Abstract
Hypoxemia and multiple organ dysfunction are significant contributors to mortality in patients with pediatric acute respiratory distress syndrome (PARDS). P50, the oxygen tension at which hemoglobin is 50% saturated, is a measure of hemoglobin-oxygen affinity, and its alteration might have implications for tissue hypoxia and organ dysfunction. The purpose of this single-center, retrospective study was to evaluate P50 levels in PARDS and to determine the association between P50 and clinical outcomes. The study included 212 children diagnosed with PARDS according to the Pediatric Acute Lung Injury Consensus Conference definition who required invasive mechanical ventilation and had arterial blood gas results of hemoglobin oxygen saturation < 97% at the time of diagnosis. P50 levels were calculated using Doyle’s method, and organ dysfunction was assessed using the Pediatric Logistic Organ Dysfunction-2 score. Most patients exhibited more than one dysfunctional extrapulmonary organ at PARDS onset. P50 increased with increasing PARDS severity (mild (26.6 [24.9–29.6]), moderate (26.8 [25.0–29.5]), and severe PARDS (29.1 [26.1–32.4] mmHg; P = 0.025). Moreover, P50 demonstrated a significant positive association with extrapulmonary organ dysfunction score (β = 0.158, P = 0.007) and risk of mortality (adjusted hazard ratio, 1.056; 95% confidence interval, 1.015–1.098; P = 0.007), irrespective of initial PARDS severity. The relationship between P50 and mortality was largely mediated by extrapulmonary organ dysfunction. A high P50 value at the time of PARDS diagnosis may be associated with mortality via dysfunctional extrapulmonary organs. Future studies should consider P50 as a potential candidate index for risk stratification of PARDS patients.
Similar content being viewed by others
Introduction
Acute respiratory distress syndrome (ARDS) refers to hypoxic respiratory failure due to diffuse pulmonary inflammation. ARDS results in increased capillary endothelial permeability following a variety of direct and indirect injuries to the lung1. Although improvements in pediatric critical care support have led to a decrease in mortality rates, pediatric ARDS (PARDS) remains a significant cause of childhood morbidity and mortality worldwide2,3,4,5.
Of note, the predominant cause of death in PARDS does not appear to be severe hypoxemia, which is one of the defining criteria in PARDS, but multiple organ dysfunction6,7. PARDS is a severe lung disease exhibiting complex pathophysiology that involves not only the respiratory system but also the extrapulmonary end-organs. Therefore, extrapulmonary organ dysfunction is common in both adults and children8,9,10. It generally occurs concurrently with respiratory dysfunction; however, additional organ dysfunction may develop after the onset of respiratory failure11. Previous studies have consistently demonstrated that extrapulmonary organ dysfunction is a strong risk factor for mortality that is independent of hypoxemia degree, or other respiratory criteria7,10,12. The Pediatric Acute Lung Injury Consensus Conference (PALICC) sub-committee has stated that multiple organ dysfunction is ‘the single most important independent clinical risk factor for mortality at the onset of ARDS’13. However, the pathophysiological mechanisms linking multiple organ dysfunction to PARDS remain unclear.
At the tissue level, oxygen supply and demand are dependent on various factors including peripheral oxygen delivery, diffusion from microcirculation to tissue mitochondria, and local tissue oxygen consumption. Abnormalities of systemic gas exchange, such as imbalances between oxygen delivery and uptake, have been suggested as potential mechanisms underlying extrapulmonary organ dysfunction in ARDS with a low level of oxygen uptake below the critical threshold14. Nearly 98% of circulating oxygen is bound to hemoglobin, and the affinity of hemoglobin for oxygen in relation to the partial pressure of oxygen (pO2) is demonstrated by the hemoglobin-oxygen dissociation curve. The oxygen tension at which hemoglobin is 50% saturated (P50) is a measure of the affinity of hemoglobin for oxygen that determines the release of oxygen from microcirculation into tissues15. Therefore, alterations in P50 might have implications for tissue hypoxia and subsequent organ dysfunction via altered oxygen extraction15,16.
Few studies have investigated P50 in ARDS. In addition, no investigation has reported P50 in relation to multiple organ dysfunction in PARDS. Thus, we aimed to evaluate the level of P50 in PARDS patients, investigate the associations between P50 and various organ dysfunctions, and assess the possible link between P50, extrapulmonary organ dysfunction, and clinical outcomes in patients with PARDS.
Materials and methods
Patient selection and P50 calculation
First, we extracted data from the Severance Hospital electronic database and retrospectively reviewed the records of patients aged 1 month to 19 years who were admitted to the intensive care unit (ICU) from January 1, 2010 to January 30, 2017. A total of 1,101 patients were then screened for inclusion in this study. Next, we identified patients with respiratory difficulty requiring invasive mechanical ventilation. Finally, we reviewed medical records to identify if the patient met all the diagnostic criteria of PALICC definition consistent with the timing of onset, etiology for ARDS, chest radiographic images for the presence of pulmonary infiltrates, the origin of edema not fully explained by cardiac failure or fluid overload, and oxygenation parameters. The eligibility criteria were as follows: (1) diagnosis of PARDS according to the PALICC criteria17, which requires invasive mechanical ventilation; and (2) at least one documented arterial blood gas result at the time of PARDS diagnosis. Patients with congenital cyanotic heart disease were excluded because these patients were cared for in a separate cardiothoracic intensive care unit.
In vivo P50 values were calculated using the method described by Doyle18 based on Hill’s equation19 \(\left( {{\text{P5}}0 = {\text{pO}}_{2} \times \left( {\frac{{1 - {\text{SO}}_{2} }}{{{\text{SO}}_{2} }}} \right)^{{\frac{1}{{\text{n}}}}} ,\,{\text{n}} = {2}.{711}} \right)\), which uses pO2 and hemoglobin oxygen saturation (sO2) from a single-point measurement of arterial gases. All arterial gas results were the nearest approximation to the time of PARDS diagnosis and within a maximum of 4 h after diagnosis. Only results with measured sO2 < 97% were utilized because sO2 values ≥ 97% might lead to erroneous calculations at the extremes of the hemoglobin-oxygenation equilibrium curve20. In addition, patients younger than 1 year were excluded from the analysis because fetal to adult hemoglobin switching might not yet fully occurred in this population, and fetal hemoglobin has a higher affinity for oxygen than adult hemoglobin21.
This study was approved, and a waiver was obtained from the Institutional Review Board of Yonsei University Health System, Severance Hospital for informed consent (IRB No. 4-2013-0207). The study was carried out according to the Declaration of Helsinki.
Variable definitions
During the ICU stay, demographics and clinical data were assessed, including PARDS etiology, comorbidity, clinical progress, and outcomes. The Pediatric Index of Mortality 3 scores at ICU admission, and Pediatric Logistic Organ Dysfunction (PELOD)-2 score at the time of PARDS diagnosis were collected. ICU mortality and degree of multiple organ dysfunction were selected as the main outcomes. The PELOD-2 score is generally adopted as a clinically meaningful descriptor for the number and severity of organ dysfunctions in critically ill children22. The total score was subdivided into five types of organ dysfunction (neurological, cardiovascular, renal, respiratory, and hematologic) by relevant variables. Similarly, extrapulmonary organ dysfunction was assessed using the non-respiratory PELOD-223, which was calculated by simply removing the corresponding respiratory variables.
Clinical outcomes of PARDS, such as ICU mortality, duration of invasive mechanical ventilation, and ventilator-free days at 28 days post-diagnosis were also collected. Ventilator-free days were determined for survivors by subtracting the total duration of invasive ventilation from 28 days. In patients who required ≥ 28 ventilator days or ICU non-survivors, the number of ventilator-free days was 0.
Statistical analysis
Categorical data were presented as counts and percentages. Continuous data were tested for normality using the Kolmogorov–Smirnov test and reported as the median with interquartile range. Categorical variables were analyzed using the Chi-square test or Fisher’s exact test, and continuous variables were compared using the Kruskal–Wallis H test with Dunn’s method for multiple comparisons. Correlation between the P50 level and PARDS severity was analyzed with the Spearman’s rank correlation test. Multivariate linear regression analyses controlling for age, sex, weight, comorbidity, and initial PALICC grade were performed to assess the associations between P50 and degree of various organ dysfunctions. Cox’s regression model was employed for survival analysis by adjusting for the aforementioned variables. To investigate the possible mechanism underlying P50 and mortality in PARDS patients, mediation analysis was performed for extrapulmonary organ dysfunction as a potential mediator using the method proposed by Lange et al.24. All statistical analyses were conducted using software SPSS Statistics (version 25.0; IBM Corp., Armonk, NY, USA) and R (version 3.5.2; R Foundation for Statistical Computing, Vienna, Austria). Two-tailed P value < 0.05 was considered to indicate statistical significance.
Ethics approval and consent to participate
This study was approved by the Severance Hospital’s Institutional Review Board, and the requirement for informed consent was waived (IRB No. 4-2013-0207).
Results
Characteristics of the study population
Of the 288 children with PARDS during the study period, 257 exhibited an arterial blood gas of sO2 < 97%. Among them, 45 patients were aged younger than 1 year. The remaining 212 patients were included in the final analysis (Supplementary Fig. 1). The demographics and clinical data of the studied population were stratified according to PARDS severity (Table 1). The subgroups did not differ in age, sex, and weight. The Pediatric Index of Mortality 3 and PELOD-2 scores showed significant differences between groups stratified according to PARDS severity. The scores increased with increasing disease severity. The mortality rate increased with PARDS severity, from mild (26.2%) to moderate (38.9%) to severe (68.3%). Among survivors, there were no significant differences in the ICU length of stay, duration of invasive mechanical ventilation, and ventilator-free days between the severity groups (Table 1).
P50 levels in children with PARDS
A trend of increasing P50 levels with increasing PARDS severity was observed (Fig. 1). P50 was significantly higher (P = 0.049) in patients with severe PARDS (29.1 [26.1–32.4] mmHg) than in those with mild (26.6 [24.9–29.6] mmHg) or moderate (26.8 [25.0–29.5] mmHg) PARDS. The correlation analysis showed a weak but significant positive correlation between the P50 level and PARDS severity (r = 0.153, P = 0.026).
Organ dysfunction in children with PARDS
Most patients (92.0%) exhibited at least one extrapulmonary organ dysfunction at PARDS onset. The number of extrapulmonary organs with dysfunction increased with increasing hypoxemia severity (Table 1). Furthermore, mortality increased with increasing numbers of dysfunctional extrapulmonary organs (Supplementary Fig. 2). Multivariate Cox’s regression analyses demonstrated that PARDS mortality risk was significantly increased with each organ dysfunction included in the nonrespiratory PELOD-2 score, even after adjustment for initial PALICC grade (Supplementary Table 1).
Association between P50 and organ dysfunction
Multiple regression analyses were used to estimate the regression coefficients of P50 and organ dysfunction scores (Table 2). P50 exhibited significant positive associations with the pulmonary (β = 0.024, P = 0.007), extrapulmonary (β = 0.158, P = 0.004), and overall organ dysfunction (β = 0.182, P = 0.001) scores. Extrapulmonary organ dysfunction was further divided into neurological, cardiovascular, renal, and hematologic dysfunction, which revealed significant associations between cardiovascular and renal dysfunction and P50 (β = 0.075, P = 0.001, and β = 0.022, P = 0.046, respectively) (Table 2).
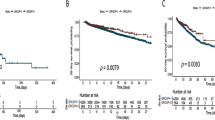
Association between P50 and clinical outcomes in PARDS
Univariate analysis using Cox’s regression revealed that the mortality risk was significantly increased with increasing P50 levels (hazard ratio [HR] for 1 mmHg change in P50, 1.035; 95% confidence interval [CI], 1.003–1.068; P = 0.029). The same association was found after adjustment for potential covariates such as age, sex, weight, comorbidities, and initial PALICC grade (HR, 1.056; 95% CI, 1.015–1.098; P = 0.007). In contrast, no significant associations were observed between P50 and ICU length of stay, invasive mechanical ventilation duration, and ventilator-free days (data not shown).
Putative implications linking P50 to mortality in PARDS
The mediation analysis produced models demonstrating that extrapulmonary organ dysfunction partially mediated the relationship between P50 and mortality in PARDS (Fig. 2). After controlling for the aforementioned potential confounders, including initial PALICC grade, P50 was associated with mortality (HR, 2.045; 95% CI, 1.950–2.143; P < 0.001). The analysis confirmed a significant direct effect (HR, 1.142; 95% CI, 1.037–1.262; P = 0.008) and indirect effect (HR, 1.791; 95% CI, 1.600–2.001; P < 0.001) of extrapulmonary organ dysfunction consistent with the presence of mediation. Extrapulmonary organ dysfunction was estimated to mediate 81.5% of the effect of P50 in PARDS mortality.
Analysis of the effect of P50 on mortality mediated by extrapulmonary organ dysfunction. The effect estimates on hazard ratio scale and 95% confidence intervals (CI) are tabulated for all paths: direct effect, A; indirect effect, B·C; and total effect, A·B·C. The model is adjusted for age, sex, weight, comorbidity, and initial PALICC grade. Proportion mediation is 81.5% (67.3–94.9%). PALICC; Pediatric Acute Lung Injury Consensus Conference.
Discussion
In this study, P50 levels increased with increasing PARDS severity, with a notable difference in children with severe PARDS. P50 exhibited a significant correlation with the degree of extrapulmonary organ dysfunction as well as respiratory dysfunction. The mortality risk was significantly associated with the P50 level, even after adjusting the initial PARDS severity criteria. Moreover, we demonstrated that extrapulmonary organ dysfunction partially mediated the relationship between P50 and mortality in PARDS patients.
In PARDS patients, extrapulmonary organ dysfunction occurred frequently, with an incidence above 90% at the time of PARDS onset. These findings are consistent with previous studies in children with acute respiratory failure or ARDS. Weiss et al.11 reported a prevalence of 63% of concurrent multiple organ dysfunction within a day of the onset of acute respiratory failure, using a multi-centered, prospectively collected dataset of 2449 children. In addition, Kallet et al.8 conducted an analysis on 15 years of data from 1747 adults with ARDS and demonstrated that at least one dysfunctional extrapulmonary organ system was present in 80–90% of patients. This pervasive early-onset extrapulmonary organ dysfunction further supports the concept of PARDS as a pulmonary manifestation of a systemic syndrome9,25.
The exact nature of the association between lung injury and extrapulmonary organ failure in ARDS remains largely unknown. ARDS could be both the cause and the consequence of multiple organ dysfunction9. In ARDS, the redistribution of cardiac output or a loss of recruitable capillary reserve may compromise perfusion within individual organs. Direct endothelial injury and the ensuing alveolar edema increase the diffusion distance for oxygen from the alveoli to the capillaries, and parenchymal damage may impair oxygen utilization14. Furthermore, the concept of systemic microcirculatory injury has been supported by the presence of globally activated intravascular inflammatory mediators in ARDS26,27,28. Other than the lung, a primary target organ, the inflammatory process may spill over into the systemic circulation, resulting in widespread endothelial and parenchymal damage. This may cause altered gas exchange in distal organs in an analogous manner as pulmonary injury and dysfunction29,30.
Our results have demonstrated that the degree of extrapulmonary organ dysfunction and the number of dysfunctional organ systems increased as the PARDS severity increased. All extrapulmonary organ dysfunctions were closely related to the mortality risk, and the greater the number of dysfunctional organs, the higher the mortality rate. Indeed, mortality in critically ill children results from the interactions among multiple failing organs31,32. The pathology of multiple organ dysfunction includes the primary insult, which evokes the host response of the systemic inflammatory process, and the resultant phenomenon of 'organ cross-talk' among individual systems25. Our findings support this reciprocal interaction between the lung and other organs, as well as the contribution of extrapulmonary organ dysfunction to mortality in PARDS, which reinforces the results of previous studies11,12,33,34.
Increased P50, which is equivalent to a rightward shift of the hemoglobin-oxygen dissociation curve, is indicative of a decreased hemoglobin-oxygen binding affinity, which promotes oxygen unloading35. Factors that increase P50 include decreased pH, high levels of erythrocyte 2,3-diphosphoglycerate (2,3-DPG), and fever36. The complicated interplay among these various factors makes it difficult to determine the final P50. For instance, acidemia may increase P50 via the Bohr effect; however, it also reduces 2,3-DPG production, which may decrease P50. Chronic hypoxemia and anemia increase 2,3-DPG, whereas hypophosphatemia decreases 2,3-DPG.
Although this area of clinical research remains rather small, several previous studies that have investigated hemoglobin-oxygen affinity in critical illness have demonstrated conflicting results15. Myburgh et al. reported reduced P50 in critically ill patients37, whereas two recent investigations38,39 revealed no difference in P50 compared to the healthy population. Focusing on ARDS, an Australian group demonstrated leftward shifts of the oxyhemoglobin dissociation curves40. In contrast, a group of Belgium ARDS patients demonstrated a rightward shifted curve41, which is consistent with our findings.
In addition, our study revealed that P50 was associated with mortality regardless of initial PARDS severity, and extrapulmonary organ dysfunction largely mediated this relationship. P50 is ultimately thought to be a comprehensive reflection of increased systemic oxygen demand following increased consumption. Moreover, P50 showed a significant association with the dysfunction of several types of extrapulmonary organs. Extrapulmonary organ dysfunction was a strong risk factor for mortality in PARDS, and the mediation analysis confirmed the link between P50 and death with concurrent extrapulmonary organ dysfunction being a significant mediator independent of potential covariates, including the degree of hypoxemia. Our findings support the role of extrapulmonary organ dysfunction as a potential risk stratification system, and P50 as a likely explanation for this organ cross-talk.
The strength of this study was that it investigated P50 in association with clinical outcomes in PARDS patients. It builds upon the findings of previous studies and demonstrates causal inferences with explanatory variables, including validated criteria for organ dysfunctions. Nevertheless, we acknowledge several limitations that should be considered when interpreting the results. First, our study was conducted using a limited number of patients as this was a single-center study. Only patients who were older than 1 year and had arterial gas results of sO2 < 97% were included. We utilized Doyle’s method to determine P50. This method is a single-point analysis using a pair of oxygen tension and saturation measurements, which is thought to be suitable in daily practice, even for the pediatric population. Although this method had been validated using the data provided by Severinghous42, the calculated P50 involves fundamental limitations, as the values are estimates at best. Finally, our findings primarily focused on P50 and organ dysfunction at the time of PARDS onset, but we did not consider subsequent changes or newly develo** organ dysfunctions. Further prospective validations with a larger sample size are needed to overcome the inherent limitations of this study design.
Conclusions
In conclusion, P50, a measure of hemoglobin-oxygen affinity, may reflect the degree of extrapulmonary organ dysfunction in PARDS and may be associated with mortality. Future studies should consider P50 as a potential candidate index for risk-stratification in PARDS.
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available because they contain information that could compromise research participant privacy.
References
Thompson, B. T., Chambers, R. C. & Liu, K. D. Acute respiratory distress syndrome. N. Engl. J. Med. 377, 562–572 (2017).
Cheifetz, I. M. Pediatric ARDS. Respir. Care 62, 718–731 (2017).
Hough, R. F. Recent advances in pediatric acute respiratory distress syndrome (PARDS). Curr. Pediatr. Rep. 5, 228–236 (2017).
Wong, J.J.-M. et al. Mortality in pediatric acute respiratory distress syndrome: A systematic review and meta-analysis. J. Intensive Care Med. 34, 563–571 (2019).
Beltramo F, Khemani RG. Definition and global epidemiology of pediatric acute respiratory distress syndrome. In Annals of Translational Medicine 7 (2019).
Suchyta, M. R., Orme, J. F. Jr. & Morris, A. H. The changing face of organ failure in ARDS. Chest 124, 1871–1879 (2003).
Dowell, J. C., Parvathaneni, K., Thomas, N. J., Khemani, R. G. & Yehya, N. Epidemiology of cause of death in pediatric acute respiratory distress syndrome. Crit. Care Med. 46, 1811 (2018).
Kallet, R. H., Lipnick, M. S., Zhuo, H., Pangilinan, L. P. & Gomez, A. Characteristics of nonpulmonary organ dysfunction at onset of ARDS based on the berlin definition. Respir. Care https://doi.org/10.4187/respcare.06165 (2019).
Del Sorbo, L. & Slutsky, A. S. Acute respiratory distress syndrome and multiple organ failure. Curr. Opin. Crit. Care 17, 1–6 (2011).
Khemani, R. G. et al. Paediatric acute respiratory distress syndrome incidence and epidemiology (PARDIE): An international, observational study. Lancet Respir. Med. 7, 115–128 (2019).
Weiss, S. L. et al. Multiple organ dysfunction in children mechanically ventilated for acute respiratory failure. Pediatr. Crit. Care Med. 18, 319 (2017).
López-Fernández, Y. et al. Pediatric acute lung injury epidemiology and natural history study: Incidence and outcome of the acute respiratory distress syndrome in children. Crit. Care Med. 40, 3238–3245 (2012).
Group PALICC, Flori, H., Dahmer, M. K., Sapru, A. & Quasney, M. W. Comorbidities and assessment of severity of pediatric acute respiratory distress syndrome: Proceedings from the Pediatric Acute Lung Injury Consensus Conference. Pediatr. Crit. Care Med. 16, S41–S50 (2015).
Dorinsky, P. M. & Gadek, J. E. Mechanisms of multiple nonpulmonary organ failure in ARDS. Chest 96, 885–892 (1989).
Morgan, T. The oxyhaemoglobin dissociation curve in critical illness. Crit. Care Resusc. 1, 93 (1999).
Morgan, T. The significance of the P50. In Yearbook of Intensive Care and Emergency Medicine 1999 (ed. Vincent, J. L.) 433–447 (Springer, 1999).
Group PALICC. Pediatric acute respiratory distress syndrome: Consensus recommendations from the Pediatric Acute Lung Injury Consensus Conference. Pediatr. Crit. Care Med. 16, 428 (2015).
Doyle, D. J. A simple method to calculate P 50 from a single blood sample. Int. J. Clin. Monit. Comput. 14, 109–111 (1997).
Hill, A. V. The possible effects of the aggregation of the molecules of haemoglobin on its dissociation curves. J. Physiol. 40, 4–7 (1910).
Wimberley, P. et al. Guidelines for routine measurement of blood hemoglobin oxygen affinity: International federation of clinical chemistry (IFCC). Scand. J. Clin. Lab. Invest. 50, 227–234 (1990).
Zipursky, A., Neelands, P. J., Pollock, J., Chown, B. & Israels, L. G. The distribution of fetal hemoglobin in the blood of normal children and adults. Pediatrics 30, 262–268 (1962).
Pédiatriques GFdRedU et al. PELOD-2: An update of the PEdiatric logistic organ dysfunction score. Crit. Care Med. 41, 1761–1773 (2013).
Pédiatriques GFdRedU et al. Nonrespiratory pediatric logistic organ dysfunction-2 score is a good predictor of mortality in children with acute respiratory failure. Pediatr. Crit. Care Med. 15, 590–593 (2014).
Lange, T., Vansteelandt, S. & Bekaert, M. A simple unified approach for estimating natural direct and indirect effects. Am. J. Epidemiol. 176, 190–195 (2012).
Khadaroo, R. G. & Marshall, J. C. ARDS and the multiple organ dysfunction syndrome: Common mechanisms of a common systemic process. Crit. Care Clin. 18, 127–141 (2002).
Bhatia, M. & Moochhala, S. Role of inflammatory mediators in the pathophysiology of acute respiratory distress syndrome. J. Pathol. 202, 145–156 (2004).
Crimi, E. & Slutsky, A. S. Inflammation and the acute respiratory distress syndrome. Best Pract. Res. Clin. Anaesthesiol. 18, 477–492 (2004).
Spadaro, S. et al. Biomarkers for Acute Respiratory Distress syndrome and prospects for personalised medicine. J. Inflamm. 16, 1 (2019).
Marshall, J. C. Inflammation, coagulopathy, and the pathogenesis of multiple organ dysfunction syndrome. Crit. Care Med. 29, S99–S106 (2001).
Meduri, G. U., Annane, D., Chrousos, G. P., Marik, P. E. & Sinclair, S. E. Activation and regulation of systemic inflammation in ARDS: Rationale for prolonged glucocorticoid therapy. Chest 136, 1631–1643 (2009).
Watson, R. S., Crow, S. S., Hartman, M. E., Lacroix, J. & Odetola, F. O. Epidemiology and outcomes of pediatric multiple organ dysfunction syndrome (MODS). Pediatr. Crit. Care Med. 18, S4 (2017).
Proulx, F., Gauthier, M., Nadeau, D., Lacroix, J. & Farrell, C. A. Timing and predictors of death in pediatric patients with multiple organ system failure. Crit. Care Med. 22, 1025–1031 (1994).
Flori, H. R., Glidden, D. V., Rutherford, G. W. & Matthay, M. A. Pediatric acute lung injury: Prospective evaluation of risk factors associated with mortality. Am. J. Respir. Crit. Care Med. 171, 995–1001 (2005).
Yehya, N., Servaes, S. & Thomas, N. J. Characterizing degree of lung injury in pediatric acute respiratory distress syndrome. Crit. Care Med. 43, 937–946 (2015).
Srinivasan, A. J., Morkane, C., Martin, D. S. & Welsby, I. J. Should modulation of p50 be a therapeutic target in the critically ill?. Expert Rev. Hematol. 10, 449–458 (2017).
Morgan, T. J. What is p50 (2003).
Myburgh, J., Webb, R. & Worthley, L. The P50 is reduced in critically ill patients. Intensive Care Med. 17, 355–358 (1991).
McLellan, S. A. & Walsh, T. S. Red blood cell 2, 3-diphosphoglycerate concentration and in vivo P50 during early critical illness. Crit. Care Med. 33, 2247–2252 (2005).
Morgan, T., Koch, D., Morris, D., Clague, A. & Purdie, D. Reduced red cell 2, 3-diphosphoglycerate concentrations in critical illness without decreased in vivo P50. Anaesth. Intensive Care 29, 479–483 (2001).
Huang, W., Cade, J. & Pain, M. Oxygen dissociation curve in the adult respiratory distress syndrome. Anaesth. Intensive Care 20, 456–459 (1992).
Clerbaux, T., Detry, B., Reynaert, M. & Frans, A. Right shift of the oxyhemoglobin dissociation curve in acute respiratory distress syndrome. Parodontol. Biol. 45, 269–273 (1997).
Severinghaus, J. W. Blood gas calculator. J. Appl. Physiol. 21, 1108–1116 (1966).
Author information
Authors and Affiliations
Contributions
All authors were involved in the conceptualization and design of the study, and the discussion of the results. Y.K., J.H.J., G.E.K., and M.P. were responsible for acquiring the data. M.L., S.Y.K., and M.J.K. contributed to the analysis of the data and interpretation of the result. Y.K. and S.Y.K. wrote the manuscript. Y.H.K., K.W.K., and M.H.S. revised the article critically for important intellectual content. S.Y.K., as the corresponding author, takes responsibility for the content of the manuscript, including the data and analysis. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, Y., Jung, J.H., Kim, G.E. et al. P50 implies adverse clinical outcomes in pediatric acute respiratory distress syndrome by reflecting extrapulmonary organ dysfunction. Sci Rep 12, 13666 (2022). https://doi.org/10.1038/s41598-022-18038-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-18038-6
- Springer Nature Limited