Abstract
Nicotine-induced dopamine (DA) release constitutes a pharmacological probe of the DA system that has potential use in patients with schizophrenia, who have abnormally elevated DA release after amphetamine administration and possibly abnormalities in nicotinic signaling. We performed positron emission tomography studies in five rhesus monkeys that received i.v. nicotine doses ranging from 0.01 to 0.06 mg/kg. [11C]raclopride was administered with either a bolus plus constant infusion or with paired bolus injections. The dynamics of D-2-binding potential (BP) after nicotine administration were studied and compared to amphetamine. Nicotine caused a significant albeit small reduction (5%, p<0.03) in BP, regardless of methodology of tracer administration. This effect disappeared 2.5 h after nicotine administration. Amphetamine caused much larger and prolonged displacement of [11C]raclopride as compared to nicotine. There was no correlation between changes in BP and nicotine dose or plasma level. Regional differences in the nicotine effect within the basal ganglia were not found. Our data are consistent with the increase in DA detected with microdialysis in animals after acute nicotine administration, however, a larger effect size would be desirable to attempt studies comparing human smokers with and without schizophrenia.
Similar content being viewed by others
INTRODUCTION
The interaction between dopaminergic and nicotinic neurotransmitter systems may be important to understand the neuropharmacology of schizophrenia. Abundant evidence indicates that both dopamine (DA) and nicotine pathways are affected in schizophrenia, but it is unknown how the two interact in this illness. For example, D2 blockers are effective treatment for psychosis, and patients with schizophrenia are much more likely to smoke tobacco and to be heavier smokers than the general population or other psychiatric patients (Dalack et al, 1998; de Leon et al, 1995; Diwan et al, 1998; Olincy et al, 1997). Patients with schizophrenia have excessive DA release in the striatum after challenge with amphetamine (Breier et al, 1997; Laruelle et al, 1996,1999) and after relative DA depletion (Abi-Dargham et al, 2000).
There is also substantial evidence that nicotinic function interacts with and regulates dopaminergic and glutamatergic neurons, both of which are likely to play a role in schizophrenia. DA is released in the striatum of animals who receive nicotine infusions (Di Chiara, 2000; Di Chiara and Imperato, 1988; Pontieri et al, 1996). Nicotinic receptors appear to be present on the cell bodies of DA neurons in the ventral tegmental area (VTA) (Pidoplichko et al, 1997). The activation of DA neurons in the VTA and the consequent release of DA in the nucleus accumbens are thought to underlie the rewarding effects of nicotine and other drugs of abuse (Di Chiara, 2000; Di Chiara and Imperato, 1988; Pontieri et al, 1996). Moreover, it has been recently shown that acetylcholine in the striatum is necessary for DA release induced by action potentials and that this regulatory effect of acetylcholine is mediated by nicotinic receptors (Zhou et al, 2001). Nicotine also appears to facilitate glutamatergic neurotransmission in the prefrontal cortex and the hippocampus (Gioanni et al, 1999; Gray et al, 1996; Radcliffe et al, 1999; Vidal and Changeux, 1993), which is in turn thought to enhance DA release in the accumbens (reviewed in Dalack et al, 1998). The effects of nicotine on hippocampal glutamatergic tone appear to underlie its effects on sensory gating in animals (Leonard et al, 1996), a phenomenon that has been found to be altered in schizophrenia and restored by smoking tobacco (Adler et al, 1993).
It would therefore be of interest to assess DA release after nicotine administration in patients with schizophrenia in vivo. In principle, this might be done by measuring the change in binding potential (BP) of [11C]raclopride or other reversible tracers for DA receptors using positron emission tomography (PET). These ligands allow for a dynamic equilibrium in the synapse with endogenous DA. Therefore, perturbations of DA release may alter the apparent BP of the ligand to DA receptors. Several studies have shown the feasibility of this technique and such measurements have been performed with drugs that act directly on the DA system, for example, amphetamine (Breier et al, 1997; Carson et al, 1997; Dewey et al, 1993) and cocaine (Schlaepfer et al, 1997), and drugs that cause DA release indirectly, for example, ketamine (Breier et al, 1998) or serotonergic agents (Dewey et al, 1995). Such experiments have been conducted in patients with schizophrenia with amphetamine administration (Breier et al, 1997; Laruelle et al, 1996); amphetamine, however, has the potential to cause short-term exacerbation of psychosis. Therefore, nicotine may constitute a more desirable alternative to provide similar information in patients who smoke.
Prior to conducting experiments in humans, it is desirable to collect data in animals to get an estimate of the expected effect size. The current study examines the effect size of [11C]raclopride displacement after nicotine infusion (at doses compatible with administration in humans) in nonhuman primates under isoflurane anesthesia. Similar experiments were performed by Dewey et al (1999), but the effect size could not be deduced from that study. Other such studies have appeared in abstract form Cumming and Gjedde (2001). Tsukada et al (2002) recently showed that even a high dose of nicotine that produced significant changes in vital signs did not cause [11C]raclo-pride displacement in four conscious monkeys, but a small effect was seen in the same animals under anesthesia. In the current study, the dynamics of DA receptor occupancy changes over a period of a few hours after nicotine infusion were compared with the effects of amphetamine. In addition, two methods of tracer administration were compared: (1) ‘bolus plus constant infusion (B/I)’ (Carson et al, 1997; Laruelle et al, 1996), in which constant ligand-receptor equilibrium is reached during the scan, and nicotine administration perturbs this equilibrium, allowing for pre- vs postmeasures of BP in one scan, and (2) paired bolus injections (eg Dewey et al, 1993) where two separate scans, before and after nicotine administration, are used to calculate changes in BP.
MATERIALS AND METHODS
Animals
Five rhesus monkeys (mean weight: 9.8 kg) were studied. Indwelling arterial ports had been placed previously to facilitate arterial blood sampling during the PET scans. Anesthesia was initially induced with ketamine and intubation was performed. After transportation to the PET suite, the animals were placed under isoflurane anesthesia (1–2%). The head of the animal was immobilized in a stereotactic frame. Scans started at least 2 h after ketamine administration. Vital signs were monitored throughout the experiment. These procedures were approved by the Animal Care and Use Committee of the NIH Clinical Center.
PET Procedure
PET scans were performed with a GE Advance scanner (General Electric Medical Systems, Waukesha, WI; reconstructed resolution of 6 mm full-width half-maximum in all directions). Coronal slices covering the whole brain were obtained. A transmission scan was initially performed for attenuation correction. Three [15O]water scans were performed prior to the [11C]raclopride scans. These scans were averaged and used for registration with T1-weighted MRI (SPGR, 0.4 × 0.4 × 1 mm resolution, coronal acquisition) scans for all animals. These [15O]water scans provide for high-quality images with adequate statistics that are generally superior to the sum of the initial time points of the [11C]raclopride scans described below.
The radiotracer was [11C]raclopride (specific activity ranging between 379 and 1142 Ci/mmol, mean 675 Ci/mmol). The monkeys received 2.13 mCi per scan on average. Two modalities of radiotracer administration were used: bolus plus constant infusion (B/I), and two bolus injections (‘bolus’). In the B/I scans, the volume of the bolus portion was equal to that during 60 min of infusion (Carson et al, 1997). Scan frames were 3 × 60, 2 × 90, 2 × 120, 8 × 300, 6 × 200, 16 × 300 s (150 min total scan duration). Two B/I scans were obtained per scanning day (Table 1). In the first one, nicotine was administered i.v. as a prolonged (1 min) bolus at 60 min into the [11C]raclopride infusion, at doses between 0.01 and 0.06 mg/kg (Table 1); no intervention was performed in the second scan in four monkeys out of five. This was done in order to follow the dynamics of change in BP over time. In one animal (MA), nicotine administration was repeated in the second scan at a higher dose. In another animal (PI), the dose of nicotine was doubled in a separate experimental session. For all monkeys who had accessible arterial ports, arterial blood was sampled every 15 s during the first 1.5 min, then at 2, 3, 4, 7, 10, 15, 20, 25, 30, 40, 50, 60, 75, 90, 105, 120, 135, 150 min postinjection. These samples were used to correct for intravascular radioactivity. In one case, the arterial port was inaccessible. In this case, only venous sampling for nicotine levels was performed. There were at least 3 h between the starting times of tracer infusions.
The same animals underwent a scan session with two bolus injections of [11C]raclopride at least 1 month later, with nicotine administration 5 min prior to the second bolus injection, at the same doses as during the B/I scans. A total of 17 PET frames were obtained over 60 min (scan frames were 3 × 60, 2 × 90, 2 × 120, 10 × 300 s). No arterial sampling was performed in these scans. A period of 3 h was allowed between tracer administrations.
Data on the effect of amphetamine administration were obtained from three monkeys of the same species with the same B/I design in which amphetamine 0.4 mg/kg was administered 50 min into the first scan (Carson et al, 2000). One of these animals also underwent the nicotine studies above.
Nicotine samples were obtained from arterial blood at 2, 8, and 15 min after nicotine injection, stored on ice and sent to Medtox Laboratories (St Paul, Minnesota), for quantitative HPLC measurements of nicotine concentration. In the animal without arterial sampling, nicotine measurements were obtained from venous samples.
Data Analysis
Images of BP before and after nicotine were obtained as follows. For B/I scans, decay-corrected PET frames were averaged from 50 to 60 min after the start of raclopride infusion, just prior to nicotine (or amphetamine) injection, and over 40 min starting from 20 min after drug administration. The longer averaging period after drug injection was used to obtain signal-to-noise comparable to that in the images prior to nicotine (Watabe et al, 2000). For follow-up scans without pharmacological intervention, the same time frames were averaged as in the first scan. The [15O]water scans were averaged and registered to the high resolution MRI with a rigid-body six-parameter algorithm using Automated Image Registration (Woods et al, 1993,1998). All the [11C]raclopride-derived images were resampled using the same transformation matrix. A region-of-interest (ROI) over the cerebellum was drawn on the MRI scan and applied to the coregistered, averaged [11C]raclopride PET images. This yielded a value for a receptor-poor reference region. BP images were calculated as

with ‘RAC’ being the average image of the concentration over 10 or 40 min (before or after nicotine, respectively, see above) and CER the average value for the cerebellum during the same time frames. A separate calculation was also performed to correct for vascular contribution:

where blood activity is the decay-corrected radioactivity concentration per milliliters of blood multiplied by the blood volume fraction in brain tissue (0.04 was used; Phelps et al, 1979). All image processing related to calculation of BP images for B/I scans was done with Medx (Sensor Systems, Inc., Sterling, VA).
BP images for paired bolus scans were obtained with the Simplified Reference Tissue Method (SRTM), based on the work of Lammertsma and Hume (1996). The time activity curve for the cerebellum reference region was obtained from an ROI drawn on the registered MRI and applied to each frame of the bolus scans.
ROIs were drawn around the full extent of the basal ganglia on the coregistered MRI, and the BP images were sampled, yielding BP values before and after nicotine (or amphetamine) infusion for all experiments. For the B/I scans, where a follow-up scan was available, two additional measurements were made, approximately 180 and 220 min after drug administration.
The significance of change in BP in the basal ganglia before and after nicotine was investigated with repeated measures ANOVA. Separate tests were performed on the B/I (with and without vascular correction) and bolus scans. An overall repeated measures ANOVA including all measures (B/I without vascular correction and bolus scans) was performed to assess the effect of nicotine administration and of method of radiotracer administration (considered as a repeated measure). We calculated effect size since it is the measure most closely associated with statistical power, and therefore allows prediction of sample size requirements for human studies. Effect size was calculated for the B/I and ‘bolus’ methods separately, according to Cohen (1988); f=absolute value of BP mean difference before−after nicotine/standard deviation of the differences). Power computations were done with GPower (Erdfelder et al, 1996). Amphetamine and nicotine effects were also compared with a repeated measures ANOVA, which was applied to three BP values: before, after 30 min from drug administration, and at follow-up (average of 180- and 220-min postdrug) as repeated measures.
Regional effects within the basal ganglia were also considered. Microdialysis studies have shown that all drugs of abuse, including nicotine, cause DA release in the nucleus accumbens shell in excess of the ‘motor’ striatum (Di Chiara and Imperato, 1988). Our hypothesis was therefore that the area of the basal ganglia including the accumbens and the ventral putamen (the so-called ‘ventral striatum’; Haber and McFarland, 1999), would be most sensitive to the effects of nicotine. To investigate regional differences in BP changes, we used two levels of analysis.
The first one was an exploratory analysis implemented through SPM99 (www.fil.ion.ucl.ac.uk/spm). A template was created for macaca mulatta (the species under investigation) by following the methods of Black et al (1997): each of 12 monkey brain MRIs (resolution 0.4 × 0.4 × 1 mm) was deformed (12 parameter registration) to a single brain. All 12 scans were then averaged to obtain an initial template, which became the reference image for another iteration of registrations, which then were averaged to get a second template. This process was repeated three times. The BP images were masked to remove noisy values outside the basal ganglia, and transformed into the group template space using the product of two transformation matrices ([15O]water PET to individual MRI × individual MRI to group template MRI). The first registration was accomplished in Medx with a rigid body algorithm (AIR), while the second one was a 12 parameter affine registration that relied on FMRIB software library (FSL) algorithms (http://www.fmrib.ox.ac.uk/fsl/ Smith, 2002; Jenkinson and Smith, 2001). The images were then smoothed with an 8 × 8 × 8 mm filter and voxel-by-voxel paired t-statistics were performed. Given the exploratory nature of this analysis, a threshold level of α=0.01 uncorrected for multiple comparisons was chosen.
To confirm the results of the SPM analysis, an ROI analysis was performed. This method consisted of the following steps. (1) Landmarks were established on the template MRI in order to identify physiologically meaningful subsections of the basal ganglia and at the same time segregate areas with the highest t-values on the paired t-group statistics obtained with SPM from those with lower t-values. The landmarks (Figure 1) were: the anterior commissure (AC: separating anterior from posterior putamen), the MRI contour of the basal ganglia on the slice containing the AC, diagonal lines separating the caudate from the putamen on both sides, and a horizontal line connecting the top of left and right putamina in front of the AC (separating ventral and dorsal anterior caudate). (2) These landmarks were drawn on the individual MRI of each animal. (3) The landmarks were then superimposed on the BP images coregistered to the MRI. The landmarks were shifted if they appeared not to match the BP images, which were thresholded to a minimum value of 0.8 to maintain consistency between animals. (4) ROIs were drawn directly on the BP images, following the contour of the basal ganglia and using the landmarks to delimit the ROIs. The B/I BP images were used because they had better statistical quality and the same set of ROIs was used to sample bolus scans for the same animal. The scheme for ROI placement is illustrated in Figure 1. The ROIs included: ventral striatum (roughly corresponding to the definition of Drevets et al, 1999; and Mawlawi et al, 2001), dorsal anterior caudate, posterior caudate, and posterior putamen. The posterior caudate and putamen started 2 mm posterior to the AC. We chose this line of separation rather than the AC, which generally is chosen to separate rostral from caudal sections of the basal ganglia, because our SPM analysis indicated somewhat larger changes in BP of the caudate anterior but not posterior to this line. All regions had a left and right subdivision (eight ROIs for each scan).
Landmark placement on the template and ROIs drawn on PET-BP images registered to the MRI of the animal. The upper row of images shows the positioning of the landmarks on the MRI (the MRI template constructed from 12 high resolution MR images of monkeys of the same species is shown): the image in the center represents a slice through the AC, the images on the left are 3 mm posterior and the images on the right are 2 mm anterior to the AC, respectively. Landmark positioning is described in the text. The lower row of images is an example of how the landmarks are used to delimit the ROIs on the BP images, with posterior putamen in blue, posterior caudate in cyan, ventral striatum in dark green, and anterior-dorsal caudate in magenta. The color scale on the right shows BP range for this monkey.
These ROIs were sampled on all scans and repeated measures ANOVAs were performed with BP before and after nicotine (two levels), ROI (four levels), and side (left/right) as the repeated measures. The interaction terms of these analyses addressed the following questions: (1) are there any ROIs that change more than others under the effect of nicotine (nicotine × ROI interaction)? and (2) is the effect of nicotine lateralized (nicotine × side)? Method of tracer administration was ignored in this analysis so that the entire sample of scans could be used.
Pearson's correlations were used to study the association of nicotine dose and plasma levels with changes in BP before and after nicotine in the basal ganglia as a whole and in single regions. All methods of tracer administration were grouped for this analysis.
Statistical calculations were performed with Statistica (StatSoft Inc., Tulsa, OK).
RESULTS
Nicotine-Induced BP Changes in the Basal Ganglia as a Whole
Table 2 shows the BP without vascular correction for the basal ganglia for all scans, the effect size of the difference before and after nicotine, and nicotine levels measured at each time point.
The change in BP induced by nicotine was −5.6±6.8% SD (F(1,6)=4.51, p=0.07) for B/I scans, −5.1±7.8% (F(1,4)=1.9, NS) for bolus scans, and −5.4±6.9% for the entire sample (F(1,11)=6.8, p<0.03). When comparing the B/I and bolus methods with an ANOVA with two repeated measures factors (nicotine and method) on the five animals that had both scans, no significant difference emerged for method of tracer administration and there was no significant interaction between the effects of nicotine and method. Effect sizes (Table 2) showed a small advantage for B/I scans. Power analyses, performed as a preliminary to human studies, indicated that 12 subjects are sufficient to detect a change in BP with power of 0.8 (α=0.05). For B/I scans alone, 10 subjects would be sufficient, while for bolus scans 17 subjects would be necessary. When B/I scans were corrected for vascular activity, effect size was somewhat reduced as compared to the absence of vascular correction (see Table 3).
There were no significant correlations between nicotine dose or plasma levels and BP changes. The nicotine level used was the one at 8 min, given that the other time points had missing data.
Dynamics of BP Changes Compared Between Nicotine and Amphetamine
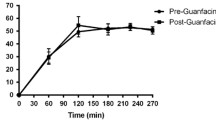
When amphetamine and nicotine were compared for B/I scans, there was a significant effect of group (F(1,7)=8.1, p<0.03), meaning that nicotine studies had overall higher BP than amphetamine, a significant effect of drug administration (F(2,14)=40.6, p<0.00001), meaning that both nicotine and amphetamine caused a significant reduction in BP, and a significant interaction between the drug and group effects (F(2,14)=29.6, p<0.00001), meaning that amphetamine induced a larger and more long-lasting reduction in BP. In fact, BP at baseline and after 180–220 min from nicotine injection were not significantly different (F(1,5)=0.03). The mean change in BP over time for amphetamine and nicotine is summarized in Figure 2.
Regional Effects of Nicotine: SPM Analysis
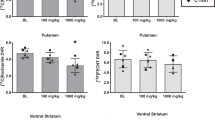
Figure 3 shows the results for the regional exploratory analysis with SPM99 for all 12 scans (p<0.01, uncorrected). A region in the dorsal anterior caudate bilaterally (but more on the right) appeared to be statistically significant above the p=0.01 threshold. The average percent reduction in BP in the region of maximal change around the center of the right anterior-dorsal caudate was −6.5±6% SD (a spherical ROI 6 mm in diameter was sampled around the most significant voxel). To obtain a similar extent of change in the region encompassing the ventral striatum, the significance level had to be thresholded to p=0.1. Other areas of significance were in the right posterior putamen, where the mean percent reduction in BP was −8.1±8.5% SD.
Results of SPM99 analysis for nicotine administration. The panels show sagittal (left top), coronal (right top), and axial views of the macaca mulatta template represented with a gray scale, with superimposed p-values for a paired t-test (thresholded at p<0.01) between 12 BP images before and after nicotine administration represented in color. The color scale on the right represents the range of t-values in the image. The coronal image is in radiological convention (left of the brain displayed on the right of the screen). In the axial image, left is on the bottom, right on top.
Regional Effects of Nicotine: ROI Analysis
When all 12 scans were considered together, with four repeated measures for ROIs (ventral striatum, dorsal anterior caudate, posterior caudate, and posterior putamen), two repeated measures for side (left and right) and two repeated measures for nicotine (before and after), all three factors were statistically significant (F(3,33)=56.9, p<0.00001; F(1,11)=5.46, p=0.04; and F(1,11)=5.07, p=0.04, respectively). The only statistically significant interaction was between side and ROI (F(3,33)=8.1, p<0.001). To describe the origin of these effects, the mean BP across ROIs, hemisphere and nicotine conditions regardless of the other factors were calculated and a Tukey honest significance test was used to test for the differences between means. All ROIs differed significantly from each other (p<0.001), except for dorsal-anterior caudate and posterior putamen, the BP on the left was slightly higher than the right (mean BP across regions and nicotine condition 2.64±0.29 vs 2.60±0.28, respectively) and the BP after nicotine was lower compared to baseline (mean BP across regions and side before nicotine: 2.70±0.29 and 2.56±0.3 after). Moreover, the significant interaction between side and ROI was due to all regions being higher on the left, except for the posterior putamen that was higher on the right.
DISCUSSION
Nicotine produced a small reduction of [11C]raclopride BP in the basal ganglia as a whole at 30 min after its administration. This effect, although statistically significant, was small (5–6% reduction as compared to the baseline BP prior to nicotine administration). As a term of reference, reproducibility measures for the B/I technique in non-human primates are 0±5% in our laboratory, with maximal variation up to 10% for an individual scan (unpublished observations). Mawlawi et al (2001) reported an average % change in BP of 2.8±5.9% in repeat examinations of the whole striatum in humans (where the effects of motion, even after careful correction, are likely to be more significant than in anesthetized monkeys). Given the comparable magnitude of the observed change in BP and the reproducibility ranges of the methods, the conclusion that nicotine caused the changes in [11C]raclopride BP would have been strengthened by reproducibility studies in the same animals. However, our observations that similar results were obtained with the bolus and B/I methods, and that BP returned to baseline levels at 180–210 min after nicotine injection, support the conclusion that this is a nicotine-induced effect.
The observed magnitude of change in BP after nicotine administration is consistent with other literature: Dewey et al (1999) and Schiffer et al (2000) reported a 12% change in BP after nicotine in anesthetized nonhuman primates treated with approximately the same dose of nicotine used here. Other published abstracts report smaller [11C]raclopride displacements after nicotine injections and required higher nicotine doses to achieve the effect. For example, Kim et al (1998), reported no change in [3H]raclopride binding at doses of nicotine below 5 mg/kg in mice; Cumming and Gjedde (2001) found that 0.05 mg/kg nicotine was insufficient to cause changes in [11C]raclopride binding in pigs, but that 0.5 mg/kg caused a 10% reduction in BP. Of particular interest is a recent paper by Tsukada et al (2002), who found that in awake monkeys nicotine at 0.03 mg/kg (bolus) plus a steady infusion at 0.008 mg/kg for 30 min caused no change in [11C]raclopride BP. When the same animals were studied under anesthesia, however, raclopride BP decreased by approximately 10% with the same doses of nicotine. Tripling the dose of nicotine caused a 30–50% larger [11C]raclopride displacement but only during anesthesia. This paper raised interesting issues regarding anesthesia, which appears to increase the effect not only of nicotine but also of amphetamine on DA release. The mechanism of this effect remains obscure, but prior work by that group has shown that both isoflurane anesthesia and cholinergic agonists reduce the availability of the DA transporter in vivo (Tsukada et al, 1999b,2001). Prior to these investigations, studies in brain slices (Salord et al, 1997) had found that anesthesia diminished responsivity of DA neurons to nicotine, an effect in the opposite direction.
Assuming that our measurements reflect a true increase in synaptic DA due to nicotine, it is of interest to verify whether the magnitude of the change is compatible with data obtained from microdialysis. Extrapolating from the data of Breier et al (1997), a 5% change in BP of [11C]raclopride should correspond to a 150% increase in DA release. Clearly, this is only a rough estimate given the differences between that study and the current one. However, Pontieri et al (1996) reported increases in DA output during microdialysis in rats to be between 25 and 50% after doses of nicotine comparable to those used in this experiment. Therefore a much smaller effect would be expected than with amphetamine, where doses of 0.2–0.4 mg/kg in monkey studies caused a 500–1400% increase in extracellular DA (Breier et al, 1997). One would expect smaller effects with drugs that act indirectly on the DA system and do not block the DA transporter. However, Tsukada et al (1999a) have shown the opposite: ketamine and benztropine were 10–20 times more efficient than methamphetamine and GBR12909 in causing reductions in [11C]raclopride BP for the same amount of extracellular secretion of DA. The dose of nicotine administered might also have been a contributor to the small change in BP we observed. We elected to keep the dose of nicotine around 0.03 mg/kg, because this was a dose that Stein et al (1998) reported to be well tolerated when administered as a 1 min i.v. bolus in human smokers (a cigarette contains between 0.01 and 0.03 mg/kg nicotine for a 70 kg person). In summary, the effect of nicotine on DA release is small compared to that of amphetamine; nevertheless it is observable with [11C]raclopride PET scans.
In interpreting this effect, it is also important to note that the competition of DA released through nicotinic activation with [11C]raclopride may not be the only mechanism involved. For example, D2 receptor internalization has been proposed as a possible mechanism for the prolonged displacement of [11C]raclopride after amphetamine administration (Laruelle, 2000) and a recent study has identified this as the primary mechanism in rats (Sun et al, 2003). It is therefore possible that this mechanism contributes to some extent to the reduction of BP observed in this study. We are not aware of in vitro studies showing D2 receptor internalization after exposure to nicotine. Studies in monkeys in vivo have detected an increase in Kd rather than a reduction in Bmax after amphetamine (Carson et al, 2002; Doudet et al, 2000), which would be more consistent with the classical model of competition of DA with [11C]raclopride at the D2 receptor, rather than loss of receptor availability through internalization. Moreover, our observation that the reduction of [11C]raclopride binding was much shorter than with amphetamine, makes this mechanism less likely. Nevertheless, the exact mechanism by which the binding of [11C]raclopride diminishes after infusions of DA agonists has not been elucidated.
We expected to find a significant correlation between BP changes and nicotine dose or nicotine concentrations in the blood. The study by Pontieri et al (1996) showed that at 0.025 mg/kg nicotine, there was an increase of about 25% in the DA output with microdialysis, which doubled at 0.05 mg/kg nicotine, implying a linear relationship between nicotine dose and DA release, at least in the nucleus accumbens shell. A similar experiment at higher doses of nicotine (0.16 and 0.32 mg/kg) also showed dose-dependent increases in DA release with microdialysis (Maisonneuve et al, 1997). The lack of such a correlation in our study may be due to technical factors such as restricted dose range of nicotine, imprecision in the measurements of plasma nicotine levels (eg note the discrepancy in Table 2 between MA at 0.01 and 0.02 mg/kg, and between JE with B/I and bolus scans), and imprecision in the BP measures with PET, or to biological factors such as a threshold effect of nicotine due to rapid receptor desensitization (Grady et al, 1994) and nicotine receptor occupancy increasing in a nonlinear fashion, indicating the possible presence of high and low affinity states of the receptors (Ding et al, 2000). Moreover, results by Endres et al (1997) indicate that for drugs with a short-lived action such as nicotine, it is the integral of nicotine-induced DA release over time that relates best to [11C]raclopride displacement. Therefore, ideally we should have used the integral of nicotine plasma levels rather than the 8 min concentration in our correlations; however, because of several missing data points, this was not possible.
Despite the small change in BP, effect sizes were large enough to indicate that studies in humans are feasible. If the same effects were seen in humans, between 10 and 15 subjects would be required to detect this degree of change in [11C]raclopride BP before and after nicotine with α=0.05 and power of 0.80. This does not generalize though to studies of differences between groups (such as patients with schizophrenia vs controls). A rather large alteration in regulation of nicotine–DA interactions would be required for a difference in percent raclopride displacement to be observed between two groups, possibly requiring in excess of 20 subjects per group to detect differences reliably. The relevance of the current investigation to human applications is further limited by the effects of anesthesia mentioned above.
Although there was no statistically significant difference between the two methods of tracer administration (B/I and bolus), we believe the B/I technique offers some advantages: it is more economical because it provides the same information with a single [11C]raclopride synthesis; calculation of BP images is simplified; values outside the immediate area of the basal ganglia are less noisy than with images created with SRTM, potentially enabling analysis of BP changes over the whole brain; even within the basal ganglia the statistical quality of the images is improved; and it is less sensitive to changes in blood flow (Carson, 2000) induced by nicotine (Domino et al, 2000; Stein et al, 1998; Zubieta et al, 2001). Although these arguments support the use of the B/I method for studies of nicotine-induced DA release, this decision has to be weighted according to the characteristics of the tracer and the displacement expected. The bolus method has the advantage of ease of tracer administration. Furthermore, the B/I method depends upon reaching equilibrium prior to pharmacologic manipulation, which may not always occur. When vascular corrections were applied to the BP values for B/I scans, some reduction of effect size was seen, but this was rather modest. Vascular correction was not applied to bolus studies.
When comparing the effect of nicotine to that of amphetamine, it is obvious that amphetamine causes a much larger reduction in BP, and one that is of much longer duration. This is likely due to the different mechanisms of action of the two drugs. Amphetamine blocks DA transporters and causes presynaptic DA release (Kuczenski and Segal, 1989), while nicotine presumably increases burst firing of dopaminergic neurons for a short period of time (Grenhoff et al, 1986; Murase et al, 1993). The return to baseline binding seen here is consistent with the hypothesis that the change in [11C]raclopride BP is produced by direct competition with transiently increased synaptic DA. However, the issue of dose is also relevant here. Cumming and Gjedde (2001) reported a prolonged reduction in [11C]raclopride BP in pigs given nicotine 0.5 mg/kg, and it is unclear whether very low doses of amphetamine (apt to cause a 5% change in BP of [11C]raclopride, eg, around 0.1 mg/kg) would have a different time course.
The SPM regional analysis showed a tendency for an area compatible with the dorsal-anterior caudate bilaterally and the posterior putamen on the left to decrease in BP after nicotine administration in the B/I scans. However, due to the dimensions of the monkey brain, small misalignments during registration could reduce the sensitivity of SPM analysis. Moreover, the smoothing applied to the data results in an inevitable loss of resolution and partial volume effects that also affect the size and location of the statistically significant areas. Our ROI-based analysis avoided smoothing, minimized misregistration artifacts and at the same time maintained some of the advantages of registration to MRI, such as availability of landmarks not visible on the PET scans. This analysis showed no significant ROI × nicotine interaction, indicating that while nicotine had a significant effect on the basal ganglia as a whole, this was not regionally specific. In particular, the region of the ventral striatum that has been more strongly implicated in reward mechanisms of drugs of abuse (Di Chiara and Imperato, 1988; Drevets et al, 1999) did not show changes in BP to any different extent than other regions within the basal ganglia.
Our regional analysis revealed some unexpected findings: an effect of side (left BP larger than right) and an effect of region (posterior caudate having lower BP than the other regions). Although deserving of further investigation, the left/right difference in BP was minute, and therefore is unlikely to be of clinical relevance. However, several studies have shown that the distribution of DA and its metabolites is lateralized and associated with other measures of lateralization in animals (Cabib et al, 1995) and handedness in humans (de la Fuente-Fernandez et al, 2000; Glick et al, 1982). It is therefore plausible that the small asymmetry we see might be related to the side preference of our animals.
The differences between regions are more consistent than the effects of side, but are most likely entirely attributable to partial volume effects. Also the significant interaction between side and ROI appears to be of little interest.
In conclusion, nicotine infusion causes small displacements of [11C]raclopride of short duration, presumably related to endogenous DA release caused by increased firing of DA neurons, but possibly also due to other mechanisms such as receptor internalization. The effect size should be sufficient to study this phenomenon in human smokers, especially if the B/I technique is used, although a recent abstract claimed no effect on [11C]raclopride binding of cigarette smoking (Barrett et al, 2001). Use of this technique in patients with schizophrenia, however, would be more arduous because of the need to study patients off neuroleptics and the relatively large sample size required for an appropriately powered study.
References
Abi-Dargham A, Rodenhiser J, Printz D, Zea-Ponce Y, Gil R, Kegeles LS et al (2000). Increased baseline occupancy of D2 receptors by dopamine in schizophrenia. Proc Natl Acad Sci USA 97: 8104–8109.
Adler LE, Hoffer LD, Wiser A, Freedman R (1993). Normalization of auditory physiology by cigarette smoking in schizophrenic patients. Am J Psychiatry 150: 1856–1861.
Barrett SP, Okker J, Pihl RO, Dagher A (2001). [11C] Raclopride PET technique used to assess the dopaminergic response to acute tobacco smoking in humans. 7th Annual Meeting of the Society on Research on Nicotine and Tobacco. Seattle, WA. pp 88.
Black KJ, Gado MH, Videen TO, Perlmutter JS (1997). Baboon basal ganglia stereotaxy using internal MRI landmarks: validation and application to PET imaging. J Comput Assist Tomogr 21: 881–886.
Breier A, Adler CM, Weisenfeld N, Su TP, Elman I, Picken L et al (1998). Effects of NMDA antagonism on striatal dopamine release in healthy subjects: application of a novel PET approach. Synapse 29: 142–147.
Breier A, Su TP, Saunders R, Carson RE, Kolachana BS, de Bartolomeis A et al (1997). Schizophrenia is associated with elevated amphetamine-induced synaptic dopamine concentrations: evidence from a novel positron emission tomography method. Proc Natl Acad Sci USA 94: 2569–2574.
Cabib S, D'Amato FR, Neveu PJ, Deleplanque B, Le Moal M, Puglisi-Allegra S (1995). Paw preference and brain dopamine asymmetries. Neuroscience 64: 427–432.
Carson RE (2000). PET physiological measurements using constant infusion. Nucl Med Biol 27: 657–660.
Carson RE, Breier A, de Bartolomeis A, Saunders RC, Su TP, Schmall B et al (1997). Quantification of amphetamine-induced changes in [11C]raclopride binding with continuous infusion. J Cereb Blood Flow Metab 17: 437–447.
Carson RE, Channing MA, Der MG, Hescovitch P, Eckelman WC (2002). Scatchard analysis with bolus/infusion administration of [11C]raclopride: amphetamine effects in anesthetized monkeys. In: Senda M, Kimura Y, Herscovitch P (eds). Brain Imaging Using PET. Academic Press: San Diego, CA. pp 63–69.
Carson RE, Channing MA, Vuong BK, Watabe H, Herscovitch P, Eckelman WC (2000). Amphetamine-induced dopamine release: duration of action assessed with [11C]raclopride in anesthetized monkeys. In: Gjedde A, Hansen SB, Knudsen GM, Paulson OB (eds). Physiological Imaging of the Brain with PET. Academic Press: San Diego, CA. pp 205–209.
Cohen J (1988). Statistical Power Analysis for the Behavioral Sciences, 2nd edn. Erlbaum: Hillsdale, NJ.
Cumming P, Gjedde A (2001). Nicotine induced reduction of [11C]raclopride in pig striatum. J Cereb Blood Flow Metab 21(Suppl 1): S111.
Dalack GW, Healy DJ, Meador-Woodruff JH (1998). Nicotine dependence in schizophrenia: clinical phenomena and laboratory findings. Am J Psychiatry 155: 1490–1501.
de la Fuente-Fernandez R, Kishore A, Calne DB, Ruth TJ, Stoessl AJ (2000). Nigrostriatal dopamine system and motor lateralization. Behav Brain Res 112: 63–68.
de Leon J, Dadvand M, Canuso C, White AO, Stanilla JK, Simpson GM (1995). Schizophrenia and smoking: an epidemiological survey in a state hospital. Am J Psychiatry 152: 453–455.
Dewey SL, Brodie JD, Gerasimov M, Horan B, Gardner EL, Ashby Jr CR (1999). A pharmacologic strategy for the treatment of nicotine addiction. Synapse 31: 76–86.
Dewey SL, Smith GS, Logan J, Alexoff D, Ding YS, King P et al (1995). Serotonergic modulation of striatal dopamine measured with positron emission tomography (PET) and in vivo microdialysis. J Neurosci 15: 821–829.
Dewey SL, Smith GS, Logan J, Brodie JD, Fowler JS, Wolf AP (1993). Striatal binding of the PET ligand 11C-raclopride is altered by drugs that modify synaptic dopamine levels. Synapse 13: 350–356.
Di Chiara G (2000). Role of dopamine in the behavioural actions of nicotine related to addiction [In Process Citation]. Eur J Pharmacol 393: 295–314.
Di Chiara G, Imperato A (1988). Drugs abused by humans preferentially increase synaptic dopamine concentrations in the mesolimbic system of freely moving rats. Proc Natl Acad Sci USA 85: 5274–5278.
Ding YS, Volkow ND, Logan J, Garza V, Pappas N, King P et al (2000). Occupancy of brain nicotinic acetylcholine receptors by nicotine doses equivalent to those obtained when smoking a cigarette. Synapse 35: 234–237.
Diwan A, Castine M, Pomerleau CS, Meador-Woodruff JH, Dalack GW (1998). Differential prevalence of cigarette smoking in patients with schizophrenic vs mood disorders. Schizophr Res 33: 113–118.
Domino EF, Minoshima S, Guthrie S, Ohl L, Ni L, Koeppe RA et al (2000). Nicotine effects on regional cerebral blood flow in awake, resting tobacco smokers. Synapse 38: 313–321.
Doudet DJ, Jivan S, English C, Holden JE (2000). Differential effects of amphetamine and a dopamine transporter blocker on the density and affinity of DA D2 receptors in monkeys: PET studies with [11C]raclopride. Neuroimage 11: S5.
Drevets WC, Price JC, Kupfer DJ, Kinahan PE, Lopresti B, Holt D et al (1999). PET measures of amphetamine-induced dopamine release in ventral versus dorsal striatum. Neuropsychopharmacology 21: 694–709.
Endres CJ, Kolachana BS, Saunders RC, Su T, Weinberger D, Breier A et al (1997). Kinetic modeling of [11C]raclopride: combined PET-microdialysis studies. J Cereb Blood Flow Metab 17: 932–942.
Erdfelder E, Faul F, Buchner A (1996). GPOWER: a general power analysis program. Behav Res Methods, Instrum Comput 28: 1–11.
Gioanni Y, Rougeot C, Clarke PB, Lepouse C, Thierry AM, Vidal C (1999). Nicotinic receptors in the rat prefrontal cortex: increase in glutamate release and facilitation of mediodorsal thalamo-cortical transmission. Eur J Neurosci 11: 18–30.
Glick SD, Ross DA, Hough LB (1982). Lateral asymmetry of neurotransmitters in human brain. Brain Res 234: 53–63.
Grady SR, Marks MJ, Collins AC (1994). Desensitization of nicotine-stimulated [3H]dopamine release from mouse striatal synaptosomes. J Neurochem 62: 1390–1398.
Gray R, Rajan AS, Radcliffe KA, Yakehiro M, Dani JA (1996). Hippocampal synaptic transmission enhanced by low concentrations of nicotine [see comments]. Nature 383: 713–716.
Grenhoff J, Aston-Jones G, Svensson TH (1986). Nicotinic effects on the firing pattern of midbrain dopamine neurons. Acta Physiol Scand 128: 351–358.
Haber SN, McFarland NR (1999). The concept of the ventral striatum in nonhuman primates. Ann NY Acad Sci 877: 33–48.
Jenkinson M, Smith S (2001). A global optimization method for robust affine registration of brain images. Medical Image Analysis 5: 143–156.
Kim SE, Shim I, Oh SJ, Kim SH, Choe YS, Choi Y et al (1998). Nicotine-induced dopamine release evaluated with in vivo H-3 raclopride binding studies: comparison with in vivo microdialysis data. J Nucl Med 39: 206.
Kuczenski R, Segal D (1989). Concomitant characterization of behavioral and striatal neurotransmitter response to amphetamine using in vivo microdialysis. J Neurosci 9: 2051–2065.
Lammertsma AA, Hume SP (1996). Simplified reference tissue model for PET receptor studies. Neuroimage 4: 153–158.
Laruelle M (2000). Imaging synaptic neurotransmission with in vivo binding competition techniques: a critical review. J Cereb Blood Flow Metab 20: 423–451.
Laruelle M, Abi-Dargham A, Gil R, Kegeles L, Innis R (1999). Increased dopamine transmission in schizophrenia: relationship to illness phases. Biol Psychiatry 46: 56–72.
Laruelle M, Abi-Dargham A, van Dyck CH, Gil R, D'Souza CD, Erdos J et al (1996). Single photon emission computerized tomography imaging of amphetamine-induced dopamine release in drug-free schizophrenic subjects. Proc Natl Acad Sci USA 93: 9235–9240.
Leonard S, Adams C, Breese CR, Adler LE, Bickford P, Byerley W et al (1996). Nicotinic receptor function in schizophrenia. Schizophr Bull 22: 431–445.
Maisonneuve IM, Mann GL, Deibel CR, Glick SD (1997). Ibogaine and the dopaminergic response to nicotine. Psychopharmacology (Berl) 129: 249–256.
Mawlawi O, Martinez D, Slifstein M, Broft A, Chatterjee R, Hwang DR et al (2001). Imaging human mesolimbic dopamine transmission with positron emission tomography: I. Accuracy and precision of D(2) receptor parameter measurements in ventral striatum. J Cereb Blood Flow Metab 21: 1034–1057.
Murase S, Grenhoff J, Chouvet G, Gonon FG, Svensson TH (1993). Prefrontal cortex regulates burst firing and transmitter release in rat mesolimbic dopamine neurons studied in vivo. Neurosci Lett 157: 53–56.
Olincy A, Young DA, Freedman R (1997). Increased levels of the nicotine metabolite cotinine in schizophrenic smokers compared to other smokers. Biol Psychiatry 42: 1–5.
Phelps ME, Huang SC, Hoffman EJ, Kuhl DE (1979). Validation of tomographic measurement of cerebral blood volume with C-11-labeled carboxyhemoglobin. J Nucl Med 20: 328–334.
Pidoplichko VI, DeBiasi M, Williams JT, Dani JA (1997). Nicotine activates and desensitizes midbrain dopamine neurons. Nature 390: 401–404.
Pontieri FE, Tanda G, Orzi F, Di Chiara G (1996). Effects of nicotine on the nucleus accumbens and similarity to those of addictive drugs. Nature 382: 255–257.
Radcliffe KA, Fisher JL, Gray R, Dani JA (1999). Nicotinic modulation of glutamate and GABA synaptic transmission of hippocampal neurons. Ann NY Acad Sci 868: 591–610.
Salord F, Keita H, Lecharny JB, Henzel D, Desmonts JM, Mantz J (1997). Halothane and isoflurane differentially affect the regulation of dopamine and gamma-aminobutyric acid release mediated by presynaptic acetylcholine receptors in the rat striatum. Anesthesiology 86: 632–641.
Schiffer WK, Gerasimov MR, Bermel RA, Brodie JD, Dewey SL (2000). Stereoselective inhibition of dopaminergic activity by gamma vinyl-GABA following a nicotine or cocaine challenge: a PET/microdialysis study. Life Sci 66: L169–L173.
Schlaepfer TE, Pearlson GD, Wong DF, Marenco S, Dannals RF (1997). PET study of competition between intravenous cocaine and [11C]raclopride at dopamine receptors in human subjects. Am J Psychiatry 154: 1209–1213.
Smith S (2002). Fast robust automated brain extraction. Human Brain Map** 17: 143–155.
Stein EA, Pankiewicz J, Harsch HH, Cho JK, Fuller SA, Hoffmann RG et al (1998). Nicotine-induced limbic cortical activation in the human brain: a functional MRI study. Am J Psychiatry 155: 1009–1015.
Sun W, Ginovart N, Ko F, Seeman P, Kapur S (2003). In vivo evidence for dopamine-mediated internalization of D2-receptors after amphetamine: differential findings with [3H]raclopride versus [3H]spiperone. Mol Pharmacol 63: 456–462.
Tsukada H, Miyasato K, Kakiuchi T, Nishiyama S, Harada N, Domino EF (2002). Comparative effects of methamphetamine and nicotine on the striatal [(11)C]raclopride binding in unanesthetized monkeys. Synapse 45: 207–212.
Tsukada H, Nishiyama S, Kakiuchi T, Ohba H, Sato K, Harada N (1999a). Is synaptic dopamine concentration the exclusive factor which alters the in vivo binding of [11C]raclopride? PET studies combined with microdialysis in conscious monkeys. Brain Res 841: 160–169.
Tsukada H, Nishiyama S, Kakiuchi T, Ohba H, Sato K, Harada N et al (1999b). Isoflurane anesthesia enhances the inhibitory effects of cocaine and GBR12909 on dopamine transporter: PET studies in combination with microdialysis in the monkey brain. Brain Res 849: 85–96.
Tsukada H, Nishiyama S, Ohba H, Sato K, Harada N, Kakiuchi T (2001). Cholinergic neuronal modulations affect striatal dopamine transporter activity: PET studies in the conscious monkey brain. Synapse 42: 193–195.
Vidal C, Changeux JP (1993). Nicotinic and muscarinic modulations of excitatory synaptic transmission in the rat prefrontal cortex in vitro. Neuroscience 56: 23–32.
Watabe H, Endres CJ, Breier A, Schmall B, Eckelman WC, Carson RE (2000). Measurement of dopamine release with continuous infusion of [11C]raclopride: optimization and signal-to-noise considerations. J Nucl Med 41: 522–530.
Woods RP, Grafton ST, Holmes CJ, Cherry SR, Mazziotta JC (1998). Automated image registration: I. General methods and intrasubject, intramodality validation. J Comput Assist Tomogr 22: 139–152.
Woods RP, Mazziotta JC, Cherry SR (1993). MRI-PET registration with automated algorithm. J Comput Assist Tomogr 17: 536–546.
Zhou FM, Liang Y, Dani JA (2001). Endogenous nicotinic cholinergic activity regulates dopamine release in the striatum. Nat Neurosci 4: 1224–1229.
Zubieta J, Lombardi U, Minoshima S, Guthrie S, Ni L, Ohl LE et al (2001). Regional cerebral blood flow effects of nicotine in overnight abstinent smokers. Biol Psychiatry 49: 906–913.
Acknowledgements
We wish to acknowledge the excellent work of the technical staff of the PET Department, especially Tonya Howe, Paul Baldwin, and Wendy Territo, the work of the cyclotron staff, and the contribution of Margaret Der, without whom this study would not have been possible. There is no conflict of interest pertaining to this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Marenco, S., Carson, R., Berman, K. et al. Nicotine-Induced Dopamine Release in Primates Measured with [11C]Raclopride PET. Neuropsychopharmacol 29, 259–268 (2004). https://doi.org/10.1038/sj.npp.1300287
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1300287
- Springer Nature Switzerland AG
Keywords
This article is cited by
-
Measuring Cigarette Smoking-Induced Cortical Dopamine Release: A [11C]FLB-457 PET Study
Neuropsychopharmacology (2015)
-
Neurobiological background of negative symptoms
European Archives of Psychiatry and Clinical Neuroscience (2015)
-
Dopamine Function in Cigarette Smokers: An [18F]-DOPA PET Study
Neuropsychopharmacology (2014)
-
Elevation of Dopamine Induced by Cigarette Smoking: Novel Insights from a [11C]-(+)-PHNO PET Study in Humans
Neuropsychopharmacology (2014)
-
Imaging Nicotine- and Amphetamine-Induced Dopamine Release in Rhesus Monkeys with [11C]PHNO vs [11C]raclopride PET
Neuropsychopharmacology (2014)