Abstract
Background
Human parvovirus B19 infection has been postulated to the anti-phospholipid syndrome (APS) in autoimmunity. However, the influence of anti-B19-VP1u antibody in autoimmune diseases is still obscure.
Methods
To elucidate the effect of anti-B19-VP1u antibodies in systemic lupus erythematosus (SLE), passive transfer of rabbit anti-B19-VP1u IgG was injected intravenously into NZB/W F1 mice.
Results
Significant reduction of platelet count and prolonged thrombocytopenia time were detected in anti-B19-VP1u IgG group as compared to other groups, whereas significant increases of anti-B19-VP1u, anti-phospholipid (APhL), and anti-double strand DNA (dsDNA) antibody binding activity were detected in anti-B19-VP1u group. Additionally, significant increases of matrix metalloproteinase-9 (MMP9) activity and protein expression were detected in B19-VP1u IgG group. Notably, phosphatidylinositol 3-phosphate kinase (PI3K) and phosphorylated extracellular signal-regulated kinase (ERK) proteins were involved in the induction of MMP9.
Conclusion
These experimental results firstly demonstrated the aggravated effects of anti-B19-VP1u antibody in disease activity of SLE.
Similar content being viewed by others
Background
Human parvovirus B19 (B19) is known as a parvovirus of human pathogen [1] that consists two structural proteins including VP1 and VP2, which are identical except for the 227 amino acids at the amino-terminal end of the VP1-protein, the so-called VP1-unique region (VP1u) [2]. Recently, B19-VP1u has been reported to have the phospholipase A2 (PLA2) motif and secreted phospholipases A2 (sPLA2) activity [3–6], and is associated with various autoimmune diseases [7].
The infection of B19 has been postulated to the generation of various autoantibodies including anti-nuclear antibody (ANA), anticardiolipin antibody (aCL), and anti-phospholipid antibody (APhL) [7–11], as well as the anti-phospholipid syndrome (APS) [8]. Notably, a significant similarity existed in the specificity of APhL between patients with B19 infection or systemic lupus erythematosus (SLE) was reported [9, 10]. Recent studies have suggested that B19 may exacerbate or even induce SLE [7, 8]. Our recent findings indicated that serum from patients with acute B19 infection have a high frequency in recognition of cardiolipin (CL) and β2GPI, and the phospholipase domain observed in the B19-VP1u may contribute to the generation of APhL [12]. Additionally, the BALB/c mice immunized with anti-B19-VP1u IgG developed thrombocytopenia, prolongation of aPTT, and autoantibody against β2GPI and PhL and suggested the association among anti-B19-VP1u IgG and production of anti-β2GPI antibodies, APhL, and APS-like autoimmunity [13].
However, no further study was performed in elucidating the effect of anti-B19-VP1u antibody on disease activity in SLE. In current study, we treated NZB/W F1 mice with passive transfer of rabbit anti-B19-VP1u antibody to investigate the effect of elicited anti-B19-VP1u antibody on diseases activity in SLE.
Methods
Preparation of recombinant human B19-VP1 unique region protein and rabbit anti-B19-VP1 unique region antibody
Construction of B19-VP1u cDNA into pET-32a expression vector (Novagene, Cambridge, MA) was performed and the recombinant B19-VP1u protein was purified as described in our recent publication [12, 13]. For generation of antisera against the B19-VP1u, four female New Zealand White rabbits were immunized subcutaneous in the neck region with 0.5 mg of purified recombinant B19-VP1u protein in Freund's complete adjuvant (Sigma, Saint Louis Mo, USA) followed by injection at two-week intervals with 0.25 mg of B19-VP1uproteininFreund'sincompleteadjuvant (Sigma, Saint Louis Mo, USA). A control group were immunized with Freund's complete adjuvant and followed by injection with Freund's incomplete adjuvant. All sera reacted specially with the B19-VP1u by immunoblotting analysis.
Animals and induction of experimental APS by passive transfer
Twenty-four female NZB/W F1 mice at age of 8 weeks were purchased from National Taiwan University, Laboratory Animal Center, Taiwan and housed under supervision of the Institutional Animal Care and Use Committee at Chung Shan Medical University, Taichung, Taiwan. Induction of experimental APS by passive transfer was performed according to the method of Blank [14]. Disease activity of mice was determined by monitoring the proteinuria biweekly with Albustix test strips from the age of 14 weeks for ten weeks as described previously [15]. All rabbit IgG were isolated using Protein A beads as described in our recent report [13, 16]. The dosage of anti-B19-VP1u IgG is based on a previous study of inducing APS in mice with anti-cardiolopin antibodies [14]. Proportionally, the common used concentration of immunoglobulins-preparations in mice is 20 ug/dosage and the titer of 20 ug rabbit anti-B19-VP1u IgG is similar to 27 U after determination and mathematics conversion (IBL-America, MN, USA) while the values of other control IgG preparations are less than 7 U. The titer greater than 12 U is considered as positive. The mice at age of 20 weeks were divided into four groups and were intravenously received rabbit anti-B19-VP1u IgG (20 ug), normal rabbit IgG (20 ug), rabbit anti-B19-NS1 IgG (20 ug), and PBS through the tail vein, respectively. The mice were then sacrificed on day 30 by CO2 asphyxiation and the heart blood samples were collected. APS clinical parameters, including thrombocytomenia and prolonged activated partial thromboplastin time [aPTT], were evaluated and the platelet counts were detected using Systemex (KX-21, KOBE, Japan). The presence of lupus anticoagulants were evaluated by the prolongation of aPTT in a mixing tests by adding 1 volume of plasma from whole blood mixed with sodium citrate 0.123 mol/l in a 9:1 ratio to 1 volume of each cephalin and incubating for 2 minutes at 37°C. Another volume of 0.025 M CaCl2 (Sigma, Saint Louis Mo, USA) was added, and the clotting time was recorded in seconds using Coatron M1 (TECO GmbH, Neufahrn NB, Germany).
ELISA
Direct antigen-specific ELISA kits were used to detect APhL IgG (Louisville APL Diagnostics, Inc. GA, USA) and anti-dsDNA IgG (INOVA Diagnostics, Inc. CA, USA) was performed as described in our recent publication [12, 13]. The color reaction was performed as described above. For detecting the binding activity of anti-B19-VP1u antibody, recombinant B19-VP1u was coated in a 96 well plate and ELISA was performed as described in our recent report [13]. The cutoff value for each ELISA experiment was obtained (mean+3SD) and the absorbance above the value is regarded as positive.
Preparation of tissue extract and determination of protein
All procedures were performed at 4°C. Liver samples obtained from NZB/W F1 mice were homogenized in 600 ul PRO-PREP™ solution (iNtRON Biotech, Korea) by 30 strokes using a Dounce Homogenizer (Knotes Glass, Vineland, NJ). The homogenates were centrifuged at 13,000 rpm for 10 minutes at 4°C and the supernatant was stored at -80°C until use. Protein concentration of tissue extracts was determined according to the method described by Bradford [17] using bovine serum albumin as standards.
Gel zymography
MMP-2 and MMP-9 activities were analyzed by gelatin-zymography assays as previously described [18]. Ten microliters of ten-fold diluted serum or 25 μg protein lysates of liver tissue from NZB/W F1 mice with passive transfer anti-idiotype antibodies were separated by an 8% Sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) gels containing 0.1% gelatin. Gels were washed for 30 min in 2.5% Triton X-100 to remove the SDS and then soaked in the reaction buffer containing 40 mM Tris-HCl, pH8.0, 10 mM CaCl2 and 0.02% NaN3 for 30 min. The reaction buffer was changed to a fresh one, and the gels were incubated at 37°C for 24 h. Gelatinolytic activity was visualized by staining the gels with 0.5% Coomassie brillant blue R-250, destained with methanol-acetic acid water, and relative MMP levels were quantitated by a gel documentation and analysis system (Appraise, Beckman-Coulter, Brea, California, USA).
Western blot
The loading sample for each lane of Western blot was a pool of four random selected mice of the same group. Protein samples were separated in 12.5 or 10% of SDS-PAGE and electrophoretically transferred to nitrocellulose membrane (Amersham Biosciences, Piscataway, NJ, USA) according to the method of Towbin [19]. After blocking with 5% non-fat dry milk in (PBS), antibodies against MMP2, MMP9, phosphatidylinositol 3-phosphate kinase (PI3K) and phosphorylated extracellular signal-regulated kinase 1/2 (p-ERK1/2), and actin (Upstates, Charlottesville, Virginia, USA) were diluted in PBS with 2.5% BSA and incubated for 1.5 hr with gentle agitation at room temperature. The membranes were then incubated with horseradish peroxidase (HRP) conjugated secondary antibody. Pierce's Supersignal West Dura HRP Detection Kit (Pierce Biotechnology Inc., Rockford, IL) was used to detect the antigen-antibody complexes. The blots were scanned and quantified by densitometry (Appraise, Beckman-Coulter, Brea, California, USA).
Statistical analyses
The paired t test and one-way ANOVA were used to analyze for statistical significance. A P value < 0.05 was considered significant.
Results
Enhanced APS-like syndrome in NZB/W F1 by passive transfer of purified rabbit anti-B19-VP1u antibody
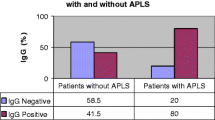
To clarify the influence of anti-B19-VP1u antibody in disease activity and development of SLE, we employed and modified the experimental model as described in our previously report by immunizing NZB/W F1 mice intravenously with various kinds of purified rabbit IgG. The body weight and various clinical parameters including, WBC, RBC, HGB, HCT, MCV, MCH and MCHC revealed no significant variation in all groups of mice (Table 1). Notably, significant decreases of platelet counts and aPTT were observed in sera from NZB/W F1 mice that were received purified rabbit anti-B19-VP1u IgG, compared to those mice that were received normal rabbit IgG, rabbit anti-B19-NS1 IgG, or PBS, respectively (Table 1). Additionally, ELISA experiments were performed to elucidate the effect of anti-B19-VP1u IgG by analyzing the binding activities of APhL antibodies in NZB/W F1 mice that were received purified rabbit anti-B19-VP1u IgG. Elevated titers of anti-B19-VP1u and APhL and anti-dsDNA antibodies were detected in serum from NZB/W F1 mice that were received purified rabbit anti-B19-VP1u IgG as compared to those mice that were received normal rabbit IgG, anti-B19-NS1 IgG, or PBS, respectively (Fig. 1).
Binding activity of various autoantibodies. Anti-sera from the 4 groups of mice were analyzed for the binding activities of (A) B19-VP1u and (B) PhL, and (C) dsDNA. Bars represent the values of optical density. *, # and ¥ indicate significant differences as compared to the PBS, IgG, or B19-NS1 group, respectively. Similar results were obtained in three independent experiments.
Enhanced MMP-9 activity and expression in liver from NZB/W F1 by passive transfer of purified rabbit anti-B19-VP1u antibody
To further examine the effect of anti-B19-VP1u antibody on pathogenesis of liver in NZB/W F1 mice, MMPs activity and protein expression were examined. Significant increase of MMP9 activity was observed in liver of NZB/W F1 mice that were received rabbit anti-B19 VP1u IgG as compared to PBS, Control IgG, or B19-NS1 IgG group, respectively (Fig. 2A). However, no significant variation was detected in MMP-2 activity among all experimental groups (Fig. 2A). The quantified results of MMP-9/MMP-2 ratio were shown in lower panel of Fig 2A. Moreover, Western blots were performed to examine the expression of MMP9 and MMP2. Significant increase of MMP-9/MMP-2 ratio was detected in B19-VP1u group as compared to PBS, Control IgG, or B19-NS1 IgG group, respectively (Fig 2B). Quantified results were shown in the lower panel of Fig 2B.
Activities and protein expression of MMP-9 andMMP-2. Liver samples obtained from the 4 groups of mice were analyzed for the (A) MMP-9 and MMP-2 activity and (B) MMP-9 and MMP-2 protein expression. The quantified results of MMP-9/MMP-2, MMP-9/actin, and MMP-2/actin ratio were shown in the lower panels, respectively. *, # and ¥ indicate significant differences as compared to the PBS, IgG, or B19-NS1 group, respectively. Similar results were obtained in three independent experiments.
Increased phosphorylation of ERK 1/2 and PI3K proteins in NZB/W F1 by passive transfer of purified rabbitanti-B19-VP1u antibody
To clarify the possible signaling pathway involved in the activation of MMP9 by B19-VP1u, various signaling molecules including, PI3K, Erk1/2-p, p38-p, and JNK-p were examined. Notably, the PI3K and phosphorylation of ERK 1/2 proteins were observed in liver from NZB/W F1 mice that were treated with rabbit anti-B19 VP1u IgG, as compared to PBS, Control IgG, or B19-NS1 IgG group, respectively (Fig 3). However, no significant variations of p38-p and JNK-p were observed in all experimental groups (data not shown). Quantified results were shown in lower panels of Fig. 3A and 3B.
Presence of PI3K and phosphorylated ERK proteins. Liver samples obtained from the 4 groups of mice were analyzed for the (A) PI3K and (B) phosphorylated ERK (ERK-p) proteins. The quantified results of PI3K/actin and ERK-p/actin ratios were shown in the lower panels, respectively. *, # and ¥ indicate significant differences as compared to the PBS, IgG, or B19-NS1 group, respectively. Similar results were obtained in three independent experiments.
Discussion
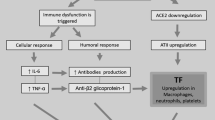
B19 infection has been implicated as a trigger of various autoimmune diseases including the induction of autoantibodies in patients with SLE [7–11]. However, the roles of B19-VP1u and anti-B19-VP1u antibody in pathogenesis of autoimmune diseases remain unclear. In current study, we demonstrated the aggravated effect of anti-B19-VP1u antibody on disease activity in SLE by analyzing the APS-like syndrome. Significant aggravated disease activities, including reduced platelet count, prolonged thrombocytopenia time, increased binding activity of autoantibody, elevated MMP9 activity and protein expression, were observed in NZB/W F1 mice that were received anti-B19-VP1u IgG as compared to those mice that were received rabbit control IgG, rabbit anti-B19-NS1 IgG or PBS, respectively.
APS-like syndrome is recognized as a striking analogy between the clinical features and hematologic findings in patients with SLE or B19 infection [7–11]. APS is characterized by raised titers of circulating APhL that bind target molecules primarily via β2GPI, and/or lupus anticoagulant in association with recurrent fetal loss, thromboembolic phenomena, thrombocytopenia, CNS, heart, and other organ involvement [20, 21]. β2GPI shares a common amino acid sequence with various microbial pathogens, and may be the cause of APS or production of the cross reacting autoantibodies [22–24]. Our previous study identified four cases of B19 infection associated with the production of aCL and anti-β2GPI antibodies [12]. Consistently, our recent study has demonstrated a spectrum of experimental APS-like autoimmunity induced by passive transfer of purified rabbit anti-B19-VP1u IgG antibodies and provided a connection between anti-B19-VP1u IgG and pathogenesis of SLE [13]. In current study, we indicated the significant increases of APS-like syndromes including increased platelet count, prolonged PTT, and increased binding activity of APhL and dsDNA in NZB/W F1 mice that were received purified anti-B19-VP1u IgG. These findings strikingly suggested the aggravated effect of anti-B19-VP1u IgG in SLE.
Numerous studies have suggested that B19-VP1u plays a crucial role in induction of anti-β2GPI and APhL antibodies [8, 9, 13]. Adsorption experiment revealed the partially reduced reactivity of anti-B19-VP1u antibody to CL and β2GPI [12], suggesting similar epitopes or conformation may exist between B19-VP1u, CL and β2GPI [8, 9, 12, 13]. These experimental results may also account for the cross-reactivity of anti-B19-VP1u antibody against CL, β2GPI, and ph ospholipid and suggest underlying mechanisms in development of APS-like syndrome such as APhL antibody. In current study, significant increase of APhL antibodies was observed in NZB/W F1 mice that were received purified rabbit anti-B19-VP1u IgG, as compared to those mice that were received control rabbit IgG, rabbit anti-B19-NS1 IgG or PBS, respectively. This finding may be due to the similar epitopes and anti-idiotype networks among anti-B19-VP1u IgG, and APhL antibody. However, the underlying mechanism is still unclear and deed merited further investigations.
Previous studies have postulated MMPs to the pathogenesis of SLE [25–28]. Cleavage of myelin basic protein or type II gelatins by MMP-9 will produce remnant epitopes and contribute to the development of autoimmunity [27, 28]. In recent studies, elevated MMP-9 activity was founded in both human and mice model with SLE [28–31] and recognized to play crucial roles in development of SLE. Additionally, various studies have indicated the involvement of ERK and PI3K in activation of MMP-9. In monocytes from patients with rheumatoid arthritis, inhibition of extracellular signal-regulated kinase (ERK) abolished Cyclosporine A-induced MMP-9 expression [32]. Another study reported that PI3K/Akt activation promotes transcriptional co-factor p300 recruitment and activation and led to increased proMMP-9 expression in rat astrocyte [33]. In current study, significant increases of MMP-9 activity and protein expression were detected in NZB/W F1 mice that were received anti-B19-VP1u IgG, as well as the increased PI3K and phosphorylated ERK proteins. These data suggest the aggravated effect of anti-B19-VP1u IgG in pathogenesis of SLE and the involvement of activation of MMP-9 via PI3K and ERK signaling pathway. It could provide clues in treatment of SLE by inhibiting PI3K and EKR signaling pathway.
Conclusion
Taken together, our experimental results firstly demonstrated the aggravated APS-like syndromes in NZB/W F1 mice that were received anti-B19-VP1u IgG. Additionally, it could provide clues in understanding the roles of anti-B19-VP1u IgG in SLE and suggest possible therapeutic potential by inhibiting PI3K or AKT signaling pathway.
References
Young NS, Brown KE: Parvovirus B19. N Engl J Med. 2004, 350: 586-597. 10.1056/NEJMra030840.
Rayment FB, Crosdale E, Morris DJ, Pattison JR, Talbot P, Clare JJ: The production of human parvovirus capsid proteins in Escherichia coli and their potential as diagnostic antigens. J Gen Virol. 1990, 71: 2665-2672. 10.1099/0022-1317-71-11-2665.
Dorsch S, Liebisch G, Kaufmann B, von Landenberg P, Hoffmann JH, Drobnik W, Modrow S: The VP1 unique region of parvovirus B19 and its constituent phospholipase A2-like activity. J Virol. 2002, 76: 2014-2018. 10.1128/JVI.76.4.2014-2018.2002.
Canaan S, Zádori Z, Ghomashchi F, Bollinger J, Sadilek M, Moreau ME, Tijssen P, Gelb MH: Interfacial enzymology of parvovirus phospholipases A2. J Biol Chem. 2004, 279: 14502-14508. 10.1074/jbc.M312630200.
Lu J, Zhi N, Wong S, Brown KF: Activation of Synoviocytes by the Secreted Phospholipase A2 Motif in the VP1-Unique Region of Parvovirus B19 Minor Capsid Protein. J Infect Dis. 2006, 193: 582-590. 10.1086/499599.
Filippone C, Zhi N, Wong S, Lu J, Kajigaya S, Gallinella G, Kakkola L, Söderlund-Venermo M, Young NS, Brown KE: VP1u phospholipase activity is critical for infectivity of full-length parvovirus B19 genomic clones. Virology. 2008, 374: 444-452. 10.1016/j.virol.2008.01.002.
Lehmann HW, Modrow S: Parvovirus B19 infection and autoimmune disease. Autoimmun Rev. 2003, 2: 218-223. 10.1016/S1568-9972(03)00014-4.
von Landenberg P, Modrow S: Human parvovirus B19 infection and antiphospholipid-syndrome: the two sides of one medal. J Vet Med B Infect Dis Vet Public Health. 2005, 52: 353-355.
von Landenberg P, Lehmann HW, Modrow S: Human parvovirus B19 infection and antiphospholipid antibodies. Autoimmun Rev. 2007, 6: 278-285. 10.1016/j.autrev.2006.09.006.
Loizou S, Cazabon JK, Walport MJ, Tait D, So AK: Similarities of specificity and cofactor dependence in serum antiphospholipid antibodies from patients with human parvovirus B19 infection and from those with systemic lupus erythematosus. Arthritis Rheum. 1997, 40: 103-108. 10.1002/art.1780400115.
von Landenberg P, Lehmann HW, Knoll A, Dorsch S, Modrow S: Antiphospholipid antibodies in pediatric and adult patients with rheumatic disease are associated with parvovirus B19 infection. Arthritis Rheum. 2003, 48: 1939-1947. 10.1002/art.11038.
Tzang BS, Tsay GJ, Lee YJ, Li C, Sun YS, Hsu TC: The association of VP1 unique region protein in acute parvovirus B19 infection and antiphospholipid antibody production. Clin Chim Acta. 2007, 378: 59-65. 10.1016/j.cca.2006.10.016.
Tzang BS, Lee YJ, Yang TP, Tsay GJ, Shi JY, Tsai CC, Hsu TC: Induction of antiphospholipid antibodies and antiphospholipid syndrome-like autoimmunity in naive mice with antibody against human Parvovirus B19 VP1 unique region protein. Clin Chim Acta. 2007, 382: 31-36. 10.1016/j.cca.2007.03.014.
Blank M, Cohen J, Toder V, Shoenfeld Y: Induction of anti-phospholipid syndrome in naive mice with mouse lupus monoclonal and human polyclonal anti-cardiolipin antibodies. Proc Natl Acad Sci USA. 1991, 88: 3069-3073. 10.1073/pnas.88.8.3069.
Hsu TC, Chiang SY, Huang CY, Tsay GJ, Yang CW, Huang CN, Tzang BS: Beneficial effects of treatment with transglutaminases inhibitor cystamine on macrophage response in NZB/W F1 mice. Exp Biol Med. 2007, 232: 195-203.
Tzang BS, Tsai CC, Chiu CC, Shi JY, Hsu TC: Up-regulation of adhesion molecule expression and induction of TNF- on vascular endothelial cells by antibody against human parvovirus B19 VP1 unique region protein. Clin Chim Acta. 2008, 395: 77-83. 10.1016/j.cca.2008.05.012.
Bradford MM: A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem. 1976, 72: 248-254. 10.1016/0003-2697(76)90527-3.
Kuo WH, Yang SF, Chu SC, Lu SO, Chou FP, Hsieh YS: Differential inductions of matrix metalloproteinase-2 and -9 in host tissues during the growth of ascitic sarcoma 180 cells in mice. Cancer Lett. 2003, 189: 103-112. 10.1016/S0304-3835(02)00323-3.
Towbin H, Staehelin T, Gordon J: Electrophoretic transfer of proteins from polyacrylamide gels to nitrocellulose sheet: procedure and some applications. Proc Natl Acad Sci USA. 1979, 76: 4350-4354. 10.1073/pnas.76.9.4350.
Blank M, Shoenfeld Y: Beta-2-glycoprotein-I, infections, antiphospholipid syndrome and therapeutic considerations. Clin Immunol. 2004, 112: 190-199. 10.1016/j.clim.2004.02.018.
Lim W, Crowther MA, Eikelboom JW: Management of antiphospholipid antibody syndrome: a systematic review. JAMA. 2006, 295: 1050-1057. 10.1001/jama.295.9.1050.
Shoenfeld Y, Blank M, Cervera R, Font J, Raschi E, Meroni PL: Infectious origin of the antiphospholipid syndrome. Ann Rheum Dis. 2006, 65: 2-6. 10.1136/ard.2005.045443.
Harel M, Aron-Maor A, Sherer Y, Blank M, Shoenfeld Y: The infectious etiology of the antiphospholipid syndrome: links between infection and autoimmunity. Immunobiology. 2005, 210: 743-747. 10.1016/j.imbio.2005.10.004.
Gharavi EE, Chaimovich H, Cucurull E, Celli CM, Tang H, Wilson WA, Gharavi AE: Induction of antiphospholipid antibodies by immunization with synthetic viral and bacterial peptides. Lupus. 1999, 8: 449-455. 10.1177/096120339900800607.
Goetzl EJ, Banda MJ, Leppert D: Matrix metalloproteinases and immunity. J Immunol. 1996, 156: 1-4.
Zucker S, Hymowitz M, Conner C, Zarrabi HM, Hurewitz AN, Matrisian L, Boyd D, Nicolson G, Montana S: Measurement of matrix metalloproteinases and tissue inhibitors of metalloproteinases in blood and tissues. Clinical and experimental applications. Ann N Y Acad Sci. 1999, 878: 212-227. 10.1111/j.1749-6632.1999.tb07687.x.
Opdenaker G, Steen Van der PE, Van Damme J, Gelatinase B: A turner and amplifier of immune functions. Trends Immunol. 2001, 22: 571-579. 10.1016/S1471-4906(01)02023-3.
Ram M, Sherer Y, Shoenfeld Y: Matrix Metalloproteinase-9 and autoimmune diseases. J Clin Immunol. 2006, 26: 299-307. 10.1007/s10875-006-9022-6.
Faber-Elmann A, Sthoeger Z, Tcherniack A, Dayan M, Mozes E: Activity of matrix metalloproteinase-9 is elevated in sera of patients with systemic lupus erythematosus. Clin Exp Immunol. 2002, 127: 393-398. 10.1046/j.1365-2249.2002.01758.x.
Ainiala H, Hietaharju A, Dastidar P, Loukkola J, Lehtimäki T, Peltola J, Korpela M, Heinonen T, Nikkari ST: Increased serum matrix metalloproteinase 9 levels in systemic lupus erythematosus patients with neuropsychiatric manifestations and brain magnetic resonance imaging abnormalities. Arthritis Rheum. 2004, 50: 858-865. 10.1002/art.20045.
Hsu TC, Chen YC, Lai WX, Chiang SY, Huang CY, Tzang BS: Beneficial effects of treatment with cystamine on brain in NZB/W F1 mice. Eur J Pharmacol. 2008, 591: 307-314. 10.1016/j.ejphar.2008.06.078.
Yang Y, Lu N, Zhou J, Chen ZN, Zhu P: Cyclophilin A up-regulates MMP-9 expression and adhesion of monocytes/macrophages via CD147 signalling pathway in rheumatoid arthritis. Rheumatology. 2008, 47: 1299-310. 10.1093/rheumatology/ken225.
Wu CY, Hsieh HL, Sun CC, Tseng CP, Yang CM: IL-1 beta induces proMMP-9 expression via c-Src-dependent PDGFR/PI3K/Akt/p300 cascade in rat brain astrocytes. J Neurochem. 2008, 105: 1499-1512. 10.1111/j.1471-4159.2008.05318.x.
Acknowledgements
All experiments were performed in accordance with the guidelines of the Ethics Committee of Institutional Animal Care, Chung Shan Medical University, Taichung, Taiwan. This study was supported by the grant NSC 97-2314-B-040-009 from the National Science Council, Taiwan, Republic of China.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
CCT performed the animal study, ELISA, zymography, and Western blotting. BST conceived this study, drafted the manuscript, and performed the performed statistical analyses. SYC and GJH provided material support and encouragement for this work. TCH provided material support and direction, and drafted significant portions of the manuscript.
Chun-Chou Tsai, Bor-Show Tzang contributed equally to this work.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Tsai, CC., Tzang, BS., Chiang, SY. et al. Increased expression of Matrix Metalloproteinase 9 in liver from NZB/W F1 mice received antibody against human parvovirus B19 VP1 unique region protein. J Biomed Sci 16, 14 (2009). https://doi.org/10.1186/1423-0127-16-14
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1423-0127-16-14