Abstract
Background
Pubertal changes in body composition significantly influence future health, with links to various diseases. This study aimed to evaluate the weight changes, fat-free mass (FFM), and body fat mass (BFM) during pubertal growth in Korean children and adolescents.
Methods
We utilized mixed longitudinal data, employing bioelectrical impedance analysis for 4641 height measurements (2204 boys, 2437 girls) from 361 individuals (170 boys, 191 girls) aged 7–18 years. Utilizing the Superimposition by Translation and Rotation (SITAR) model, a shape-invariant growth curve model, reference curves for height, weight, and body composition change velocities were estimated.
Results
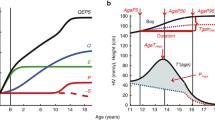
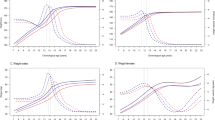
Korean boys experience peak weight velocity (PWV) at an average age of 12.41 years, with a rate of 8.19 kg/year, peak fat-free mass velocity (PFFV) at 12.70 years (7.60 kg/year), and peak body fat mass velocity (PBFV) at 9.69 years (2.67 kg/year). Korean girls show PWV at 11.28 years (6.33 kg/year), PFFV at 11.13 years (4.86 kg/year), and PBFV at 12.33 years (2.72 kg/year). Positive correlations exist among the ages of peak height velocity, PWV, PFFV, and PBFV.
Conclusions
This research represents the groundbreaking application of the SITAR model in analyzing changes in body composition during pubertal growth in Korean children and adolescents.
Impact
-
This study utilized the SITAR model to analyze longitudinal changes in the body composition of the general pediatric population in Korea across pre- and post-pubertal stages, addressing overlooked aspects in cross-sectional studies.
-
Examining growth parameters, including size (mean mass), tempo (timing), and velocity (compression and expansion) for each body component, revealed positive correlations among ages at peak velocities for various body composition parameters.
-
This study can be employed for further investigations that compare the tempo, size, and velocity of various body composition parameters in pediatric disease cohorts and the general population.



Similar content being viewed by others
Data availability
The data that support the findings of this study are available from The Global Prediction Co., Ltd. but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of The Global Prediction Co., Ltd.
References
Lister, N. B. et al. Child and adolescent obesity. Nat. Rev. Dis. Prim. 9, 24 (2023).
Choi, K. M. Sarcopenia and sarcopenic obesity. Korean J. Intern. Med. 31, 1054–1060 (2016).
Kyle, U. G., Schutz, Y., Dupertuis, Y. M. & Pichard, C. Body composition interpretation. Contributions of the fat-free mass index and the body fat mass index. Nutrition 19, 597–604 (2003).
Córdoba-Rodríguez, D. P. et al. Fat-free/lean body mass in children with insulin resistance or metabolic syndrome: a systematic review and meta-analysis. BMC Pediatr. 22, 58 (2022).
Xu, R., Zhang, X., Zhou, Y., Wan, Y. & Gao, X. Percentage of free fat mass is associated with elevated blood pressure in healthy Chinese children. Hypertens. Res. 42, 95–104 (2019).
Alberga, A. S., Sigal, R. J., Goldfield, G., Prud’ homme, D. & Kenny, G. P. Overweight and obese teenagers: why is adolescence a critical period? Pediatr. Obes. 7, 261–273 (2012).
Cheng, G. et al. Velocities of weight, height and fat mass gain during potentially critical periods of growth are decisive for adult body composition. Eur. J. Clin. Nutr. 69, 262–268 (2015).
Uauy, R., Kain, J. & Corvalan, C. How can the developmental origins of health and disease (DOHaD) hypothesis contribute to improving health in develo** countries? Am. J. Clin. Nutr. 94, 1759S–1764S (2011).
Kyle, U. G., Earthman, C. P., Pichard, C. & Coss-Bu, J. A. Body composition during growth in children: limitations and perspectives of bioelectrical impedance analysis. Eur. J. Clin. Nutr. 69, 1298–1305 (2015).
Chula de Castro, J. A., Lima, T. R. & Silva, D. A. S. Body composition estimation in children and adolescents by bioelectrical impedance analysis: a systematic review. J. Bodyw. Mov. Ther. 22, 134–146 (2018).
Cole, T. J., Donaldson, M. D. & Ben-Shlomo, Y. SITAR—a useful instrument for growth curve analysis. Int. J. Epidemiol. 39, 1558–1566 (2010).
McCarthy, A. et al. Birth weight; postnatal, infant, and childhood growth; and obesity in young adulthood: evidence from the Barry Caerphilly growth study. Am. J. Clin. Nutr. 86, 907–913 (2007).
Kuzawa, C. W. et al. Birth weight, postnatal weight gain, and adult body composition in five low and middle income countries. Am. J. Hum. Biol. 24, 5–13 (2012).
Dietz, W. H. Critical periods in childhood for the development of obesity. Am. J. Clin. Nutr. 59, 955–959 (1994).
Zheng, Y. et al. Association of body composition with pubertal timing in children and adolescents from Guangzhou, China. Front. Public Health 10, 943886 (2022).
Chen, Y. C. et al. Assessing causality between childhood adiposity and early puberty: a bidirectional Mendelian randomization and longitudinal study. Metabolism 100, 153961 (2019).
Nyati, L. H., Pettifor, J. M., Ong, K. K. & Norris, S. A. The association between the timing, intensity and magnitude of adolescent growth and body composition in early adulthood. Eur. J. Clin. Nutr. https://doi.org/10.1038/s41430-023-01293-9 (2023).
Cheng, H. L. et al. The tempo and timing of puberty: associations with early adolescent weight gain and body composition over three years. Child Adolesc. Obes. 5, 16–27 (2022).
Cole, T. J. et al. Using super-imposition by translation and rotation (SITAR) to relate pubertal growth to bone health in later life: the Medical Research Council (MRC) National Survey of Health and Development. Int. J. Epidemiol. 45, 1125–1134 (2016).
Tanner, J. M. & Whitehouse, R.H. Atlas of Children’s Growth (Academic Press, 1982).
Cole, T. J. Tanner’s tempo of growth in adolescence: recent SITAR insights with the Harpenden Growth Study and ALSPAC. Ann. Hum. Biol. 47, 181–198 (2020).
Eckert-Lind, C. et al. Worldwide secular trends in age at pubertal onset assessed by breast development among girls: a systematic review and meta-analyzis. JAMA Pediatr. 174, e195881 (2020).
Pierce, M. & Hardy, R. Commentary: the decreasing age of puberty—as much a psychosocial as biological problem? Int. J. Epidemiol. 41, 300–302 (2012).
Gluckman, P. D. & Hanson, M. A. Changing times: the evolution of puberty. Mol. Cell. Endocrinol. 254, 26–31 (2006).
Cole, T. J. Secular trends in growth. Proc. Nutr. Soc. 59, 317–324 (2000).
Kaplowitz, P. B. Link between body fat and the timing of puberty. Pediatrics 121, S208–216, (2008).
Aksglaede, L., Olsen, L. W., Sørensen, T. I. & Juul, A. Forty years trends in timing of pubertal growth spurt in 157,000 Danish school children. PLoS ONE 3, e2728 (2008).
Ohlsson, C. et al. Secular trends in pubertal growth acceleration in Swedish boys born from 1947 to 1996. JAMA Pediatr. 173, 860–865, (2019).
Tanner, J. M. & Davies, P. S. Clinical longitudinal standards for height and height velocity for North American children. J. Pediatr. 107, 317–329 (1985).
Gerver, W. J. M. & De Bruin, R. Growth velocity: a presentation of reference values in Dutch children. Horm. Res. 60, 181–184, (2003).
De Onis, M. et al. Comparison of the World Health Organization growth velocity standards with existing US reference data. Pediatrics 128, e18–26, (2011).
Wells, J. C. et al. Body-composition reference data for simple and reference techniques and a 4-component model: a new UK reference child. Am. J. Clin. Nutr. 96, 1316–1326 (2012).
Forte, G. C. et al. Can skinfold thickness equations be substituted for bioimpedance analysis in children? J. Pediatr. 97, 75–79 (2021).
Ekelund, U. et al. Upward weight percentile crossing in infancy and early childhood independently predicts fat mass in young adults: the Stockholm weight development study (SWEDES). Am. J. Clin. Nutr. 83, 324–330 (2006).
Wasyluk, W., Wasyluk, M., Zwolak, A. & Łuczyk, R. J. Limits of body composition assessment by bioelectrical impedance analysis (BIA). J. Educ. Health Sport 9, 35–44 (2019).
Khalil, S. F., Mohktar, M. S. & Ibrahim, F. The theory and fundamentals of bioimpedance analysis in clinical status monitoring and diagnosis of diseases. Sensors 14, 10895–10928 (2014).
Coppini, L. Z., Waitzberg, D. L. & Campos, A. C. Limitations and validation of bioelectrical impedance analysis in morbidly obese patients. Curr. Opin. Clin. Nutr. Metab. Care 8, 329–332 (2005).
Faria, S. L., Faria, O. P., Cardeal, M. D. & Ito, M. K. Validation study of multi-frequency bioelectrical impedance with dual-energy X-ray absorptiometry among obese patients. Obes. Surg. 24, 1476–1480 (2014).
Antonio, J. et al. Comparison of dual-energy X-ray absorptiometry (DXA) versus a multi-frequency bioelectrical impedance (InBody 770) device for body composition assessment after a 4-week hypoenergetic diet. J. Funct. Morphol. Kinesiol. 4, 23 (2019).
Potter, A. W. et al. High precision but systematic offset in a standing bioelectrical impedance analysis (BIA) compared with dual-energy X-ray absorptiometry (DXA). BMJ Nutr. Prev. Health 5, 254–262 (2022).
Kabiri, L. S., Hernandez, D. C. & Mitchell, K. Reliability, validity, and diagnostic value of a pediatric bioelectrical impedance analysis scale. Child. Obes. 11, 650–655 (2015).
Ramnitz, M. S. & Lodish, M. B. Racial disparities in pubertal development. Semin. Rneprod. Med. 31, 333–339 (2013).
Meyer, K. A. et al. Ethnic variation in body composition assessment in a sample of adolescent girls. Int. J. Pediatr. Obes. 6, 481–490 (2011).
Acknowledgements
We would like to thank Enago for their English editing services.
Funding
This research was supported by “Regional Innovation Strategy (RIS)” through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (MOE) in 2024 (2022RIS-005).
Author information
Authors and Affiliations
Contributions
Dohyun Chun: acquisition of data, analysis, drafting the article, final approval of article. Seo Jung Kim: drafting the article, revising it critically for important intellectual content, final approval of article. Junghwan Suh: conception, design, interpretation of data, final approval of article. Jihun Kim: conception, design, interpretation of data, final approval of article. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
D.C. and J.K. are employees and holding stocks of Global Prediction Co., Ltd. S.J.K. and J.S. declare that they have no competing interests.
Ethics approval and consent to participate
This study was approved by the Institutional Review Board (IRB) of Yonsei Medical University, and the need for informed consent was waived because this was a de-identified retrospective study (IRB No. 4-2023-1312).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chun, D., Kim, S.J., Suh, J. et al. Timing, velocity, and magnitude of pubertal changes in body composition: a longitudinal study. Pediatr Res (2024). https://doi.org/10.1038/s41390-024-03299-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-024-03299-w
- Springer Nature America, Inc.