Abstract
Background
This trial aims to investigate the effectiveness and cost implications of 'pharmaceutical care' provided by community pharmacists to elderly patients in the community. As the UK government has proposed that by 2004 pharmaceutical care services should extend nationwide, this provides an opportunity to evaluate the effect of pharmaceutical care for the elderly.
Design
The trial design is a randomised multiple interrupted time series. We aim to recruit 700 patients from about 20 general practices, each associated with about three community pharmacies, from each of the five Primary Care Trusts in North and East Yorkshire. We shall randomise the five resulting groups of practices, pharmacies and patients to begin pharmaceutical care in five successive phases. All five will act as controls until they receive the intervention in a random sequence. Until they receive training community pharmacists will provide their usual dispensing services and so act as controls.
The community pharmacists and general practitioners will receive training in pharmaceutical care for the elderly. Once trained, community pharmacists will meet recruited patients, either in their pharmacies (in a consultation room or dispensary to preserve confidentiality) or at home. They will identify drug-related issues/problems, and design a pharmaceutical care plan in conjunction with both the GP and the patient. They will implement, monitor, and update this plan monthly. The primary outcome measure is the 'Medication Appropriateness Index'. Secondary measures include adverse events, quality of life, and patient knowledge and compliance. We shall also investigate the cost of pharmaceutical care to the NHS, to patients and to society as a whole.
Similar content being viewed by others
Background
What is the problem to be addressed?
Up to 80% of elderly people may receive inappropriate therapy [1, 2]. This includes over-treatment, causing adverse drug reactions [3] and under-treatment, e.g. for atrial fibrillation [4]. In the UK over-treatment is often due to the process of repeat prescribing. About 75% of all prescribed items are 'repeats' [5], that is items issued without the patient seeing the doctor. Doctors review only about 75% of these [6]. As a result elderly people are more likely to experience drug-related adverse events [7–9]. Thus they are more in need of improved prescribing than younger age groups.
In England the net drug cost for elderly people (those aged 60 and over) was £2,000 million in 1998 [10]. On average they had 3.6 times more prescriptions than younger adults (those aged 15–59 years). Additionally the percentage aged 75 or over of the UK population will double by 2020 [11]. This unprecedented age distribution will have profound effects on society and its institutions, including health care [12].
In the US Hepler and Strand [13] proposed a system of 'pharmaceutical care' (PC). In this system, while doctors continue to take ultimate care of patients, pharmacists are responsible for moderating their drug care. In doing so pharmacists co-operate with doctors, patients and carers in designing, implementing and monitoring a 'pharmaceutical care plan' (PCP) [e.g. Table 1]. By involving patients in decision-making, PC aims to improve communication, promote compliance and concordance with treatment, and achieve specified therapeutic outcomes. This has the potential to reduce the drug bill and drug-related problems, and improve patients' quality of life.
In the UK Lord Hunt (then Parliamentary Under-Secretary of State for Health) recognised that the clinical skills of pharmacists have long been underused [14]. In contrast the workload of general practitioners (GPs) has been rising in recent years. Hence using community pharmacists to manage the medication of elderly patients will rationalise the use of human resources in community health care. Furthermore US studies have shown that better prescribing reduces drug-related problems in hospital [15], drug costs [16] and thus the health care budget. However there has been insufficient information to conduct a full economic analysis. The proposed trial will provide better economic information for policy makers and the pharmacy profession in the UK.
What are the principal research questions to be addressed?
A Is shared pharmaceutical care for elderly people in the community effective in:
i improving the quality of prescribing?
ii improving patient's knowledge about their disease and medication?
iii improving compliance?
iv reducing adverse events?
v and thus improving quality of life?
B Is shared pharmaceutical care for elderly people in the community cost-effective?
Why is a trial needed now?
The UK is facing unprecedented growth in the number of elderly people. So the Department of Health [17] has prepared the National Service Framework for the Elderly to improve health care for elderly people. In May 2000 research funders including the Department of Health, Medical Research Council, Biotechnology Biological Sciences Research Council and Engineering and Physical Sciences Research Council announced plans to develop a co-ordinated approach to ageing research by forming the Ageing Research Funders Forum. The Forum intends to stimulate and facilitate multi-disciplinary research to improve the health of elderly patients.
The Royal Pharmaceutical Society of GB [RPSGB] [18] and the UK Clinical Pharmacy Association [UKCPA] [19] both recommend that UK pharmacists provide 'pharmaceutical care' for their patients. More specifically the Crown report [20] recommends that pharmacists take on the extra role of looking after the long-term drug treatment of patients. Although the pharmacy profession has started to adopt this extended role, there is insufficient rigorous evidence to substantiate this practice. Hence the proposed trial will be important in underpinning these political and professional initiatives.
Most recently the Department of Health [21] has proposed that Primary Care Trusts (PCTs) across England should invest in pharmaceutical care services giving patients access to more help from pharmacists in using their medicines. Consequently pharmacy practice in the community may be completely transformed by 2004. Hence there is a 'window of opportunity' for a randomised trial to evaluate the effectiveness and cost-effectiveness of pharmaceutical care provided by community pharmacists.
More specifically RESPECT will study the co-operation needed between community pharmacists and GPs. The Royal Pharmaceutical Society of Great Britain fully supports this trial and believes it will provide vital scientific evidence for the development of the pharmacy profession within primary health care.
Two recent local developments have helped us to build research infrastructure and capacity, and thus facilitate the proposed trial. First the East Riding Health Authority funded three of us (IW, HE & PDC) to undertake a feasibility study of pharmaceutical care. This focused on 'vulnerable' people, defined as elderly people who were housebound, living alone, mentally ill, or recently discharged from hospital. Fourteen pharmacies offered pharmaceutical care to all general practices within two PCTs – Eastern Hull (urban) and East Yorkshire (rural). This feasibility study enabled us to assess patient cooperation in research and the logistics of undertaking such research. Because many practices in East Yorkshire are dispensing practices, two pharmacists worked directly with these practices to provide pharmaceutical care but not medication. Without formal training pharmacists adapted pharmaceutical care to British primary health care and tested the use of PCPs in collaboration with GPs. Preliminary analysis suggests that pharmaceutical care is entirely feasible and merits rigorous evaluation. The PCP in Table 1 illustrates its potential. Although recruitment was slow, we identified two reasons for this – the lack of research costs for GPs and the shortage of treatment costs for pharmacists. In designing and costing RESPECT we have addressed and, we believe, overcome both problems. We have also developed a training programme for community pharmacists, focusing on the clinical content of pharmaceutical care, and on collaboration with GPs.
Secondly another of us (HE) received a grant from NHS Northern & Yorkshire to deliver a training programme to build up the research capacity of East Riding and Hull community pharmacists. This funding has helped us to prepare community pharmacists to take on the proposed trial, and to overcome the problems we have identified.
Relevant systematic reviews and the need for a trial
Numerous articles have discussed pharmaceutical care and 'medicines management' (which some British researchers regard as a synonym for pharmaceutical care) [22]. Two systematic reviews [23, 24] of pharmaceutical care and medicines management report that only eight papers, all from the US, report randomised studies [15, 25–31]. Only one was in primary health care [30]. Another review shows that none of the studies met accepted pharmaco-economic criteria [32]. All three reviews recommended more randomised trials to evaluate pharmaceutical care.
To extend these reviews in response to comments on our application to the Medical Research Council, in particular to identify newly published or current research, we adopted five distinct strategies. First we conducted our own systematic search of the Cochrane Library, Embase, EPIC and International Pharmaceutical Abstracts (IPA). We based our search strategy for Embase, EPIC and IPA on the algorithm: (pharmaceutical care OR pharmaceutical service* OR ambulatory care clinical OR ambulatory care pharmac* OR clinical pharmac* OR clinical pharmacy program* OR clinical pharmacy specialis* OR community pharmac* OR comprehensive pharmaceutical service* OR medic* management OR patient oriented service* OR pharmac* intervention* OR pharmac*-managed clinic* OR polypharmacy OR polytherapy OR repeat dispens* OR repeat medic* OR repeat prescription) AND (elderly OR aged OR old OR geriatric). We found six more randomised trials on pharmaceutical services or medicines management for the elderly [33–38]. However none evaluated pharmaceutical care for the elderly as we have defined it. Furthermore only Bond's study of repeat dispensing was conducted in British primary health care.
Secondly we searched the current European Union BIOMED database. We identified a recently completed multi-national study of pharmaceutical care for elderly patients in the community. The UK arm in Northern Ireland includes about 100 patients in the intervention group. Though only interim results were available (McElney, personal communication), preliminary findings were encouraging [39]. As health care varies across the EU, however, it is unlikely that the rest of the project is relevant to British primary health care.
Thirdly we searched the current UK National Research Register using the search term 'pharmacy'. We identified seven continuing randomised studies. In one study of patients with coronary heart disease community pharmacists are drawing up care plans [40]. Another four are trials of medication review programmes undertaken by hospital pharmacists, practice pharmacists (pharmacists working in GP surgeries) or research pharmacists rather than traditional community pharmacists (Nazareth, Reid, Thomas, Zermansky). The remaining two interventions cannot be classified as pharmaceutical care or medicines management (Barber, Peat).
Fourthly we contacted the 16 current Schools of Pharmacy in the UK to seek other pharmaceutical care projects. We identified two randomised studies at Robert Gordon University using practice pharmacists to run 'medication review clinics' in GP surgeries rather than community pharmacists in their own pharmacies. Other Schools of Pharmacy have confirmed that no study has been or is being conducted except that in Northern Ireland [39].
Finally we contacted known experts in pharmaceutical care – Dr Susan Ambler (RPSGB), Professor Alison Blenkinsopp (University of Keele), Professor Joseph Hanlon (University of Minnesota), Dr Janet Krska (College of Pharmacy Practice), Professor James McElney (Queen's University Belfast), and Dr Foppe Van Mil (Pharmaceutical Care Network Europe Foundation). This identified four more trials [41–44].
Most of the 19 completed trials have reported positive findings including improved knowledge of and adherence to treatment, improved biochemical outcomes, and even reduced mortality in heart failure. However only two addressed the economics of pharmaceutical care and medicines management [31, 38].
In summary the literature suggests that pharmaceutical care can benefit patients. As the majority of randomised studies were in the US, their relevance to the UK is limited. Furthermore very few were in community pharmacies, and only two related to elderly patients in the UK [39, 42]. So the evidence about the effectiveness of 'pharmaceutical care' within British primary care remains weak.
Nevertheless PC is being promoted by all the pharmaceutical organisations – National Pharmaceutical Association, Pharmaceutical Services Negotiating Committee [45], RPSGB [18, 46] and UKCPA [19]. To implement this advice without more evidence would therefore create an 'evidence gap'. Usual practice would diverge from the objective evidence [47]. Nevertheless the NHS plan and its pharmacy sequel [17, 21] proposed alternative contracts for "personal medical services-like schemes" such as medicines management, pharmaceutical care and repeat prescribing provided by community pharmacists. However our literature review has shown that practice or research pharmacists based in clinics, rather than community pharmacists based in their pharmacies, have conducted most of the relevant research. Hence there is an urgent need for large studies to evaluate the effectiveness of pharmaceutical care and the use of PCPs in British primary care.
How will the results of this trial be used?
This study will provide policy makers and the pharmacy profession with information about the practicality and effectiveness of pharmaceutical care in British primary care. It will estimate the benefits and costs of pharmaceutical care in this context and provide information for the Department of Health to develop an appropriate remuneration formula. In short the study will provide evidence to guide the future implementation of pharmaceutical care in the UK and thus encourage 'evidence-based pharmacy practice'.
Risks to the safety of patients in the trial?
This is a pragmatic trial with very little risk to patients. Those receiving pharmaceutical care will be at no greater risk than in normal clinical practice. Thus there is no need for an (independent) Data Monitoring and Ethics Committee. Instead two (statutory) Local Research Ethic Committees (LREC) – Hull & East Riding and Selby & York LREC – have given ethical approval.
Design
Brief summary
In PC doctors continue to take ultimate care of patients and pharmacists are responsible for moderating their drug care, in particular by designing, implementing and monitoring a PCP. Our feasibility study of PC in fourteen pharmacies in Eastern Hull and East Yorkshire Primary Care Trusts (PCTs) suggested that the approach was feasible and merited rigorous evaluation. We are therefore expanding the size and scope of our research within a randomised multiple interrupted time series design. We are collecting data on prescribing and resource use from about 20 general practices and about 60 pharmacies and on health outcomes from 400 patients.
What is the proposed trial design?
The Medical Research Council (MRC) has defined 'complex interventions in health care' as "interventions comprising separate elements which seem essential to the proper functioning of the intervention although the effective ingredient is difficult to specify" [48]. PC is an archetypal complex intervention. The MRC has identified five essential steps in the evaluation of such an intervention – theory, modelling, exploratory trial, definitive randomised trial and long-term implementation [48]. A definitive trial must be generalisable in the sense that it recruits a range of patients or conditions across a number of centres. It must also be 'pragmatic' in the sense that it evaluates the complex intervention in routine clinical practice and in a form close to that in which implementation is likely in the long term [49]. In contrast exploratory trials evaluate complex interventions in controlled experimental conditions and in a prototype or idealised form [49]. Of the 19 trials summarised previously most are exploratory, few definitive. Thus it is a pragmatic multi-centre trial that PC now needs.
It is difficult to design a pragmatic trial for PC that randomises individual patients [50]. Both GPs and pharmacists learn the relevant techniques cumulatively, with the result that those who use these techniques for experimental patients cannot readily withhold them from control patients. It follows that randomisation must be by 'clusters' of patients, for example patients associated with a practice or pharmacy. Unfortunately practices and pharmacies are rarely coterminous. Hence if we take practices as the clusters to be randomised, then neighbouring pharmacies will serve some patients randomised to PC and others randomised to usual care. Thus there will be contamination within pharmacies. Similarly if we take pharmacies as clusters, there will be contamination within practices. We conclude that PCTs are the most appropriate clusters for randomisation. Our feasibility study lent support to this analysis. Encouraged by the recent establishment of the Hull York Medical School [51], we have therefore recruited five PCTs in North and East Yorkshire to take part – Eastern Hull, East Yorkshire, Selby & York, West Hull, and Yorkshire Wolds & Coast.
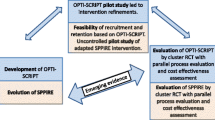
If we select half of the PCTs at random for training in pharmaceutical care, there is a real danger that the other half will suffer from 'resentful demoralisation' [52]. At the very least, therefore, the second half should receive training at the end of the trial. Fortunately we can do even better by phasing the training in PCTs in a random order, as shown in Figure 1. Because each PCT has a period before training to compare with the period after training, each can act as its own control. This design, known as a randomised multiple interrupted time series [52], has three major advantages:
a organisational – because training needs fewer resources over a longer period;
b statistical – because it is more powerful; and
c epidemiological – because staggering the introduction of PC across PCTs helps to protect the evaluation from potentially contaminating changes in health and other policies by ensuring that such changes affect different PCTs at different stages of the cycle of develo** PC.
Our feasibility study also suggested that within each PCT we could recruit at least four general practices and about three community pharmacies associated with each practice – about 20 practices and 40 pharmacies in all. We have randomised the resulting five clusters of practices, pharmacies and patients to begin pharmaceutical care in five successive waves. All five stay in the control group until they receive the intervention in a random sequence.
What are the planned trial interventions?
Intervention group
The experimental intervention is PC, in which pharmacists co-operate with doctors, patients and carers in designing, implementing and monitoring a PCP for example Table 1. The London and Bradford schools of pharmacy are providing five blocks of training, each consisting of one workshop for community pharmacists on PC for the elderly and one joint workshop for pharmacists and GPs on how to work together. GPs and community pharmacists in the same PCT attend the same training block (Figure 1)). The workshops encourage them to adopt a problem-based approach to the application of pharmaceutical care. In particular they enable pharmacists to assess patients' pharmaceutical care, to withdraw unwanted medicines, and to draw up PCPs. The training also enables GPs to work with PCPs. Hence these workshops are accredited for both professions. They also take account of experiences with our feasibility study. Thereafter with the support of Bradford School of Pharmacy and Hull Postgraduate Medical School we shall extend the function of Hull and East Riding Pharmacy Development Group and establish a local PC network to support all participating pharmacists and GPs.
Once trained, community pharmacists meet recruited patients. Although few pharmacists previously provided PC in the way we are training pharmacists, they often had private conversations with patients in a separate room. PC is building on these existing arrangements. Participating pharmacists have professional discretion, either to interview patients in the pharmacy or to visit them at home. This pragmatic choice enhances the external validity of RESPECT.
The community pharmacists follow the following steps to develop the PCP (adapted from Strand et al 1992) [53]:
A Establish pharmacist-patient relationship.
B Collect, synthesise and interpret relevant information on patient, disease and drug, working with GP and patient.
C Define and rank drug-related problems ["an event or circumstance involving a drug treatment that (potentially) prevents a patient experiencing an optimum outcome of medical care" – Strand et al 1990] [54]:
i Failure to receive drug: the patient has a medical problem that resulted from his or her not receiving a drug.
ii Untreated indication: the patient has a medical problem that requires drug therapy (an indication for drug use) but is not receiving a drug for that indication.
iii Improper drug selection: the patient has a drug indication but is taking the wrong drug.
iv Sub-therapeutic dosage: the patient has a problem that is being treated with too little of the correct drug.
v Overdosage: the patient has a medical problem that is being treated with too much of the correct drug.
vi Adverse drug reaction: the patient has a medical problem that stems from an adverse reaction to a drug.
vii Drug interaction: the patient has a medical problem that is the result of a drug-drug or drug-food interaction.
viii Drug use without indication: the patient is taking a drug for which there is no medically valid indication.
D Establish therapeutic goals for each drug-related problem with patient and GP.
E Identify feasible alternative treatments.
F Select the best pharmaceutical solution and decide with patient the best drug, formulation and dose.
G Agree pharmaceutical care plan with both patient and GP (e.g. Table 1).
H Implement and monitor plan.
I Follow up and measure outcome.
In addition pharmacists educate patients and, if appropriate, carers about the indication for each medication and its use, and withdraw unwanted medicines with patients' consent. If patients need compliance aids such as dosette boxes or reminder charts, the pharmacists provide these services. They continue to update and implement the PCP, and monitor outcome at least monthly in association with patients and their GPs.
The patient has a Study Membership Card to remind hospital staff to contact the patient's community pharmacist when the patient is admitted to and discharged from hospital. The community pharmacists can then change the patient's PCP accordingly and avoid drug-related problems arising from miscommunication after hospital discharge. If patients are unable to visit the pharmacy, for example after hospital discharge, pharmacists should arrange a domiciliary visit to provide the pharmaceutical care.
We are monitoring the process of pharmaceutical care by collecting PCPs and analysing pharmacists' time sheets, continuing education records and professional development portfolios.
Although patients have the right to take their prescriptions to any pharmacy for dispensing, there is evidence that more than 80% consistently use the same pharmacy. To facilitate pharmaceutical care, we encourage, but not require, them to do so. As PC is time-consuming, however, it is unlikely that a second pharmacy would duplicate the plan. As the potential use of more than one pharmacy is an inevitable part of this complex intervention, this pragmatic arrangement will enhance external validity.
If a trained pharmacist leaves a participating pharmacy, we shall give individual training to his or her successor – another example of the pragmatic nature of this trial.
Control group
Until they receive training and join the intervention group, community pharmacists provide their usual dispensing service and so act as controls. At this stage pharmacists do not know which patients have consented to join the trial.
What are the proposed arrangements for allocating patients to trial groups?
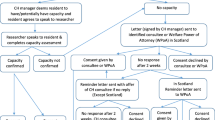
The PCT is the natural unit within which to train and support community pharmacists and GPs in PC care and to allocate this intervention in sequence. One of us (PDC) wrote to all practices in the five PCTs, outlining the project, making clear the nature of the working agreement between practices, associated community pharmacies, and the project team, and inviting expressions of interest. From those responding in each PCT who are close to potential participating pharmacies, we recruited a sample of at least four practices after stratifying for number of partners and about 60 associated pharmacies. When appropriate we recorded reasons given by practices and pharmacies for not taking part. Recruited practices then helped us recruit samples of about 35 eligible patients, depend on the size of the practice, the sampling method varies:
-
a)
For smaller practices (consisting of one or two partners) with less than 100 patients there was no sampling. For practices with over 100 eligible patients sampling (stratified by age and the number of drugs) was completed. A list of eligible patients was obtained from the practice computer record and from them a random sample of up to 100 patients was obtained. This list was given to the GPs to obtain their consent for researchers to approach those patients concerned. Following this each patient was written to and where appropriate a meeting arranged with a member of the research team. The decision to participate in the trial was therefore the patients choice.
-
b)
For larger practices (consisting of three or more partners) – sampling (stratified by age and total number of drugs) was undertaken if there were more than 200 eligible patients. A list of eligible patients was obtained from the practice computer and the GPs were then asked to provide consent for researchers to approach a maximum of 200 patients. Again the decision to participate in the trial involved choice on the part of those patients concerned.
There is conflicting evidence whether age is a risk factor for drug-related adverse events [55–57]. Fortunately stratification is a technique that generally yields statistical gains, but not costs.
In principle we did not restrict the pharmacies that could volunteer for RESPECT. This pragmatic approach enhances external validity, especially if pharmacists can volunteer to provide PC in future. In practice we sampled general practices after stratifying by size. This limited the final sample of participating pharmacies to those associated with sampled practices. Whether a pharmacy is independent or part of a chain is a potential covariate in our eventual multi-level analysis. Both our palliative pharmaceutical care study [58] and our feasibility study have shown that single-handed pharmacists can provide PC. However both studies have also shown that resource constraints limit the numbers of patients in PC at any time. The NHS treatment costs available within RESPECT have helped to address this hurdle.
What are the proposed methods for protecting against other sources of bias?
Blinding is not possible for pharmacists, GPs or patients because the nature of the intervention requires their full knowledge. However pharmacists do not know which patients have been recruited into the trial until they receive training and join the intervention group. Furthermore patient questionnaires are self-administered or administered by the research pharmacist and trial co-ordinator rather than pharmacists or GPs. Finally the assessors of one of the main outcome measures, the Medication Appropriateness Index will remain blind throughout.
The trial co-ordinator and research pharmacist used practice computer records to identify potential trial participants and asked GPs to give consent. Although GPs withheld consent for some patients, the research staff asked for reasons. (To identify, and if necessary adjust for, selection bias we shall also compare the personal characteristics of all consented and non-consented patients.) The research staff then invited potential participants into the trial using practice headed letters and visits to practice or home.
What are the planned inclusion and exclusion criteria?
Inclusion criteria
Patients aged more than 75 years with repeat prescriptions for five or more drugs (excluding drugs taken only when required), who are living at home, well oriented in time and place, and able to give their consent to take part. Abbreviated Mental Test is used to confirm patients' mental state, patients score 7 or above (out of 10) will be included. Their GPs' consent is also necessary.
Exclusion criteria
Patients in residential or nursing homes. Patients who took part in our feasibility study of vulnerable elderly people or who normally use a pharmacy which has refused to participate in the trial. Patients with memory impairment who score 6 or below on the Abbreviated Mental Test.
What is the proposed duration of treatment period?
12 months (Figure 1)
What is the proposed frequency and duration of follow up?
We plan to observe patients for 36 months between recruitment and final visit (Figure 1). We have asked them to provide data at recruitment, at the beginning of pharmaceutical care and three and 12 months thereafter, and at the final visit 36 months after recruitment. We have asked their practices and pharmacies to provide access to their medical records at the end of the study.
What are the proposed outcome measures?
Primary
Medication Appropriateness Index
Secondary
Patients' knowledge, compliance and concordance, practice-reported (and therefore more serious) adverse events, and self-assessed health outcome
Economic
Cost of treatment to NHS, patients and society as a whole
How will the outcome measures be measured at follow-up?
Medication Appropriateness Index (MAI)
The MAI was devised by Hanlon [59] to measure the appropriateness of medication, validated by Samsa [60] and Schmader [61], and successfully used within a randomised trial by Hanlon [15]. The resulting score depends on the number of drugs regularly taken by the patient and the assessed appropriateness of each. In this study we shall use blinded and independent (though paid) clinical pharmacists to assess the appropriateness of drugs prescribed within the trial. Clinical pharmacologists and gerontologists will validate a sample of these data. They will use the information available from patient medical records at recruitment, at the beginning of pharmaceutical care and three and 12 months thereafter, and at the final visit 36 months after recruitment. The research pharmacist and trial co-ordinator will collect these data from the records of participating practices, including their repeat prescription indices, electronically wherever possible. By designing the panel assessment forms for electronic scanning we shall quickly identify patients about whom the assessors disagree. They will then meet to resolve such differences. Although the MAI is an intermediate outcome, it is correlated with the absence of adverse reactions and interactions. We shall investigate whether it is also correlated with better patient outcomes. Few British studies have used the MAI. We shall therefore use psychometric methods [62] to revalidate it for the UK. Meanwhile we are undertaking a feasibility study to compare scores within and between expert professionals.
Knowledge, compliance, adverse events and health outcomes
Research staffs are monitoring knowledge, compliance, adverse events and self-assessed health outcomes in all trial patients over the duration of the study. Depending on the mental state and accessibility of the patient they use patient-completed questionnaires, telephone interviews or home interviews – at recruitment, at the beginning of pharmaceutical care and three and 12 months thereafter, and at the final visit 36 months after recruitment. There is evidence that method of completion affects health outcome measures [63, 64]. To prevent this affecting the internal validity of the trial we shall check that the proportions of patients using the three modes of completion are consistent across both PCTs and time. If necessary we shall use analysis of covariance to adjust for any imbalance in these proportions.
Compliance and patients' knowledge of medication
We ask patients to complete a questionnaire to measure compliance, originally devised by researchers at Keele University. Before its use in RESPECT we are enhancing and revalidating it
Pharmacists ask patients how they take each drug during pharmaceutical care. We shall calculate the proportion of medications for which their response agrees with the directions on the records in the pharmacy or practice [15]. For patients with at least six months' continuous drug records we shall calculate expected percentage compliance from the expected finish date for each prescription and the date on which the next prescription was filled. We are using general practice data to validate pharmacy records, particularly important during the control period.
We use tablet counts as a further measure of compliance. We ask pharmacists to request patients to bring all tablets to the pharmacy at the start and end of the intervention. The pharmacist conducts a tablet count on both occasions. If a patient is housebound, the pharmacist visits the patient's home. Pharmacists also ask patients about the indications for the medication, using questions like "what is this drug for?" or "how does this drug help?" To measure patients' knowledge of medication we shall calculate the proportion of drugs for which they give a correct response, based upon their medical problems and accepted indications for prescribing each drug [15].
To validate pharmacists' tablet counts and patients' knowledge about medication, researchers conduct further tablet counts and ask samples of patients about indications for medications on two separate occasions. At recruitment and at the start of the intervention they visit a 1 in 5 stratified random sample of patients at home and count their supply of tablets. This sample of approximately 140 patients consists of 70 housebound patients and 70 patients able to visit the practice. They visit a second stratified random sample of 140 patients and count their tablets at the start of the intervention and at either three or twelve months thereafter, selected at random.
Adverse events
Throughout the study we collect data from general practices on serious adverse events, consultations in primary care, and hospital referrals and admissions. We define a serious adverse event as one that carries a risk of death or persistent or significant disability or incapacity, or requires hospitalisation or medical or surgical intervention. Though there is evidence that patients can enhance the measurement of mild adverse events, [65–67] pharmaco-vigilance in the UK traditionally focuses on practice-reported adverse events, which are generally more serious, and provide a more cost-effective monitoring system.
Health outcomes
We shall use two instruments that are acceptable to elderly patients. To measure general health status we shall use the SF-36. To underpin cost-utility analysis we shall use the EQ5D [68], acceptable to elderly people if one omits the 'thermometer'.
Home interviews
Rather than interview all respondents face to face on all occasions, we invite able respondents to complete postal questionnaires, and conduct interviews by telephone whenever feasible. To this end we have developed criteria to guide the completion mode appropriate to each respondent. We shall also take account of completion mode in our analysis. In particular we shall compare the validity, reliability and responsiveness of each data collection method [62, 69].
Will health services research issues be addressed?
The economic evaluation will take the form of an incremental cost-utility analysis from the perspective of both the NHS and society in general. The main focus of the economic evaluation will be the EQ5D. We shall also analyse other outcomes, in particular the SF-36 and MAI, to establish whether the choice of measure affects the results of the economic evaluation.
Given the difficulty of disentangling the costs of pharmaceutical care and its sequelae from other costs, economic analysis will include all health care costs, including hospital admissions and referrals, ambulance journeys and consultations in primary care and at the pharmacy.
We shall extract data from practice records on medications prescribed, number and type of consultations in the practice or at home, outpatient referrals and length of any inpatient stay. We shall also extract data from pharmacy records on medications dispensed. All these data will relate to the period from 12 months before the intervention until 24 months after completion of recruitment. In addition pharmacists contributing to RESPECT will complete a questionnaire at baseline to identify the average time spent dealing with patients like those to be recruited into RESPECT, both in dispensing medications and providing advice and support. They will also record prospectively the contact and non-contact time spent on the PCP for each patient, as part of that PCP. Patients and carers will provide data on the costs to themselves in both time and money of seeking pharmaceutical and other health care, as well as estimates of time off from normal activities. They will also provide data on the carer support they normally receive, including help with taking their medication and using compliance aids. These data from patients will serve to validate and enhance the estimates of health care use derived from practice records. The costs associated with training general practitioners and pharmacists will also be assessed, including fixed costs, consumables, patients' time, locum cover and travel costs. Later sensitivity analysis will allow us to assess the extent to which the cost-effectiveness of pharmaceutical care depends on the process of implementation, especially on the relative increase in pharmacist workload.
We shall derive an annual cost of management for the control and intervention period for each patient and use these data to calculate an incremental cost for each patient. As patients serve as their own control, if a patient dies during the control period they will not be included in any of the analysis. If the patient dies during the intervention period, their data will be included in the analysis. Censored data will be adjusted accordingly using appropriate techniques.
Cost-effectiveness will be assessed via the ratio of additional cost to additional benefit, measured according to the change in the EQ5D between the control and intervention period. The confidence region surrounding the average incremental cost effectiveness ratio will be estimated using appropriate statistical techniques such as the bootstrap method and Monte-Carlo simulation. Stochastic analyses such as this will allow a cost effectiveness acceptability curve to be generated. This will represent a plot of the probability of management with a PCP being more cost-effective than usual care under alternative assumptions about the threshold cost per QALY. Based on the average incremental cost, cost-effectiveness ratio and the uncertainty surrounding the estimates, we will explore the implications of a widespread implementation of pharmaceutical care.
What is proposed sample size and justification for power calculations?
After losses to follow up the final sample size will be about 400, viz 20 practices × 20 patients on average or 40 pharmacies × 10 patients on average. It is difficult to estimate the power of this complex design to detect changes in the MAI, the principal outcome measure. To simplify this calculation we discount the likely advantages conferred by time series analysis and estimate the power of analysing the change in the MAI between baseline and three (or 12) months.
The 400 or more patients completing the proposed trial will not be a simple random sample, but a sample from 40 or so clusters – the patients who use each of the participating pharmacies. If these pharmacies are at all consistent in their approach to pharmaceutical care, findings will be more homogeneous within them than between them. The effect of this is to reduce the power of the trial by the factor [1 + ICCC × (n - 1)], where ICCC is the 'intra-cluster correlation coefficient' and n is the average cluster size [70].
Although we know of no data on ICCCs for the MAI, we have access to the full data set of the North of England Study of Standards and Performance in General Practice (1992), [71] including data on practitioners' adherence to clinical guidelines analogous to the MAI. Since none of those intra-practice CCs exceeded 0.1 and few exceeded 0.05, we base our preliminary estimate of the power of RESPECT on an intra-pharmacy CC of 0.1. Since the average cluster size is 10 (viz 400 divided by 40), the effective sample size of RESPECT for the MAI could be as low as 210 (viz 400 divided by 1.9).
An effective sample size of 210 would yield 80% power when using a significance level of 5% to detect a difference in MAI between intervention and control groups of 0.4 of a standard deviation (SD) [72] – usually regarded as a moderate effect size. Although we cannot yet estimate the SD of the MAI within RESPECT, Hanlon's trial reported that the MAI had an SD close to 10 points [15]. Under conservative assumptions about loss to follow up and intra-pharmacy correlation, therefore, RESPECT can detect a change of four points in the MAI. In contrast Hanlon's trial achieved a change of five points [15]. The grant-holders, who include four clinicians, therefore judge that a change of four points is both achievable and clinically important.
We cannot yet estimate the SD of EQ-5D scores within RESPECT. In the general population the EQ-5D has an SD of the order of 16 points [73]. Although we know of no data on ICCCs for the EQ-5D, none of the intra-practice CCs for patient outcomes in the North of England Study of Standards and Performance in General Practice (1992) [71] exceeded 0.01. We therefore base our preliminary estimate of the power of the RESPECT trial to detect changes in EQ-5D on an IPCC of 0.01. So RESPECT should have an effective sample size of at least 370 for outcomes (viz 400 divided by 1.09). This would yield 80% power when using a significance level of 5% to detect a change in EQ-5D scores equivalent to 0.3 standard deviations, ie about five points. Although the applicants do not expect much change in generic outcomes following the introduction of pharmaceutical care, they judge that a change of five points would indeed be clinically meaningful.
What is the planned recruitment rate?
There are nearly 150 practices in the East Riding and Selby & York PCT, all computerised and linked to the NHS network through the East Riding Health Authority. From a survey of four practices we established that there are more than enough patients meeting the inclusion criteria for the trial. In one practice of 8,000 patients, for example, there were 180 men over 75, of whom 25% took five or more different drugs. The numbers and proportion of women were greater. We therefore expect no difficulty in recruiting 35 patients from each practice.
Are there likely to be any problems with compliance?
Compliance with the intervention is unlikely to be a problem, either by professionals or by patients. We did not encounter any problems with professional compliance in a previous study of pharmaceutical care within palliative care [58]. If a pharmacist leaves a participating branch, however, we shall ask for a permanent replacement and give the replacement pharmacist individual training. Furthermore patient compliance with drugs is an outcome rather than a threat.
What is the likely rate of loss to follow-up?
From East Riding data we estimate that losses from mortality (about 5%), leaving home for institutional care or elsewhere (about 10%), and non-response to questionnaires (about 20%) will not exceed 40% in total.
How many centres will be involved?
Twenty general practices – four within each of the five PCTs likely to take part. With the encouragement of the former East Riding & Hull Health Authority (ERHHA) the four PCTs within ERHHA have agreed to support the study and meet excess treatment costs. The Selby and York PCT has also agreed to do so.
What is the proposed type of analysis?
All analyses will be by 'intention to treat'. Whenever possible we shall include patients lost to follow up by using all available data, including those from pharmacies' patient medication records and general practices' repeat prescription indices. We shall analyse the five interrupted time series by the methods expounded by Box and Jenkins (1976) [74]. Within each time series the analysis will in effect compare the process and outcome data collected before training in pharmaceutical care with those collected after that training. Because the definitive analysis combines these sub-analyses, it is much more robust against external events like changes in health policy than a single time series would have been. Nevertheless because the five PCTs differ in patient characteristics, notably socio-demographic characteristics, the time series models for the four main outcome measures will take as covariates the known risk factors for drug-related adverse events We shall analyse the five multiple interrupted time series by the latest Statistical Analysis System Econometrics and Time Series (SAS/ETS) procedures [75]. In doing so we shall distinguish between four levels – PCT, practice, pharmacy and patient.
Are there any planned subgroup analyses?
To guide the implementation of PC we shall use analysis of covariance to compare effectiveness and cost-effectiveness between patients at low risk of adverse events and those at high risk. The covariates will be age, total number of drugs, and oral anti-coagulants, hypoglycaemic and non-steroidal anti-inflammatory drugs [76].
What is the proposed frequency of analyses (including any interim analyses)?
Although we shall monitor the incidence of adverse events throughout the trial, we shall analyse only once (Figure 1).
Has any pilot study been carried out using this design?
We have modelled this trial on two current studies:
A The UK BEAM trial of low back pain in 150 practices across the UK, of which ITR is principal investigator.
B The feasibility study of the use of pharmaceutical care in 'vulnerable' elderly patients in ERHHA, of which IW, HE and PDC are co-investigators.
Over what period is funding requested?
42 months (Figure 1)
Details of trial team, trial management and participating centres
What are the arrangements for day to day management of the trial?
The management structure of RESPECT has been derived from that successfully adopted by the UK BEAM trial, led by Ian Russell. Ian Wong will lead RESPECT with support from Ian Russell in York, and from Peter Campion and the trial co-ordinator in Hull. The co-ordinator will report directly to Ian Wong and take day-to-day responsibility for the conduct of the trial, including fieldwork and liaison with practices, pharmacies and patients. Under Ian Russell's supervision York University will take responsibility for trial design, remote randomisation, data management, health economics and statistical analysis. The Trial Management Group comprising applicants, collaborators, trial co-ordinator, research pharmacist, data manager, economist, statistician and both secretaries will meet monthly to manage the trial.
Authors Contributions
IW will be responsible for the clinical and scientific co-ordination of the trial. PDC will be responsible for general practice recruitment and co-ordination, and oversee the trial co-ordinating centre. SC will be responsible for the design, development and implementation of the data management and quality control strategy. BC will undertake the design, programming, maintenance, quality control and management of trial databases, and contribute to preliminary analysis and reporting. HE, GH will be responsible for the co-ordination of pharmaceutical care networking and training. AF will contribute to trial design, methods and data management and be responsible for data quality, analysis and reporting. AH will be responsible for recruitment and support of practices, pharmacists and patients from these practices; collection of data from practices, pharmacies and patients, if necessary in their homes; and the development and delivery of training materials. ZP will be responsible for the design, methods, conduct, analysis and reporting of the economic evaluation. SR will manage the trial, including support for principal investigators, co-ordination of research team, liaison with trial practices, co-ordination of data collection, and preliminary analysis and reporting. IR will take responsibility for trial design, data management and analysis and oversee the trial data centre in York. Other contributors will be listed in definitive publications.
References
Aparasu RR, Fliginger SE: Inappropriate drug prescribing for the elderly by office-based physicians. Ann Pharmacotherapy. 1997, 31: 823-9.
Lunn J, Chan K, Donoghue J, Riley B, Walley T: A study of the appropriateness of prescribing in nursing homes. Int J Pharm Pract. 1997, 5: 6-10.
Mannesse CK, Derkx FMH, de Ridder MAJ, Man in't Veld AJ, Van der Cammen TJM: Adverse drug reactions in elderly patients as contributing factor for hospital admission: cross sectional study. BMJ. 1997, 315: 1057-8.
Howard PA: Guidelines for stroke prevention in patients with atrial fibrillation. Drugs. 1999, 58: 997-1009.
Harries CM: The scale of repeat prescribing. Br J Gen Pract. 1996, 46: 549-63.
Zermansky A: Who controls the repeat?. Br J Gen Pract. 1996, 46: 643-7.
Leape LL, Brennan TA, Laird NM, Lawtheres AG, Lacolio AR, Barnes BA, Hebert L, Newhousr JP, Weiler PC, Hialt H: Nature of adverse events in hospitalized patients: results of the Harvard medical practice study II. N Engl J Med. 1991, 324: 377-84.
Gray SL, Sager M, Lestico MR, Jalaluddin M: Adverse drug events in hospitalized elderly. J Gerontol Biol Med Sci. 1998, 53: M59-63.
Thomas EJ, Brennan TA: Incidence and types of preventable adverse events in elderly patients: population based review of medical records. BMJ. 2000, 329: 741-4. 10.1136/bmj.320.7237.741.
Prescription Pricing Authority: Statistics of prescriptions dispensed in the community: England 1988 to 1998. 1999, London: HMSO
Hobbs F, Damon B: 65+ in the United States. In Current population reports. 1996, Washington: US Bureau of the Census, 23-190.
Butler RN: Population ageing and health. BMJ. 1997, 315: 1082-4.
Hepler CD, Strand LM: Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm. 1990, 47: 533-42.
Anon: Electronic prescribing and medicines management pilots next year. Pharm J. 2000, 265: 384-5.
Hanlon JT, Weinberger M, Samsa GP, Schmader KE, Uttech KM, Lewis IK, Cowper PA, Landsman PB, Cohen HJ, Feussner JR: A randomised controlled trial of a clinical pharmacist intervention to improve inappropriate prescribing in elderly outpatients with polypharmacy. Am J Med. 1996, 100: 428-37. 10.1016/S0002-9343(97)89519-8.
McMullin ST, Hennenfent JA, Ritchie DJ, Huey WY, Lonergan TP, Schaiff RA, Tonn ME, Bailey K: A prospective, randomised trial to assess the cost impact of pharmacist-initiated interventions. Arch Intern Med. 1999, 159: 2306-9. 10.1001/archinte.159.19.2306.
Department of Health: The NHS Plan – a plan for investment, a plan for reform. 2000, London: HMSO
Royal Pharmaceutical Society of Great Britain: Report on June Council meeting. 1998, London: RPSGB
United Kingdom Clinical Pharmacy Association: 2000, [http://www.ukcpa.org]
Department of Health: Review of prescribing, supply & administration of medicines. 1999, London: HMSO
Department of Health: Pharmacy in the future – implementing the NHS plan. 2000, London: HMSO
Anon: Kee** up on care. Pharm J. 2000, 264: 609.
Kennie NR, Schuster BG, Einsarson TR: Critical analysis of the pharmaceutical care research literature. Ann Pharmacotherapy. 1998, 32: 17-26. 10.1345/aph.17113.
Singhal PK, Raisch DW, Gupchup GV: The impact of pharmaceutical services in community and ambulatory care settings: evidence and recommendations for future research. Ann Pharmacotherapy. 1999, 33: 1336-55. 10.1345/aph.18440.
Sczupak CA, Conrad WF: Relationship between patient-orientated pharmaceutical services and therapeutic outcomes of ambulatory patients with diabetes mellitus. Am J Hosp Pharm. 1977, 34: 1248-42.
Hawkins DW, Fiedler FP, Douglas HL, Eschbach RC: Evaluation of a clinical pharmacist in caring for hypertensive and diabetic patients. Am Hosp Pharm. 1979, 34: 1321-5.
Gray DR, Garabedian-Ruffalo SM, Chretien SD: Cost-justification of a clinical pharmacist-managed anticoagulation clinic. Drug Intell Clin Pharm. 1985, 19: 575-80.
Lipton HL, Bird JA: The impact of clinical pharmacists' consultations on geriatric patients' compliance and medical care use: a randomised controlled trial. Gerontologist. 1994, 34: 307-15.
Jaber LA, Halapy H, Fernet M, Tummalapallis S, Diwakaran H: Evaluation of a pharmaceutical care model on diabetes management. Ann Pharmacotherapy. 1996, 30: 238-43.
Park JJ, Kelly P, Carter BL, Burgess PP: Comprehensive pharmaceutical care in the chain setting. J Am Pharm Assoc. 1996, NS36: 443-51.
Solomon DK, Portner TS, Gourley DR, Gourley GA, Holt JM, Wicke WR, Braden RL, Eberle TN, Self TFI, Lawrence BL: Clinical and economic outcomes in the hypertension and COPD arms of a multi-center outcomes study. J Am Pharm Assoc. 1998, 38: 574-85.
Plumridge RJ, Wojnar-Horton RE: Review of the pharmacoeconomics of pharmaceutical care. Pharmacoeconomics. 1998, 14: 175-89.
Carter BL, Barnette DJ, Chrischilies E, Mazzotti GJ, Asali ZJ: Evaluation of hypertensive patients after care provided by community pharmacists in a rural setting. Pharmacotherapy. 1997, 17: 1274-85.
Erickson SR, Slaughter R, Halapy H: Pharmacists' ability to influence outcomes of hypertension therapy. Pharmacotherapy. 1997, 17: 140-7.
Konzem SL, Gray DR, Kashyap ML: Effect of pharmaceutical care on optimum colestipol treatment in hypercholesterolemic veterans. Pharmacotherapy. 1997, 17: 576-83.
Gattis WA, Hasselblad V, Whellan DJ, O'Connor CM: Reduction in heart failure events by the addition of a clinical pharmacist to the heart failure management team: results of the Pharmacist in Heart Failure Assessment Recommendation and Monitoring (PHARM) study. Arch Intern Med. 1999, 13: 159-64.
Verma S, McElnay JC, Hughes CM: Pharmaceutical care of patients with congestive heart failure: intervention and outcomes. Pharmacotherapy. 1999, 19: 860-9. 10.1592/phco.19.10.860.31565.
Bond C, Matheson C, Williams S, Williams P, Donnan P: Repeat prescribing: a role for community pharmacists in controlling and monitoring repeat prescriptions. Br J Gen Pract. 2000, 50: 271-5.
Sturgess IK, McElnay JC, Hughes CM: Community pharmacy provision of pharmaceutical care to older patients: an international European study (abstract). Pharm J. 1999, 263: R8.
Bond C, Blenkinsopp A, Anderson C, Krska J: A randomised controlled trial of Merdicines Management in the community pharmacy setting. National Research Register. 2003, publication ID N0572099159
Kimberlin CL, Berardo DH, Pendergast JF, McKenzie LC: Effects of an education program for community pharmacists on detecting drug-related problems in elderly patients. Med Care. 2001, 39: 109-12.
Krska J, Cromarty JA, Arris F, Jamieson D, Hansford D, Duffus PRS, Downie G, Seymour DG: Pharmacist-led medication review in patients over 65: a randomized controlled trial in primary care. Age and Ageing. 2001, 30: 205-11. 10.1093/ageing/30.3.205.
Malone DC, Carter BL, Billups SJ, Valuck RJ, Barnette DJ, Sintek CD, Okano GJ, Ellis S, Covey D, Mason B, Jue S, Carmichael J, Guthrie K, Sloboda L, Dombrowski R, Geraets DR, Amato MG: Can clinical pharmacists affect SF36 scores in veterans at high risk for medication-related problems?. Med Care. 2001, 39: 113-22. 10.1097/00005650-200102000-00002.
Weinberger M, Murray MD, Marrero DG, Brewer N, Lykens M, Harris LE, Seshadri R, Caffrey H, Roesner JF, Smith F, Newell AJ, Collins JC, McDonald CJ, Tierney WM: Effectiveness of pharmacist care for patients with reactive airways disease: a randomized controlled trial. JAMA. 2002, 288: 1642-3.
Mason P: Pharmaceutical care: what it is and what it isn't. Pharm J. 1998, 261: 348-9.
Royal Pharmaceutical Society of Great Britain: Pharmaceutical care: the future for community pharmacy. 1992, London: RPSGB
NHS Executive: Research & development in primary care: national working group report. 1997, London: Department of Health
Medical Research Council: A framework for development of RCTs to evaluate complex interventions to improve health. London: MRC
Schwartz D, Lellouch D: Pragmatic and explanatory attitudes in clinical trials. J Chron Dis. 1967, 20: 637-644. 10.1016/0021-9681(67)90041-0.
Medical Research Council: Cluster randomised trials: methodological and ethical considerations. London: MRC
Campion PD, Russell IT, The Hull York Medical School (HYMS): A new resource for North & East Yorkshire and North Lincolnshire. Regional Review. 2002, 12: 7-8.
Cook TD, Campbell DT: Quasi experimentation: design and analysis issues for field settings. 1979, Boston, Massachusetts: Houghton Mifflin
Strand LM, Cipolle RJ, Morley PC: Pharmaceutical care: an introduction. 1992, Kalamazoo, Michigan: Upjohn
Strand LM, Morley PC, Cipolle R, Ramsey R, Lamsom GD: Drug-related problems: their structure and function. Ann Pharmacotherapy. 1990, 24: 1093-7.
Mannesse CK, Derkx FMH, de Ridder MAJ, Man in't Veld AJ, Van der Cammen TJ: Adverse drug reactions in elderly patients as contributing factor for hospital admission: cross sectional study. BMJ. 1997, 315: 1057-8.
Thomas EJ, Brennan TA: Incidence and types of preventable adverse events in elderly patients: population based review of medical records. BMJ. 2000, 329: 741-4. 10.1136/bmj.320.7237.741.
Gurwitz JH, Avorn J: The ambiguous relation between ageing and adverse drug reactions. Ann Itern Med. 1991, 114: 956-66.
Needham DS, Wong ICK, Campion PD: Evaluation of the effectiveness of UK community pharmacists' interventions in the community palliative care. Palliative Medicine. 2002, 16: 219-25. 10.1191/0269216302pm533oa.
Hanlon JT, Schmader KE, Samsa GP, Weinberger M, Uttech KM, Lewis IK, Cohen HJ, Feussner JR: A method for assessing drug therapy appropriateness. J Clin Epidemiol. 1992, 45: 1045-51. 10.1016/0895-4356(92)90144-C.
Samsa G, Hanlon JT, Schmader KE, Weinberger M, Clipp EC, Uttech KM, Lewis IK, Landsman PB, Cohen HJ: A summated score for Medication Appropriateness Index: development and assessment of clinimetric properties including content validity. J Clin Epidemiol. 1994, 47: 891-6.
Schmader K, Hanlon JT, Weinberger M, Landsman PB, Samsa GP, Lewis I, Uttech K, Cohen HJ, Feussner JR: Appropriateness of medication prescribing in ambulatory elderly patients. J Am Geriatr Soc. 1994, 42: 1241-7.
Streiner DL, Norman GR: Health measurement scales: a practical guide to their development and use. 1995, Oxford: Oxford University Press, 2
Weinberger M, Oddone EZ, Samsa GP, Landsman PB: Are health-related quality-of-life measures affected by the mode of administration?. J Clin Epidemiol. 1996, 49: 135-40. 10.1016/0895-4356(95)00556-0.
Hanlon JT, Artz MB: Drug-related problems and pharmaceutical care: what are they, do they matter, and what's next?. Med Care. 2001, 309: 109-12. 10.1097/00005650-200102000-00001.
Gandhi TK, Burstin HR, Cook F, Puopolo AL, Haas JS, Brennan TA, Bates DW: Drug complications in outpatients. J Gen Intern Med . 2000, 15: 149-54. 10.1046/j.1525-1497.2000.04199.x.
Hanlon JT, Maher R, Lindblad C, Ruby CM, Twersky J, Cohen HJ, Schmader KE: Comparison of methods to detect potential adverse drug events in frail elderly inpatients and outpatients. Am J Health Syst Pharm. 2001, 58: 1622-6.
Jarernsiripornkul N, Krska J, Richards RME, Capps PAG: Patient reporting of adverse drug reactions: useful information for pain management?. Euro J Pain. 2003, 7: 219-24. 10.1016/S1090-3801(02)00114-3.
EuroQol Group: EuroQol – a new facility for the measurement of health related quality of life. Health Policy. 1990, 16: 199-208. 10.1016/0168-8510(90)90421-9.
Russell IT, Garratt AM: The need for patient-assessed measures of health outcome. In: Vascular and endovascular opportunities. Edited by: Greenhalgh RM, Powell JT, Mitchell AW. 2000, London: WB Saunders
Donner A, Klar NS: Design and analysis of cluster randomisation trials in health research. 2000, London: Arnold
North of England Study of Standards & Performance in General Practice: Medical audit in practice: effects on doctors' clinical behaviour for common childhood conditions. BMJ. 1992, 304: 1480-4.
Altman DG: How large a sample?. In Statistics and ethics in medical research. 1981, London: BMJ
Kind P, Hardman G, Macran S: UK population norms for EQ-5D. Discussion Paper 172. 1999, York: Centre for Health Economics
Box GEP, Jenkins GM: Time series: forecasting & control. 1976, San Francisco: Holden-Day
SAS Institute Inc: SAS/ETS software: applications guide 1 version 6. 1995, Cary N, Carolina: SASII
Beyth RJ, Shorr RI: Epidemiology of adverse drug reactions in elderly by drug class. Drugs & Aging. 1999, 4 (3): 231-239.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1472-6963/4/11/prepub
Acknowledgments
The Trial Steering Committee comprises Lewis Ritchie (University of Aberdeen), Alain LiWanPo (University of Aston) and Susan Ambler (Royal Pharmaceutical Society of Great Britain). We acknowledge the support of Robert Calvert, Karen Goodyear and Andrew Hersom. In addition, John Young (Consultant Geriatrician, St Luke's Hospital, Bradford) advised on medical care of the elderly, and Mark Sculpher (Professor of Health Economics, York University) advised on health economic. Elizabeth Jones (University of Hull) provides secretarial support to the trial co-ordinating centre, including participant recruitment and data collection. Valerie Wadsworth (University of York) provides secretarial support to the trial data centre, including data collation and scanning, Bee Lian Sim (University of London) provides secretarial support to the principal investigator.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing Interest
The RESPECT Trial has been funded by the Medical Research Council and Five Primary Care Trusts in the UK (Eastern Hull, East Yorkshire, Selby & York, West Hull, and Yorkshire Wolds and Coast). IW's post is funded by the Department of Health Public Health Career Scientist Award.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Wong, I., Campion, P., Coulton, S. et al. Pharmaceutical care for elderly patients shared between community pharmacists and general practitioners: a randomised evaluation. RESPECT (Randomised Evaluation of Shared Prescribing for Elderly people in the Community over Time) [ISRCTN16932128]. BMC Health Serv Res 4, 11 (2004). https://doi.org/10.1186/1472-6963-4-11
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1472-6963-4-11