Abstract
Auditory evoked potential (AEP) is an effective index for the effects of general anesthetics. However, it’s unknown if AEP can differentiate the effects of general anesthetics on nerve fibers and synapses. Presently, we investigated AEP latency and amplitude changes to different acoustic intensities during pentobarbital anesthesia. Latency more regularly changed than amplitude during anesthesia. AEP Latency monotonically decreased with acoustic intensity increase (i.e., latency-intensity curve) and could be fitted to an exponential decay equation, which showed two components, the theoretical minimum latency and stimulus-dependent delay. From the latency-intensity curves, the changes of these two components (∆L and ∆I) were extracted during anesthesia. ∆L and ∆I monitored the effect of pentobarbital on nerve fibers and synapses. Pentobarbital can induce anesthesia and two side effects, hypoxemia and hypothermia. The hypoxemia was not related with ∆L and ∆I. However, ∆L was changed by the hypothermia, whereas ∆I was changed by the hypothermia and anesthesia. Therefore, we conclude that, AEP latency is superior to amplitude for the effects of general anesthetics, ∆L monitors the effect of hypothermia on nerve fibers and ∆I monitors a combined effect of anesthesia and hypothermia on synapses. When eliminating the temperature factor, ∆I monitors the anesthesia effect on synapses.
Similar content being viewed by others
Introduction
Precisely estimating the effects of general anesthetics is advantageous to decreasing the incidence of intra-operative awareness1, maintaining the hemodynamics more stable and reducing the requirements for intra-operative general anesthetics, fluids and vasopressors2. It is necessary to continually estimate the effects of general anesthetics during anesthesia to avoid excessively deep or light anesthesia. Because auditory evoked potential is easy to be recorded and sensitive to general anesthetics3,4, it has been widely used as a measure of the effects of general anesthetics5,6. Generally, AEP is characterized by its latency (the time from stimulus beginning to the AEP wave peak) and amplitude (the voltage of the wave peak). AEP latency monotonically increases in a concentration-dependent manner during anesthesia7,8,9,10,11,12,13, while AEP amplitude can decrease7,8,9,10,11,12,13, increase14 or change in multiple manners during anesthesia15. These results suggest that AEP latency is superior to amplitude for reflecting the effects of general anesthetics. It is well known that general anesthetics have effects on both nerve fibers16,17,18 and synapses16,19,20. However, it is unknown whether or not the AEP latency change during anesthesia can reflect the effects of general anesthetics on nerve fibers and synapses.
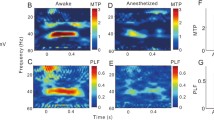
Although some auditory neurons exhibited paradoxical latency shifts (i.e., the spike latency increases with acoustic intensity increase) in bats21,22 or a much smaller/independent latency change with acoustic intensity in bats and gerbils23,24,25, the first spike latency decreases as the acoustic intensity increases (i.e., the latency-intensity curve) in the inferior colliculus (IC) of mice and cats26,Fig. 2f, the cyan curve, R2 = 0.147). The fitting resulted in the residual of each data. The residual, i.e., the difference between the actual value and the regression predicted value, can reflect the degree of variation of each data point. The absolute values of residuals obtained by fitting normalized A80-time curves were larger than those obtained by fitting normalized L80-time curves (Fig. 2g, 2 Independent Samples Tests, Z = −12.519, P = 5.890 × 10−36). Therefore, the AEP L80 from all mice changed with more regularity and less variability than the AEP A80 during pentobarbital anesthesia.
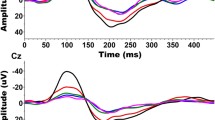
Changes in AEP latency and amplitude to various acoustic intensities during anesthesia
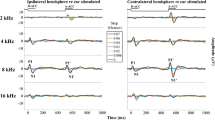
Although AEP L80 exhibited more regular and less variable changes than A80, whether AEPs to acoustic stimuli at other intensities undergo similar changes during anesthesia is still unclear. Therefore, we applied multiple acoustic intensities other than 80 dB to the subjects. The latency to each acoustic intensity (No. 18 mouse (M20110417)) showed an initial increase followed by a gradual decrease during anesthesia (Fig. 3a). The maximal latency to each acoustic intensity always occurred in the same recording session (Fig. 3a, the vertical green line). The latency change ranges (the maximal latency—the minimal latency) to different acoustic intensities were, respectively, 13.475, 12.344, 8.935, 6.23, 6.147 and 5.41 ms from 40 dB to 90 dB at 10 dB intervals and were negatively correlated with the acoustic intensity. These results indicated that AEP latencies to low intensity acoustic stimuli were more suitable for reflecting the effects of general anesthetics.
Changes in AEP latency and amplitude to different acoustic intensities.
(a,b) Changes in latency and amplitude to 40–90 dB acoustic stimuli with anesthesia time, hereafter, latency- and amplitude-time curves. (c and d) R2 values and absolute values of residuals obtained by fitting normalized latency- and amplitude-time curves (computing methods were similar to those in Fig. 2) (*P < 0.05, **P < 0.01, 2 Independent Samples Tests).
Although the amplitude (No. 18 mouse (M20110417)) also increased and then decreased during anesthesia to a given intensity acoustic stimulus, less regularity was found (Fig. 3b). Generally, the amplitude change to higher acoustic intensity was at a higher level (Fig. 3b. the curves for 40–80 dB). However, the amplitude change to a 90 dB acoustic stimulus (Fig. 3b, the black line with squares) decreased paradoxically when compared with those to 70 and 80 dB (Fig. 3b, the blue line with triangles and red line with circles). The maximal amplitudes to different acoustic intensities occurred in different recording sessions (Fig. 3b). Furthermore, the amplitude change ranges (the maximal amplitude—the minimal amplitude) to different acoustic intensities were, respectively, 0.132, 0.202, 0.137, 0.148, 0.16 and 0.178 mV from 40 dB to 90 dB at 10 dB intervals and showed little regular change with acoustic intensity increase.
When we applied the same methods as those in Fig. 2e to latency- and amplitude-time curves in Fig. 3a,b, at any acoustic intensity, the R2 value of fitting the normalized latency-time curve was larger than that of fitting the normalized amplitude-time curve (Fig. 3c). The fitting R2 values at low intensity acoustic stimuli (40, 50, 60 and 70 dB in latency; 40 dB in amplitude) were larger than those at high-intensity acoustic stimuli (80 and 90 dB in latency; 50, 60, 70, 80 and 90 dB in amplitude) (Fig. 3c). Additionally, at any acoustic intensity, the absolute values of residuals of fitting normalized latency-time curves were smaller than those of fitting the normalized amplitude-time curve, although at 40 and 50 dB, there was no statistically significant difference between two absolute values of residuals (Fig. 3d, 2 Independent Samples Tests). For latency, the absolute values of residuals of fitting at various intensity acoustic stimuli were similar to each other (Fig. 3d, the blue column). For amplitude, the absolute values of residuals of fitting at low intensity acoustic stimuli (40 and 50 dB) were smaller than those at high intensity acoustic stimuli (60, 70, 80 and 90 dB) (Fig. 3d, the cyan column).
Extracting changes in nerve fibers and synapses from AEP latencies during anesthesia
Recently, we have developed a method (DCASF) to first spike latency-intensity curves recorded in single cells, to extract changes in the theoretical minimum and stimulus-dependent components of latency57. The penetration depth was 100–1800 μm from the surface of the ICC. During penetration, the AEP was detected with a sample rate of 25 kHz by presenting 50 ms noise bursts (60 dB) to the mouse. The electrical signals were amplified 10,000 times, filtered by a band-pass of 10–300 Hz with a digital amplifier RA16 and recorded and displayed with Brain Ware software.
After AEP was detected in the ICC, a frequency scan (F-scan) was performed in which pure tone bursts (from 2 to 64 kHz in 1 kHz steps, 80 dB SPL, 50 ms duration, 5 ms rise-fall time) were randomly presented at a rate of 1/s with 10 repetitions to identify the BF of the recording site (Fig. 1c). Then, the mouse was anesthetized with sodium pentobarbital (60–70 mg/kg i.p.). Once the mouse was immobilized on the table without paw withdrawal (approximately five minutes after pentobarbital injection), an intensity scan (I-scan) was performed and was repeated every 10 min until the mouse limbs autonomously moved and paw withdrawal occurred. In this scan, the frequencies of pure tone bursts (50 ms duration with a 5 ms rise-fall time) were set at BF and were randomly presented from 30 to 90 dB SPL in 10 dB steps at a rate of 1/s and repeated 10 times. The AEPs (time window: 500 ms after stimulus onset) and the acoustic stimuli parameters in a recording session were recorded and stored in a DAM file.
The exposed brain was treated with physiological saline continuously to prevent the tissue from drying and the pinnae were maintained as in a normal awake mouse during recording. After the recording, pontamine sky blue was iontophoretically (~20 μA, 15 min) applied to the recording site with a microiontophoresis (Neurophore BH-2, Holliston, MA) to confirm the recording location in ICC. Data recorded outside the ICC were discarded.
The above AEP recording was performed without body warming, temperature monitoring and SPO2 monitoring for mice. Pentobarbital can induce hypothermia35 and hyoxemia34. And hypothermia51 and hyoxemia45 can change AEP. To analyze the effects of hypothermia and hyoxemia on AEP, the rectal temperatures (home-made thermometer) of eleven mice and the SPO2 (pulse oximetry, Nellcor, N-550) of five mice were measured every 10 min after pentobarbital injection without body warming. In addition, with body warming (home-made homeothermic blanket), rectal temperature monitoring and SPO2 monitoring, AEP was also re-recorded in five mice, as AEP recording in mice without body warming.
Ketamine, urethane and sodium pentobarbital are three common anesthetics for animal experiments. Ketamine is usually mixed with other anesthetics for use58. Urethane has a long anesthesia time59. Thus, we chose sodium pentobarbital for our experiment, as it can be used alone and has a relatively short anesthesia time (2–3 h, preliminary experimental data). In addition, noises and clicks with a wider frequency range can activate more auditory pathways60. Therefore, tones, which activate a relatively simple auditory pathway, were chosen as the acoustic stimuli to reduce data variability.
Data processing
For off-line data processing, we employed a custom-made Matlab program. First, we extracted and averaged the ten AEPs corresponding to each identical stimulus to measure the latency and amplitude. Then, we plotted the latencies and amplitudes of AEPs against anesthesia time and acoustic intensities. To fit latency-intensity curves, DCASF (for details, see Results) was used. With this fitting method, we obtained latency and intensity shifts (∆L and ∆I, respectively) of all latency-intensity curves. Then, we plotted ∆L and ∆I against anesthesia time. Next, the SPO2 and temperatures were also plotted against anesthesia time. In addition, the L80-, A80-, ∆L-, ∆I- and temperature-time curves were normalized and fit with a polynomial regression equation (polynomial order = 4). After this fitting, five groups of absolute values of residuals were obtained and compared.
The values of relevant parameters were calculated in Microsoft Excel software (version 2003). All statistical analysis was performed in SPSS statistical software (version 13). Before performing appropriate parametric statistics, datasets were first tested for normal distribution (Shapiro-Wilk test) and equal variances (Levene test). Normally distributed data were presented in figures as mean ± SD. Non-normally distributed data were presented in figures as P25, P50 , P75 and mean ± SD. For two-group comparisons, unpaired t test (Normally distributed data) or 2 Independent Samples Tests (Non-normally distributed data) was applied to test significance (two-tailed). For three or more group comparisons, one-way ANOVA (Normally distributed data) or K Independent Samples Tests (Non-normally distributed data) was applied to test significance (two-tailed). For one-way ANOVA, LSD’s test was used to further compare group means. For K Independent Samples Tests, 2 Independent Samples Tests was used to further compare any two group data. In most cases, a p-value less than 0.05 was deemed significant. However, in multiple comparison 2 Independent Samples Tests, a p-value less than 0.008 (0.05/6) was deemed significant. The data fitting and plotting were carried out in OriginPro software (version 8). The figures were arranged in Canvas software (version 9).
Additional Information
How to cite this article: Huang, B. et al. Latency of auditory evoked potential monitoring the effects of general anesthetics on nerve fibers and synapses. Sci. Rep. 5, 12730; doi: 10.1038/srep12730 (2015).
References
Schwender, D., Daunderer, M., Klasing, S., Conzen, P., Finsterer, U. & Peter, K. [Intraoperative awareness and auditory evoked potentials]. Der Anaesthesist 45 Suppl 1, S46–51 (1996).
Jildenstal, P. K., Hallen, J. L., Rawal, N., Gupta, A. & Berggren, L. Effect of auditory evoked potential-guided anaesthesia on consumption of anaesthetics and early postoperative cognitive dysfunction: a randomised controlled trial. European journal of anaesthesiology 28, 213–219 (2011).
Stronks, H. C., Aarts, M. C. & Klis, S. F. Effects of isoflurane on auditory evoked potentials in the cochlea and brainstem of guinea pigs. Hearing research 260, 20–29 (2010).
Szalda, K. & Burkard, R. The effects of nembutal anesthesia on the auditory steady-state response (ASSR) from the inferior colliculus and auditory cortex of the chinchilla. Hearing research 203, 32–44 (2005).
Thornton, C. & Sharpe, R. M. Evoked responses in anaesthesia. British journal of anaesthesia 81, 771–781 (1998).
Plourde, G. Auditory evoked potentials. Best practice & research. Clinical anaesthesiology 20, 129–139 (2006).
Goto, T., Nakata, Y., Saito, H., Ishiguro, Y., Niimi, Y., & Morita, S. The midlatency auditory evoked potentials predict responsiveness to verbal commands in patients emerging from anesthesia with xenon, isoflurane and sevoflurane but not with nitrous oxide. Anesthesiology 94, 782–789 (2001).
Sainz, M., Martinez, F., Ciges, M., De Carlos, R. & De La Cruz, T. Brainstem and middle latency auditory evoked responses in rabbits with halothane anaesthesia. Acta oto-laryngologica 103, 613–619 (1987).
Saito, T., Takeichi, S., Tokunaga, I., Nakajima, Y., Osawa, M. & Yukawa, N. Experimental studies on effects of barbiturate on electroencephalogram and auditory brain-stem responses. Nihon hoigaku zasshi=The Japanese journal of legal medicine 51, 388–395 (1997).
Savoia, G., Esposito, C., Belfiore, F., Amantea, B. & Cuocolo, R. Propofol infusion and auditory evoked potentials. Anaesthesia 43 Suppl, 46–49 (1988).
Schwender, D., Klasing, S., Conzen, P., Finsterer, U., Pöppel, E. & Peter, K. Midlatency auditory evoked potentials during anaesthesia with increasing endexpiratory concentrations of desflurane. Acta anaesthesiologica Scandinavica 40, 171–176 (1996).
Thornton, C., Catley, D. M., Jordan, C., Lehane, J. R., Royston, D. & Jones, J. G. Enflurane anaesthesia causes graded changes in the brainstem and early cortical auditory evoked response in man. British journal of anaesthesia 55, 479–486 (1983).
Thornton, C., Heneghan, C. P., Navaratnarajah, M., Bateman, P. E. & Jones, J. G. Effect of etomidate on the auditory evoked response in man. British journal of anaesthesia 57, 554–561 (1985).
Church, M. W. & Shucard, D. W. Pentobarbital-induced changes in the mouse brainstem auditory evoked potential as a function of click repetition rate and time postdrug. Brain research 403, 72–81 (1987).
Shaw, N. A. The effect of pentobarbital on the auditory evoked response in the brainstem of the rat. Neuropharmacology 25, 63–69 (1986).
Barker, J. L. & Ransom, B. R. Pentobarbitone pharmacology of mammalian central neurones grown in tissue culture. The Journal of physiology 280, 355–372 (1978).
Blaustein, M. P. Barbiturates block sodium and potassium conductance increases in voltage-clamped lobster axons. The Journal of general physiology 51, 293–307 (1968).
Narahashi, T., Frazier, D. T., Deguchi, T., Cleaves, C. A. & Ernau, M. C. The active form of pentobarbital in squid giant axons. The Journal of pharmacology and experimental therapeutics 177, 25–33 (1971).
Pittson, S., Himmel, A. M. & MacIver, M. B. Multiple synaptic and membrane sites of anesthetic action in the CA1 region of rat hippocampal slices. BMC neuroscience 5, 52 (2004).
Ito, S., Sugiyama, H., Kitahara, S., Ikemoto, Y. & Yokoyama, T. Effects of propofol and pentobarbital on calcium concentration in presynaptic boutons on a rat hippocampal neuron. Journal of anesthesia 25, 727–733 (2011).
Hechavarría, J. C., Cobo, A. T., Fernández, Y., Macías, S., Kössl, M. & Mora, E. C. Sound-evoked oscillation and paradoxical latency shift in the inferior colliculus neurons of the big fruit-eating bat, Artibeus jamaicensis. Journal of comparative physiology. A, Neuroethology, sensory, neural and behavioral physiology 197, 1159–1172 (2011).
Ma, X. & Suga, N. Corticofugal modulation of the paradoxical latency shifts of inferior collicular neurons. Journal of neurophysiology 100, 1127–1134 (2008).
Suga, N. Amplitude spectrum representation in the Doppler-shifted-CF processing area of the auditory cortex of the mustache bat. Science 196, 64–67 (1977).
Klug, A., Khan, A., Burger, R. M., Bauer, E. E., Hurley, L. M., Yang, L., Grothe, B., Halvorsen, M. B. & Park, T. J. Latency as a function of intensity in auditory neurons: influences of central processing. Hearing research 148, 107–123 (2000).
Covey, E. & Casseday, J. H. The monaural nuclei of the lateral lemniscus in an echolocating bat: parallel pathways for analyzing temporal features of sound. The Journal of neuroscience : the official journal of the Society for Neuroscience 11, 3456–3470 (1991).
Heil, P. Auditory cortical onset responses revisited. I. First-spike timing. Journal of neurophysiology 77, 2616–2641 (1997).
Tan, X., Wang, X., Yang, W. & **ao, Z. First spike latency and spike count as functions of tone amplitude and frequency in the inferior colliculus of mice. Hearing research 235, 90–104 (2008).
Liang, F., Yang, W., Zheng, X., Wang, X., Tan, X., Zhang, F. & **ao, Z. Response property of inferior collicular neurons inherited from peripheral origin in mouse. Brain research 1369, 46–59 (2011).
Wang, N., Bo, L., Zhang, F., Tan, X. & **ao, Z. An approach to identify the functional transduction and transmission of an activated pathway. Chinese Science Bulletin 58, 1274–1284 (2013).
Picton, T. W., Hillyard, S. A., Krausz, H. I. & Galambos, R. Human auditory evoked potentials. I. Evaluation of components. Electroencephalography and clinical neurophysiology 36, 179–190 (1974).
Daunderer, M., Feuerecker, M.S., Scheller, B., Pape, N. B., Schwender, D. & Kuhnle, G. E. Midlatency auditory evoked potentials in children: effect of age and general anaesthesia. British journal of anaesthesia 99, 837–844 (2007).
Alpiger, S., Helbo-Hansen, H. S. & Jensen, E. W. Effect of sevoflurane on the mid-latency auditory evoked potentials measured by a new fast extracting monitor. Acta anaesthesiologica Scandinavica 46, 252–256 (2002).
Fudickar, A., Kluzik, A., Weiler, N., Scholz, J., Tonner, P. H. & Bein, B. A comparison of auditory evoked potentials derived from a monitor integrated module versus standard technique. Journal of neurosurgical anesthesiology 21, 120–126 (2009).
Schwarzkopf, T. M., Horn, T., Lang, D. & Klein, J. Blood gases and energy metabolites in mouse blood before and after cerebral ischemia: the effects of anesthetics. Exp Biol Med (Maywood) 238, 84–89 (2013).
Kiyatkin, E. A. & Brown, P. L. Brain and body temperature homeostasis during sodium pentobarbital anesthesia with and without body warming in rats. Physiology & behavior 84, 563–570 (2005).
Kuhnle, G. E., Hornuss, C., Lenk, M., Salam, A. P., Wiepcke, D., Edelmann-Gahr, V., Flake, G., Daunderer, M., Oberhauser, M., Müller, H. H. & Feuerecker, M. Impact of propofol on mid-latency auditory-evoked potentials in children. British journal of anaesthesia 110, 1001–1009 (2013).
Palm, S., Linstedt, U., Petry, A. & Wulf, H. Dose-response relationship of propofol on mid-latency auditory evoked potentials (MLAEP) in cardiac surgery. Acta anaesthesiologica Scandinavica 45, 1006–1010 (2001).
Schwender, D., Daunderer, M., Mulzer, S., Klasing, S., Finsterer, U. & Peter, K. Midlatency auditory evoked potentials predict movements during anesthesia with isoflurane or propofol. Anesthesia and analgesia 85, 164–173 (1997).
Feuerecker, M., Lenk, M., Flake, G., Edelmann-Gahr, V., Wiepcke, D., Hornuss, C., Daunderer, M., Müller, H. H. & Kuhnle, G. E. Effects of increasing sevoflurane MAC levels on mid-latency auditory evoked potentials in infants, schoolchildren and the elderly. British journal of anaesthesia 107, 726–734 (2011).
Iselin-Chaves, I. A., El Moalem, H. E., Gan, T. J., Ginsberg, B. & Glass, P. S. Changes in the auditory evoked potentials and the bispectral index following propofol or propofol and alfentanil. Anesthesiology 92, 1300–1310 (2000).
Henry, K. R. Differential changes of auditory nerve and brain stem short latency evoked potentials in the laboratory mouse. Electroencephalography and clinical neurophysiology 46, 452–459 (1979).
Picton, T. W. in Current Practice of Clinical Electroencephalography, 2nd edn (eds D. D., Daly & T. A., Pedley ) 625–678 (Raven Press, 1990).
Kuwada, S., Batra, R. & Stanford, T. R. Monaural and binaural response properties of neurons in the inferior colliculus of the rabbit: effects of sodium pentobarbital. Journal of neurophysiology 61, 269–282 (1989).
Goldstein, A. & Aronow, L. The durations of action of thiopental and pentobarbital. The Journal of pharmacology and experimental therapeutics 128, 1–6 (1960).
Inagaki, M., Kaga, M., Isumi, H., Hirano, S., Takashima, S. & Nanba, E. Hypoxia-induced ABR change and heat shock protein expression in the pontine auditory pathway of young rabbits. Brain research 757, 111–118 (1997).
Okutan, V., Demirkaya, S., Lenk, M. K., Hamamcioğlu, K., Unay, B., Vural, O. & Gökçay, E. Auditory brainstem responses in children with congenital heart disease. Pediatr Int 41, 620–623 (1999).
Goldman, Z., Sohmer, H., Godfrey, C. & Manheim, A. Auditory nerve, brainstem and cortical response correlates of learning capacity. Physiology & behavior 26, 637–645 (1981).
Benita, M. & Conde, H. Effects of local cooling upon conduction and synaptic transmission. Brain research 36, 133–151 (1972).
Katz, B. & Miledi, R. The effect of temperature on the synaptic delay at the neuromuscular junction. The Journal of physiology 181, 656–670 (1965).
Weight, F. F. & Erulkar, S. D. Synaptic transmission and effects of temperature at the squid giant synapse. Nature 261, 720–722 (1976).
Markand, O. N., Lee, B. I., Warren, C., Stoelting, R. K., King, R. D., Brown, J. W. & Mahomed, Y. Effects of hypothermia on brainstem auditory evoked potentials in humans. Annals of neurology 22, 507–513 (1987).
Richards, C. D. The actions of pentobarbitone, procaine and tetrodotoxin on synaptic transmission in the olfactory cortex of the guinea-pig. British journal of pharmacology 75, 639–646 (1982).
Jensen, E. W., Nygaard, M. & Henneberg, S. W. On-line analysis of middle latency auditory evoked potentials (MLAEP) for monitoring depth of anaesthesia in laboratory rats. Medical engineering & physics 20, 722–728 (1998).
Pesaran, B. Uncovering the mysterious origins of local field potentials. Neuron 61, 1–2 (2009).
Stiebler, I. & Ehret, G. Inferior colliculus of the house mouse. I. A quantitative study of tonotopic organization, frequency representation and tone-threshold distribution. J Comp Neurol 238, 65–76 (1985).
Willott, J. F. Changes in frequency representation in the auditory system of mice with age-related hearing impairment. Brain research 309, 159–162 (1984).
Yu, X., Wadghiri, Y. Z., Sanes, D. H. & Turnbull, D. H. In vivo auditory brain map** in mice with Mn-enhanced MRI. Nature neuroscience 8, 961–968 (2005).
Zhou, Y., Liu, B. H., Wu, G. K., Kim, Y. J., **ao, Z., Tao, H. W. & Zhang, L. I. Preceding inhibition silences layer 6 neurons in auditory cortex. Neuron 65, 706–717 (2010).
Koblin, D. D. Urethane: help or hindrance?Anesthesia and analgesia 94, 241–242 (2002).
Narayan, S. S., Temchin, A. N., Recio, A. & Ruggero, M. A. Frequency tuning of basilar membrane and auditory nerve fibers in the same cochleae. Science 282, 1882–1884 (1998).
Acknowledgements
This work was supported by grants from Science and Technology Planning Project of Guangdong Province (2012A032200017 to Z **ao and 2012B010100024 to J **ao), the National Natural Science Foundation of China (U1301225, 31171059) and a 973 program (2014CB943002) to Z **ao.
Author information
Authors and Affiliations
Contributions
Z.X. and J.X. conceived and designed the experiments. B.H. and F.L. performed the experiments. B.H. and F.L. and analyzed the data. F.L., L.Z., M.L., J.Y. and L.Y. contributed reagents/materials/analysis tools. Z.X. wrote the paper.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Huang, B., Liang, F., Zhong, L. et al. Latency of auditory evoked potential monitoring the effects of general anesthetics on nerve fibers and synapses. Sci Rep 5, 12730 (2015). https://doi.org/10.1038/srep12730
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep12730
- Springer Nature Limited
This article is cited by
-
Nanoporous graphene-based thin-film microelectrodes for in vivo high-resolution neural recording and stimulation
Nature Nanotechnology (2024)