Abstract
High uric acid (UA) level and high salt intake are reportedly associated with cardiovascular disease. This study investigated the association between UA and urinary sodium excretion, as well as its interaction on the risk of prehypertension. A total of 1869 participants without hypertension were recruited from a previously established cohort in Shaanxi Province, China. The participants were classified as normotensive or prehypertensive on the basis of their blood pressure. Increasing quartiles of sodium excretion were associated with high urinary UA/creatinine levels in prehypertensive participants. Estimated sodium excretion positively correlated with urinary UA/creatinine excretions in the prehypertensive group. In addition, the multivariate-adjusted odds ratios for prehypertension compared with normotension were 1.68 (1.27–2.22) for sodium excretion and 1.71 (1.21–2.42) for serum UA. Increasing sodium excretion and serum UA were associated with higher risk of prehypertension. Compared with the lowest quartiles, the highest sodium excretion and serum UA quartiles entailed 3.48 times greater risk of prehypertension. Sodium excretion is associated with urinary UA excretion in prehypertensive participants. The present study shows that high levels of salt intake and serum UA simultaneously are associated with a higher risk of prehypertension.
Similar content being viewed by others
Introduction
Hypertension contributes to the burden of heart disease, stroke, and kidney failure, and it is one of the leading causes of morbidity and mortality. Prehypertension, a state between normotension and hypertension, is a strong predictor of hypertension1. According to the Seventh Report of the Joint National Committee (JNC-7) guideline, prehypertension is characterized by a systolic blood pressure (SBP) ranging from 120 mm Hg to 139 mm Hg and/or a diastolic blood pressure (DBP) ranging from 80 mm Hg to 90 mm Hg1. The prevalence of prehypertension is rapidly increasing worldwide. In the InterASIA study, the prevalence of prehypertension is 21.9% among Chinese adults (25.7% in males and 18.0% in females)2, and prehypertension is emerging as an independent risk factor for cardiometabolic disorders, including metabolic syndrome, diabetes, chronic kidney disease, stroke, and cardiovascular diseases3,4.
Excessive dietary salt intake plays an important role in the onset and maintenance of hypertension, whereas restricted salt intake lowers blood pressure (BP)5. Dietary salt intake by itself, even without causing hypertension or volume overload, might be deleterious, resulting in cardiac remodeling, renal fibrosis, and left ventricular hypertrophy6,7,8. Several mechanisms, including endothelial dysfunction, oxidative stress, inflammation, insulin resistance, and neurogenically mediated increase in peripheral resistance, contribute to the harmful effects of dietary salt9,10. Recent studies have shown that increased salt intake may be associated with the pathogenesis of prehypertension11,12,13. However, data on the association between dietary salt intake and prehypertension are lacking.
Uric acid (UA) is the metabolic end product of purine degradation in humans; xanthine oxidase is the enzyme responsible for UA production and free radical damage14. Epidemiological studies have identified serum UA is an important risk factor for cardiovascular disease and hypertension15,16,17. For example, Puddu et al.16,17 found that serum UA could predict not only short-term but also long-term incidence of cardiovascular events as well as cardiovascular death and all-cause mortality. Recent studies have shown that increased sodium intake significantly lowers serum UA18,19. However, no research has focused on the relationship between dietary salt intake and UA levels, especially urinary UA excretion, in prehypertensive participants. Furthermore, the relationship between UA and prehypertension and the synergistic effects of UA and dietary salt intake on the risk of prehypertension remain unclear to date.
In the present study, we used our previously established cohort that has been followed up for 30 years to examine the possible associations between urinary sodium excretion, which was used as surrogate for salt intake, and serum and urinary UA levels in prehypertensive participants. We particularly sought to investigate the interactions between urinary sodium excretion and serum UA on the risk of prehypertension in Chinese young adults.
Methods
Cohort of study
In March and April 1987, we established the cohort of Hanzhong Adolescent Hypertension Study based on a baseline survey of 4623 adolescents aged 6–15 years in over 20 schools of three towns (Qili, Laojun, and Shayan) in Hanzhong, Shaanxi, China20,21. To explore the BP trajectory and its risk factors from children to adults, we made the long-term follow-ups of this cohort in 1989, 1992, 1995, 2005, 2013, and 2017 (Supplementary Figure S1).
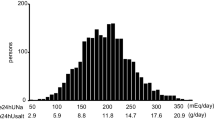
In this study, we followed up this cohort from April to July 2017, and a total of 2780 were followed up this time. The total rate of this follow-up was 60.3%, which was very rare for such a long-term follow-up. The participant selection process is described in Fig. 1. Of the 2780 participants, 911 were excluded from the current analysis for the following reasons: hypertension defined as a SBP ≥140 mm Hg or DBP ≥90 mm Hg or current use of antihypertensive medications (n = 584), missing important data (BP, n = 29; height and weight, n = 1; blood biochemistry, n = 207; urinary biochemistry, n = 87; urinary creatinine, n = 1), and self-identified history of stroke (n = 2). The remaining 1869 individuals were included in the analysis. Data including social demographic survey (age, gender, education, occupation, medical conditions, and prescription and nonprescription medication use), physical activity, physical examination with anthropometric measurements, and laboratory testing were collected by trained physicians or medical students.
The present study complied with the Declaration of Helsinki, and the research protocol was approved by the Ethics Committee of the First Affiliated Hospital of ** hypertension. Circulation 125, 3108–3116 (2012)." href="/article/10.1038/s41598-018-26148-3#ref-CR32" id="ref-link-section-d222118526e3216">32. Another trial performed in 27 men showed that increasing sodium intake from 20 mEq/day to 200 mEq/day decreased UA levels by 1 mg/dL33. In addition, a randomized crossover trial of 103 adults with prehypertension or stage I hypertension showed that 30 days of low versus high sodium intake (60 versus 180 mmol/day) significantly decreased serum UA18,19. In this study, we showed that the serum UA levels were similar between each quartile of estimated sodium excretion in prehypertensive subjects. Furthermore, sodium excretion was not correlated with serum UA and hyperuricemia in the unadjusted and adjusted analyses. The discrepant results of these studies may be attributed to their different study populations, designs, sample sizes, and racial differences.
UA is a product of the metabolic breakdown of purine nucleotides. Approximately 70% of UA is excreted into the urine but is easily filtered into the renal tubule, and about 90% of filtered UA is reabsorbed by the S1 segment of the proximal convoluted tubule32. Approximately 10% of filtered UA is excreted34. To the best of our knowledge, this present study is the first to demonstrate that urinary excretions of UA were significantly associated with sodium excretion in prehypertensive subjects. The mechanism by which sodium intake increases urinary excretion of UA remains unclear. It is possible that the relationship between sodium intake and urinary urate excretion results from effects of sodium intake on glomerular filtration rate and excretion or absorption of urate. Previous physiology studies have shown that reabsorption of sodium and urate accompanies one another at different sites in the nephron35,36. Thus, it is possible that decreased renal reabsorption of sodium from excess sodium intake contributes to a decrease in urate reabsorption. This hypothesis has been evidenced by our interventional study showing that urinary UA excretions were markedly increased during high-salt intake, which was further reinforced by the observation that urinary UA positively correlated with urinary sodium excretion37. Furthermore, a Spanish study also found a directly correlation between the clearance of UA and fractional excretion of sodium, indicating the potential interaction of sodium and UA excretion38. Finally, this relationship may reflect action of the renin-angiotensin system, as uric acid is inversely related to vascular resistance39 and renal blood flow40. Similarly, angiotensin II has been shown to decrease urate excretion after an acute infusion41,42. Determining the molecular mechanism and signaling molecules responsible for the effects of salt intake on urinary UA can be of great interest.
A limited number of studies have examined the relationship serum UA and prehypertension, and findings are conflicting. One US study found a positive association between serum UA and prehypertension with an OR of 1.96 for the top category of serum UA levels compared with the lowest43. Jiang et al.44 described that the OR for prehypertension is 1.36 in subjects with UA ≥365 μmol/L compared with those with UA <215.9 μmol/L after adjusting for many confounders. The other two cross-sectional studies demonstrated that serum UA was independently related to the prevalence of prehypertension in Chinese adults45,46. In contrast, Vucak et al.47 determined that no association existed between elevated serum UA level and prehypertension; this might be because of higher background rate of prehypertension with increasing age that would contribute to a reduction in the odd ratios for serum UA. Recently, a prospective cohort study demonstrates that serum UA is an independent predictor for develo** prehypertension48. In addition, Soletsky et al.49 reported that UA reduction rectifies prehypertension in obese adolescents. In the present study, we consistently showed that higher serum UA category was significantly associated with an increased OR for the presence of prehypertension, compared with the reference group. And the observed positive association between serum UA and prehypertension consistently occurred when serum UA was considered as a continuous variable.
Previously, ample evidence suggests that excess salt intake is positively associated with elevated blood pressure and it can be lowered with reductions in dietary salt5. However, clinical trials scarcely examined the relationship between salt intake and prehypertension. Moinuddin et al.11 showed that daily salt intake of prehypertensives (21.2 ± 1.2 g/day) was significantly greater than normotensive subjects (9.0 ± 0.5 g/day). This result is similar to our study, which found that compared with participants without prehypertension, those with prehypertension tended to have higher urinary sodium excretions (5.20 ± 1.38 vs. 4.86 ± 1.34; P < 0.001). We further observed that the risk of prehypertension was significantly increased with the increasing quartiles of sodium excretion. In addition, Forman et al.32 in a large, prospective, population-based cohort, found that a higher sodium intake is associated with an increased risk of develo** hypertension, particularly in those individuals who have higher levels of serum UA. Our results also showed that salt intake significantly interacted with serum UA. Taken both serum UA and sodium excretion into consideration to assess prehypertension, we found that the risk of prehypertension in the highest quartiles of serum UA and sodium excretion was 3.48 (95% CI, 3.32–5.86) times greater than in the lowest quartile. In other words, participants with higher serum UA levels and salt intake simultaneously were more likely to have a higher risk for prehypertension.
This study has limitations that deserve mention. Firstly, since the study population was included from our previously established cohort, all participants in the present work were middle aged and youth between the ages of 35 and 48 years during the follow-up at 2017. In addition, 24-h urinary sodium excretion was estimated using spot urine samples. Estimated sodium excretions may change according to the urine sampling time because urinary sodium excretion has a circadian rhythm and may also be influenced by the time at which food is consumed. Thus, a single measurement may be insufficient to assess the sodium excretion of individuals. However, spot urine samples are practical at general medical facilities, and the reliability of the findings obtained may be improved using a calculation formula incorporating the estimated 24-hour urinary creatinine excretion based on age, height, and body weight. The validation of the Kawasaki formula was conducted by Mente et al.27. Finally, the study was a single-center, cross-sectional study. A multi-center, prospective trial will be conducted to further understand and confirm the conclusions.
In conclusion, the present study showed that urinary sodium excretion was significantly associated with urinary UA excretions in prehypertensive individuals. However, we failed to find a significant relationship between sodium excretion and serum UA in this Chinese population. In addition, elevated serum UA and sodium excretions appeared to be associated with the development of prehypertension. Individuals with higher serum UA levels and sodium excretions simultaneously had a higher risk for prehypertension. Further clinical trials that include participants with hypertension to investigate evaluate the joint effects of salt intake and serum UA on hypertension and other cardiovascular diseases can be of significant interest. Our findings supported the need for the development of a salt reduction programme.
References
Chobanian, A. V. et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 42, 1206–1252 (2003).
Yu, D. et al. Prevalence and risk factors of prehypertension among Chinese adults. J Cardiovasc Pharmacol 52, 363–368 (2008).
Hsia, J. et al. Prehypertension and cardiovascular disease risk in the Women’s Health Initiative. Circulation 115, 855–860 (2007).
Zhang, Y. et al. Incidence and risk factors for stroke in American Indians: the Strong Heart Study. Circulation 118, 1577–1584 (2008).
Meneton, P., Jeunemaitre, X., de Wardener, H. E. & MacGregor, G. A. Links between dietary salt intake, renal salt handling, blood pressure, and cardiovascular diseases. Physiol Rev 85, 679–715 (2005).
Wang, Y. et al. Salt-induced epithelial-to-mesenchymal transition in Dahl salt-sensitive rats is dependent on elevated blood pressure. Braz J Med Biol Res 47, 223–230 (2014).
Fang, Y., Mu, J. J., He, L. C., Wang, S. C. & Liu, Z. Q. Salt loading on plasma asymmetrical dimethylarginine and the protective role of potassium supplement in normotensive salt-sensitive asians. Hypertension 48, 724–729 (2006).
Frohlich, E. D. & Varagic, J. Sodium directly impairs target organ function in hypertension. Curr Opin Cardiol 20, 424–429 (2005).
Zhu, J., Mori, T., Huang, T. & Lombard, J. H. Effect of high-salt diet on NO release and superoxide production in rat aorta. Am J Physiol Heart Circ Physiol 286, H575–583 (2004).
Li, J. et al. Salt inactivates endothelial nitric oxide synthase in endothelial cells. J Nutr 139, 447–451 (2009).
Moinuddin, A., Gupta, R. & Saxena, Y. Assessment of Anthropometric Indices, Salt Intake and Physical Activity in the Aetiology of Prehypertension. J Clin Diagn Res 10, CC11–14 (2016).
Pal, G. K. et al. Preference for salt contributes to sympathovagal imbalance in the genesis of prehypertension. Eur J Clin Nutr 67, 586–591 (2013).
Wang, Y. et al. The Role of Uric Acid in Hypertension of Adolescents, Prehypertension and Salt Sensitivity of Blood Pressure. Med Sci Monit 23, 790–795 (2017).
So, A. & Thorens, B. Uric acid transport and disease. J Clin Invest 120, 1791–1799 (2010).
Feig, D. I. Serum uric acid and the risk of hypertension and chronic kidney disease. Curr Opin Rheumatol 26, 176–185 (2014).
Puddu, P. E. et al. Serum uric acid and eGFR_CKDEPI differently predict long-term cardiovascular events and all causes of deaths in a residential cohort. Int J Cardiol 171, 361–367 (2014).
Puddu, P. E. et al. Serum uric acid for short-term prediction of cardiovascular disease incidence in the Gubbio population Study. Acta Cardiol 56, 243–251 (2001).
Juraschek, S. P., Choi, H. K., Tang, O., Appel, L. J. & Miller, E. R. 3rd. Opposing effects of sodium intake on uric acid and blood pressure and their causal implication. J Am Soc Hypertens 10, 939–946.e2 (2016).
Juraschek, S. P., Gelber, A. C., Choi, H. K., Appel, L. J. & Miller, E. R. 3rd. Effects of the Dietary Approaches to Stop Hypertension (DASH) Diet and Sodium Intake on Serum Uric Acid. Arthritis Rheumatol 68, 3002–3009 (2016).
Mu, J. et al. Baseline Na-Li countertransport and risk of hypertension in children: a 10-year prospective study in Hanzhong children. J Hum Hypertens 18, 885–890 (2004).
Mu, J. J. et al. Reduction of blood pressure with calcium and potassium supplementation in children with salt sensitivity: a 2-year double-blinded placebo-controlled trial. J Hum Hypertens 19, 479–483 (2005).
Wang, Y. et al. Effect of Salt Intake and Potassium Supplementation on Urinary Renalase and Serum Dopamine Levels in Chinese Adults. Cardiology 130, 242–248 (2015).
Wang, Y. et al. Effect of salt intake and potassium supplementation on serum renalase levels in Chinese adults: a randomized trial. Medicine (Baltimore) 93, e44 (2014).
Imai, E. et al. Prevalence of chronic kidney disease in the Japanese general population. Clin Exp Nephrol 13, 621–630 (2009).
Kawasaki, T., Itoh, K., Uezono, K. & Sasaki, H. A simple method for estimating 24 h urinary sodium and potassium excretion from second morning voiding urine specimen in adults. Clin Exp Pharmacol Physiol 20, 7–14 (1993).
Mente, A. et al. Validation and comparison of three formulae to estimate sodium and potassium excretion from a single morning fasting urine compared to 24-h measures in 11 countries. J Hypertens 32, 1005–1015 (2014).
Mente, A. et al. Association of urinary sodium and potassium excretion with blood pressure. N Engl J Med 371, 601–611 (2014).
Watanabe, S. et al. Uric acid, hominoid evolution, and the pathogenesis of salt-sensitivity. Hypertension 40, 355–360 (2002).
Mazzali, M. et al. Elevated uric acid increases blood pressure in the rat by a novel crystal-independent mechanism. Hypertension 38, 1101–1106 (2001).
Xu, W. et al. Hyperuricemia induces hypertension through activation of renal epithelial sodium channel (ENaC). Metabolism 65, 73–83 (2016).
Hou, L. et al. Influence of Salt Intake on Association of Blood Uric Acid with Hypertension and Related Cardiovascular Risk. PLoS One 11, e0150451 (2016).
Forman, J. P. et al. Association between sodium intake and change in uric acid, urine albumin excretion, and the risk of develo** hypertension. Circulation 125, 3108–3116 (2012).
Egan, B. M., Weder, A. B., Petrin, J. & Hoffman, R. G. Neurohumoral and metabolic effects of short-term dietary NaCl restriction in men. Relationship to salt-sensitivity status. Am J Hypertens 4, 416–421 (1991).
Lytvyn, Y., Perkins, B. A. & Cherney, D. Z. Uric acid as a biomarker and a therapeutic target in diabetes. Can J Diabetes 39, 239–246 (2015).
Ter, M. J. C. et al. Renal handling of urate and sodium during acute physiological hyperinsulinaemia in healthy subjects. Clin Sci (Lond) 92, 51–58 (1997).
Weinman, E. J., Knight, T. F., McKenzie, R. & Eknoyan, G. Dissociation of urate from sodium transport in the rat proximal tubule. Kidney Int 10, 295–300 (1976).
Wang, Y. et al. Effect of Salt Intake on Plasma and Urinary Uric Acid Levels in Chinese Adults: An Interventional Trial. Sci Rep 8, 1434 (2018).
Perez-Ruiz, F. et al. Renal clearance of uric acid is linked to insulin resistance and lower excretion of sodium in gout patients. Rheumatol Int 35, 1519–1524 (2015).
Omvik, P. & Lund-Johansen, P. Issodium restriction effective treatment of borderline and mild essential hypertension? A long-term haemodynamic study at rest and during exercise. J Hypertens 4, 535–541 (1986).
Messerli, F. H., Frohlich, E. D., Dreslinski, G. R., Suarez, D. H. & Aristimuno, G. G. Serum uric acid in essential hypertension: an indicator of renal vascular involvement. Ann Intern Med 93, 817–821 (1980).
Ferris, T. F. & Gorden, P. Effect of angiotensin and norepinephrine upon urate clearance in man. Am J Med 44, 359–365 (1968).
Moriwaki, Y., Yamamoto, T., Tsutsumi, Z., Takahashi, S. & Hada, T. Effects of angiotensin II infusion on renal excretion of purine bases and oxypurinol. Metabolism 51, 893–895 (2002).
Syamala, S., Li, J. & Shankar, A. Association between serum uric acid and prehypertension among US adults. J Hypertens 25, 1583–1589 (2007).
Jiang, L. et al. Joint effects of serum uric acid and body mass index on risk of prehypertension in Chinese population. Clin Chim Acta 446, 1–5 (2015).
Liang, J. et al. Serum uric acid and prehypertension among Chinese adults. J Hypertens 27, 1761–1765 (2009).
Bao, X. et al. Serum concentration of uric acid associated with prehypertension among Chinese population. Angiology 65, 800–805 (2014).
Vucak, J. et al. Association between hyperuricemia, prediabetes, and prehypertension in the Croatian adult population–a cross-sectional study. BMC Cardiovasc Disord 12, 117 (2012).
Liu, L. et al. Serum uric acid is an independent predictor for develo** prehypertension: a population-based prospective cohort study. J Hum Hypertens 31, 116–120 (2017).
Soletsky, B. & Feig, D. I. Uric acid reduction rectifies prehypertension in obese adolescents. Hypertension 60, 1148–1156 (2012).
Acknowledgements
We are indebted to the participants in the study for their outstanding commitment and cooperation. Y.W. is grateful to the China Scholarship Council (No: 201506280092) for a PhD fellowship. This work was supported by the National Natural Science Foundation of China No. 81570381 (J.-J.M.), No. 81600327 (Y.W.), No. 81600574 (L.H.) and No. 81700368 (C.C.), China Postdoctoral Science Foundation funded project (2018M631177), the Clinical Research Award of the First Affiliated Hospital of **’an Jiaotong University of China No. XJTU1AF-CRF-2015–006 (J.-J.M.) and No. XJTU1AF-CRF-2017–021 (Y.W.), Grants 2017YFC1307604 and 2016YFC1300104 from the Major Chronic Non-communicable Disease Prevention and Control Research Key Project of the Ministry of Science and Technology of the People’s Republic of China, and Grant 2017ZDXM-SF-107 from the Key Research Project of Shaanxi Province.
Author information
Authors and Affiliations
Contributions
Y.W. and J.-J.M. conceived and designed the experiments; J.-J.M. and Z.-Y.Y. were responsible for subject recruitment; J.-W.H., K.-K.W., Y.Y., C.C., W.-L.Z., X.-J.X., Y.-B.L., Q.M., K.G., Y.Y. and H.L. performed the experiments; Y.W. and P.-F.Q. analyzed the data; Y.W. and J.-W.H. wrote the paper. All authors read, critically revised and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, Y., Hu, JW., Qu, PF. et al. Association between urinary sodium excretion and uric acid, and its interaction on the risk of prehypertension among Chinese young adults. Sci Rep 8, 7749 (2018). https://doi.org/10.1038/s41598-018-26148-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-26148-3
- Springer Nature Limited
This article is cited by
-
Sex differences in impact of cumulative systolic blood pressure from childhood to adulthood on albuminuria in midlife: a 30-year prospective cohort study
BMC Public Health (2023)
-
The association of urinary prostaglandins with uric acid in hyperuricemia patients
BMC Nephrology (2022)
-
Baseline and change in serum uric acid predict the progression from prehypertension to hypertension: a prospective cohort study
Journal of Human Hypertension (2022)
-
Risk factors for electrocardiographic left ventricular hypertrophy in a young Chinese general population: the Hanzhong adolescent cohort study
BMC Cardiovascular Disorders (2021)
-
Risk factors for subclinical renal damage and its progression: Hanzhong Adolescent Hypertension Study
European Journal of Clinical Nutrition (2021)