) also show increases in expression in paediatric AML. No significant change in expression was observed for miR-16 (0.94 FC) in paediatric AML compared to non-leukaemic expression.
DLEU2 and embedded miR-15a/16-1 are regulated independently in paediatric AML
The miR-15a/16-1 cluster has been described to have potent tumour suppressor activity, targeting numerous oncogenic and cell cycle regulatory genes[19, 33]. The cluster is embedded within intron 4 of DLEU2, and has been speculated that expression is driven by the DLEU2 promoter[20, 30]. However, we found no correlation between DLEU2 expression and miR-15a/16-1 expression in paediatric AML, nor down-regulation of the miR-15a/16-1 miRNA cluster in relation to increasing DLEU2 promoter DNA methylation (Figure 2B). In contrast to previous reports for adult leukaemia, no significant change in mature miR-16 expression was observed between paediatric AML and control samples, a result we have reported elsewhere[34]. These observations are independent of the homologous miR-16 cluster embedded in SMC4 on chromosome 3q26, which shows no significant expression or DNA methylation changes in association with AML (Additional file8). Similar results have been reported for adult CLL[32]. Taken together this data suggests an alternate mode of regulation for the miR-15a/16-1 cluster, outside of the DLEU2 promoter region.
Interestingly, recent research has indicated the processing mechanisms of miRNA may be affected by cancer, such that mature miRNA expression becomes disassociated from precursor miRNA levels, and also from the levels of the host gene[3A fall into a range akin to non-leukaemic specimens. Grou** these patients, regardless of clinical subty** (M5a, M5b or M1/M2/M4), forms an additional sub-group, denoted here as ‘t(11)/+8’. The DNA methylation values obtained for probe cg12883980 are depicted, as an indication of the methylation at the DLEU2 promoter. t(11)/+8 are not differentially methylated compared to non-leukaemic specimens (t(11)/+8 sub-group Mean Methylation (MM) = 0.38, non-leukaemic MM = 0.32. p = 0.22). M5a, M5b and M1/M2/M4 AMLs (with the removal of t(11)/+8 patients) have become increasingly hypermethylated compared to non-leukaemic methylation (M5a MM = 0.81, M5b MM = 0.78, M1/M2/M4 MM = 0.87. p < 0.0001), and significantly different from t(11)/+8 (M5a/b p < 0.05; M1/M2/M4 p < 0.0001).
Cases carrying 11q rearrangements are the most heterogeneous of paediatric AML[27, 29, 47], linked to 50–104 translocation fusion partners to date[29, 46, 48]. Trisomy 8 is a frequently reported aberration in adult and paediatric AML[29]. However little is known about the gain of chromosome 8 in isolation and its relationship to disease onset. As such this has been speculated to be a disease modulating secondary event[49]. Lower DNA methylation in the t(11)/+8 subgroup may potentially confer a better prognosis, as it is well documented that hypermethylation of the DLEU2 region is involved in leukaemic transformation in adults[19, 20, 30]. Analysis of the t(11)/+8 subgroup in isolation also revealed no significant miRNA expression differences relative to non-leukaemic samples (Figure 4A), and it is well documented that miR-15a/16-1 abnormalities are also associated with leukaemic transformation in adults[19, 20]. We additionally identified a trend towards decreased risk of relapse in t(11)/+8 subgroup compared to other subtypes, and a trend towards better survival outcomes (Additional file12). These analyses combined may elucidate a connection between DLEU2 promoter DNA methylation (Figure 3B), miRNA expression (Figure 4A) and prognostic outcomes for this subgroup of paediatric AML (Additional file12).
Gene, primary, miRNA and miRNA* expression for paediatric AML defined through clinical classification and DLEU2 Methylation subty**. Mature microRNA expression, primary precursor transcript (PRI) and alternate miRNA isoform expression (*) from the miR-15a/16-1 miRNA cluster embedded within DLEU2 for paediatric AML patients (n = 26: 12 M5a, 5 M5b, 4 M1/M2/M4, 5 t(11)/+8 sub-group) all compared to non-leukaemic specimens (n = 30). Leukaemic groups refer to diagnostic bone marrow from paediatric patients. Non-leukaemic group consists of CD sorted cell populations (CD19+, CD33+, CD34+, CD45+)and patient remission specimens. Linear Fold Change (FC) is plotted using normalized data and the 2-ΔΔCt method ± SD, and shows the fold change calculated from the means of each group. DLEU2 gene expression is down-regulated in all subtypes. A. Fold change in expression comparing non-leukaemic to t(11)/+8 subtype. No significant differences in RNA expression are observed between non-leukaemic specimens and this subgroup. B. Fold change in expression comparing patients from subtype M5a to M1/M2/M4. DLEU2 is down-regulated in all subtypes (as previously described in Figure 2), and primary precursor for miR-15a also appears down-regulated (non-significant). M1/M2/M4 grou**s do not show any mature miRNA expression changes (defined as >2-fold difference from non-leukaemic). Subtype M5a shows a 2.1-fold (±0.8 SD) increase in miR-15a* and a 2.81-fold (±0.4 SD) increase in miR-16-1*. C. FAB subtype M5b shows up-regulation of miR-15a PRI compared to non-leukaemic expression (20.29-fold (±0.6 SD) p < 0.001), with miR-15a* (4.87-fold ±1 SD) and miR-16-1* (9.86-fold ±1 SD) also up-regulated. M5b additionally shows a significant up-regulation of miR-15a PRI compared to t(11)/+8 sub-group samples (p < 0.05), and also from M5a and M1/M2/M4 sub-groups (p < 0.001).
The classification of t(11)/+8 cases as an independent subgroup revealed a significant increase in pri-miR-15a expression in traditional FAB subtype M5b from non-leukaemic (20.29-fold, p < 0.001; Figure 4C) and from M5a/M1/M2/M4 (Figure 4B). The increase translates to a >2-fold increase in miR-15a, 4.87-fold increase in miR-15a*, and 9.86-fold increase in miR-16-1* expression. Based on DLEU2 DNA methylation status, in conjunction with miRNA expression analysis, we speculate that pri-miR-15a expression alone may be a useful biomarker to distinguish M5b FAB subtype from all other AML subtypes.